Abstract
Objective: The authors intended to evaluate the application of neuroendoscopic techniques for the treatment of arachnoid cysts in children and compare it with other operative methods. Methods: The analysis covered the results of treatment of 44 children with arachnoid cysts who were subjected to neuroendoscopic procedures and 62 patients who underwent other operations. Results: The neuroendoscopic treatment of arachnoid cysts was very effective because of low rate of reoperative treatment (six out of 44 patients), no need to change the operative method (40 effective out of total 44 operative procedures), and low rate of persistent worsening (none of 44 patients worsened). Conclusions: Summing up all the mentioned aspects of neuroendoscopic techniques, the neuroendoscopic techniques were the most suitable operative procedures in the treatment of arachnoid cysts in the presented group of patients, providing that the connection between the lumen of the arachnoid cyst and the cerebrospinal fluid cisterns was of good quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Still there is a lack of a fixed algorithm of surgical treatment of arachnoid cysts. Many problems are related to the choice of a proper operative technique. The aim of the presented work is to answer the question if neuroendoscopy should replace all other operative procedures in the treatment of arachnoid cysts.
Materials and methods
The analyzed group was composed of children suffering from arachnoid cysts who were operated with the use of neuroendoscopic methods. This group comprised 44 patients (16 girls and 28 boys). The children varied from 1 day to 18 years of age, 4.6 years (±5.1 SD) on the average. In the analyzed group, the period of clinical observation differed in length from 1 week to 4 years, 0.6 years (±0,76 SD) on the average. Concerning the location of arachnoid cysts, the neuroendoscopic group comprised children who suffered from arachnoid cysts of Sylvian fissure (twenty-four patients), cerebral convexity (twelve patients), cerebral base (six patients), posterior fossa (two patients).
The control group consisted of 62 children (22 girls and 40 boys) who underwent operations other than neuroendoscopic procedures. Their ages ranged from 22 days to 18 years, 7.2 years (±6.1 SD) on the average. In the control group, the period of clinical observation ranged from 6 months to 7 years and the mean period of follow-up was 2 years (±1.7 SD). The locations of the arachnoid cysts were as follows: 33 in the Sylvian fissure, 16 on the cerebral convexity, six on the cerebral basis, and seven in the posterior fossa.
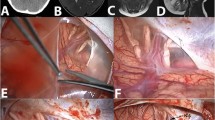
The GAAB 5.4 mm or the Aesculap 6.4 mm, both four-channel neuroendoscopes, were used during the course of each operation. These devices were assisted by Fogarthy catheters, which varied in diameter from 3 to 5 F. In the presented material, most children who were operated suffered from symptomatic arachnoid cysts. If the patients of the Research Institute of the Polish Mothers’ Memorial Hospital (RIPMMH) were free of symptoms, they were operated on due to an increase of the cyst size shown by the serial diagnostic imaging. Neuroendoscopic techniques were applied to perform cystocysternostomy (a connection between the lumen of the arachnoid cyst and: the Sylvian fissure cistern, the ambient cistern, the interpeduncular cistern, the quadrigeminal plate cistern, or cystosubdurostomy). In the control group, two main methods of operative treatment can be distinguished: the restoration of the natural cerebrospinal fluid (CSF) hydrodynamic balance (microsurgical cyst excision, tapping of a cyst through a burr hole) and the extracranial (CSF) diversion (cystoperitoneal shunt implantation, temporary external drainage of CSF) (Table 1). Comparing the effectiveness of the undertaken procedures in the treatment of arachnoid cysts, the shunt implantation was considered to be effective if there was no need for shunt revision, but other operative techniques were considered effective if there was no need to change the type of a surgical procedure. The final clinical outcome was assessed according to the change of patients’ initial clinical state and the observed neurological symptoms. The patients’ status was described as “improvement”, “no change”, or “worsening”. Those who needed more than one operation were assessed with regard to the last surgical procedure. That resulted in differences in the data between (Table 1) and (Table 2). In addition to the clinical state, the results revealed by the diagnostic imaging were also examined. Arachnoid cysts were described as: “unchanged”, “reduced insignificantly” (reduced in size by 10%), “‘noticeably reduced” (reduced in size by more than 10% and less than 50%), “significantly reduced” (more than 50% and less than 90%), and “completely reduced” (more than 90%). Also assessed in the analysis of neuroendoscopic procedures were the influence of the following events: finding and destroying the “valve mechanism” in the arachnoid cyst wall, the “pulsation” of the operation-made anastomosis between the lumen of the cyst and a CSF cistern, and the intensity of the intraoperative bleeding observed by the neuroendoscopic optic system. A special scale was established to assess the intensity of an intraoperative bleeding, based on the sharpness of the picture of the operative field. The lowest level of intraoperative bleeding was characterized by a clear vision of the operative field. The medium level was characterized by a blurred vision, and the highest intensity of bleeding was recognized when blood made the observation of the operative field completely impossible. Statistical analysis was done using statistical tests like the χ 2 Pearson test, the Fisher test, and also the nonparametric Mann–Whitney test. The choice of the nonparametric test was determined by the size of a particular sample.
Observations and results
In the presented material, the following procedures were characterized by the significantly highest effectiveness (χ 2 Pearson test p=0.01153): tapping of a cyst (2/2 effective procedures), microsurgical cyst excision (25/27 successful operations), and neuroendoscopic procedures (40/44 positive results) (Table 1). The least effective procedures were shunt implantation (17/27 successful operations) and external drainage (4/6 successful operation). Four out of six patients treated by temporary ventricular drainage, who did not need any other operative treatment after the removal of ventricular drainage, had an arachnoid cyst revealed by means of diagnostic imaging made because of a central nervous system (CNS) trauma. Two other children, who needed additional operative treatment after the removal of the intraventricular drainage, suffered from congenital arachnoid cysts confirmed by a prenatal examination. Concerning the location of arachnoid cysts, it was observed that the operative methods in restoring natural balance in the cerebrospinal fluid hydrodynamics (neuroendoscopy 21/24 effective procedures, microsurgical cyst excision 12/13 effective procedures) were more effective than extracranial CSF diversion in arachnoid cysts located in the Sylvian fissure region (shunt implantation 11/17 effective procedures, CSF drainage 2/3 effective procedures; Fisher test p=0.0337).
Analyzing separately the effectiveness of the undergone neuroendoscopic procedures, it was noticed that it was not influenced by the following factors: intensity of intraoperative bleeding (Fisher test p=0.4956), destruction of the “valve mechanism” (Fisher test p=0.24392), the “pulsation” of the operation-made anastomosis between the lumen of the cyst and a CSF cistern (Fisher test p=0.12640). However, there was a statistically significant difference in the effectiveness of the operative procedures between the two different types of neuroendoscopic operations. The cystosubdural anastomoses were less effective than the cystocysternal anastomoses (Fisher test p=0.04581).
The presented material was assessed also with regard to the change of the clinical state regarding persistent deterioration after operative treatment during the time of follow up. There was a statistically significant influence of the chosen operative method (concerning last operative treatment) on the change of the clinical state after the operation in the entire group (χ 2 Pearson test p=0.03373). Persistent worsening was observed only after shunt implantation (4/30 of that group) and after microsurgical cyst excision (1/29 of the mentioned patients) (Table 2). The shunt-related persistent deteriorations were observed only in the cases of cysts of the Sylvian fissure region, and were related to an onset of epilepsy (two children), spastic quadriparesis after a shunt-related infection of the central nervous system (one child), and a mild right hemiparesis after a shunt implantation (one child).
The only child who revealed persistent worsening after craniotomy presented left-side hemiparesis and blindness of the right eye after last operative treatment.
The overall rate of improvement in the presented material was 68.87% of the patients operated. Irrespective of the location of arachnoid cysts, there was a statistically significant relation between the observed initial symptoms and the change of the clinical state after operative treatment. The highest rate of improvement was characteristic for children with increased intracranial pressure as a dominant symptom (48/58 of the group), and with the onset of epileptic seizures (13/18 of the group). The observed difference was of statistical significance (χ 2 Pearson p=0.00033). Moreover, the higher the rate of reoperative treatment, the worse clinical outcome concerning the change of clinical state after operative treatment was obtained (χ2 Pearson p=0.00193). The observed improvement in children who needed only one operation was 57/82, but the improvement in patients who needed more than one operations was 16/24.
The statistical relation between the type of the initial operative treatment and the rate of reoperative treatment was also observed. The low rate of reoperative treatment was observed in the group treated by surgical methods restoring CSF fluid hydrodynamics like neuroendoscopic techniques (6/44 patients needed more than one procedure) and microsurgical cyst excision (2/27 patients needed more than one procedure). The highest rate of reoperative treatment was generated by shunt implantation (13/27 patients needed more than one procedure). The observed difference was of statistical significance (χ 2 Pearson test p=0.0108).
The risk of intraoperative complication was not higher in the group treated by neuroendoscopic techniques than in other groups (χ 2 Pearson test p=0.79408). In the group of patients treated by neuroendoscopic technique 11, patients suffered from complications after the operative treatment like: CSF liquorrhea from the postoperative wound (five children), irritation of the 3rd nerve by the Fogarthy catheter (two children), subdural haematomas (two children), central nervous system infections (one child), and intensive intraoperative bleeding (one child). After the microsurgical cyst excision, complications were present in three cases: CSF subcutaneous collection (one child), excessive intraoperative bleeding resulted in left-side hemiparesis and persistent blindness of the right eye (one child), and transient exacerbation of epileptic seizures (one child). After shunt implantations in six cases, complications were observed like disconnection of the peritoneal catheter, chronic subdural haematoma, suppurative peritonitis and CNS infection, intraventricular isolated compartments, dislocation of the intracystical catheter, and the overdrainage syndrome. Only one case of drainage of the Sylvian fissure arachnoid cyst was complicated by a CSF liquorrhea.
In a separate analysis of such factors as “pulsation” of the neuroendoscopically made communication between the lumen of the cyst and cerebrospinal fluid pathways (Fisher test p=0.0861), intraoperative bleeding (Fisher test p=0.5058), the presence of a “valve mechanism” in the cyst wall (Fisher test p=0.7428) in the neuroendoscopic group, it was observed that none of them had any statistically significant influence on changing clinical state after operative treatment.
There also was no statistically significant relation between the type of neurosurgical treatment, the arachnoid cyst location, and changing of the clinical state after operative treatment.
The relation between reduction of the arachnoid cyst size after the operative procedure and the chosen method of treatment was also analyzed. Only for the cysts located in the Sylvian fissure a relation of statistical significance was found (Fisher test p=0.0003). The highest rate of more than 50% cyst volume reduction was obtained for shunt implantation (13 of 17 all shunt implantations) and temporary intraventricular drainage (three of three procedures). The lowest rate of more than 50% of cyst volume size reduction was observed after neuroendoscopic procedures (eight of 24 procedures), and microsurgical cyst excision (seven of 13 procedures). There also was a statistically significant relation between the improvement of the clinical state and the degree of arachnoid cyst reduction after a surgical treatment in the whole group (χ 2 Pearson test p=0.00135). This was exemplified by the fact that 44 out of 57 patients who had a primary cyst volume reduced by more than 50% of its initial size, demonstrated clinical improvement. In contrast, only 29 out of 49 patients, whose primary cyst volume was not reduced by more than 50% showed clinical improvement. Analyzing separately only those arachnoid cysts located in the Sylvian fissure region, despite the highest degree of reduction of arachnoid cysts treated by the CSF extracranial diversion, the rate of clinical improvement was not significantly higher, (Fisher test p=0.3111). It should be added that there was a relation of statistical significance between the high degree reduction of the arachnoid cyst size (more than 50% of initial volume) and the presence of increased intracranial pressure as the dominating primary symptom (Fisher test p=0.0425). Thirty-nine out of 58 children, who demonstrated mainly symptoms of increased intracranial pressure during admission, had arachnoid cysts reduced by more than 50% of their initial size after surgical treatment.
The children who were treated by the neuroendoscopic method were hospitalized for a shorter period than other patients. An average period of hospitalization after neuroendoscopic procedures was 13.4545 days (±10.5638 SD), while the rest of patients were hospitalized on the average for 17.6557 days (±11.2448 SD). The observed difference was of statistical significance (Mann–Whitney p=0.0114).
Discussion and conclusions
In the presented material, it has been shown that the effectiveness of surgical treatment of arachnoid cysts defined by no need to change the performed operative method or by a low rate of repetitive surgical procedures depends on the chosen operative methods. Before the renaissance of neuroendoscopic techniques during the last two decades, the techniques conventionally applied to the treatment of arachnoid cyst were as follows: microsurgical excision, microsurgical fenestration of a wall (ventriculocystocysternostomies, cystosubdurostomies), stereotactic aspiration of cyst contents, and shunt implantations. Unfortunately, minimally invasive techniques like stereotactic aspiration were not very effective and repetitive procedures were sometimes necessary [1–3, 7–12, 14, 16, 17]. There are two main mechanisms of arachnoid cyst increase, namely, the valve mechanism and the “water pump”. Both mechanisms force a one-way flow of fluid into the lumen of an arachnoid cyst [1, 2, 4, 5, 7, 8, 12, 15, 16]. In the presented material, high effectiveness of neurophysiological methods restoring the CSF physiological circulation (microsurgical cyst excision, tapping of the cyst through the burr hole, neuroendoscopy) was observed in the treatment of arachnoid cysts. The main objective of neuroendoscopic procedures is to restore a free CSF circulation along fluid pathways [4, 14]. There was no statistically significant influence on the effectiveness of neuroendoscopic procedures by factors such as: “pumping” of the endoscopically made fenestration of the arachnoid cyst wall, or the presence of a “valve mechanism”. There was no statistically significant influence of high intensity of intraoperative bleeding on effectiveness of the procedures, despite the fact that other authors claimed that bleeding could result in a reclosure of the endoscopically made fenestration and a failure of the whole procedure [2]. In the presented material, the effectiveness of the neuroendoscopic treatment depended on the quality of restoring free communication between the lumen of a cyst and subarachnoid pathways, which is shown by higher effectiveness of neuroendoscopic cystocysternostomies than this of cystosubdurosotmies. The same observation was published with regard to microsurgical treatment [7, 8, 17]. The other effective operative method of treatment of arachnoid cysts, the microsurgical cyst excision, is very invasive and connected with an increased risk of complications [1, 5–8, 12, 14, 16]. In the presented material, the most effective surgical procedure was the tapping of cysts accessible by trephination. But this method had a very limited application, which was restricted to cysts located superficially on the cerebral convexity, and of limited size, which allowed the inspection of external and internal walls by loupe to partially remove them. This is why that method was used only in two cases. The least effective methods like cystoperitoneal shunts or external drainage were burdened with shunt revisions. This problem is also raised by other authors [1, 2, 7, 8, 15]. According to the available literature, only 30 to 75% of procedures do not need any other additional shunt revisions [8]. However, infants and neonates need at least one revision connected with their personal growth. What was surprising in the material presented in the article was that the temporary ventricular drainage had higher effectiveness in the treatment of arachnoid cysts than the shunt implantation. The explanation of the observed differences in effectiveness was that the disturbances of the CNS fluid hydrodynamics had a temporary character in cases of a head trauma, and was constant in the group of patients suffering from congenital arachnoid cysts. So, the only role of an intraventricular drainage was a transient decrease in raised intracranial pressure. After subsidence of brain edema connected with a CNS trauma, the CSF circulation was completely restored.
Otherwise there was no statistically important relation between the last chosen operative method and the number of complications in the presented material. The complications differed significantly in their character according to the type of the operative treatment (the high rate of significant worsening after cystoperitoneal shunt implantation and microsurgical cyst excision). Based on the available literature, the conservative surgical techniques are connected with high rate of operative complications [1]. Starting with shunt implantation, the frequency of complications is as follows: 10–40% of cases had shunt dysfunction; 40–60% had shunt dependency; 10% had intraoperative infections [1, 2, 4, 5, 8, 16, 17]. Neural structures could also be damaged during the catheter implantation [12, 13]. Open surgical procedures allow for more accurate inspection of anatomic structure in comparison to other methods, yet they are connected with the threat of: intracerebral or subdural bleeding (5–25% of operations), recurrence of intracranial cyst (10–30% of operations), aseptic meningitis (5–10% of operations), inability to treat hydrocephalus (30–100%), and most importantly, higher in comparison to other methods is the rate of mortality, ranging between 1–10% of operations [1, 2, 4, 6, 10, 12]. There were other factors—aside from the type of operative treatment—that influenced the clinical results in the presented material such as initially observed symptoms of arachnoid cysts and reduction of the volume of the archnoid cyst. In the group of patients treated at RIPMMH, 68.87% of all analyzed children improved regardless of the chosen type of operative procedure. Better results were obtained in the treatment of 285 children from Western Europe, where 75% of patients improved after the operation [8]. The same rate of positive outcomes was connected with the treatment of 46 patients published by Artico [1]. A high rate of improvement (82%) was signalized when patients additionally suffered from hydrocephalus [5]. Other authors also noticed a high rate of clinical improvement after operative treatment of arachnoid cysts [5, 14]. In the clinical material of the RIPMMH, clinical improvement referred to the group of patients who demonstrated either symptoms of an increased intracranial pressure or epileptic seizures as initial signs. Other authors obtained similar results [15]. In comparison, the clinical improvement is less frequent when arachnoid cysts are accompanied by endocrinological signs [14, 15]. The effects of treatment of the previously mentioned group of 285 children from Western Europe proved that there was a statistically significant relation between positive clinical results and improvement observed in the diagnostic imaging, but only 18% of arachnoid cysts disappeared completely [8, 10]. The observation was not fully confirmed on the clinical material of the RIPMMH because despite the highest degree of cyst involution located in the Sylvian fissure in children after shunt implantation and temporary drainage, the clinical results were worse in comparison to the rest of the patients. However, there was a statistically significant relation between the high rate of improvement and a significant involution of cyst size in the whole group of children with no regard to cyst location and to the type of surgical treatment. Perhaps it could be explained by more steady reduction in the size of the Sylvian fissure arachnoid cyst after the restoration of the CSF communication in comparison to the same type of cysts after an external CFS drainage. It was also observed in relation to the microsurgical treatment [7, 16]. Other authors suggest that although endoscopic techniques tend to be less effective in rapid reducing the size of the cyst, they can produce the same surgical outcome without the complications [2]. The shortening of the hospitalization in the neuroendoscopically treated group was secondary to the minimal invasiveness of neuroendoscopic methods. The same advantages were also raised by other authors [5].
Conclusions
-
1.
With respect to the rate of reoperative treatment, the necessity of changing operative method, the clinical effect, and the invasiveness of surgical procedures, the neuroendoscopic techniques were the most successful operative procedures in the treatment of arachnoid cysts in the presented group of patients.
-
2.
The effect of neuroendoscopic treatment depends on the quality of a communication between the lumen of the arachnoid cyst and the CSF cisterns.
-
3.
Neuroendoscopic techniques allow for the reduction of the hospitalization period.
References
Artico M, Crevoni L, Salavati M, Fiorenza F, Caruso R (1995) Supratentorial arachnoid cysts: clinical and therapeutic remarks on 46 cases. Acta Neurochir (Wien) 132:75–78
Choi JU, Kim DS, Huh R (1999) Endoscopic approach to arachnoid cyst. Child’s Nerv Syst 15:285–291
Greenberg MS (1994) Handbook of neurosurgery. Greenberg, Lakeland Florida
Hopf NJ, Perneczky A (1998) Endoscopic neurosurgery and endoscope-assisted microneurosurgery for the treatment of intracranial cysts. Neurosurgery 43:1330–1336
Hopf NJ, Resch KDM, Ringel K, Perneczky A (1998) Endoscopic management of intracranial arachnoid cysts. In: Hellwig D, Bauer BL (eds) Minimally invasive techniques for neurosurgery. Springer, Berlin Heidelberg New York, pp 111–119
Jackowski A, Kulshresta M, Sgouros S (1995) Laser-assisted flexible endoscopic fenestration of giant cyst of the septum pellucidum. Br J Neurosurg 9:527–531
Kang JK, Lee KS, Lee IW, Jeun SS, Son BC, Jung CK, Park YS, Lee SW (2000) Shunt-independent surgical treatment of middle cranial fossa arachnoid cysts in children. Child’s Nerv Syst 16:111–116
Oberbauer RW (1999) Intracranial and intraspinal arachnoid cysts. In: Choux M, DI Rocco C, Hockley A, Walker ML (eds) Pediatric neurosurgery. Churchill Livingstone, London, pp 137–149
Parsch CS, Krauβ J, Hofmsnn E, MeixensbergerJ, Roosen K (1997) Arachnoid cysts associated with subdural hematomas and hygromas: analysis of 16 cases, long-term follow-up, and review of the literature. Neurosurgery 40:483–490
Peter JC, Fieggen G (1999) Congenital malformations of the brain—a neurosurgical perspective at the close of the twentieth century. Child’s Nerv Syst 15:635–645
Pyrich M, Barnaś P, Plezia B (1998) Torbiele wewntrzczaszkowe leczone metod neuroendoskopow—opis dwóch przypadków. Neurol Neurochir Pol 32:425–431
Samii M, Carvalho GA, Schuhmann MU, Matthies C (1999) Arachnoid cysts of the posterior fossa. Surg Neurol 51:376–382
Sandberg DI, Souweidane MM (1999) Endoscopic-guided proximal catheter placement in treatment of posterior fossa cysts. Pediatr Neurosurgery 30:180–185
Schroeder HWS, Gaab MR (1998) Endoscopic management of intracrnial arachnoid cysts. In: Hellwig D, Bauer BL (eds) Minimally invasive techniques for neurosurgery. Springer, Berlin Heidelberg New York, pp 101–105
Shapiro KN, Swift DM (1996) Intracranial arachnoid cyst. In: Tindall GT, Cooper PR, Barrow DL (eds) The practice of neurosurgery. Williams & Wilkins, Baltimore, pp 2667–2679
Shigemori M, Okura A, Takahashi Y, Takashi T (1996) New surgical treatment of middle fossa arachnoid cyst. Surg Neurol 45:189–192
Takeuchi T, Kasahara E, Iwasaki M (1996) Cystoplastic cyst-subarachnoid shunt procedure for arachnoid cyst of the middle cranial fossa. Neurol Med Chir 36:396–399
Acknowledgement
The work was supported by the grant No 4P05E05016 of the Polish Academy of Science. The paper was presented at the ISGNE meeting in 2003.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nowosławska, E., Polis, L., Kaniewska, D. et al. Neuroendoscopic techniques in the treatment of arachnoid cysts in children and comparison with other operative methods. Childs Nerv Syst 22, 599–604 (2006). https://doi.org/10.1007/s00381-006-0068-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-006-0068-9