Abstract
Objective
Quadrigeminal cistern arachnoid cysts are rare lesions, accounting for 5% to 10% of all intracranial arachnoid cysts and 9% of all supratentorial localizations. We reviewed the patients with quadrigeminal arachnoid cyst (QAC) who were treated with neuroendoscopic intervention.
Materials and methods
Seventeen patients with QAC had been operated on between 2000 and 2007 in our institution. Four patients had undergone shunting prior to neuroendoscopic surgery. There were nine girls and seven boys with age ranging from 7 days to 17 years (mean, 40 months). All patients had hydrocephalus. A wide ventriculocystostomy (VC) and endoscopic third ventriculostomy were performed by using rigid neuroendoscopes. An aqueductal stent was also placed in two of the patients. Psychometric evaluation was administered postoperatively when possible. Follow-up of the patients ranged from 6 to 96 months (mean, 51.8 months).
Results
Of the 17 patients, 12 underwent endoscopic procedure as the primary surgery. Five patients had been previously shunted. Macrocrania and psychomotor retardation were the main symptom and sign in all infants with QAC. Older children presented with the symptoms and signs of intracranial hypertension. Of the eight patients who were 6 months old or younger, only one did not need a ventriculo-peritoneal (VP) shunt. Endoscopic procedures were successful in all patients older than 6 months of age (P = 0.005).
Conclusion
The patients presenting in their infancy had a psychomotor retardation, and all patients except for one, younger than 6 months of age, needed a VP shunt. Neuroendoscopic procedure is effective particularly in the patients with QAC older than 6 months of age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arachnoid cysts constitute 1% of all intracranial mass lesions not resulting from trauma. Arachnoid cyst can arise in any part of the central nervous system where arachnoid is found.
Quadrigeminal cistern arachnoid cysts are rare lesions, accounting for 5% to 10% of all intracranial arachnoid cysts [2, 13] and 9% of all supratentorial localizations [2]. We report on 17 patients with quadrigeminal arachnoid cyst (QAC) who were treated with neuroendoscopic intervention.
Materials and method
Seventeen patients with QAC had been operated on between 2000 and 2007 in our institution. Five patients had undergone shunting prior to neuroendoscopic surgery. These five patients presented with symptoms and signs of shunt malfunction. There were nine girls and eight boys, with age ranging from 7 days to 17 years (mean 40 months). All patients had hydrocephalus.
Diagnostic workup
In all patients, magnetic resonance imaging (MRI) scans and/or computed tomographic (CT) scans were performed. X-ray films of the shunt system and abdominal ultrasound were also performed in the patients presenting with shunt malfunction. CT scan was obtained following surgery on the same day in all patients. MRI scans containing particularly flow studies were performed in the first postoperative week.
Neuroendoscopic technique
All surgical procedures were performed under general anesthesia by the same neurosurgeon. Patient is positioned in neutral supine position and head is elevated minimally. A skin incision and a burr hole 1 cm in front of the coronal suture in the midpupillary line are done. In children under the age of 1 year, an incision for the entry point of the endoscope was made at the lateral margin of the open anterior fontanel. Rigid endoscope sheath or peel-away sheath is used to cannulate the lateral ventricle. Then, zero-degree straightforward rigid neuroendoscope (Karl Storz, Tutlingen, Germany and Channel Neuroendoscope, Medtronic, Minneapolis, MN, USA) is inserted into the endoscope sheath. Anatomic landmarks are identified including the choroid plexus, thalamostriate, and septal veins, and the endoscope was advanced to the foramen of Monro. QAC was bulging into the lateral ventricle in all cases. A wide ventriculocystostomy (VC) is performed by using bipolar coagulation and sharp dissection. Then, the endoscope is advanced into the third ventricle, and endoscopic third ventriculostomy (ETV) was performed when feasible, since a secondary aqueductal stenosis due to the compression of QAC was detected in all patients. An aqueductal stent was also placed in two of the patients. At the end of the procedure, the burr hole is plugged with a piece of gel foam, and the skin incision is sutured in layers.
Psychological evaluation
Information obtained from two sources, i.e., the Ankara Developmental Screening Inventory (ADSI) for children 6 years old or younger [15], and Wechsler Intelligence Scale for Children-Revised for children older then 6 years old [20].
The ADSI is a 154-item scale widely used in Turkey for the assessment and evaluation of social, cognitive, and communicative levels of children between 0 and 6 years old. Each item has three choices (yes, no, and do not know). The inter-rater reliability of the instrument for all age groups is high (Cronbach’s α = 0.99 for 0–12 months; 0.98 for 13–44 months; 0.88 for 45–72 months) [15]. The ADSI includes four subscales. The total development score reflects the general development level of the child, and it is obtained from the total of the four subscales:
-
1.
The language-cognitive subscale contains 65 items related to the child’s understanding and use of language, simple problem solving abilities, and notions of numbers and time.
-
2.
The fine motor subscale contains 26 items related to visual-motor skills ranging from simple eye–hand coordination to complex fine motor behaviors.
-
3.
The gross motor subscale contains 24 items related to movement, strength, balance and coordination.
-
4.
The social interaction skills and self-care abilities subscale contains 39 items related to eating, drinking, dressing, self-care, toilet training, independence, social interaction and initiative taking.
Outcome
When the symptoms and signs of intracranial pressure and hydrocephalus improve and when the patient does not need a ventricular shunt, the endoscopic procedure was considered as successful. All patients were followed up with postoperative MRI in 3 and 6 months after surgery and annually thereafter. Follow-up of the patients ranged from 6 to 96 months (mean, 51.8 months). Fisher’s exact test was used in statistical analysis.
Results
Clinical presentation
Of the 17 patients, 12 underwent endoscopic procedure as the primary surgery. Macrocrania and psychomotor retardation were the main symptom and sign in all infants with QAC. Older children presented with the symptoms and signs of intracranial hypertension such as headache and vomiting. The five patients who had undergone ventriculo-peritoneal (VP) shunting presented with shunt malfunction at the time of endoscopic surgery (Table 1). All patients diagnosed in their infancy had a psychomotor retardation in varying degrees.
Endoscopic treatment
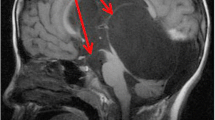
QACs were bulging into the lateral ventricles in all patients. Therefore, VC was performed in the right lateral ventricles, the endoscope was advanced into the third ventricle, and ETV was done in 13 patients (Fig. 1). Two patients also underwent aqueductal stenting in addition to these procedures (Fig. 2). In three patients, ETV was not possible, and only VC could be performed. In one of the patients, QAC recurred and endoscopic VC was repeated 3 years after the first procedure. A temporal ependymal cyst developed 6 months following the first procedure (Fig. 3).
a Axial and b sagittal MRI scans of a week-old boy (Patient 7) showing a QAC, c postoperative axial and d sagittal MRI scans showing a marked reduction in the volume of QAC and resolution of hydrocephalus, e note the ependymal cyst in the right temporal horn on the coronal MRI scan 6 months later and f coronal MRI scan following the endoscopic cyst fenestration
Radiology
MRI showed the dilated third and lateral ventricles in addition to QAC in all patients. In some patients, QAC was also extending the retrocerebellar region. Holoprosencephaly, porencephaly, Chiari type II malformation, encephalocele, and temporal ependymal cyst were the associated brain lesions in two, two, two, one, and one patient, respectively. QACs had either decreased or disappeared on the follow-up MRI scans except for one. A second VC was done in that patient 3 years later. Ventricular dilatation had increased in seven patients who underwent a VP shunting.
Complications
There was no surgical mortality. Postoperative subdural fluid collection developed in three patients. A subduro-peritoneal shunt was implanted in two, and it was asymptomatic in one of them (Fig. 4). Cerebrospinal fluid fistula (CSF) leak and then meningitis developed in one patient in which endoscopic procedure failed and a VP shunt was subsequently needed.
a Preoperative sagittal MRI scan showing hydrocephalus and QAC (Patient 3), b note reduction in the volume of QAC on the postoperative sagittal MRI, c CT scan showing bilateral subdural fluid collection and holoprosencephaly, d CT scan following subduro-peritoneal shunt implantation, e sagittal MRI showing the disappearance of QAC and marked hydrocephalus, and e CT after ventriculo-peritoneal shunt
Psychological evaluation
The raw values from three subjects were assessed with the standardization version and computed with the Turkish Wechsler Intelligence Scale for Children Revised (WISC-R) norms. Two individuals showed a significantly lower performance intelligent quotient (PIQ) than verbal intelligent quotient (VIQ). Only one subject’s total score was under the normal IQ limits, but her subtests scores were heterogeneous. This subject also has a significant discrepancy between VIQ and PIQ scores like the other two. Comparing VIQ scores with the lower test scores for PIQ shows us that these two subjects have more spatial capacity problems (visual attention and visual memory problems then language related problems) and has some difficulty short-term auditory sequential memory problems on performance scores while having relatively normal verbal capacity (Table 2).
Only one of ten patients’ total developmental scores were within the normal range. Nine subjects had a developmental delay in almost all subscales of inventory. Especially, they have more problems in gross motor domain (Fig. 5).
Outcome
One of the patients in whom endoscopic procedure had not been successful died of shunt infection 7 months later. Endoscopic intervention was successful in ten of 17 patients with QAC. Of right patients who were 6 months old or younger, only one did not need a VP shunt. Endoscopic procedures were successful an all patients older than 6 months of age. This difference was found statistically significant (P = 0.005).
Discussion
QACs comprised 10% of 208 arachnoid cysts, as analyzed by Reganchary and Watanabe [13]. Only four of those were over 20 years old. In the review of Hayashi et al. [6], there were 15 male and ten female patients, with age ranging from 3 weeks to 37 years. Of the 25 patients with QAC, 22 (88%) were less than 15 years old. In this series, the youngest and the oldest patient were 7 days and 17 years old, respectively.
QACs usually lead to symptoms and signs of increased intracranial pressure and non-communicating hydrocephalus [4, 6, 8, 10, 17]. QACs are benign, tumor-like lesions, which can present with symptoms and signs associated with either tectal plate compression or secondary to obstructive hydrocephalus. Parinaud syndrome is an unusual primary presentation [5]. Infants with QAC usually present with macrocrania and psychomotor retardation [4, 6, 17]. One of our patients presented with seizure. Vertigo, tinnitus, trochlear nerve paresis, and apneic spells have also been reported [5, 6, 10–12, 14, 18]. There is no unique symptom or sign for QACs.
The traditional surgical treatments of QACs include craniotomy and cyst excision or fenestration, ventricular shunt, shunt of the cyst, and combined procedures [2, 6, 16, 19, 21]. In 1996, Ruge et al. [14] used a neuroendoscopic approach to QAC in two patients via a suboccipital supracerebellar approach. Hopf and Perneczky [7] treated two cases of QAC with endoscope-assisted microneurosurgery via a suboccipital craniotomy. Tamburrini et al. [17] reported that a significant percentage of the patients with QAC presented indeed with associated obstructive triventricular dilatation and signs of increased intracranial pressure, and six of 11 patients (54.5%) in their series presented with triventricular hydrocephalus, which was severe in five. Their policy was to combine ETV to VC; the last patient presented with a moderate asymptomatic ventricular dilatation and was successfully managed with VC alone [3, 16, 21]. Hopf and Perneczky [7] reported some cases of failure of endoscopically assisted fenestration without ventriculostomy, in which an ETV was later added to obtain improvement. We performed ETV in all cases when feasible. However almost all patients younger than 6 months old who had undergone both cyst fenestration and ETV needed a VP shunt. This was probably due to the failure in CSF resorption. Choi et al. [1] also reported a failure in one among the nine reported cases treated by cyst fenestration and ETV.
We used rigid endoscopes in all patients. Rigid [1, 14], flexible endoscopes [4, 5], or both [8, 9] have been preferred by the different authors. A frontal burr hole is usually used to access the lateral ventricle. We did perform VC through the lateral ventricle. VC has been done via either the third ventricle [5, 8, 9] or the lateral ventricle [1, 9, 17]. Gangemi et al. [4] used the both routes. In the review of Gangemi et al. [4], the overall rate of patients cured or improved was rather similar in the two groups (87.5% in the endoscopic group vs. 85% in the surgical group). The endoscopic group had a significantly higher complete cure rate (62s.5%) than the surgical group (35%). All QACs in this series either decreased in size or disappeared after endoscopic surgery. However, hydrocephalus persisted almost in all patients younger than 6 months of age, and they needed a VP shunt. It is possible that subarachnoid spaces were not patent yet or the CSF resorption was diminished in those patients.
No complication regarding the endoscopic procedure in patients with QAC has been reported [1, 4, 5, 7, 14, 17]. Subdural fluid collection and CSF fistula were seen in our patients.
To our knowledge, there has been no study containing psychometric evaluation in patients with QAC. Of the ten patients with QAC presenting in their infancy, nine had a developmental delay. Of the three patients who had underwent WISC-R testing, only one had a normal IQ. Eight of the 17 patients also had associated other central nervous system lesions such as holoprosencephaly, porencephaly, and Chiari Type II malformation. We could not find a statistically significant association between these lesions and developmental delay.
In conclusion, QACs may be associated with the other central nervous system malformations such as holoprosencephaly, Chiari type II malformation, and encephalocele. Those patients with QAC presenting in infancy usually have a psychomotor retardation. Although endoscopic VC and ETV are minimally invasive and effective in the management of QACs, hydrocephalus usually persists in patients younger than 6 months of age.
References
Choi JU, Kim DS, Huh R (1999) Endoscopic approach to arachnoid cyst. Childs Nerv Syst 15:285–291
Di Rocco C, Caldarelli M (1993) Supratentorial interhemispheric and pineal region cysts. In: Raimondi AG, Choux M, Di Rocco C (eds) Intracranial cyst lesions. Springer, New York, pp 153–168
Fujita K, Sato H, Tamaki N, Matsumoto S (1984) Arachnoid cyst of the quadrigeminal cistern. No Shinkei Geka 12:1315–1322
Gangemi M, Maiuri F, Colella G, Magro F (2005) Endoscopic treatment of quadrigeminal cistern arachnoid cysts. Minim Invasive Neurosurg 48:289–292
Hayashi N, Endo S, Tsukamoto E, Hohnoki S, Masuoka T, Takaku A (1999) Endoscopic ventriculocystocisternostomy of a quadrigeminal cistern arachnoid cyst. Case report. J Neurosurg 90:1125–1128
Hayashi T, Kuratomi A, Kuramoto S (1980) Arachnoid cyst of the quadrigeminal cistern. Surg Neurol 14:267–273
Hopf NJ, Perneczky A (1988) Endoscopic neurosurgery and endoscope-assisted microneurosurgery for the treatment of intracranial cysts. Neurosurgery 43:1330–1337
Inamasu J, Ohira T, Nakamura Y, Saito R, Kuroshima Y, Mayanagi K, Ohba S, Ichikizaki K (2003) Endoscopic ventriculo-cystomy for non-communicating hydrocephalus secondary to quadrigeminal cistern arachnoid cyst. Acta Neurol Scand 107:67–71
Karabatsou K, Hayhurst C, Buxton N, O’Brien DF, Mallucci CL (2007) Endoscopic management of arachnoid cysts: an advancing technique. J Neurosurg 106(6 Suppl):455–462
Kumar K, Peng EWK, Fitzpatrick MO, Whittle IR (2006) Tectal plate cyst in adults. Acta Neurochir (Wien) 148:805–808
Kurita H, Nitta Y, Nakamura M, Shiokawa Y (2004) Defecation-induced vertigo. Arch Neurol 61:1137–1138
Ohtsuka K, Hashimoto M, Nakamura Y (1998) Bilateral trochlear nerve palsy with arachnoid cyst of the quadrigeminal cistern. Am J Ophthalmol 125:268–270
Reganchary SS, Watanabe I (1981) Ultrastructure and pathogenesis of intracranial arachnoid cysts. J Neuropathol Exp Neurol 40:61–83
Ruge JR, Johnson R, Bauer J (1996) Burr hole neuroendoscopic fenestration of quadrigeminal cistern arachnoid cyst: technical case report. Neurosurgery 38:830–837
Savasir I, Sezgin N, Erol N (1998) Ankara developmental screening inventory manual. Psikologlar Derneği, Ankara
Spaziante R, Cirillo S, Constans JP, de Divitiis E, Donzelli R, Stella L (1986) Arachnoid cyst of the quadrigeminal cistern. Neurochirurgia (Stuttg) 29:117–120
Tamburrini G, D’Angelo L, Paternoster G, Massimi L, Caldarelli M, Di Rocco C (2007) Endoscopic management of intra and paraventricular CSF cysts. Childs Nerv Syst 23:645–651
Topsakal C, Kaplan M, Erol F, Çetin H, Özercan I (2002) Unusual arachnoid cyst of the quadrigeminal cistern in an adult presenting with apneic spells and normal pressure hydrocephalus. Neurol Med Chir (Tokyo) 42:44–50
Wakisaka S, Yoneda K, Kitano I, Kinoshita K, Matsuoka S (1986) Arachnoid cyst in the quadrigeminal cistern. Surg Neurol 26:52–58
Wechsler D (1974) Manual for the Wechsler intelligence scale for children—revised. Psychological Corporation, New York
Wong CW, Lee ST, Lui TN, Wu T, Wu LL (1996) Fluctuating hemiparesis caused by a quadrigeminal arachnoid cyst: case report. Surg Neurol 45:193–195
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erşahin, Y., Kesikçi, H. Endoscopic management of quadrigeminal arachnoid cysts. Childs Nerv Syst 25, 569–576 (2009). https://doi.org/10.1007/s00381-008-0778-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0778-2