Abstract
Objective
The aim of this study was to investigate the endoscopic treatment of cerebral hemisphere convexity arachnoid cyst.
Methods
Eight cases of hemisphere convexity arachnoid cyst treated with cyst–ventricular or cisternal endoscopic approach in September 2007 to March 2011 were retrospectively recruited. The clinical symptoms, radiological findings, surgical indications, surgical approach, complications, and follow-up studies were analyzed.
Results
All patients showed convexity arachnoid cysts adjacent to the ventricles or cisternal. After treatment, all patients showed decrease in size of the cysts (100 %), with preoperative symptoms disappeared in six patients and improved in two cases. In one case, postoperative subdural effusion was found without symptoms reported.
Conclusion
Endoscopic surgery is ideal for treatment of arachnoid cysts adjacent to the ventricles or cisternal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial arachnoid cyst is common in middle cranial fossa, posterior fossa, cerebral hemisphere convex, quadrigeminal cistern, as well as sellar/suprasellar regions. Among these, the cerebral hemisphere convexity arachnoid cyst (hemisphere arachnoid cyst) contributes to 5 % of the total cases [2, 3, 12].
Four types of surgical approaches are suitable for hemisphere arachnoid cysts: cyst–peritoneal shunt, craniotomy–microsurgery, stereotactic cyst–ventricular shunt, and endoscopic surgery [1, 3, 4, 9, 10, 13, 14, 16]. The cyst–peritoneal shunt and craniotomy–microsurgery were widely adopted in clinical practices of past decades, while in recent years, the endoscopic surgery gained increasing attention due to the significant progresses in this area [1, 5–7, 9, 10, 13, 16]. Due to the rare incidence of hemisphere convexity arachnoid cyst, the reported cases in the literature, especially those treated with endoscopic approach, were very little, only 20 cases to our knowledge [1, 9, 10, 13, 16]. Here, we reported eight cases of cerebral hemisphere convexity arachnoid cyst patients that were treated with endoscopic surgery in our department from September 2007 to March 2011.
Materials and methods
General information
Eight patients (five males and three females, aged 4–60 years old, with disease duration of 1 month to 5 years) were recruited in the present study. All patients showed cerebral convexity arachnoid cyst near the brain ventricles or cisternal. The main symptoms and signs include the following: two cases of head pain associated with limb convulsive seizures, one case of limbs convulsive seizures, one cases of headache with limb hemiparesis, one case of dizziness and headache, one case with eyes squint and nystagmus, one case of headache and body numbness on the right side, and one case of headache with the walk instability.
Radiological evidences
CT and MRI examination revealed the hemisphere convex cyst separated from the subarachnoid area, containing cyst fluids with similar signal to the cerebrospinal fluid. The distribution of cysts are the following: one case left occipital, adjacent to the occipital horn of the left ventricle and triangle area; one case right frontal, adjacent to the frontal horn of the right ventricle; one case left frontal, adjacent to the frontal horn of the left ventricle; one case right temporal–parietal, adjacent to the occipital horn of the right ventricle; one case right temporal–occipital, adjacent to the occipital horn of the right ventricle; one case left frontoparietal, adjacent to the longitudinal pool; one case left parietal–occipital with large cyst, adjacent to the occipital horn of the left ventricle, resulting in the compression of the occipital horn and expansion of the bilateral ventricles; and one case of bilateral parietal–occipital arachnoid cyst, adjacent to the quadrigeminal cistern and the occipital cistern.
Endoscopic surgery treatment
The endoscopic surgery followed the steps below:
-
1.
The fistula location for cyst–ventricle or cyst–cistern approach was determined from MRI, which allowed for the scalp incision and body position during surgery.
-
2.
After opening of the bone, curved incision of the dura was chosen for patients aged less than 8 years old, and cross incision for patients aged older. The complete hemostasis is necessary to avoid the blood flow into the cyst cavity.
-
3.
Zero degree working endoscope with working channel and flush channel was used. Endoscopic equipment includes scissor bipolar coagulation, microscissors, and grasping forceps. The cyst–ventricle or cyst–cistern or cyst–subarachnoid fistula was made according to the position of the cyst.
-
4.
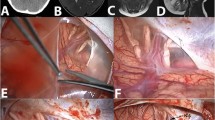
Cyst–ventricle fistula is suitable for hemisphere cysts close to ventricles but not cistern [9] (Fig. 1) and is compatible with cyst–subarachnoid fistula if feasible. The cyst walls should be removed as much as possible. The detailed steps include the following: cyst–subarachnoid fistula was made first with removal of cyst walls; electrically coagulated the cyst wall and use blunt approach to communicate the ventricle and the cyst. The successful cyst–ventricle fistula allowed the visualization of the choroid plexus and ventricle wall (Fig. 1). Then, the fistula was expanded to more than 0.5 cm. No stent is required after the successful fistula.
-
5.
Cyst–cistern fistula is suitable for hemisphere cysts adjacent to the cistern. The approach is similar and the successful cyst–cistern fistula allowed the visualization of internal structures of the cistern. The cyst walls were removed to expand the fistula opening.
-
6.
For hydrocephalus occurring concurrent with the cyst, the third ventricle septum fistula or colostomy were made after cyst–ventricle or cyst–cistern fistula, to recover the circulation of the cerebrospinal fluid.
-
7.
For patients that are unsuitable for both cyst–ventricle fistula and cyst–cistern fistula, dual approach for a wide range of communication between cysts and the surrounding subarachnoid space was recommended [10].
-
8.
The cyst was rinsed and the endoscope was removed after confirmation of hemostasis. The skin was closed.
a–c Preoperative MRI prompted the left occipital arachnoid cyst, lateral triangle with the adjacent wall. d, e Cyst seen after subarachnoid fistula tentorial and transverse sinus. f Coagulation cyst underwent cyst wall–lateral triangle fistula. g Observation of the left ventricle through the stoma wall and choroid plexus. h–j MRI after 1 month prompted cysts smaller in size. k, l After 2 months of CT prompted further reduced cyst
Follow-up
All patients received head CT examination shortly after the surgery. Head CT or MRI examinations were performed 3 and 9 months after surgery. Then head CT was done once every year. The follow-up studies lasted for 6–48 months with an average of 21 months.
Results
Clinical symptoms
The clinical symptoms were improved in all eight patients. The headache, dizziness, and paralysis disappeared; strabismus improved with nystagmus reduction; and the seizures disappeared with oral antiepileptic drugs administration. No complications were found in all eight cases.
Follow-up
The follow-up studies revealed reduction of cysts in all eight patients, and the reduction of ventricle sizes in those cases with hydrocephalus. The case with left parietal–occipital huge cyst showed subdural effusion after surgery; however, all pre-operation symptoms disappeared and no new symptoms occurred.
Discussion
Selection of the endoscopic treatment
Surgical treatment of intracranial arachnoid cysts should be based on the patient’s age, cyst location, size, and clinical symptoms. It is important to know whether the cyst lead to pressure on the brain tissue, nerves, and blood vessels, which could contribute to the clinical symptoms observed. Further, whether the size of cyst is increasing with progressing exacerbation of clinical symptoms was examined. It was believed that most intracranial arachnoid cysts would maintain the size and morphology after formation, and few cysts could increase, even resulting in the rupture and subdural hematoma; in rare cases, the cysts disappeared (all the cases reported in the literature showed disappearance before 20 years old) [8]. Some cases showed gradual reduction of the cyst size, while some other cases just vanished, possibly because of the formation of communication between cysts and ventricle, for example.
Surgical treatment was recommended for intracranial cysts associated with clear clinical symptoms. While in some cases with the huge cyst formation lacking clear symptoms, it is still controversial in selecting the treatment approach. The rationales supporting the surgical treatments were: (1) minor head trauma might cause rupture of these large cysts and acute intracranial hypertension, with serious complications [11, 17]; (2) the pressure caused by cysts could affect the cerebral blood flow in infants and pediatric patients, leading to abnormal development and relevant disorders such as epilepsy. On the other hand, the rationales not supporting the surgical treatment for asymptomatic arachnoid cysts without size progression were the following: (1) in patients with cyst disappearance, the head trauma still causes subdural hematoma [15]; (2) there is no clear evidence showing that the cysts would affect the brain development; (3) in some cases the cysts disappear following minor trauma, forced breathing, breath, pinch nose and blow, severe coughing, crying out loud, vigorous exercise, purulent meningitis, or lacking apparent induction. Many cases were children with large cysts [8].
The authors therefore recommend surgical treatment for convexity arachnoid cysts in the following conditions: (1) there is a clear increase in intracranial pressure, with headache, vomiting, papilledema, opening of anterior fontanelle, or increased head circumference; (2) concurrent intracystic hemorrhage, subdural bleeding, or hydrocephalus; (3) signs of focal neurological deficits such as hemiplegia, aphasia, etc.; (4) confirmed cyst-induced epilepsy; (5) progressing increase in the cyst size; (6) the expansion of cyst caused skull uplift, with compression of surrounding brain tissues; and (7) if the cyst compression caused a low metabolic state in surrounding brain tissue, the surgery is recommended. If the epilepsy was observed but no correlation was proved to be linked with the cyst growth, the surgery is not recommended.
Surgical options
The aim of the surgery is to remove the compression on the brain tissues and prevent recurrence. The available surgical approaches included stereotactic cyst puncture–ventricular shunt, microsurgery, endoscopic surgery, and cysts–peritoneal shunt surgery [1, 3, 4, 9, 10, 13, 14, 16]. The endoscopic surgery showed the following advantages [1, 9, 10, 13, 16]: (1) less injury with accurate manipulation when compared to microsurgery; (2) avoid blind puncture injury and recurrence when compared to the stereotactic method; (3) avoid foreign implant when compared to cysts–peritoneal shunt surgery, as well as potential infection and blockage of the stent; and (4) the surgery is fast and with few complications, as well as shorter hospital stay. In our cases, all patents showed improvement and none with complications.
The endoscopic surgical methods should rely on the detailed information of each individual. The location, size, adjacent nerves, and blood vessels in relation to the ventricle and cistern should be understood by radiological approach prior to the surgery, in order to determine the surgical incision, cyst fistula site, etc. The detailed approach was described in above paragraphs in the “Materials and methods” section.
In summary, we proved that endoscopic surgery is ideal for treatment of arachnoid cysts adjacent to the ventricles or cisternal. The preoperative understanding of the cyst information is critical for determining the surgical path and details during the surgery.
References
Chernov MF, Kamikawa S, Yamane F, Hori T (2004) Double-endoscopic approach for management of convexity arachnoid cyst: case report. Surg Neurol 61:483–486. doi:10.1016/S0090-3019(03)00574-3, discussion 486–487
Choi JU, Kim DS, Huh R (1999) Endoscopic approach to arachnoid cyst. Childs Nerv Syst 15:285–291
Ciricillo SF, Cogen PH, Harsh GR, Edwards MS (1991) Intracranial arachnoid cysts in children. A comparison of the effects of fenestration and shunting. J Neurosurg 74:230–235. doi:10.3171/jns.1991.74.2.0230
D'Angelo V, Gorgoglione L, Catapano G (1999) Treatment of symptomatic intracranial arachnoid cysts by stereotactic cyst–ventricular shunting. Stereotact Funct Neurosurg 72:62–69, 29672
Gui SB, Wang XS, Zong XY, Li CZ, Li B, Zhang YZ (2011) Assessment of endoscopic treatment for middle cranial fossa arachnoid cysts. Childs Nerv Syst 27:1121–1128. doi:10.1007/s00381-011-1399-8
Gui SB, Wang XS, Zong XY, Zhang YZ, Li CZ (2011b) Suprasellar cysts: clinical presentation, surgical indications, and optimal surgical treatment. BMC Neurol 11:52. doi:10.1186/1471-2377-11-52
Karabatsou K, Hayhurst C, Buxton N, O'Brien DF, Mallucci CL (2007) Endoscopic management of arachnoid cysts: an advancing technique. J Neurosurg 106:455–462. doi:10.3171/ped.2007.106.6.455
Moon KS, Lee JK, Kim JH, Kim SH (2007) Spontaneous disappearance of a suprasellar arachnoid cyst: case report and review of the literature. Childs Nerv Syst 23:99–104. doi:10.1007/s00381-006-0161-0
Nowoslawska E, Polis L, Kaniewska D et al (2006) Neuroendoscopic techniques in the treatment of arachnoid cysts in children and comparison with other operative methods. Childs Nerv Syst 22:599–604. doi:10.1007/s00381-006-0068-9
Oertel JM, Baldauf J, Schroeder HW, Gaab MR (2009) Endoscopic cystoventriculostomy for treatment of paraxial arachnoid cysts. J Neurosurg 110:792–799. doi:10.3171/2008.7.JNS0841
Parsch CS, Krauss J, Hofmann E, Meixensberger J, Roosen K (1997) Arachnoid cysts associated with subdural hematomas and hygromas: analysis of 16 cases, long-term follow-up, and review of the literature. Neurosurgery 40:483–490
Rengachary SS, Watanabe I (1981) Ultrastructure and pathogenesis of intracranial arachnoid cysts. J Neuropathol Exp Neurol 40:61–83
Shim KW, Lee YH, Park EK, Park YS, Choi JU, Kim DS (2009) Treatment option for arachnoid cysts. Childs Nerv Syst 25:1459–1466. doi:10.1007/s00381-009-0930-7
Sommer IE, Smit LM (1997) Congenital supratentorial arachnoidal and giant cysts in children: a clinical study with arguments for a conservative approach. Childs Nerv Syst 13:8–12
Spacca B, Kandasamy J, Mallucci CL, Genitori L (2010) Endoscopic treatment of middle fossa arachnoid cysts: a series of 40 patients treated endoscopically in two centres. Childs Nerv Syst 26:163–172. doi:10.1007/s00381-009-0952-1
Tamburrini G, D'Angelo L, Paternoster G, Massimi L, Caldarelli M, Di Rocco C (2007) Endoscopic management of intra and paraventricular CSF cysts. Childs Nerv Syst 23:645–651. doi:10.1007/s00381-007-0327-4
Wester K, Helland CA (2008) How often do chronic extra-cerebral haematomas occur in patients with intracranial arachnoid cysts? J Neurol Neurosurg Psychiatry 79:72–75. doi:10.1136/jnnp.2007.117358
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gui, S., Zong, X., Li, C. et al. Endoscopic treatment of convexity arachnoid cysts. Childs Nerv Syst 29, 505–508 (2013). https://doi.org/10.1007/s00381-012-1957-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1957-8