Abstract
Purpose
To test whether a novel guide template we designed can facilitate accurate insertion of antegrade lag screws in the fixation of acetabular posterior column fractures.
Methods
We created virtual three-dimensional reconstruction models of the pelvis from CT scan data obtained from 96 adult patients without any bony problems. A virtual cylindrical implant was placed along the longitudinal axis of the acetabular posterior column passing through the ischial tuberosity. The diameter of cylindrical implant was augmented to 6.5 mm, and the direction was adjusted until the optimal screw path was found using the reverse engineering technique. The orifice of this cylinder from the iliac fossa was determined as the entry point for the antegrade lag screw. The anatomical parameters of the screw entry path were measured and saved in .stl format. The guide template was designed according to the acetabular morphology and the measured anatomical parameters before it was put into manufacture of a solid template with the rapid prototyping technique. The feasibility and accuracy of the guide template were tested in cadaveric pelvises. Finally, the guide template was used in real surgery for five patients. Furthermore, the time required for surgery was recorded.
Results
Under the guide of this navigation template, antegrade lag screws were successfully placed in the posterior column of the acetabulum in the cadaveric test. And five lag screws were successfully placed in five patients. The mean time of antegrade lag screw insertion required 5.8 (3–10) min.
Conclusions
Antegrade lag screws can be more accurately put into the posterior column of the acetabulum with the help of this navigation template.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fixation of acetabular fractures is always a great clinical challenge for orthopaedic surgeons [1, 2], because acetabular fractures, usually high-energy injuries, occur deep in a complicated anatomical structure, often leading to numerous complications. Open reduction and internal fixation (ORIF) is the “gold standard” treatment for the acetabulum fractures that involve the weight-bearing regions, resulting in a shift of over 3 mm or intra-articular fractured segments [3–5]. Giannoudis et al. [6] reported that the fractures involving the posterior column, such as transverse fracture, anterior column with posterior hemitransverse fracture, T-type fracture, and fracture of both columns, accounted for 44 % of all the acetabulum fractures. Most of them have to receive ORIF with reconstruction plates through combined anterior and posterior approaches [7, 8]. However, surgery with double incisions and wide fracture exposure may often lead to complications like massive bleeding, neurovascular injury, postoperative infection and heterotopic ossification [1, 2, 9]. Compared with the reconstruction plates, lag screw fixation for acetabulum fractures needs less surgical exposure and is less traumatic. Biomechanical tests showed that lag screw fixation for a transverse or T-shaped fracture was at least as effective as plate fixation [10, 11]. It has been recommended that the lag screw technique should be used in the complex acetabular fractures affecting the posterior column, such as transverse and T-shaped ones [12–14]. Therefore, for patients with an acetabular fracture affecting both columns, whose posterior column fracture is easy to reset, some surgeons [12–14], including us, prefer only the anterior approach, like an ilioinguinal approach [15], as their first choice, to reduce the displaced anterior and posterior column factures simultaneously, followed by plate fixation of the anterior column and lag screw fixation of the posterior column to minimize invasion and complications caused by an additional posterior approach.
However, screw placement in the posterior column of the acetabulum has a narrow margin of safety. Anatomical morphology of the acetabulum is complicated, with rich vessels and nerves in the periacetabular area. Body position of the patient is changeable during surgery. Soft tissue may also interfere with the procedure. All these make it difficult to ensure a safe placement of a lag screw at an accurate angle and depth [16–18]. Therefore, placement of lag screws, no matter whether antegrade or retrograde, into the posterior column of the acetabulum can cause problems. Although three-dimensional (3D) fluoroscopy guidance has improved the accuracy of inserting lag screws into the posterior column, and pre-operative locating and intra-operative positioning as well [19, 20], not many hospitals can afford the expensive computational guidance system. All these problems limit extensive application of lag screw placement into the posterior column of the acetabulum. Therefore, we have been exploring a solution which can address the difficulty and risk in lag screw placement independently of computational navigating system. In this study, we designed a novel guide template which could help accurate screw placement in the posterior column and manufactured it using a rapid prototyping technique. Finally, we tested the safety and accuracy of screw insertion aided by the synthetic template, first in human cadavers and then in patients. The purpose of the present study was to evaluate its feasibility and clinical value.
Materials and methods
Design and manufacture of the guide template
Data collection and 3D reconstruction models of the pelvis
An analysis of 96 (54 men and 42 women) consecutive CT scans on polytrauma adult patients who were admitted to a level-I trauma centre over a 12-month period, was performed. Scans with evidence of bony and/or ligamentous pelvic ring or acetabular injury or other pathology (primary or secondary malignancy, metabolic bone disease, severe degenerative changes, previous trauma) were excluded. All CT scans were performed using a 64-slice Siemens SOMATOM Sensation (GE Medical systems/light speed 16), from the Diagnostic Imaging Centre of our hospital between April 2006 and December 2012. The virtual 3D model of the pelvis was created from the CT data (DICOM format), using image-processing software (Mimics, Materialise Interactive Medical Image Control System; Materialise, Leuven, Belgian).
Measurement of parameters regarding placement of antegrade lag screws in the 3D reconstruction models of the pelvis
Since the pelvis can be considered as a structure of bilateral symmetry, we only measured the parameters on the right side of the pelvis.
The 3D models of the pelvis were dealt with translucence. A virtual cylindrical implant was placed along the longitudinal axis of the right posterior column of the acetabulum passing through the ischial tuberosity. According to the report by Mu et al. [21], we took 6.5 mm as the optimal diameter of the lag screw. In order to determine the optimal implant path and accurate position, the diameter of the cylindrical implant was gradually augmented to 6.5 mm while the direction was adjusted and monitored to make sure that the virtual cylinder did not penetrate into the articular cavity or came out of the cortex of the posterior column. In addition, two-dimensional images of the pelvis in transverse, coronal and sagittal planes were observed to confirm that the virtual cylindrical implant was intraosseous.
As illustrated in Fig. 1, the orifice of this cylinder from the iliac fossa (point O) was determined as the entry point for the lag screw. The other end of the shortest distance between the entry point (point O) and the arcuate edge was determined as point D. Point G was the frontmost edge of the sacroiliac joint, and point P was the iliopubic eminence. The lengths of lines OD and DG, the angle between the cylinder and the coronal plane (angle α), the angle between the quadrilateral surface and the iliac wing plane (angle β), and the radian of the arcuate edge between point P and point G were measured with UG 6.0 software (Unigraphics Solutions, Plano, TX, USA).
The orifice of this cylinder from the iliac fossa (O) was determined as the entry point for the antegrade lag screw. Point D was found in the arcuate edge, making the distance of OD the shortest between the entry point and the arcuate edge. Point G was the frontmost edge of the sacroiliac joint, point P was the iliopubic eminence, and points D and G were connected
Design and manufacture of the guide template
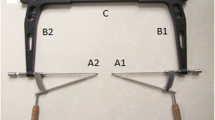
The statistical analyses showed no significant differences between males and females regarding all the above parameters but the OD value (Table 1). However, considering there is a safe area wide enough for screw insertion in the posterior column, we neglected the difference in the OD value between males and females. Therefore, mean parameters of OD and DG lengths, angle α, angle β, and the radian of the PG arcuate edge were used for the design of an adult universal guide template. The design of the optimal path of antegrade lag screw was conducted using UG 6.0 software in the 3D reconstruction models of the right hemipelvis. The inner side of the template, which was also the side in touch with the bone surface, was designed according to the extracted anatomical data of the quadrilateral surface and the iliac fossa. We designed one additional entry point on either side, 8.0 mm away from the optimal screw entry point. The two additional side entry points were designed to provide two more alternatives that can be chosen for accurate screw insertion or for need of insertion of one more screw. In addition, placement of three guiding needles (Kirschner wire) before insertion of the antegrade lag screw can help stabilize the guide temple closely onto the two bone surfaces. Consequently, digital design of a 3D guide template universal for Chinese adults with three orientation entry points was completed for the placement of lag screws into the posterior column of the acetabulum. The three orientation entry points at the guide template labeled as 1, 2 and 3 (Fig. 2) from the anterior to the posterior on the AP view indicated the first, second and third screw entry points on the acetabulum respectively. The digital template was then imported into the 3D reconstruction model of the right hemipelvis, which had been imported in .stl format into UG software. In the 3D reconstruction model, the template which was made attaching closely the quadrilateral surface was rotated in all directions to observe the fitness of the three screw paths to the posterior column of the acetabulum. After fine fitness was determined, a synthetic guide template for the left hemipelvis was manufactured by stereolithography apparatus (SLA) with light-sensitive resin (Fig. 2). The synthetic guide template for the left hemipelvis could be manufactured in a similar manner.
a Three-dimensional imaging of the navigation template. b The matching accuracy of template and the posterior column of acetabulum. the solid model of navigation template was manufactured by stereolithography apparatus (SLA) with light-sensitive resin. c The guide template was placed in the area of quadrilateral. d The three orientation entry points at the guide template, labeled as 1, 2 and 3 from the anterior to the posterior on the AP view, indicated the first, second and third screw entry points on the acetabulum, respectively
Insertion of guiding needles with the guide template in cadaveric specimens of the pelvis
Thirty right adult pelvises from the corpses (16 males and 14 females), stripped from soft tissue, were used for the screw placement. The guide template was attached to the quadrilateral surface and the ala ilii, with the posterior edge of the vertical plane of the template aligned with the posterior rim of the square area as much as possible. The operator held the template with his left hand and stabilized it on the pelvis, and then drilled and placed three guiding needles into the orientation entry points of the template with his right hand.
Evaluation of the accuracy of needle and screw placement aided by the guide template
Localization of the guide needles and screws in the posterior column was observed by naked-eye and X-ray examinations. The quality of guide-needle placement aided by the template in each hole was evaluated according to the following criteria: accurate insertion, defined as the exit point of the guide needle was close to the ischial tuberosity; fine insertion, defined as the exit point of the guide needle was located at the superior border of the lesser sciatic notch; failed insertion, defined as the exit point of the guide needle was penetrating the inner bone cortex or into the articular cavity. After assessment of the needle placement, lag screws were inserted into the holes with accurate and fine insertion. Finally, X-ray examination was performed to further assess the quality of screw placement.
Statistical analysis
The data were analyzed using SPSS 13.0 software and presented as mean ± SD. The t-test was used for two independent quantitative variables. Multiple samples ranked data were analyzed with Kuskal-Wallis H test. A value of p < 0.05 was regarded as statistically significant.
Clinical application of the template
Five patients with displaced acetabular fractures were operated on in our hospital by the same surgical team. There were three men and two women with a mean age of 35 years (28–56). The associated fracture types included four simple-pattern both-column fractures and one transverse fracture (Table 3). An ilioinguinal approach was considered only in all patients. When the fracture reduction was performed, spring plates would be used for the anterior column and the posterior column be fixed with lag screws under the navigation template. (Fig. 3). Finally, we recorded the time required for the lag screw insertion and the number of X-ray images that needed to be taken.
Results
Parameter measurements
Patient demographics showed 54 male and 42 female patients with a mean age of 40.3 ± 16.5 years (15-72 years) and 41.4 ± 18.9 years (17-74 years), respectively. The average distance of OD was 13.6 ± 2.2 mm, that of DG was 15.3 ± 4.0 mm, the angle α between the cylinder and coronal plane was 15.4 ± 4.1 °, the angle β between the square area and acetabulum wing was 132.3 ± 6.3 °, and the PG arch degree of arcuate edge was 41.1 ± 7.6 R. There were multiple gender-specific differences in the measured parameters, which are summarized in Table 1. For all parameters, independent sample t-test was performed. The DG distance in females (13.4 ± 2.6 mm) was longer than in males (17.1 ± 4.4 mm) (p < 0.05). There were no significant differences between males and females in OD length, the PG radian of the arcuate edge, angle α, and angle β.
Accuracy of guiding needle insertion aided by the guide template in the cadaveric test
The quality assessment of each insertion of guiding needle at each entry hole in each cadaveric specimen is shown in Table 2. There were significant differences regarding insertion accuracy between the three entry holes (χ2 = 21.158, p = 0.000). The second yielded the best accuracy, followed by the first and then the third. Of the second entry hole, the exit point was located close to the ischial tuberosity of the pelvis in 14 male and 9 female specimens, and superior to the border of the lesser sciatic notch in two male and five female specimens, suggesting a 100 % rate of accurate and fine insertion.
Accuracy of lag screw insertion aided by the guide template in clinic application
One lag screw was accurately inserted into the posterior column of the pelvis through the first or second entry holes in each of the five selected patients. Table 3 lists the detailed information concerning the insertion of guiding needles and lag screws and the surgery as well. The mean time required was 5.8 (3–10) minutes and 5.2 (4–8) X-ray images were taken for placement the lag screw. Postoperative follow-up ranged from six to 24 months with a mean of eight months (Fig. 4). The functional outcome evaluated according to the D’Aubigne-Postel scoring system [22], which is based on the level of pain, the patient’s walking ability and the range of motion of the hip joint. In the present study, the overall clinical result was excellent (17-18 points) in two patients, good (15-16 points) in two, fair (12-14 points) in one, and no poor result.
Discussion
The present study testified the accuracy and safety of a novel guide template we designed with virtual 3D reconstruction models of the pelvis. The final metal version of the template facilitated accurate insertion of antegrade lag screws into the posterior column in operative management of complex acetabular fractures, indicating it is a useful tool in clinic.
It has been widely accepted and recommended that the lag screw technique should be used in the posterior column as a useful fixation for complex acetabular fractures, such as transverse and T-shaped fractures [12–14, 23]. The conventional posterior column lag screw fixation for acetabular fracture is a difficult technique and has potential risks of vessel injury [24, 25], hip joint penetration and excessive radiation exposure, due to complex 3D pelvic and acetabular anatomy with narrow placement corridors. In order to place the lag screws accurately, in this study we had designed and manufactured a guide template which successfully assisted the lag screw placement in the posterior column and was tested for feasibility and accuracy in the cadaveric test.
Several cadaveric studies [20, 26] provided the anatomic basis for lag screw fixation in the posterior column. However, there were some differences in entry point, angle, diameter and length of the lag screw in the posterior column, due to different measuring methods used. Mu et al. [21] believed that the optimal entry point was located at the inner table of the ilium for antegrade lag screw fixation, 23.5 ± 3.4 mm (posterior distance) anterior to the junction of the anterior border of iliosacral articulation and the linea terminalis and 16.8 ± 2.1 mm (lateral distance) laterally perpendicular to the linea terminalis. The mean inclination of the functional axis of the posterior column was 119.18° ± 2.32° in the coronal plane and 57.36° ± 4.28° in the sagittal plane. The length of lag screw was 104.8 ± 4.2 mm. Dienstknecht et al. [27] found that the distance of antegrade entry point for the posterior column screw to the anterior superior iliac spine was 7.4 ± 0.86 cm, to the anterior inferior iliac spine was 5.3 ± 0.22 cm, to the iliopectineal eminence was 5.1 ± 0.97 cm, to the ischial spine was 8.0 ± 1.38 cm, to the sacroiliac joint on height linea terminalis was 3.5 ± 0.49 cm, and to the linea terminalis was 1.5 ± 0.99 cm in the male specimens. There were no gender differences in measurements around the antegrade entry point of the posterior column. As in this study, the entry points were determined by retrograde penetration, but we had different results from theirs. The ischial tuberosity has the highest bone mass and is generally regarded as the most suitable exit point. In this study, a virtual cylindrical implant was placed along the longitudinal axis of the acetabular posterior column, passing through the ischial tuberosity; its diameter was augmented and its direction was adjusted. We rendered the maximum freedom for the cylinder in the posterior column, making it pass along the posterior column at its maximum diameter. The orifice (O) of this cylinder out of the acetabulum was thought as the entry point of the lag screw. We made an iliac inguinal incision before we performed subperiosteal dissection of the iliac inner panel afterwards until the sacroiliac joint was exposed in the lateral window of the incision. After finding the frontmost edge of the sacroiliac joint (point G) with careful finger exploration and the sacroiliac eminence at the front (point P), we measured the distance between the entry point and arcuate edge (OD), which was 13.6 ± 2.2 mm. Point D was determined at the arcuate edge and OD as the shortest distance between the entry point and arcuate edge (15.3 ± 4.0 mm). The arch degree between arcuate PG was 41.1 ± 7.6 R, the angle α between cylinder and coronal plane was 15.4 ± 4.1 °, and the angle β between square area and iliac wing plane was 132.3 ± 6.3 °. The data provided anatomical basis for future design of a guide template.
Application of computational software, reverse engineering principle and rapid prototyping technique in the medical field provided technical support for design of a guide template [28–32]. In this study, we successfully determined entry points of the screws, and designed the reverse template adhesion to the bone surface according to the measured anatomical parameters, using the reverse engineering technique at the base of the 3D reconstruction digital anatomical model. The template employed the exact information for the antegrade lag screw. The solid model of the template was made with a rapid prototyping technique. Fu et al. [31] constructed a patient-specific biocompatible drill template and evaluated its accuracy in placing cervical anterior transpedicular screws. Jin et al. [32] also set up a kind of sacroiliac joint screw insertion. They all performed successfully with the same method. Our template had a good match with the cadaveric pelvis, with no significant difference between males and females. Using the guide template, we placed the antegrade lag screw in the pelvic samples and had the following outcomes. When the screw was placed from the first entry point, 76.7 % (n = 23) of the orifices were located at the superior border of the lesser sciatic notch. We thought the lag screw could be placed with this entry point guiding, if the involved fracture line of the posterior column was located at the middle and upper segments of the quadrilateral surface. For the second entry point, 76.7 % (n = 23) of the orifices were located close to the ischial tuberosity, with no screw penetration into the joint or through the bone cortex, especially in the male pelvis, whose orifices were all located near the ischial tuberosity. Therefore, we suggest that the second entry point should be the first choice when this guide template is used to assist the lag screw placement in the posterior column. When the third entry point was used, the screw easily slipped into the joint, giving a failure rate of 50 % (n = 15). Therefore, for patients with a relatively small pelvis, this entry point should not be suggested or a tinier screw is recommended for combined fixation of the posterior column.
This template has the following advantages. It is a simple entry procedure, only requiring an operator to place this guide template closely adhered to the anatomical structure. Because this is enough for exact localization and orientation for the posterior column, X-ray examination during the procedure will be greatly reduced. Since this template design is based on the most precise path information, there may not be a bad localization even if the patient position changes during the operation. To the best of our knowledge, no similar template has been reported for posterior column fractures of the acetabulum. Since our present template is novel, simple and easy to prepare, it may be hopefully applied to solve the problem of posterior column screw placement. However, the template was based on the CT scanning data we collected from 96 adult pelvises in this study. The sample size of study is not big enough. Moreover, the pelvic size varies from person to person and between sexes. We only designed one size of guide template, which may not fit all patients. Further studies are warranted for test of its accuracy. This template can assist the antegrade lag screw placement to fix the acetabular posterior column fractures only through the anterior approach, but it is not fit for percutaneous fixation. Before placing the screw, the posterior column must be reset satisfactorily. Even after this accurate template is used, X-ray imaging is still needed to observe the screw placement by an experienced operator.
Digital orthopedic science is a discipline to study bone morphology with imaging software. It is a new method for basic and applied research in orthopedic science. Compared with traditional cadaveric study, it is characterized with high accuracy, consistent results, repeatability, and economy in medical resources.
References
Gansslen A, Oestern HJ (2001) Acetabular fractures. Chirurg 82:1133–1148, quiz 49-50
Schmidt-Rohlfing B, Reilmann H, Pape HC (2010) Fractures of the acetabulum. Diagnostic and therapeutic strategies. Unfallchirurg 113(3):217–229
Matta JM, Anderson LM, Epstein HC, Hendricks P (1986) Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res 205:230–240
Milenkovic S, Saveski J, Radenkovic M, Vidic G, Trajkovska N (2011) Surgical treatment of displaced acetabular fractures. Srp Arh Celok Lek 139(7-8):496–500
Briffa N, Pearce R, Hill AM, Bircher M (2011) Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg (Br) 93(2):229–236
Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg (Br) 87(1):2–9
Harris AM, Althausen P, Kellam JF, Bosse MJ (2008) Simultaneous anterior and posterior approaches for complex acetabular fractures. J Orthop Trauma 22(7):494–497
Wang G, Pei G, Gu L, Zhu L, Guo G, Xia T (2002) Operative treatment of acetebular fractures. Zhonghua Wai Ke Za Zhi 40:657–661
Kaempffe FA, Bone LB, Border JR (1991) Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma 5(4):439–445
Chang JK, Gill SS, Zura RD, Krause WR, Wang GJ (2001) Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Relat Res 392:433–441
Shazar N, Brumback RJ, Novak VP, Belkoff SM (1998) Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res 352:215–222
Mouhsine E, Garofalo R, Borens O, Wettstein M, Blanc CH, Fischer JF, Moretti B, Leyvraz PF (2005) Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury 36(11):1330–1336
Starr AJ, Reinert CM, Jones AL (1998) Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma 12(1):51–58
Hong G, Cong-Feng L, Cheng-Fang H, Chang-Qing Z, Bing-Fang Z (2010) Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based computerized guide. Arch Orthop Trauma Surg 130(9):1177–1183
Gansslen A, Krettek C (2009) Internal fixation of acetabular both-column fractures via the ilioinguinal approach. Oper Orthop Traumatol 21(3):270–282
Connelly CL, Archdeacon MT (2012) Transgluteal posterior column screw stabilization for fractures of the acetabulum: a technical trick. J Orthop Trauma 26(10):e193–e197
Yu YH, Tseng IC, Su CY, Huang JW, Wu CC (2011) Modified technique of percutaneous posterior columnar screw insertion and neutralization plate for complex acetabular fractures. J Trauma 71(1):198–203
Rommens PM (2007) Is there a role for percutaneous pelvic and acetabular reconstruction? Injury 38(4):463–477
Ochs BG, Gonser C, Shiozawa T, Badke A, Weise K, Rolauffs B, Stuby FM (2010) Computer-assisted periacetabular screw placement: comparison of different fluoroscopy-based guide procedures with conventional technique. Injury 41(12):1297–1305
Oberst M, Hauschild O, Konstantinidis L, Suedkamp NP (2012) Effects of three-dimensional guide on intraoperative management and early postoperative outcome after open reduction and internal fixation of displaced acetabular fractures. J Trauma Acute Care Surg 73(4):950–956
Mu WD, Wang XQ, Jia TH, Zhou DS, Cheng AX (2009) Quantitative anatomic basis of antegrade lag screw placement in posterior column of acetabulum. Arch Orthop Trauma Surg 129(11):1531–1537
D’Aubigne RM, Postel M (1984) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg 36A:451–475
Prasartritha T, Chaivanichsiri P (2013) The study of broken quadrilateral surface in fractures of the acetabulum. Int Orthop 37(6):1127–1134
Abo-Elsoud M, Radwan YA, Gobba M, Sadek F (2014) Short-segment fixation through a limited ilioinguinal approach for treating anterior acetabular fractures: a historical-control study. Int Orthop 38(7):1469–1475
Bronsema E, te Stroet MA, Zengerink M, van Kampen A, Schreurs BW (2014) Impaction bone grafting and a cemented cup after acetabular fracture. Int Orthop 38(12):2441–2446
Shahulhameed A, Roberts CS, Pomeroy CL, Acland RD, Giannoudis PV (2010) Mapping the columns of the acetabulum—implications for percutaneous fixation. Injury 41(4):339–342
Dienstknecht T, Muller M, Sellei R, Nerlich M, Muller FJ, Fuechtmeier B et al (2012) Screw placement in percutaneous acetabular surgery: gender differences of anatomical landmarks in a cadaveric study. Int Orthop 37(4):673–679
Zhang YZ, Lu S, Xu YQ, Shi JH, Li YB, Feng ZL (2009) Application of guide template to fixation of sacral fracture using three-dimensional reconstruction and reverse engineering technique. Chin J Traumatol 12(4):214–217
Hernigou P, Ratte L, Roubineau F, Pariat J, Mirouse G, Guissou I, Allain J, Lachaniette CH (2013) The risk of dislocation after total hip arthroplasty for fractures is decreased with retentive cups. Int Orthop 37(7):1219–1223
Bagaria V, Deshpande S, Rasalkar DD, Kuthe A, Paunipagar BK (2011) Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol 80:814–820
Fu M, Lin L, Kong X, Zhao W, Tang L, Li J, Ouyang J (2013) Construction and accuracy assessment of patient-specific biocompatible drill template for cervical anterior transpedicular screw. PLoS One 8(1), e53580
Jin D, Wang D, Zhang YZ, Xiang DY, Qin Y, Pei GX (2009) Design and preliminary clinical application of a new digitalized guide template for fixation of the inferior tibiofibular joint. Nan Fang Yi Ke Da Xue Xue Bao 29(7):1364–1366
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, H., Wang, G., Li, R. et al. A novel navigation template for fixation of acetabular posterior column fractures with antegrade lag screws: design and application. International Orthopaedics (SICOT) 40, 827–834 (2016). https://doi.org/10.1007/s00264-015-2813-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2813-8