Abstract
Introduction
The treatment of displaced acetabular fractures with formal open reduction and internal fixation has gained general acceptance. However, extensile exposure can lead to complications. Two-dimensional fluoroscopy-based computerized navigation for placement of percutaneous screw across non-displaced acetabular fractures has attracted interest by making use of stored patient-specific imaging data to provide real-time guidance in multiple image planes during implant placement. The purpose of the present study was to document early treatment results and complications associated with this new technique and evaluate its clinical application to displaced acetabular fractures amenable to closed or limited open reduction.
Materials and methods
Eighteen adult patients with 12 non-displaced and 8 displaced acetabular fractures were treated with percutaneous screw fixation under the guidance of a fluoroscopy-based navigation system. There were 14 men and four women with a mean age of 42.1 years (range 19–54 years). According to the AO and Orthopaedic Trauma Association Classification, there were nine 62-A3, five 62-B1, three 62-B2, and three 62-B3. The mean follow-up was 21 months (range 12–28 months). The mean time from injury to surgery was 4 days (range 2–7 days).
Results
A total of 30 acetabular screws were inserted, including 21 anterior column screws and 9 posterior column screws. The average operation time was 24.6 min (range 16–47 min) from the image acquisition to wound closure. The average fluoroscopic time was 28.4 s (range 11–58 s). Compared to the final position of the screw, the average deviated distance of wire tip was 2.5 mm (range 1.1–3.6 mm) and the average trajectory difference was 2.45° (range 1.5°–4.6°). Maximal gap displacement averaged 10 mm (range 2–22 mm) preoperatively and 3 mm (range 0–5 mm) postoperatively; while maximal step displacement averaged 4 mm (range 1–10 mm) preoperatively and 2 mm (range 0–4 mm) postoperatively. One patient sustained a transient femoral nerve palsy and resolved 2 months after the operation. No superficial or deep infection occurred. Using the rating system of D’Aubigne and Postel, 13 patients had excellent results, 4 patients had good results, and 1 patient had a fair result.
Conclusion
Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based navigation could be applied not only to non-displaced fractures but also to displaced fractures amenable to closed or limited open reduction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The treatment of displaced acetabular fractures with formal open reduction and internal fixation has gained general acceptance [21, 27, 40]. Although non-displaced or mild displaced acetabular fractures can be managed with non-operative treatment modality, internal fixation of these fractures may facilitate to prevent unstable fracture displacement and to allow early weight bearing in patients who have contralateral lower extremity injuries that preclude weight bearing [36]. However, traditional surgical treatment requires extensive exposure, which may be complicated by infection, blood loss, wound healing problems, abductor weakness, sciatic nerve palsy, and heterotopic ossification [15, 30, 31]. Therefore, it seems reasonable to find less invasive surgical procedures to achieve the same goals as in conventional open reduction and internal fixation. Percutaneous screw fixation of acetabular fractures has been reported [25, 36, 37]. As a 3D complex with susceptible structures crowded in a relatively small space, the pelvis provides only some narrow safe corridors for percutaneous screw fixation of acetabular fractures [2, 8, 24, 25]. Inaccurate insertion of screw can jeopardize intrapelvic organ [4, 29, 36]. To achieve good accuracy and avoid neural or vascular injury, the image intensifier is used most frequently in percutaneous acetabular fractures fixation in operation room environment [4, 37]. Because conventional fluoroscopy provides only a 2D image and interpretability to radiographic image is explicitly limited by superimposition of anatomical structures, it requires multiple images in different projections to determine the correct point of entry and direction of the screw. Furthermore, using conventional fluoroscopy, imaging is available in only one projection at a time. Thus, its use lengthens the procedure and exposes the patient and the medical team to a prolonged radiation time [1, 12, 23, 29, 35]. Moreover, as working around the complex anatomy of the acetabulum, initial screw placement with imaging in only one plane may result in an erroneous first pass of the guide wire, with potentially disastrous consequences [25].
Recently, fluoroscopy-based computerized navigation for the placement of percutaneous screw across non-displaced or minimally displaced acetabular fractures has attracted interest. With the use of stored patient-specific imaging data to provide real-time guidance in multiple image planes during implant placement, this technique not only potentially reduces operation time and radiation exposure to the patient and the surgeon significantly but also allows the surgeon to achieve maximum accuracy [6, 20, 24]. However, to date, little has been published in the literature regarding treatment of displaced acetabular fractures with a percutaneous screw fixation technique under a fluoroscopy-based navigation system [6]. We proposed that percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based navigation could be applied not only to non-displaced fractures but also to displaced fractures amenable to closed or limited open reduction. The purpose of the present study was to document the clinical application of percutaneous screw fixation under 2D fluoroscopy-based computerized navigation for non-displaced and displaced acetabular fractures, to describe early results of treatment and complications associated with this new technique, and to determine if this new technique can be a reliable method in some patients with displaced acetabular fractures amenable to closed or limited open reduction.
Materials and methods
From February 2007 to June 2008, 31 adult patients with 33 acutely closed acetabular fractures were attempted to stabilize fractures with percutaneous screw fixation under the guidance of a 2D fluoroscopy-based navigation system. Patients treated after 7 days from the primary injury or with significant subchondral impaction, free intra-articular fragments or displaced fractures of the posterior wall of the acetabulum visible on the standard X-rays and CT scans were not included in the attempt of percutaneous screw fixation. Patients were eligible for inclusion in this retrospective study if they had a non-displaced acetabular fracture with contralateral lower extremity or other part injuries, an unstable acetabular fracture, or displaced acetabular fractures that could be reduced with a closed or limited open reduction method. Due to inadequate reduction of displaced acetabular fracture with closed or limited open reduction method, 13 acetabular fractures were conventional open reduction and internal fixation. Therefore, 18 patients with 20 acetabular fractures were included in this retrospective study. All procedures in this study were approved by our Institutional Review Board. All patients were treated by two senior surgeons. They were familiar with the usage of this navigation system and had gained a lot of experience in percutaneous screw placement. There were 14 men and 4 women, with a mean age of 42.1 years (range 19–54 years). Ten right and left acetabulums were involved, respectively. Two of the patients had bilateral acetabular fractures. The mechanisms of injury were a vehicle accident for 13 patients and a fall for 5. According to the AO and Orthopaedic Trauma Association Classification [26], there were nine 62-A3, five 62-B1, three 62-B2, and three 62-B3. There were 12 non-displaced acetabular fractures and 8 displaced fractures. Seven patients had an isolated acetabular fracture. In four of the patients, there was iliac wing fracture, sacroiliac joint fracture-dislocation, or diastasis of the symphysis pubis. Four patients presented with contralateral or ipsilateral lower extremity fractures. One patient sustained an injury of the ipsilateral limb fractures, lumbar fracture, and traumatic ipsilateral sciatic nerve palsy. All patients underwent surgical treatment of the acetabulum within 7 days of the injury. The mean time from injury to surgery was 4 days (range 2–7 days).
Under general anesthesia, the patient was placed in the supine position on a radiolucent operating table. For displaced acetabular fracture, reduction was performed first via manipulation of the injured hip [36]. The hip was manipulated in external and internal rotation, abduction, adduction, and longitudinal traction. Traction on the muscle was used to bring the fracture fragments into alignment. Schanz screws, sometimes, were inserted into the ilium and the greater trochanter to facilitate reduction. A temporary external fixator was applied to maintain reduction. Reduction was judged using fluoroscopy. If acetabular fracture alignment was not acceptable, reduction was performed through a limited open approach with the aid of a reduction clamp [36]. Six acetabular fractures required this method to achieve an adequate reduction. The clamp was placed through a small stab wound above the anterior–superior iliac spine or at the medial of iliacus muscle, down over the pelvic brim and was then seated against the displaced acetabular fracture. During the use of the clamp, the hip was flexed in order to relax the iliopsoas muscle complex. The outer tine of the clamp was passed through a small wound in the abductor muscles and was seated in the supra-acetabular region. Reduction was judged again on fluoroscopy. If reduction was adequate, stabilization was performed with percutaneously placed cannulated screws under the fluoroscopy-based computerized navigation. Otherwise, it was advisable to attempt formal open reduction and internal fixation.
The fluoroscopy-based Navigation System II (Stryker, Freiburg, Germany) consists of a system platform, a C-arm fluoroscope adapted for use with a navigation system, and an equipment for optoelectronic position detection called tracking. A Siremobil Compact L C-arm fluoroscope (Siemens Medical Engineering, Germany) was prepared for use with navigation system by attaching a tracker with affixed infrared emitting diodes to the image intensifier component of the C-arm fluoroscope. The system platform with an infrared camera was used for tracking and positioning the fluoroscope, patient’s skeletal anatomy, and a customized specific surgical drill guide by the trackers attached.
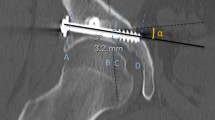
Acetabular fractures fixation with percutaneous screws under the guidance of the fluoroscopy-based computerized navigation system was performed in two steps (Fig. 1). The first step was image acquisition. After reduction of the fracture, a patient tracker was attached to the iliac crest to allow tracking of the acetabulum during the procedure. Fluoroscopic images of the acetabulum, such as pelvic inlet, outlet, Judet, and anterior–posterior views, were obtained and transferred and stored on the computer platform. As many as four standard fluoroscopic projections were displayed on the screen simultaneously. The second step was drilling a guide wire across acetabular fracture with continuous guidance by fluoroscopy-based navigation. A cannulated drill guide sleeve with a tool tracker transmitting infrared light to the digitizing camera was used. During navigation, the real-time position of the guide sleeve was overlaid onto the stored images on a computer monitor and the infrared camera continuously updated the sleeve 3D position simultaneously on all displayed images, allowing real-time feedback of the acetabulum and surgical tool position as the guide sleeve was moved by the surgeon. This helped the surgeon to determine accurately the entry point and direction of each screw. At the same time, by means of an extended virtual line from the planned screw, the correct length of the planned screw was calculated on the monitor screen. Depth of drilling was controlled by placing a stop on the guide wire. After identification of the precise entry point, the skin was incised about 1 cm center at the point. For anterior column screw placed in an antegrade direction, a small drill bit opened the outer cortex of the pelvis at the desired entry point. After satisfactory virtual alignment was achieved, the wire was inserted under the navigation system. Then the position of the wire was verified with the fluoroscopy in different views. Only the wire without intra-articular penetration and cortical perforation was acceptable. Otherwise the second attempt of guide wire inserting was performed. After the guide sleeve with the tool tracker was driven through the guide wire, the spatial position of the actual line of wire inserting and the virtual line from the intended screw was presented simultaneously on four views. These views was stored intra-operatively and analyzed postoperatively to calculate the angle between the actual and virtual line and the distance between the actual wire tip and the virtual line with a special software (MB-Ruler 3.4, Markus Bader). A 6.5-mm Asnis III cannulated screw (Stryker Trauma, Switzerland) was then placed over the guide wire. The position of screw was checked again and the small stab incision was irrigated and closed with statures.
A 54-year-old male sustained a closed left acetabular fracture and contralateral lower extremity fractures in a vehicle accident. a Preoperative anteroposterior radiograph shows a minimally displaced acetabular fracture. b The real-time spatial position of the guide sleeve is presented simultaneously on four fluoroscopic projections on a computer monitor. A dotted line is a virtual linear continuation presenting the track in which the guide wire is planned to be inserted. c An antegrade anterior column screw and d a retrograde posterior column screw were driven through the guide wire. e Anteroposterior postoperative radiograph demonstrates satisfactory fixation and alignment
The anterior column screw could be placed in either an antegrade (cephalad to caudad) or retrograde (caudad to cephalad) direction [10, 25, 37]. For antegrade placement, the screw was inserted from the body of the iliac bone toward the symphysis pubis and passes the acetabular cavity on its medial side and runs inside the superior ramus of the pubis. The patient tracker was placed in the iliac crest on the contralateral side of the acetabular fracture. By virtue of multiple views provided simultaneously by navigation system, the optimal entry portal on the skin was chosen and the guide wire was drilled to the appropriate depth. Confirmatory images were obtained and the cannulated screw finally was passed over the guide wire. For retrograde placement, the screw was placed in the opposite direction to antegrade placement of anterior column screw with patient tracker attached to the ipsilateral iliac crest. The guide wire was placed against the ipsilateral pubic tubercle through a small incision and then passed medially to the acetabulum and finished in the superior to the acetabular cavity. A chosen cannulated screw was inserted finally. As for the posterior column screw, retrograde placement was performed under the guidance of navigation system. To place retrogradely the posterior column screw, the ipsilateral leg should be held in flexion position of the hip and knee and slightly external rotation position of the hip to relax the sciatic nerve. A guide wire was placed in the center of the tuberosity and drilled up the posterior column. Then a cannulated screw was placed across the fracture.
Physiotherapy was started on the first postoperative day with continuous passive motion. Assisted active range of motion and isometrical exercises were initiated on the second postoperative day. Patients were followed postoperatively until fracture healing was achieved. One independent observer who was not involved in the clinical care of the patients performed a complete follow-up assessment. The mean follow-up was 21 months (range 12–28 months). For all cases, acetabular fracture reduction was assessed using preoperative and postoperative computed tomography scans [3] (Fig. 2).
A 51-year-old male sustained a closed acetabular fracture from a vehicle accident. a–c Preoperative CT scan images show an obviously displaced acetabular fracture. d–f Postoperative CT scan images demonstrate fracture fixation and residual displacement despite obtaining a perfect reduction determined by intra-operative radiographs
Clinical outcome was assessed at final follow-up using the rating system described by D’Aubigne and Postel [7].
Results
A total of 30 acetabular screws were inserted, including 21 anterior column screws and 9 posterior column screws. There were one acetabular screw in ten patients, two in five patients, three in two patients, and four in one patient. The average operation time was 24.6 min (range 16–47 min) from the image acquisition to wound closure. The average fluoroscopic time was 28.4 s (range 11–58 s). With the use of computer assistance, the first pass of the guide wire was acceptable without intra-articular penetration or cortical perforation in 83.3% of the procedures with the second attempt in 10% and the third attempt in 6.7%. Compared to the final position of the screw, the average deviated distance of wire tip was 2.5 mm (range 1.1–3.6 mm) and the average trajectory difference was 2.45° (range 1.5°–4.6°). Maximal gap displacement averaged 10 mm (range 2–22 mm) preoperatively and 3 mm (range 0–5 mm) postoperatively; while maximal step displacement averaged 4 mm (range 1–10 mm) preoperatively and 2 mm (range 0–4 mm) postoperatively.
One patient sustained a transient femoral nerve palsy which was attributed to reduction clamp inserting from the use of the limited open reduction method rather than screw fixation itself and resolved 2 months after the operation. No superficial or deep infection occurred. No evidence was noted of secondary displacement of the fragment, degenerative articular changes, or screw failure. No heterotopic ossification was noted.
Using the rating system of D’Aubigne and Postel, 13 patients had excellent results, 4 patients had good results, and 1 patient had a fair result. The excellent to good rate was 94%. The patient with the fair result was a polytrauma patient with ipsilateral limb fractures and sciatic nerve lesion.
Discussion
Fluoroscopy-based computerized navigation offers the capability of decreasing operation time and radiation exposure chance [6, 12, 20, 24]. As up to four fluoroscopic projections can be displayed simultaneously on the navigation screen, no intra-operative re-orientation of fluoroscope is needed so as to save fluoroscopic radiation exposure and reduce operation time. Lin et al. [20] reported an average of 38 s of fluoroscopy time and 40 min of operation time in three patients with percutaneous retrograde screw fixation of non-displaced or mild displaced anterior column fracture of the acetabulum under fluoroscopy-based navigation. Crowl et al. [6] showed the fluoroscopy time of less than 45 s in nine patients with closed reduction and percutaneous fixation of anterior column acetabular fractures under the guidance of computer-assisted virtual fluoroscopy images. With the similar technique, our results of the average fluoroscopy time of 28.4 s and average operation time of 24.6 min compared well with these series and were superior to that of conventional fluoroscopy alone with a mean fluoroscopic time of 62-73 s and a mean operation time of 30-75 min [6, 25, 36].
Fluoroscopy-based navigation offers the advantage of the 3D visualization of the drilling procedure, and thus improves the precision of the procedure [32]. In a series of 55 iliosacral screws using virtual fluoroscopy, Kahler [16] showed that the mean deviation from the intended path was 1.9 mm at a drilling depth of 100 mm and the final position of the guide wire was within 5 mm of the intended path in 96% of all trials. Using percutaneous insertion of 45 cannulated screws in 29 patients, Mosheiff et al. [24] reported that the wire tip deviation was less than 2 mm, and the maximum trajectory difference was less than 5°. In the current series, the mean wire tip deviation of 2.5 mm and the mean deviation angle of 2.45° are comparable to that of these above studies.
The patient who sustains an acetabular fracture may have other associated injuries that require early assessment and simultaneous management. Multiple changes of patient’s position and extensive surgical procedure of acetabular fractures and associated injuries can aggravate the adverse impact on a multiply injured patient who is at risk for multiple organ failure [32, 33]. Virtual fluoroscopic navigation provides potentially some advantages in a multiply injured patient over traditional surgical methods. The change of patient intra-operative position generally is unnecessary to percutaneous screw fixation of acetabular fractures, whether anterior column or posterior column fractures, with fluoroscopy-based computerized navigation. This technique may allow surgeons to manage other associated injuries and perform other surgical procedures simultaneously so as to reduce the whole operation time and improve functional recovery. Moreover, the skin incision can be determined more accurately using the virtual extended line from the planned screw, which may significantly reduce soft tissue dissection.
The main treatment goal of acetabular fractures is anatomic or near-anatomic reduction of articular surface [19, 22]. The quality of reduction of articular surface is a very important prognostic factor. It should be kept in mind that fluoroscopy-based navigation for percutaneous screw fixation of acetabular fractures is used only after an accurate fracture reduction has been achieved [8, 13, 34]. Despite excellent reduction of displaced acetabular fractures shown in the images of the C-arm fluoroscope during the operation, some fractures were still not able to achieve anatomic reduction in the postoperative assessment of fracture reduction using CT scans. Computed tomography has been shown to be superior to radiography for detection of gap and step information of the joint surface [3]. Although the CT-navigated system’s ability to provide tremendous accuracy in percutaneous implant placement is impressive, the image used for this virtual model cannot be updated readily in the operating room after fracture reduction maneuvers or trial positioning of implants, rendering it unsuitable for fracture cases in which reduction will be done after obtaining the CT scans [11, 16]. Moreover, performing CT-guided procedure in a conventional CT suite sometimes increases infection risk for hygienic reasons [6, 8]. On the other hand, although fluoroscopy-guided percutaneous fixation of acetabular fractures requires a lower radiation dose than percutaneous fixation under CT navigation does, it is difficult to evaluate 3D information on 2D images, particularly in the aspect of accurate detection of articular incongruity [5, 17]. Recently, developed Iso-C3D navigation seems to be an ideal application for reduction judgment and navigated implant placement [14]. Compared to the CT-based technique, this new technology requires neither a preoperative CT scan nor the preoperative application of external markers and can be used in a sterile operation theater. However, image quality of the Iso-C3D is found to be generally inferior to modern CT machines and is affected by body habitus, retained contrast medium, and bowel gas, as the bone can be thresholded more easily to eliminate such artifacts in CT scan [14, 28, 39]. Despite limitation of reduced image quality, 3D fluoroscopic imaging appears to be extremely accurate in evaluating acetabular fracture constructs and yields more detailed and accurate information regarding implant placement and articular reduction than standard fluoroscopy [9]. Therefore, the future use of 3D fluoroscopy-based navigation technique may help more accurately intra-operative assessments of acetabular facture reduction and lead to a better long-term outcomes.
Percutaneous screw fixation of acetabular fractures with fluoroscopic navigation is a technically demanding procedure [18, 20]. Surgeons who perform this kind of procedure should be familiar with not only the underlying concepts of the usage of this navigation system and the complications that may result from incorrect handling but also formal open reduction and internal fixation of acetabular fractures [18, 20]. In the event that adequate fluoroscopic images cannot be obtained, the surgeon must have the discipline to abandon the surgical navigation and use an alternative method [16]. Moreover, an experienced fluoroscopy technician who is familiar with percutaneous screw techniques and fluoroscopic navigation also facilitates the successful applications of these techniques. Despite good experience in computer-assisted percutaneous placement of iliosacral screws, cannulated hip screws, and distal locking screws of long bone nails, sometimes we had to correct the guide wire position after the first attempt in order to achieve optimal guide wire placement. In current study, the first pass of the guide wire was acceptable without intra-articular penetration or cortical perforation in 83.3% of the procedures.
Fluoroscopy-based navigation technique has a learning curve and may result in complications if any step of the navigation, from the image acquisition to cannulated screw insertion, is not done with sufficient care [16]. Good quality of the fluoroscopy projections is mandatory for safe and precise screw positioning. As the patient tracker is the only way the infrared camera can track acetabular fractures, this device should be fixed stably to iliac crest and remains in its initial position during the operation. Unnoticed manipulations of the tracker can lead to a complete shift of the images. Thus, any doubts about the consistency of the tracker position at any time must be verified immediately [18]. Moreover, the camera system needs a direct line-of-sight to the trackers and tracks the C-arm and the patient simultaneously. Incorrect spot and direction for the placement of the patient tracker and the camera system can obstruct the acquisition of acetabular images during the movement of C-arm fluoroscopy. In addition, for the navigation system, each tracked surgical tool is assumed to be non-deformable. Duo to plenty of muscles in the hip and the tendency of the long guide wire to bend, obviously, the use of a navigated rigid drill sleeve can prevent the extra osseous guide wire bending by soft tissues and reduce the deviation at the starting point and thus is safer and more accurate [18, 38].
There are several limitations of this study including the small cohort of patients, the retrospective methodology, and the selection bias of the patients. Additionally, the follow-up was relatively short. Therefore, although union could be documented in all patients, a longer follow-up period would help quantify to what extent, if any, the development of post-traumatic arthritis. Moreover, we did not choose to use X-, Y-, Z-coordinates of the wire or screw to document its spatial position for two reasons. First, using a 2D fluoroscopy navigation system, it was impossible to describe the spatial position of the wire or screw using X-, Y-, Z-coordinates. Here, multiple 2D images were used to provide a quasi-3D visualization to the surgeon. Thus, all the deviated distances and angles on four views of every screw were measured and used to evaluate the final results. Second, the acceptable standard of wire insertion without intra-articular penetration and cortical perforation indicated that the spatial position of the whole screw was more important than digital information of entry point or wire tip.
In conclusion, percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based navigation can be applied not only to non-displaced fractures but also to displaced fractures amenable to closed or limited open reduction. This treatment method can become a safe and effective alternative to traditional open reduction and internal fixation for the treatment of some displaced acetabular fractures in the future.
References
Alonso JA, Shaw DL, Maxwell A, McGill GP, Hart GC (2001) Scattered radiation during fixation hip fractures: is distance alone enough protection? J Bone Joint Surg (Br) 83:815–818
Attias N, Lindsey RW, Starr AJ, Borer D, Bridges K, Hipp JA (2005) The use of a virtual three-dimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures. J Bone Joint Surg (Br) 87:1520–1523
Borrelli J, Goldfarb C, Catalano L, Evanoff BA (2002) Assessment of articular fragment displacement in acetabular fractures: a comparison of computerized tomography and plain radiographs. J Orthop Surg 16:449–456
Carmack DB, Moed BR, McCarroll K, Freccero D (2001) Accuracy of detecting screw penetration of the acetabulum with intraoperative fluoroscopy and computed tomography. J Bone Joint Surg (Am) 83:1370–1375
Chmelova J, Sir M, Jecminek V (2005) CT-guided percutaneous fixation of pelvic fractures. Case reports. Biomed Papers 149:177–181
Crowl AC, Kathler DM (2002) Closed reduction and percutaneous fixation of anterior column acetabular fractures. Comput Aided Surg 7:169–178
D’Aubigne M, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg (Am) 36:451–475
Gay SB, Sistrom C, Wang GJ, Kahler DA, Boman T, McHugh N, Goitz HT (1992) Percutaneous screw fixation of acetabular fractures with CT guidance: preliminary results of a new technique. AJR 158:819–822
Geerling J, Gosling T, Gosling A, Ortega G, Kendoff D, Citak M, Krettek C (2008) Navigated pedicle screw placement: experimental comparison between CT- and 3D fluoroscopy-based technique. Comput Aided Surg 13:157–166
Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS (2007) Percutaneous fixation of the pelvic ring. J Bone Joint Surg (Br) 89:145–154
Gross T, Jacob AL, Messmer P, Regazzoni P, Steinbrich W, Huegli RW (2004) Transverse acetabular fracture: hybrid minimal access and percutaneous CT-navigated fixation. Am J Roentgenol 183:1000–1002
Hinsche AF, Giannoudis PV, Smiths RM (2002) Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res 395:135–144
Huegli RW, Staedele H, Messmer P, Regazzoni P, Steinbrich W, Gross T (2004) Displaced anterior column acetabular fracture: closed reduction and percutaneous CT-navigated fixation. Acta Radiol 45:618–621
Hufner T, Gebhard F, Grutzner PA, Messmer P, Stockle U, Krettek C (2004) Which navigation when? Injury 35(Suppl A):SA30–SA34
Kaempfe FA, Bone LB, Border JR (1991) Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma 5:439–445
Kahler DM (2004) Image guidance. Clin Orthop Relat Res 421:70–76
Kendoff D, Gardner MJ, Citak M, Kfuri M, Thumes B, Krettek C, Hufner T (2008) Value of 3D fluoroscopic imaging of acetabular fractures comparison to 2D fluoroscopy and CT imaging. Arch Orthop Trauma Surg 128:599–605
Langlotz F (2004) Potential pitfalls of computer aided orthopedic surgery. Injury 35(Suppl 1):17–23
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151:81–106
Lin YC, Chen CH, Huang HT, Chen JC, Huang PJ, Hung SH, Liu PC, Lee TY, Chen LH, Cheng JK (2008) Percutaneous antegrade screwing for anterior column fracture of acetabulum with fluoroscopic-based computerized navigation. Arch Orthop Trauma Surg 128:223–226
Matta JM (1994) Operative treatment of the acetabular fractures through the ilioinguinal approach—a ten year perspective. Clin Orthop Relat Res 305:10–19
Matta JM, Merritt PO (1988) Displaced acetabular fractures. Clin Orthop Relat Res 230:83–97
Mehlman CT, DiPasquale TG (1997) Radiation exposure to orthopaedic surgical team during fluoroscopy: how far away is far enough. J Orthop Trauma 11:392–398
Mosheiff R, Khoury A, Weil Y, Liebergall M (2004) First generation computerized fluoroscopic navigation in percutaneous pelvic surgery. J Orthop Trauma 18:106–111
Mouhsine E, Garofalo R, Borens O, Wettstein M, Blanc CH, Fischer JF, Moretti B, Leyvraz PF (2005) Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury 36:1330–1336
Muller ME (1996) The comprehensive classification of fractures of long bones, spine and pelvis, 2nd edn. Springer, Berlin
Myao KA (1994) Open reduction and internal fixation of the acetabulum. Clin Orthop Relat Res 305:31–37
Nolte LP, Beutler T (2004) Basic principles of CAOS. Injury 35(Suppl A):SA6–SA16
Norris BL, Hahn DH, Bosse MJ, Kellam JF, Sims SH (1999) Intraoperative fluoroscopy to evaluate fracture reduction hardware placement during acetabular surgery. J Orthop Trauma 13:414–417
Pantazoupoulos T, Mousafiria C (1989) Surgical treatment of central acetabular fractures. Clin Orthop Relat Res 246:57–64
Pennal GF, Davidson J, Garside H, Plewes J (1980) Results of treatment of acetabular fractures. Clin Orthop Relat Res 151:115–123
Przkora R, Bosch U, Zelle B, Panzica M, Garapati R, Krettek C, Pape HC (2002) Damage control orthopedics: a case report. J Trauma 53:765–769
Roberts CS, Pape HC, Jones AL, Malkani AL, Rodriguez JL, Giannoudis PV (2005) Damage control orthopaedics. J Bone Joint Surg Am 87:434–449
Rommens PM (2007) Is there a role for percutaneous pelvic and acetabular reconstruction? Injury 38:463–477
Sanders R, Koval KJ, DiPaquale T, Schmelling G, Stenzlert S, Ross E (1993) Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg Am 75:326–330
Starr AJ, Jones AL, Reinert CM, Borer DS (2001) Preliminary results and complications following limited open reduction and percutaneous screw fixation of displaced fractures of the acetabulum. Injury 32(Suppl 1):45–50
Starr AJ, Reinert CM, Jones AL (1998) Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma 12:51–58
Stöckle U, Krettek C, Pohlemann T, Messmer P (2004) Clinical applications—pelvis. Injury 35(Suppl 1):46–56
Wieners G, Pech M, Beck A, Konig B, Erdmenger U, Stockle U, Wust P, Felix R, Schroder RJ (2005) Comparison of radiation dose and image quality of Siremobil-IsoC(3D) with a 16-slice spiral CT for diagnosis and intervention in the human pelvic bone. Rofo 177:258–264
Wright R, Barrett K, Christie MJ, Johnson KD (1994) Acetabular fractures: long-term follow-up of open reduction and internal fixation. J Orthop Trauma 8:397–403
Acknowledgments
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Conflict of interest statement
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, G., Cong-Feng, L., Cheng-Fang, H. et al. Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based computerized navigation. Arch Orthop Trauma Surg 130, 1177–1183 (2010). https://doi.org/10.1007/s00402-010-1095-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1095-2