Abstract
Purpose
Active knee flexion is more important for daily activities than passive knee flexion. The hypothesis is that the intra-operative parameters such as osteotomized bone thickness and soft tissue balance affect the postoperative active flexion angle in total knee arthroplasty (TKA). Therefore, we evaluate the influence of intra-operative parameters on postoperative early recovery of active flexion after posterior-stabilized (PS) TKA.
Methods
The subjects were 45 osteoarthritic knees undergoing primary PS TKA with anterior-reference technique. Intra-operative soft tissue balance was measured using an offset type tensor, and each osteotomized bone thickness was also measured. Pre- and postoperative active knee flexion angles were measured using lateral radiographs. Liner regression analysis was used to determine the influence of these intra-operative parameters on postoperative active flexion angles or recovery of active flexion angles.
Results
Pre-operative flexion angle was positively correlated with postoperative flexion angle (R = 0.52, P = 0.0002). Postoperative flexion angle was negatively correlated with the osteotomized bone thickness of femoral medial posterior condyle (R = −0.37, P = 0.012), and femoral lateral posterior condyle (R = −0.36, P = 0.015). Recovery of flexion angle was slightly negatively correlated with gap difference calculated by subtracting joint gap at extension from that at flexion between osteotomized surfaces (R = −0.30, P = 0.046).
Conclusions
The osteotomized bone thickness of the femoral posterior condyle is a significant independent factor of postoperative flexion angles. This indicates that the restoration of the posterior condyle offset may lead to larger postoperative active flexion angles in PS TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most important goals of total knee arthroplasty (TKA) is to improve the functional range of flexion to the minimum 90° flexion that is required for normal daily activities [1]. Factors influencing range of flexion after TKA can mainly be classified into intra-capsular and extra-capsular factors. Among extra-capsular factors, the importance of pre-operative motion for postoperative results has been previously recognized [2–7]. Intra-capsular factors including implant design, ligament balance, flexion-extension gap balance, height of joint line, and patella resurfacing have also been discussed by many authors [8–12]. In this context, much enthusiasm has been recently directed towards posterior condylar offset (PCO), which was first described as a determinant for flexion by Bellemans et al. [13]. In addition, although soft tissue balancing has also been recognized as an essential surgical intervention for improving the outcome of TKA [14, 15], little has been clarified about the direct relationship between intra-operative soft tissue balance and postoperative outcomes.
We previously reported studies using an offset type tensor, in which we discussed the importance of maintaining a reduced and anatomically-oriented PF joint with the femoral trial component in place, in order to obtain accurate and more physiologically-relevant soft tissue balancing [16, 17]. We further reported the relationship between intra-operative soft tissue balance and the postoperative passive flexion angle using an offset type tensor in posterior-stabilized (PS) and cruciate-retaining (CR) TKA [18, 19]. However, there have been few reports that have considered the relationship between intra-operative parameters and the postoperative active flexion angle, which is more important for daily activities than the passive flexion angle.
The hypothesis of this study is that intra-operative parameters such as osteotomized bone thickness and soft tissue balance influence the postoperative active flexion angle. Therefore, the purpose of this study was to evaluate the influence of intra-operative parameters including soft tissue balance and osteotomized bone thickness on early recovery of active knee flexion after PS TKA.
Materials and methods
The subjects were 45 consecutive patients (45 osteoarthritic knees) who underwent primary PS TKA between March 2009 and January 2011. Those with valgus deformity and severe bony defects were excluded. The patient population comprised 39 women and six men with a mean age of 73.9 ± 6.1 years. The average pre-operative coronal plane alignment was 11.4 ± 4.4° in varus. Each surgery was performed by the same senior author (H.M.) using PS TKA (NexGen LPS Flex, Zimmer, Inc, Warsaw, IN) with a standardized surgical technique.
Surgical procedure
A medial parapatellar arthrotomy was performed using a tourniquet and the measured resection technique with a conventional resection block. The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) were both resected. A distal femoral osteotomy was performed perpendicular to the mechanical axis of the femur according to pre-operative long-leg radiographs. The surgical epicondylar axis was pre-operatively measured using computed tomography (CT). As Berger et al. [20] reported, the surgical epicondylar axis is a line connecting the sulcus of the medical epicondyle and the lateral epicondylar prominence, and the angle between the surgical epicondylar axis and posterior condylar line is defined as posterior condylar angle. Femoral external rotation was determined by pre-operative CT, intra-operative Whiteside line and transepicondylar axis. Femoral external rotation relative to the posterior condylar axis was 3° in 32 cases and 5° in 13 cases. A femoral posterior condylar osteotomy was performed using the anterior reference technique. A proximal tibial osteotomy was then performed with each cut made perpendicular to the mechanical axis in the coronal plane and with 7° of posterior inclination along the sagittal plane. No bony defects were observed along the eroded medial tibial plateau. After each osteotomy, we removed the osteophytes, released the posterior capsule along the femur and corrected any ligament imbalances in the coronal plane by appropriately releasing the medial soft tissues. The osteotomy and soft tissue release were carried out with a spacer block.
Intra-operative measurement with an offset type tensor
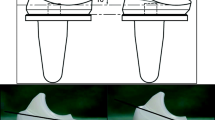
The offset type tensor consists of three parts: an upper seesaw plate, a lower platform plate with a spike and an extra-articular main body, as previously described [16–19, 21, 22].
This device is ultimately designed to permit surgeons to measure the ligament balance and joint centre gap both before and after femoral trial prosthesis placement, while applying a constant joint distraction force. Joint distraction forces ranging from 30 lb (13.6 kg) to 80 lb (36.3 kg) can be exerted between the seesaw and platform plates using a specially made torque driver which can change the maximum torque value. We evaluate two scales that correspond to the tensor: the angle (°, positive value in varus imbalance) between the seesaw and platform plates, and distance (mm, joint centre gap) between the centre midpoints of the upper surface of the seesaw plate and the proximal tibial cut. By measuring these angular deviations and distances under a constant joint distraction force, we are able to measure the ligament balance and joint centre gap. respectively.
Intra-operative measurement
The measurements were performed at extension and flexion of the knee with opposite bone surfaces in parallel orientation as usually done with conventional gap measurement. All measurements were performed with the patella-femoral (PF) joint reduced. After soft tissue balance evaluation between osteotomized surfaces, the femoral trial component was placed with tensor on the surface of the tibial bone cut, and PF joint was temporarily reduced by applying stitches both proximally and distally to the connection arm of the tensor. We also loaded 40 lbs of distraction force in all knees at 0° and 90° of flexion. The joint distraction force was set at 40 lbs, because it re-created the joint gap at full extension with femoral trial in place, which corresponds to the insert thickness indicated by our preliminary clinical studies. We loaded this distraction force several times until the joint component gap remained constant; this was done to reduce the error which can result from creep elongation of the surrounding soft tissues. During each measurement, the thigh was held and knee was aligned in the sagittal plane so as to eliminate the external load on the knee at 90° of knee flexion. Following the measurement, a NexGen prosthesis was implanted with cement.
Examined parameters
We measured the joint gap (mm) and varus ligament balance (°) with the knee at extension and flexion either before or after the femoral trial prosthesis was in place. Gap difference (mm) was calculated by subtracting joint gap at extension from joint gap at flexion between osteotomized surfaces. The thickness of each osteotomized bone of the distal femur, femoral posterior condyle, and proximal tibia was measured (mm).
Before and four weeks after surgery, each knee active flexion angle (°) was measured using the lateral radiograph of the knee with maximum active flexion in a supine position. Recovery of flexion angle (°) was calculated by subtracting pre-operative active flexion angle from postoperative flexion angle. Each postoperative passive flexion angle was also measured using a goniometer attached to the skin surface.
Statistical analysis
All values were expressed as mean ± standard error of the mean (SEM). The results were analysed statistically using a statistical software package (Statview 5.0, Abacus Concepts Inc., Berkeley, CA, USA). We performed liner regression to analyse the correlations between each factor and postoperative flexion angle or recovery of flexion angle. Furthermore, we performed multiple regressions with selected factors. P < 0.05 was considered statistically significant.
Results
Pre- and postoperative active knee flexion angles averaged 109.5 ± 1.9° and 105.9 ± 1.8°, respectively. Recovery of flexion angle averaged −3.6 ± 1.8°. Postoperative passive knee flexion angle averaged 121.0 ± 1.6° at four weeks after surgery. Osteotomized bone thickness is shown in Table 1. Gap difference was −0.36 ± 0.50 mm.
Pre-operative active flexion angle was positively correlated with postoperative active flexion angle (R = 0.52, P = 0.0002) (Fig. 1). Postoperative active flexion angle was negatively correlated with the osteotomized bone thickness of femoral medial posterior condyle (R = −0.37, P = 0.012), and femoral lateral posterior condyle (R = −0.36, P = 0.015) (Fig. 2). Recovery of flexion angle was slightly negatively correlated with gap difference (R = −0.30, P = 0.046) (Fig. 3). Furthermore, multiple regression analysis of the postoperative active flexion angle was demonstrated with the pre-operative active flexion angle and the osteotomized bone thickness of the femoral lateral posterior condyle, which were not correlated with each other. Postoperative active flexion angle was strongly correlated with pre-operative active flexion angle and the osteotomized bone thickness of femoral lateral posterior condyle (R = 0.65, P < 0.0001) (Fig. 4).
Correlation between postoperative flexion angle and osteotomized bone thickness of femoral posterior condyle. a Correlation between postoperative flexion angle and medial posterior condyle. b Correlation between postoperative flexion angle and lateral posterior condyle. Postoperative flexion angle was negatively correlated with femoral medial posterior condyle (R = −0.37, P = 0.012) and femoral lateral posterior condyle (R = −0.36, P = 0.015)
Discussion
The main findings in the present study were that the postoperative active flexion angle was negatively correlated with the osteotomized bone thickness of the femoral posterior condyle, and recovery of flexion angle was slightly negatively correlated with gap difference. This means a smaller osteotomized bone thickness of the femoral posterior condyle and smaller flexion gaps than extension gaps led to larger postoperative active flexion angles.
Knee range of motion (ROM) is one of the most important outcome variables used to assess the results of TKA. In daily activities, active knee flexion is more important than passive knee flexion, but passive ROM is usually reported and measured using a hand-held goniometer or as a visual estimation of knee flexion. Edwards et al. [23] reported 22 % of skin surface goniometric measurements and 45 % of visual measurements differed by 5° or greater from radiographic measurements. Laidlaw et al. [24] showed postoperative active knee flexion is less than postoperative passive knee flexion using the active flexion lateral radiograph, and suggested active knee flexion may be an important outcome variable for assessing functional results after TKA. Therefore, we focused on active knee flexion angle using active flexion lateral radiographs.
In the present study, the pre-operative active flexion angle was positively correlated with the postoperative active flexion angle (R = 0.52, P = 0.0002), as previous reports described [2–7, 18]. In addition, the postoperative active flexion angle was negatively correlated with the osteotomized bone thickness of the femoral posterior condyle (medial R = −0.37, P = 0.012; lateral R = −0.36, P = 0.015), and recovery of flexion angle was slightly negatively correlated with gap difference (R = −0.30, P = 0.046). Bellemans et al. [13] first defined the concept of PCO. They demonstrated the maximum knee flexion with squatting motion was limited by direct impingement of the posterior aspect of the tibial component against the posterior aspect of the femur in CR TKA. They concluded restoration of the PCO was important, since it allows a greater degree of flexion before impingement occurrences. However, the effect of PCO is uncertain with some researchers reporting increasing postoperative knee flexion with increasing PCO [13, 25], and others who report no significant correlation [26, 27]. The reasons for these differences may be attributed to the difference of the method of knee flexion as active or passive, and differences in prosthesis design—CR or PS TKA. In this study, we assessed the osteotomized bone thickness of femoral posterior condyle instead of PCO because we hypothesized that osteotomized bone thickness might be more accurate than PCO measured by lateral radiographs. As Clarke [28] reported, mean cartilage thicknesses of the posterior condyles were 1.7 mm (range, 0–4 mm) medially and 2.0 mm (range, 0–5 mm) laterally. They concluded that as the cartilage thickness is variable, future studies of PCO must adjust the preoperative radiographic measurements by the cartilage thickness measured intraoperatively. Therefore, we assessed the osteotomized bone thickness of femoral posterior condyle in the present study. With the anterior reference technique, the osteotomized bone thickness of the femoral posterior condyle depends on the femoral component size, i.e. if a larger component size is selected, the osteotomized bone thickness is smaller, which leads to a decreased flexion gap between the osteotomized surfaces, and restoration of the PCO can be obtained. Furthermore, there was no correlation between the osteotomized bone thickness of the femoral posterior condyle and the pre-operative active flexion angle, which means the osteotomized bone thickness of the femoral posterior condyles is an independent factor affecting the postoperative active knee flexion angle. One possible explanation of this mechanism is that when a larger femoral component is used, the distance between the rotational centre of the knee flexion movement and the tibial attachment site of hamstrings is longer, leading to an increase in the moment arm of the hamstrings, which is dynamically favourable in active knee flexion.
Despite the important findings in this study, there are several limitations. First, the patient number of the study is not large enough to be conclusive. Second, the postoperative flexion angle is multi-factorial. The tibial posterior slope and different prosthetic designs may afford varying results in the postoperative flexion angle. Third, the flexion angle was measured by active flexion in a supine position. Results would vary with passive knee flexion or squat motion. Further investigation is needed.
In conclusion, intra-operative parameters including soft tissue balance and osteotomized bone thickness significantly affected the postoperative active knee flexion in the early term after PS TKA. It is suggested that a larger femoral component would lead to restoration of the PCO and a better active flexion angle in PS TKA.
References
Insall J, Scott WN, Ranawat CS (1979) The total condylar knee prosthesis: a report of two hundred and twenty cases. J Bone Joint Surg Am 61-A:173–180
Anouchi YS, McShane M, Kelly F Jr, Elting J, Stiehl J (1996) Range of motion in total knee replacement. Clin Orthop Relat Res 331:87–91
Lizaur A, Marco L, Cebrian R (1997) Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br 79-B:626–629
Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75-B:950–955
Parsley BS, Engh GA, Dwyer KA (1992) Preoperative flexion. Dose it influence postoperative flexion after posterior-cruciate retaining total knee arthroplasty? Clin Orthop Relat Res 275:204–210
Ritter MA, Stringer EA (1999) Predictive range of motion after total knee replacement. Clin Orthop Relat Res 143:115–119
Matsumoto T, Tsumura N, Kubo S, Shiba R, Kurosaka M, Yoshiya S (2005) Influence of hip position on knee flexion angle in patients undergoing total knee arthroplasty. J Arthroplasty 20:669–673
Dennis DA (2001) Problems after knee arthroplasty. The stiff total knee arthroplasty: causes and cures. Orthopedics 24:901–902
Kawamura H, Bourne RB (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci 6:248–252
Schurman DJ, Matityahu A, Goodman SB, Maloney W, Woolson S, Shi H, Bloch DA (1998) Prediction of postoperative knee flexion in Insall-Burstein ll total knee arthroplasty. Clin Orthop Relat Res 353:175–184
Schurman DJ, Parker JN, Orstein D (1985) Total condylar knee replacement. A study of factors influencing range of motion as late as two years after arthroplasty. J Bone Joint Surg Am 67-A:1006–1014
Joshi AB, Lee CM, Markovic L, Murphy JCM, Hardinge K (1994) Total knee arthroplasty after patellectomy. J Bone Joint Surg Br 76-B:926–929
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84-B:50–53
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Muratsu H, Tsumura N, Yamaguchi M, Mizuno K, Kuroda R, Harada T, Yoshiya S, Kurosaka M (2003) Patellar eversion affects soft tissue balance in total knee arthroplasty. Trans Orthop Res 28:242
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2006) Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng 128:867–871
Matsumoto T, Mizuno K, Muratsu H, Tsumura N, Fukase N, Kubo S, Yoshiya S, Kurosaka M, Kuroda R (2007) Influence of intra-operative joint gap on post-operative flexion angle in osteoarthritis patients undergoing posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 15:1013–1018
Takayama K, Matsumoto T, Kubo S, Muratsu H, Ishida K, Matsushita T, Kurosaka M, Kuroda R (2012) Influence of intra-operative joint gaps on post-operative flexion angle in posterior-cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:532–537
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Matsumoto T, Kuroda R, Kubo S, Muratsu H, Mizuno K, Kurosaka M (2009) The intra-operative joint gap in cruciate-retaining compared with posterior-stabilized total knee replacement. J Bone Joint Surg Br 91-B:475–480
Muratsu H, Matsumoto T, Kubo S, Maruo A, Miya H, Kurosaka M, Kuroda R (2010) Femoral component placement changes soft tissue balance in posterior-stabilized total knee arthroplasty. Clin Biomech 25:926–930
Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ (2004) Measuring flexion in knee arthroplasty patients. J Arthroplasty 19:369–372
Laidlaw MS, Rolston LR, Bozic KJ, Ries MD (2010) Assessment of tibiofemoral position in total knee arthroplasty using the active flexion lateral radiograph. Knee 17:38–42
Massin P, Gournay A (2006) Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty 21:889–896
Kim YH, Sohn KS, Kim JS (2005) Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am 87-A:1470–1475
Hanratty BM, Thompson NW, Wilson RK, Beverland DE (2007) The influence of posterior condylar offset on knee flexion after total knee replacement using a cruciate-sacrificing mobile-bearing implant. J Bone Joint Surg Br 89-B:915–918
Clarke HD (2012) Changes in posterior condylar offset after total knee arthroplasty cannot be determined by radiographic measurements alone. J Arthroplasty 27:1155–1158
Acknowledgments
The authors acknowledge Mrs. Janina Tubby for her assistance in preparation of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagai, K., Muratsu, H., Matsumoto, T. et al. Influence of intra-operative parameters on postoperative early recovery of active knee flexion in posterior-stabilized total knee arthroplasty. International Orthopaedics (SICOT) 37, 2153–2157 (2013). https://doi.org/10.1007/s00264-013-2018-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2018-y