Abstract
Recently, we developed a new tensor for total knee arthroplasty (TKA) procedures enabling soft tissue balance assessment throughout the range of motion while reproducing post-operative joint alignment with the patello-femoral (PF) joint reduced and the tibiofemoral joint aligned. Using the tensor with a computer-assisted navigation system, we investigated the relationship between various intra-operative joint gap values and their post-operative flexion angles. An increased value during the extension to flexion gap and a decreased value during the flexion to deep flexion gap with PF joint reduced, not everted, showed an inverse correlation with post-operative knee flexion angle, not pre-operative flexion angle. In conclusion, understanding the characteristics of joint gap kinematics in posterior-stabilized TKA under physiological and reproducible joint conditions may enable the prediction of the post-operative flexion angle and help to determine the appropriate intra-operative joint gap.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most important goals of TKA is to improve the functional range of flexion to the minimum 90° flexion that is required for normal daily activities. Factors influencing range of flexion after TKA can mainly be classified as intra-capsular and extra-capsular factors. Among extra-capsular factors the importance of pre-operative motion for post-operative results has been previously recognized [1–5]. Similarly, we reported that pre-operative tightness of the extensor mechanism was an important factor for decreasing the post-operative knee flexion angle [6]. On the other hand, intra-capsular factors, including implant design, ligament balancing, flexion–extension gap balance, height of joint line, and patella resurfacing have been also discussed by many authors [7–12]. Among such factors, although soft tissue balancing has been recognized as the essential surgical intervention for improving the outcome of TKA [13, 14], the direct relationship between soft tissue balance and post-operative outcomes has never been clarified. As another concept of joint condition, posterior condylar offset has recently been described as a determinant for flexion [15–17]. A mean reduction in flexion of 12° was reported to be found with every 2 mm decrease in offset [15]. Although posterior condylar offset is thought to be related to flexion gap, this relationship has not been discussed.
In recognition of this, we introduced a CT-free navigation system and have already reported a significant improvement in the accuracy of implantations in relation to the mechanical axis in our patient population [18, 19]. In addition, we used a new tensor enabling soft tissue balance assessment throughout the range of motion while reproducing post-operative joint alignment with the patellofemoral (PF) joint reduced, and the tibiofemoral joint aligned [20] using the CT-free navigation system to clarify intra-operative knee joint kinematics under physiological condition and their relevancy for post-operative outcomes. We also recently clarified the characteristics of joint gap kinematics in posterior-stabilized (PS) TKA under physiological and reproducible joint conditions [18] again using the tensor with a computer-assisted navigation system. In the present study, we focused on the value of the tensor with a computer-assisted navigation system in improving clinical outcomes by investigating the relationship between various intra-operative joint gap values and the post-operative flexion angle. This is the first report trying to describe direct evidence of the influence of the intra-operative joint gap on post-operative knee flexion angles in patients undergoing PS TKA.
Materials and methods
The subjects were 25 consecutive patients (25 osteoarthritic knees) who underwent primary PS TKA between October 2002 and May 2003. Those with valgus deformity and severe bony defects were excluded. The patient population comprised 25 women with a mean age of 71.5 ± 7.3 years. The average coronal plane alignment was 8.2 ± 7.2° in minimal varus pre-operatively. Surgeries were performed by the same senior author (N.T.) using PS TKA (PFC Sigma, DePuy Inc., Warsaw, USA). In all cases, the CT-free navigation system (Vector Vision®, Brain LAB, Heimstetten, Germany) was used to obtain the accuracy of implantations with a standardized navigated TKA technique [15], and to measure the accurate flexion angle of the knee during the intra-operative joint gap measurement together with the newly developed tensor.
Surgical procedure
An air tourniquet was inflated with 280 mmHg in all cases during surgery. The knees were exposed with a medial parapatellar arthrotomy, and the surgeon fixed the classical cutting block to the desired orientation guided by the navigation system before the bony resection. The posterior cruciate ligament was sacrificed at the beginning of the procedure. The proximal tibial osteotomy was perpendicular to the tibial axis in the coronal plane with 3° posterior inclination in the sagittal plane. The tibial bony cut was made at 10 mm below the least compromised articular cartilage at the lateral tibial plateau. After the osteotomy, bony defect at the eroded medial tibial plateau was not observed in any cases. Following the bone resections, osteophytes were removed, the posterior capsule was released from the posterior aspect of the femur, and then, a ligament imbalance in the coronal plane was corrected using the same spacer block at knee extension by appropriate soft tissue releases for the medial structures of the knee.
Intra-operative measurement with a new TKA tensor
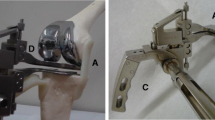
We have previously demonstrated the basic design of the new TKA tensor [17]. The new tensor consists of three parts: upper seesaw plate, lower platform plate and extra-articular main body. Two plates are connected to the extra-articular main body by the offset connection arm through medial parapatellar arthrotomy, which allows the PF joint reduction during the measurement. The platform plate is fixed to the center of proximal tibia after the osteotomy. The seesaw plate has a post at the center proximally to fit the inter-condylar space and the cam of the femoral trial prosthesis of PS TKA. This post and cam mechanism controls the tibiofemoral translation in the coronal and sagittal planes, reproducing the joint constraint and alignment after the prostheses are implanted. This combination of the tensor and femoral trial prosthesis enables soft tissue balance measurement throughout the range of motion, which is also affected by the placement and geometry of the implanted prosthesis (Fig. 1). The surgeon can evaluate soft tissue balance under a constant joint distraction force between the seesaw plate and the platform plate from 30 lb. (13.6 kg) to 80 lb. (36.3 kg), using a specially made torque drive. In the preliminary in vitro experiment, the error for joint distraction force was demonstrated to be within ±3%.
New TKA Tensor (antero-lateral view). The new tensor consists of an upper seesaw plate, lower platform plate, and an extra-articular main body. Two plates are connected to the extra-articular main body by the offset connection arm through medial parapatellar arthrotomy, which allows PF joint reduction during measurement. The relationship between the tensor and trial femoral prosthesis allows joint gap measurement throughout the full range of motion
After all bony resections and soft tissue releases were completed appropriately using a spacer block, the tensor was fixed to the proximal tibia and the femoral trial prosthesis was fitted. The joint distraction force was set at 40 lb. (18.1 kg), because the joint gap at full extension with 40 lb. of joint distraction force corresponded most closely to the insert thickness in the preliminary clinical study. The joint distraction force was loaded several times until the joint gap maintained a certain value to reduce the error due to the creep elongation of the surrounding soft tissues. Joint gap assessments were carried out at four different knee flexion angles of 0° (extension), 45° (mid-range flexion), 90° (flexion) and 135° (deep flexion), which were monitored by the navigation system. The joint gap (mm) was measured first with patella everted as performed with conventional tensors and then with the PF joint reduced. For the soft tissue balance measurement with the PF joint reduced, a patellar trial prosthesis was inserted, and the medial parapatellar arthrotomy was repaired by temporary stitches both proximally and distally to the offset connection arm of the tensor. During the measurement, an assistant surgeon held the thigh to align the knee in the sagittal plane in an attempt to eliminate the external load on the knee at each flexion angle.
Examined parameters
Before and 2 years after surgery, knee flexion angles were evaluated for each patient. Intra-operative joint gaps with both PF joint reduced and everted were assessed at extension gap (0°), mid-range gap (45°), flexion gap (90°), and deep flexion gap (135°). Each value of joint gap, the PF joint reduced and everted, was compared between each knee flexion angle. Each joint gap value was compared between the PF joint reduced and everted.
According to joint gap kinematics (Fig. 1), various altered values of the intra-operative joint gap were calculated as the value of the PF joint reduced and everted joint gap; 135–90°, 135–45°, 135–0°, 90–45°, 90–0°, and 45–0°. Each joint gap change value was used to assess the correlation between the pre- and post-knee flexion angle.
Posterior femoral condylar offset was evaluated for each patient on post-operative lateral radiographs by measuring the maximum thickness of the posterior condyle projected posteriorly to the tangent of the posterior cortex of the femoral shaft. Posterior condylar offset was used to assess the correlation with each joint gap change value.
Statistical analysis
All values were expressed as mean ± standard error of the mean (SE). The results were analyzed statistically using a statistical software package (Statview 5.0, Abacus Concepts Inc, Berkeley, CA, USA). The comparisons of the joint gaps among different flexion angles were done using the repeated measures analysis of variance (ANOVA). Post hoc analysis was performed by Fisher’s PLSD test. The joint gap was, respectively, compared between patellar everted and reduced using the paired Student’s t test. Correlations among each parameter were analyzed using linear regression. Differences and correlations of P < 0.05 were considered statistically significant.
Results
Analysis of feasibility and validity of the measurement
No displacement of the tensor from the tibia was observed during measurements. The average time required for measurement was 12.4 ± 2.1 min. The mean differences between repeated measurements for the joint gap were 0.11 mm (95% confidence interval, −0.6 to 0.28 mm). The accuracy of this measurement was estimated to be ±0.3 mm in the joint gap.
Examined parameters
The follow-up duration was 25.1 ± 0.3 months and no patient was lost during follow-up evaluation. Pre- and post-operative knee flexion angle averaged 113.7 ± 2.3° and 118.8 ± 2.3°, respectively. Pre-operative flexion angle was positively correlated with post-operative flexion angle (R = 0.407, P = 0.017), consistent with the previous reports [1–5]. Posterior condylar offset was 26.8 ± 0.7 mm. Post-operative flexion angle was positively correlated with posterior condylar offset (R = 0.460, P = 0.028), consistent with the previous report [15].
Average joint gaps were 10.6, 16.4, 19.6, and 21.7 mm with the patella everted, and 10.7, 16.8, 16.9 and 11.1 mm with the patella reduced at 0, 45, 90 and 135° of flexion, respectively (Table 1). There were significant increases in the joint gap during the initial 45° of knee flexion with both the patellar everted and reduced. In the measurement of patellar eversion, the joint gap continuously showed significant increases during knee flexion of more than 45° of flexion. In contrast, the joint gap decreased during knee flexion of more than 90° with the patella reduced. Significantly lower gaps were found at 90° and 135° of flexion with PF joint reduction compared to those with patella everted (Fig. 2).
Joint gap kinematics in PS TKA. The average joint gap increased during knee flexion from full extension to 45° of flexion, changing to decrease during deep knee bend with PF joint reduction. In contrast, the joint gap with the patellar eversion continuously showed a significant increase even with more than 60° of flexion. (†† P < 0.01 vs. patellar eversion)
Average joint gap changes were 2.1, 5.3, 11.3, 3.2, 9.2 and 6.0 mm with the patella everted, and −5.8, −5.7, 0.4, 0.1, 6.2 and 6.1 mm with the patella reduced at each range of motion between 135–90, 135–45, 135–0, 90–45, 90–0 and 45–0° of flexion, respectively (Table 2).
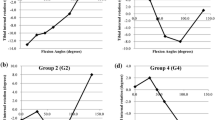
Correlation between each joint gap change value and knee flexion angle
Joint gap change value (90–0°) (R = −0.484, P = 0.019) with PF joint reduced, not everted, showed inverse correlation with post-operative knee flexion angle (Fig. 3a). It is of note that joint gap change value (135–90°) by reducing PF joint (R = 0.51, P = 0.013) showed positive correlation with post-operative knee flexion angle (Fig. 3b). However, there were no correlations in all other pairings between joint gap change value and flexion angle. Thus, all significant correlations were limited to the knee condition with PF joint reduced.
Correlation between joint gap change value with PF joint reduced and post-operative knee flexion angle. a Joint gap change value (90–0°) with PF joint reduced showed inverse correlation with post-operative knee flexion angle. b Joint gap change value (135–90°) by reducing PF joint showed positive correlation with post-operative knee flexion angle
Correlation between joint gap change value and posterior condylar offset
Joint gap change value (90–0°) (R = −0.62, P = 0.002) with PF joint reduction, not everted, showed inverse correlation with posterior condylar offset (Fig. 4). However, there were no correlations in all the other pairings between offset and joint gap change value.
Discussion
Appropriate alignment of knee implants and soft tissue balance are essential for the success of TKA [21–23]. The goal of TKA is to achieve a stable and well-aligned tibiofemoral and PF joints. Recently, computer-assisted and robot-assisted surgeries have been developed and reported to improve the accuracy of osteotomies in TKA [24–26]. We similarly introduced a CT-free navigation system and have already reported that the navigation system allowed a significant improvement in the accuracy of implantations in relation to the mechanical axis in our patient population [18, 19]. In contrast, the management of soft tissue balance during surgery remains difficult, leaving it much to the surgeon’s feel and experience. In fact, although we attempted to get a good alignment balancing during implantation in these series, the measurement resulted in a mean imbalance of 9 mm with the patellar everted between 0 and 90° of flexion. To assess detailed soft tissue balancing and to overcome the imbalance in the future, we developed a new tensor for TKA procedures enabling soft tissue balance assessment throughout the range of motion while reproducing post-operative joint alignment with the PF joint reduced and the tibiofemoral joint aligned [17]. Although soft tissue balancing has been recognized as an essential surgical intervention for improving the outcomes of TKA [13, 14], the direct relationship between soft tissue balance and post-operative outcomes has never been clarified. Using the tensor with a computer-assisted navigation system, in the previous study, we first evaluated and clarified the characteristics of joint gap kinematics reproducing the joint condition most relevant to that after PS TKA [27]. Three phases were distinguishable during knee motion. The joint gap after PS TKA is considered to be affected by tension in the posterior joint structures and the extensor mechanisms of the knee during full extension and deep flexion, respectively. Therefore, in the present study, we aimed to clarify its clinical value and relevancy to outcome by focusing on the post-operative flexion angle.
In the present study, the results showed significant correlation between some of the parameters of joint gap change value and post-operative flexion angle, not with the PF joint everted but with the PF joint reduced. The results indicate that the joint condition with the PF joint reduced is more stable and reliable than that with the PF joint everted, revealing that soft tissue balance assessment with the PF joint reduced may have the potential to help predict post-operative outcome.
The data analysis included some useful information directly relevant to the post-operative clinical setting. Joint gap value during 90° to 0° flexion angle with PF joint reduced showed inverse correlation with post-operative knee flexion angle. In our patient population, a larger flexion gap led to a poorer flexion angle. We thus speculated that an enlarged flexion gap may be related to a larger posterior bone resection. As we expected, there was an inverse correlation between the joint gap change value (90–0) and posterior condylar offset. These results may indicate that a smaller posterior condylar offset leads to a larger flexion gap, resulting in restriction of flexion angle. Although appropriate balancing of the flexion and extension gap has been recognized as a key procedure in TKA [28], posterior cruciate ligament resection leads to an increase in the size of the flexion gap [29–31]. Even if this intra-operative assessment post-resection of bone shows a larger flexion gap than expected, the size of the femoral component cannot be altered in any of the present designs of implants for primary TKA. In the future, this suggests a need for a femoral component that can change size up after the bone is resected.
In addition, a decreased joint gap value during 90° to 135° flexion angle by reducing the PF joint showed an inverse correlation with the post-operative knee flexion angle. These results indicate that a larger tightness of the extensor mechanism including PF joint leads to a poorer knee flexion angle. Many factors influencing the degree of flexion after TKA have been investigated, and the importance of pre-operative motion for post-operative results is already recognized. As the previous reports shows, the pre-operative flexion angle is positively correlated with post-operative flexion angle. However, the present results indicate that the intra-operative assessment of joint gap under physiological conditions with the PF joint reduced and the tibiofemoral joint aligned is one of the factors that can predict the post-operative flexion angle and help improve the surgical technique so that appropriate soft tissue balance is achieved.
We performed an intra-operative assessment of joint gap kinematics using our new tensor in PS TKA performed with a navigation system. We clarified that the intra-operative joint gap kinematic assessment with the PF joint reduced has the possibility to predict the post-operative flexion angle and thus allows evaluation of surgical technique throughout the range of knee motion. This may lead to improved functional outcomes after TKA. Additionally, we believe that this intra-operative joint gap kinematics measurement under physiological and reproducible joint conditions can provide more useful information for prosthetic design and selection, which could compensate for joint gap discrepancy.
References
Anouchi YS, McShane M, Kelly F Jr, Elting J, Stiehl J (1996) Range of motion in total knee replacement. Clin Orthop Relat Res 331:87–91
Lizaur A, Marco L, Cebrian R (1997) Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br 79-B:626–629
Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75-B:950–955
Parsley BS, Engh GA, Dwyer KA (1992) Preoperative flexion. Dose it influence postoperative flexion after posterior-cruciate-retaining total knee arthroplasty? Clin Orthop Relat Res 275:204–210
Ritter MA, Stringer EA (1999) Predictive range of motion after total knee replacement. Clin Orthop Relat Res 143:115–119
Matsumoto T, Tsumura N, Kubo S, Shiba R, Kurosaka M, Yoshiya S (2005) Influence of hip position on knee flexion angle in patients undergoing total knee arthroplasty. J Arthroplasty 20:669–673
Dennis DA (2001) Problems after knee arthroplasty. The stiff total knee arthroplasty: causes and cures. Orthopedics 24:901–902
Harvey IA, Barry K, Kirby SPJ, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75-B:950–955
Kawamura H, Bourne RB (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci 6:248–252
Schurman DJ, Matityahu A, Goodman SB, Maloney W, Woolson S, Shi H, Bloch DA (1998) Prediction of postoperative knee flexion in Insall-Burstein ll total knee arthroplasty. Clin Orthop Relat Res 353:175–184
Schurman DJ, Parker JN, Orstein D (1985) Total condylar knee replacement. A study of factors influencing range of motion as late as two years after arthroplasty. J Bone Joint Surg Am 67-A:1006–1014
Joshi AB, Lee CM, Markovic L, Murphy JCM, Hardinge K (1994) Total knee arthroplasty after patellectomy. J Bone Joint Surg Br 76-B:926–929
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002). Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84-B:50–53
Victor J, Bellemans J (2006) Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res 17 August 2006 [Epub ahead of print]
Kim YH, Sohn KS, Kim JS (2005) Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am 87-A:1470–1475
Matsumoto T, Tsumura N, Kurosaka M, Muratsu H, Kuroda R, Ishimoto K, Tsujimoto K, Shiba R, Yoshiya S (2004) Prosthetic alignment and sizing in computer-assisted total knee arthroplasty. Int Orthop 28:282–285
Matsumoto T, Tsumura N, Kurosaka M, Muratsu H, Yoshiya S, Kuroda R (2006) Clinical values in computer-assisted total knee arthroplasty. Orthopedics 29:1115–1120
Muratsu H, Tsumura N, Yamaguchi M, Mizuno K, Kuroda R, Harada T, Yoshiya S, Kurosaka M (2003) Patellar eversion affects soft tissue balance in total knee arthroplasty. Trans Orthop Res Soc 28:242
Dorr LD, Boiardo RA (1986) Technical consideration in total knee arthroplasty. Clin Orthop Relat Res 205:5–11
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Insall JN, Tria AJ, Scott WN (1979) The total condylar knee prosthesis: the first 5 years. Clin Orthop Relat Res 145:68–77
Siebert W, Mai S, Kober R, Heeckt PF (2002) Technique and first clinical results of robot-assisted total knee replacement. Knee 9:173–180
Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomized study. J Bone Joint Surg Br 85-B:830–835
Stulberg SD, Loan P, Sarin V (2002) Computer-assisted navigation in total knee replacement: Results of an initial experience in thirty-five patients. J Bone Joint Surg Am 84-A:90–98
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2006) Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng 128(6):867–871
Matsueda M, Gengerke TR, Murphys M (1999) Soft tissue release in total knee arthroplasty. Clin Orthop Relat Res 366:264–273
Bottros J, Gad B, Krebs V, Barsoum WK (2006) Gap balancing in total knee arthroplasty. J Arthroplasty 21(4 Suppl 1):11–15
Mihalko WM, Krackow KA (1999) Posterior cruciate ligament effects on the flexion space in total knee arthroplasty. Clin Orthop Relat Res 360:243–250
Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y (2001) Effects of posterior cruciate ligament resection on tibiofemoral joint gap. Clin Orthop Relat Res 391:210–217
Acknowledgments
The authors acknowledge Mrs. Janina Tubby for her assistance in preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matsumoto, T., Mizuno, K., Muratsu, H. et al. Influence of intra-operative joint gap on post-operative flexion angle in osteoarthritis patients undergoing posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthr 15, 1013–1018 (2007). https://doi.org/10.1007/s00167-007-0331-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0331-y