Abstract
Purpose
Both coronal and sagittal laxity of well-functioning knees after total knee arthroplasty (TKA) was examined, and the correlations between the joint laxity and the clinical outcomes were analyzed to clarify the adequate joint laxity for the prosthesis, and the relationship between the laxity and the outcomes.
Methods
Forty well-functioning TKA knees with a high-flexion posterior-stabilized (PS) prosthesis were studied. All patients were diagnosed as having osteoarthritis with varus deformity and were followed up for 2 years or more. The coronal and sagittal laxity was assessed at extension and flexion, and the correlations between the joint laxity and the clinical outcomes were evaluated.
Results
The varus and valgus laxity averaged 5.6 ± 1.8° and 3.6 ± 1.2° at 10° knee flexion, and 7.4 ± 5.1° and 3.6 ± 2.7° at 80° knee flexion, respectively, and the AP laxity at 30° and 75° knee flexion averaged 8.7 ± 3.6 mm and 6.6 ± 2.3 mm, respectively. Knee flexion angle correlated with the joint laxity, while the other outcomes including patient-reported pain and instability were adversely affected by the greater laxity.
Conclusions
This study exhibited the importance of consistent medial laxity both at extension and flexion, which averaged 3.6°. Care should be taken to maintain the medial stability and to obtain adequate laxity both at extension and flexion during surgery. A few degrees of medial tightness can be allowed to achieve excellent clinical results after TKA for preoperative varus knees.
Level of evidence
Therapeutic study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As native knees have physiological laxity [14], knees with total knee arthroplasty (TKA) need to have joint laxity to achieve proper function and to provide comfort [8]. To obtain deep flexion after surgery, a slightly greater gap at knee flexion compared with extension is essential [20]. While to obtain full extension, a tight joint gap in extension should be avoided during surgery [13, 20]. On the other hand, midflexion instability is one of the problems in TKA [4, 16], and too much laxity causes inferior functional outcome and instability [16, 17], which would lead to failure of the TKA [2, 15, 16]. Obtaining the optimum joint laxity in TKA could further improve the satisfaction of TKA, which is relatively low compared with that of total hip arthroplasty [1].
The relation between joint laxity and clinical outcomes after TKA has been studied; however, desirable laxity for TKA knees is still unclear. In the coronal plane, each varus and valgus laxity of about 5° with a total laxity of less than 10° in both extension and flexion was reported to be adequate to allow good long-term results of TKA [24]. The medial joint stability and the lateral joint laxity were reported to be important to obtain better clinical outcome [7, 18]. However, the correlations between coronal joint laxity and patient-reported outcomes have not always been detected [12]. In the sagittal plane, moderate anteroposterior (AP) laxity between 5 and 10 mm at 75° was shown to be desirable in terms of knee flexion and Knee Society Score (KSS) [6]. Another study reported that the AP laxity at 60° correlated with patient-reported pain [10]. However, similar to coronal laxity, the correlations between sagittal laxity and patient-reported outcomes have not always been detected [5]. Furthermore, both coronal and sagittal laxity have rarely been studied at the same time [3, 23]. The ideal laxity after TKA has still not been elucidated, and the influence of joint laxity on clinical outcomes should be explored more.
Therefore, the purpose of this study was (1) to examine both the coronal and sagittal laxity of the TKA knees with good function, and (2) to analyze the correlation between the joint laxity and clinical outcomes including patient-reported outcomes in order to clarify the joint laxity of the well-functioning knees, and the relationship between the laxity and the outcomes. It was assumed that the TKA knees with good function including those with wide range of knee motion would show adequate coronal and sagittal laxity in extension and flexion, while increasing joint laxity would reversely affect some of the clinical outcomes because of the instability.
Materials and methods
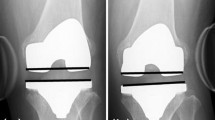
A total of 40 well-functioning knees in 20 patients who underwent bilateral TKA using a high-flexion posterior-stabilized (PS) prosthesis (ACTIYAS, Kyocera, Kyoto, Japan) were studied. Patients with bilateral TKA were selected to obtain similar conditions. In patients with unilateral TKA, the contralateral knee condition varies from mild to severe deformity with or without TKA, which would affect the clinical outcomes. The prosthesis used in this study allows consistent femoral rollback and tibial rotation (Fig. 1) [19]. All patients were diagnosed as having osteoarthritis and were followed up for 2 years or more. Eighty-six primary bilateral TKAs were performed with this prosthesis from January 2011 to June 2013. Of these 86 patients, postoperative well-functioning knees with extension deficit of 2° or less, flexion of 130° or more, and a Knee Society Function Score (FS) of 75 or more were selected as candidates for this study. Patients with a history of high tibial osteotomy, preoperative valgus deformity, hip diseases, and patients who lived far away from our institution (Tokyo Medical and Dental University Hospital) and took about 3 h or more to arrive were excluded. Adapting the above-mentioned conditions resulted in 35 patients remaining. All 35 patients were asked to participate in this study, and 20 of the 35 patients accepted our offer. The patients’ age averaged 74 ± 7 years at surgery with 17 females and 3 males (ratio of female, 85%). The patient height and body mass index averaged 152 ± 7 cm and 25 ± 4 kg/m2, and the follow-up period after arthroplasty averaged 3.2 ± 0.9 years.
Surgical procedures and postoperative management
The same surgical procedures were performed by or under the direction of three surgeons (TM, IS, and TW) on the knee team, and the same postoperative management was applied for all patients. A midvastus approach and anatomical bone cuts were applied. The distal femur was cut perpendicular to its mechanical axis in the coronal plane and perpendicular to its distal femoral axis in the sagittal plane with intramedullary instruments, removing the same amount of thickness as the femoral component. The proximal tibia was cut perpendicular to its mechanical axis in the coronal plane and with a 5°–7° posterior tibial slope in the sagittal plane using extramedullary instruments. The posterior femoral condyles were cut parallel to the femoral epicondylar axis and perpendicular to the Whiteside line with 3°–5° external rotation from the posterior condylar line. The medial and posterior soft tissues were released to achieve adequate balance while allowing slight tightness in the medial side. The components were fixed with cement, and no drainage tube was used [21]. Full weight bearing, quadriceps muscle setting, and range of motion exercises were started the day after surgery, and gait exercises were encouraged 3–4 days after surgery.
Evaluation of the coronal and sagittal laxity
The coronal laxity was assessed at extension and flexion on the stress radiographs at follow-up (Fig. 2). The varus and valgus laxity at extension was measured using a Telos device (Fa Telos, Medizinisch-Technische GmbH, Griesheim, Germany) while the patient laid on a bed (Fig. 2a–d) [9, 12, 14, 24]. The varus and valgus laxity at knee flexion was measured using a hand-held dynamometer (μTas F-1, Anima Corp., Tokyo, Japan), while the patient was seated on a table made of styrofoam (Fig. 2e–h) [14, 24]. A single examiner (TW) measured the coronal laxity for all knees. To evaluate the intra- and inter-observer reproducibility, the measurements were taken three times by the examiner and once by two other examiners (orthopedic surgeons) on the ten randomly selected knees. The intraclass correlation coefficients for intra- and inter-observer reproducibility were 0.98 and 0.97, respectively.
Coronal laxity measurements at extension and flexion on the stress radiographs. The varus (a, d) and valgus (b, c) laxity at 10° knee flexion was measured using a Telos device with an applying force of 150 N. The right (a, b) and left knees (c, d) are shown. The varus (f, g) and valgus (e, h) laxity at 80 °knee flexion was measured using a hand-held dynamometer with an applying force of 100 N. The right (e, f) and left knees (g, h) are shown
The sagittal laxity at 30° and 75° knee flexion was evaluated using a KT-1000 arthrometer (MEDmetric, San Diego, CA, USA) at the follow-up. To assess the AP laxity, 133 N was applied for anterior translation while 89 N was applied for posterior translation [5, 11] both at 30° and 75° knee flexion [5, 11]. A single examiner (TW) measured the AP laxity 3 times for all knees, and the averaged anterior and posterior translations were added to obtain AP laxity at each knee flexion.
Evaluation of clinical outcomes including patient-reported outcomes
Clinical outcomes including patient-reported outcomes were evaluated at the follow-up. The knee extension and flexion angle measured by goniometer, KSS and FS, and femorotibial angle (FTA) on the standing knee radiographs were assessed. As patient-reported outcomes, “patient overall assessment”, which ranged from 0 to the perfect score of 100, were obtained. “Pain during gait on flat surface”, “pain at rest”, “pain at first gait in the morning”, “pain during stair gait”, and “instability during stair gait” were also evaluated using numerical rating scale (NRS), which ranged from 0 to the perfect score of 10. Moreover, the 2011 Knee Society Questionnaire (2011 KSQ) was applied.
This study was approved by the institutional review board of the Tokyo Medical and Dental University under approval number M2000-1252.
Statistical analysis
Correlations between joint laxity and clinical outcomes including patient-reported outcomes were estimated using the Spearman correlation coefficient. To compare the joint laxity, the Wilcoxon signed rank test was applied. Statistical software, SPSS version 21 (IBM, Armonk, NY) was used for analyses, and a probability value of less than 0.05 was considered to be significant.
The power analysis indicated 40 knees had 77% power (1 − β) for the correlation between clinical outcomes and joint laxity using an effect size of 0.4.
Results
Coronal and sagittal laxity, and clinical outcomes
The varus and valgus laxity at 10° knee flexion averaged 5.6 ± 1.8° and 3.6 ± 1.2°, respectively, and the varus and valgus laxity at 80° knee flexion averaged 7.4 ± 5.1° and 3.6 ± 2.7°, respectively (Fig. 3a, b). The varus + valgus laxity averaged 9.2 ± 2.4° at 10° knee flexion and 11.0 ± 5.9° at 80° knee flexion, while the varus − valgus laxity averaged 1.9 ± 1.9° at 10° knee flexion and 3.8 ± 5.7° at 80° knee flexion. The AP laxity at 30° and 75° knee flexion averaged 8.7 ± 3.6 mm, 6.6 ± 2.3 mm, respectively (Fig. 3c, d). Clinical outcomes including patient-reported outcomes at the follow-up are shown in the second column of Table 1.
Correlations between the joint laxity and clinical outcomes
The knee flexion angle and the patient-reported pain and instability correlated with the joint laxity, while some other outcomes negatively correlated with the joint laxity (Table 1). Detected positive correlations included those between the flexion and the varus + valgus laxity at 10° knee flexion (Fig. 4a) or the AP laxity at 30° knee flexion (Fig. 4b), and between the “pain during gait on flat surface” (Fig. 4f) or “instability during stair gait” (Fig. 4g) and varus laxity at 80° knee flexion. Detected negative correlations included those between the KSS and the varus laxity at 80° knee flexion (Fig. 4c), between the “patient overall assessment” and valgus laxity at 10° knee flexion (Fig. 4d) or varus + valgus laxity at 10° knee flexion (Fig. 4e), between the “patient satisfaction” and varus − valgus laxity at 80° knee flexion (Fig. 4h), and between the “patient expectation” and varus laxity at 80° knee flexion (Fig. 4i).
Scatter graphs illustrating correlations. Correlations between flexion and the varus + valgus laxity at 10° knee flexion (a) or anteroposterior laxity at 30° knee flexion (b), the Knee Society Score and the varus laxity at 80° knee flexion (c), “patient overall assessment” and the valgus laxity at 10° knee flexion (d) or the varus + valgus laxity at 10° knee flexion (e), “pain during gait on flat surface” and the varus laxity at 80° knee flexion (f), “instability during stair gait” and the varus laxity at 80° knee flexion (g), “patient satisfaction” and the varus − valgus laxity at 80° knee flexion (h), and “patient expectation” and the varus laxity at 80° knee flexion (i) are shown
Discussion
The most important findings of this study were that the valgus laxity which averaged 3.6° was consistent at extension and flexion in these high-flexion PS-TKA knees with good function, and to obtain greater flexion and better patient-reported outcomes, adequate coronal and sagittal laxity was needed. As it was hypothesized, increasing joint laxity reversely affected some of the clinical outcomes because of the instability.
Several limitations of this study should be acknowledged. The first limitation is the selection bias. Only the selected knees with postoperative good range of motion were analyzed, which would have greater laxity compared to the knees with less range of motion. The knees with less range of motion would show less laxity. Moreover, if the knees with some extension deficit had been analyzed, correlations between the joint laxity and the extension angle might have been detected. However, to clarify the optimum joint laxity of the TKA knees with this type of prosthesis, well-functioning knees should be studied. Second, our results are implant-design dependent. The knees with high-flexion PS prosthesis with a relatively flat symmetrical tibial insert were analyzed in this study, and the results may not be generalized to the other designs including cruciate-retaining or cruciate-sacrificing prostheses [22]. Third, similar to the second limitation, the results in this study are surgical-technique dependent. Independent bone cuts based on the anatomical landmark, and medial soft tissue release to achieve adequate balance while allowing slight tightness in the medial side were applied. Different surgical procedures such as dependent bone cutting using a gap technique or more aggressive medial soft tissue release pursuing a perfect rectangular gap would lead to different results. Finally, the number of the cohort is small. A larger cohort may reveal more correlations between the clinical outcomes and joint laxity.
The coronal laxity in this study on high-flexion PS-TKA knees with good function suggested the ideal laxity of 5.6° in varus and 3.6° in valgus at 10° knee flexion, and 7.4° in varus and 3.6° in valgus at 80° knee flexion. The results in the current study are comparable to those reported by previous studies using different prostheses (Table 2). The coronal laxity in the current study demonstrated significantly greater varus laxity compared with the valgus laxity both at 10° and 80° knee flexion. The greater varus laxity was also reported in the normal knee [14]. Yoshihara et al. [24] noted the ideal coronal laxity of 5° in each direction with a total laxity of less than 10° in both extension and flexion for good long-term results of TKA. The laxity in this study was slightly greater than that in their study, and one of the possible explanations for this is the better knee flexion angle of the cohort in this study (average 137° vs 114°).
The results in this study suggested that the coronal laxity to some extent is important to obtain better flexion, although some other factors were adversely affected by the greater laxity. The valgus laxity at 10° knee flexion did not correlate with the flexion angle, but it did correlate with “pain at rest”, and it negatively correlated with “patient overall satisfaction”. Moreover, when the scatter graphs of flexion and varus + valgus laxity at 10° knee flexion are closely examined, three knees showed less flexion in spite of their great laxity (Fig. 4a), which suggests too much coronal laxity would adversely affect flexion angle. At 80° knee flexion, greater varus laxity also was related to the inferior clinical outcomes. These findings suggested that the greater coronal laxity, especially valgus laxity at 10° knee flexion and varus laxity at 80° knee flexion should be avoided.
The sagittal laxity in this study on high-flexion PS-TKA knees with good function suggested the ideal laxity of 8.7 and 6.6 mm at 30° and 75° knee flexion, respectively. The results in the current study are comparable to those reported by previous studies using different prostheses (Table 3). Nabeyama et al. [11] reported that the AP stability increased following PS TKA and was significantly greater than that of normal subjects by an average of 3 years after surgery. This study had a similar follow-up period of 3.2 years. Jones et al. [6] noted that the knees with AP laxity between 5 and 10 mm at 75° knee flexion demonstrated better flexion angle and greater KSS compared to the knees with AP laxity of more than 10 mm. In our study, the averaged AP laxity at 75° knee flexion was in this range, 5 to 10 mm.
The results in this study suggested that the sagittal laxity to some extent is important to obtain better knee flexion, although the KSS and “pain at rest” were adversely affected by the greater laxity. No correlations were found between the AP laxity at 75° knee flexion and the clinical outcomes; however, the AP laxity at 30° knee flexion correlated with some clinical outcomes. The reason for this would be that the AP laxity near extension is more relevant to the clinical outcomes because the knee is mostly used near extension under weight-bearing in daily activities such as standing and walking. Similar to the coronal laxity or even in the higher level, the AP laxity would be a trade-off between the range of motion and other clinical outcomes.
Both coronal and sagittal laxity together, and the correlations of each laxity with the clinical outcomes including patient-reported outcomes were examined, which is one of the strengths of this study. Although both coronal and sagittal laxity is important in TKA, our results suggested that accessing the coronal laxity would be more beneficial than assessing the sagittal laxity because the coronal laxity is more related to the clinical outcomes than the sagittal laxity is. The coronal and sagittal laxity this study showed is an ideal laxity after high-flexion PS-TKA because the cohort was selected from the well-functioning knees with a sufficient follow-up period [11]. The current study provided an optimized joint laxity to obtain excellent clinical results after TKA.
Conclusions
This study exhibited the importance of consistent medial laxity both at extension and flexion, which averaged 3.6°. Care should be taken to maintain the medial stability and to obtain adequate laxity both at extension and flexion during surgery.
Change history
28 May 2019
Unfortunately, the co-author “Hiroki Katagiri’ was omitted in the original publication from the author group. The author name is added here. The original article has been corrected.
References
Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K (2010) Comparing patient outcomes after THA and TsKA: is there a difference? Clin Orthop Relat Res 468:542–546
Calliess T, Ettinger M, Hulsmann N, Ostermeier S, Windhagen H (2015) Update on the etiology of revision TKA—evident trends in a retrospective survey of 1449 cases. Knee 22:174–179
Dejour D, Deschamps G, Garotta L, Dejour H (1999) Laxity in posterior cruciate sparing and posterior stabilized total knee prostheses. Clin Orthop Relat Res 364:182–193
Hino K, Kutsuna T, Watamori K, Kiyomatsu H, Ishimaru Y, Takeba J et al (2017) Varus-valgus stability at 90 degrees flexion correlates with the stability at midflexion range more widely than that at 0 degrees extension in posterior-stabilized total knee arthroplasty. Arch Orthop Trauma Surg 137:1429–1434
Ishii Y, Noguchi H, Takeda M, Sato J, Sakurai T, Toyabe S (2014) In vivo anteroposterior translation after meniscal-bearing total knee arthroplasty: effects of soft tissue conditions and flexion angle. Eur J Orthop Surg Traumatol 24:967–971
Jones DP, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee replacement. J Arthroplast 21:719–723
Kamenaga T, Muratsu H, Kanda Y, Miya H, Kuroda R, Matsumoto T (2018) The influence of postoperative knee stability on patient satisfaction in cruciate-retaining total knee arthroplasty. J Arthroplasty 33:2475–2479
Kuster MS, Bitschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty: a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Jt Surg Br 87:804–808
Matsumoto K, Ogawa H, Yoshioka H, Akiyama H (2017) Postoperative anteroposterior laxity influences subjective outcome after total knee arthroplasty. J Arthroplasty 32:1845–1849
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T et al (2003) Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Nakahara H, Okazaki K, Hamai S, Okamoto S, Kuwashima U, Higaki H et al (2015) Does knee stability in the coronal plane in extension affect function and outcome after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23:1693–1698
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S et al (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M et al (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Petrie JR, Haidukewych GJ (2016) Instability in total knee arthroplasty: assessment and solutions. Bone Jt J 98-B:116–119
Scuderi GR, Deshmane PP (2015) Instability of total knee replacement. In: Hirschmann MT, Becker R (eds) The unhappy total knee replacement. Springer, New York, pp 195–205
Seah RB, Yeo SJ, Chin PL, Yew AK, Chong HC, Lo NN (2014) Evaluation of medial-lateral stability and functional outcome following total knee arthroplasty: results of a single hospital joint registry. J Arthroplasty 29:2276–2279
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H et al (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24:1478–1484
Watanabe T, Muneta T, Koga H, Horie M, Nakamura T, Otabe K et al (2016) In-vivo kinematics of high-flex posterior-stabilized total knee prosthesis designed for Asian populations. Int Orthop 40:2295–2302
Watanabe T, Muneta T, Sekiya I, Banks SA (2013) Intraoperative joint gaps affect postoperative range of motion in TKAs with posterior-stabilized prostheses. Clin Orthop Relat Res 471:1326–1333
Watanabe T, Muneta T, Yagishita K, Hara K, Koga H, Sekiya I (2016) Closed suction drainage is not necessary for total knee arthroplasty: a prospective study on simultaneous bilateral surgeries of a mean follow-up of 5.5 years. J Arthroplasty 31:641–645
Wautier D, Thienpont E (2017) Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1792–1800
Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K (2003) Influence of stability on range of motion after cruciate-retaining TKA. Arch Orthop Trauma Surg 123:1–4
Yoshihara Y, Arai Y, Nakagawa S, Inoue H, Ueshima K, Fujiwara H et al (2015) Assessing coronal laxity in extension and flexion at a minimum of 10 years after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2512–2516
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
TW created the study design, conducted the study, collected, analyzed and interpreted the data, drafted the manuscript and completed the final manuscript. HKo, HKa, KO, YN, TM, IS and TJ conducted the study, collected the data and revised the drafted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of the Tokyo Medical and Dental University.
Informed consent
Written informed consent was obtained from all participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The co-author “Hiroki Katagiri” was omitted in the original publication and updated here.
Rights and permissions
About this article
Cite this article
Watanabe, T., Koga, H., Katagiri, H. et al. Coronal and sagittal laxity affects clinical outcomes in posterior-stabilized total knee arthroplasty: assessment of well-functioning knees. Knee Surg Sports Traumatol Arthrosc 28, 1400–1409 (2020). https://doi.org/10.1007/s00167-019-05500-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05500-8