Abstract
Introduction
Although soft tissue tension during total knee arthroplasty (TKA) has been targeted to achieve equal flexion and extension gaps, such a perfect gap is not always obtained. This study was performed to investigate the impact of difference between flexion and extension gaps on postoperative knee flexion angle.
Materials and methods
We reviewed 107 consecutive TKAs using a J-curve design posterior-stabilized prosthesis. Soft tissue tension was measured intraoperatively using an offset-type tensor under 30 lb force of joint distraction with the patella reduced. All TKAs were performed in a uniform manner including the subvastus approach and without use of a pneumatic tourniquet. We assessed the association between knee flexion angle 1 year after TKA and the difference between flexion and extension gaps using Pearson’s product-moment correlation and multiple regression analysis with age, sex, body mass index, diagnosis, history of diabetes mellitus, preoperative flexion angle, and gap difference as explanatory variables.
Results
The difference between flexion and extension gaps showed a slight negative correlation with postoperative knee flexion angle in univariate analysis (r = − 0.20, 95% CI, − 0.38 to − 0.01, p = 0.04). Multiple regression analysis showed that the gap difference was an independent factor associated with postoperative knee flexion angle (β = − 0.89, 95% CI, − 1.60 to − 0.18, p = 0.01).
Conclusions
The difference between flexion and extension gaps was negatively correlated with postoperative knee flexion angle. Looser flexion gap compared with extension gap should be avoided in J-curve design posterior-stabilized TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appropriate soft tissue balancing is a crucial determinant of clinical outcome after total knee arthroplasty (TKA). Equal width of flexion and extension gaps is ideal for soft tissue balancing during TKA [1, 2]. As surgeons can strictly quantify intraoperative soft tissue balancing using novel devices, recent studies revealed new targets for ideal intraoperative soft tissue balancing [3,4,5].
In posterior cruciate-retaining TKA, larger flexion gap than the extension gap provided better postoperative knee flexion angle compared with equal flexion and extension gaps [3, 4]. However, the appropriate relationship between flexion and extension gaps remains a contentious issue in posterior-stabilized (PS) TKA [5, 6]. Tsukada et al. [6] measured soft tissue balance of 329 consecutive TKAs using single anteroposterior radius PS-TKA prosthesis (Scorpio NRG; Stryker, Mahwah, NJ) in the standardized setting including the subvastus approach, reduced patella, and no use of a pneumatic tourniquet. They reported soft tissue imbalance, such as larger or smaller flexion gap compared with extension gap, was not associated with the postoperative knee flexion angle [6]. Although their measurement of soft tissue balancing was performed stringently, the unique design of the TKA prosthesis could affect the results. The more general J-curve design TKA prosthesis may provide different results because the J-curve design TKA has different in vivo kinematics to the single anteroposterior radius TKA [7].
This study was performed to examine whether the difference in soft tissue tension between flexion and extension gaps would affect postoperative knee flexion angle in the J-curve design PS-TKA. We hypothesized that the postoperative knee flexion angle was correlated with the difference in soft tissue tension between flexion and extension gaps.
Materials and methods
The study was performed after receiving approval from the institutional review board. The inclusion criterion was as follows: patients undergoing primary PS-TKA using a single prosthesis (Persona; Zimmer-Biomet, Warsaw, IN) from September 2016 to January 2018 in the Adult Knee Reconstruction Division of a single general hospital. Persona is J-curve design prosthesis, which has multiple different tangential radius curves in the sagittal plane [8]. The exclusion criterion was primary TKA without use of the Persona. This study focused on the relationship between knee flexion angle 1 year after TKA and intraoperative measurement of bone gap. The range of knee movement was measured using a goniometer at the follow-up visit.
Surgical technique
All surgeries were performed under general anesthesia. All TKAs were performed or supervised by one surgeon (ST). No pneumatic tourniquet was used during the study period. An anterolateral incision was used in all surgeries as positioning the skin incision laterally during knee surgery may reduce disruption of sensation in the anterior aspect of the knee by preserving the branches of the saphenous nerve [9]. The subvastus approach without detaching the vastus medialis was employed as the surgical approach to measure soft tissue tension more strictly than other approaches involving detachment of the vastus medialis.
The measured resection technique was applied to the bone cuts; both tibial and femoral osteotomies were carried out referencing anatomical bony landmarks. In proximal tibia osteotomy, we aimed for the cutting surface to be perpendicular to the tibial axis in both coronal and sagittal planes. The distal femoral osteotomy was made in valgus angulation, which was equal to the angle between the anatomical and functional axes of the femur. In this valgus angle of distal femoral resection, we resected 9 mm of distal femur from the distalmost point of the medial and lateral femoral condyles. For example, if the distalmost point was located at the medial femoral condyle, we resected 9 mm of medial femoral condyle and less than 9 mm of lateral femoral condyle. The thickness of 9 mm was determined by the thickness of the distal femoral component of Persona. We aimed to achieve rotational alignment of the femoral component parallel to the surgical epicondylar axis [10].
We removed osteophytes thoroughly, especially the medial posterior condylar osteophyte [11]. We routinely released the deep layer of the medial collateral ligament. The semimembranosus was released only if we could not resect the posteromedial osteophyte of the tibia without release of the semimembranosus. Other soft tissue, including the superficial layer of the medial collateral ligament or the pes anserinus, was not released during the study period. The thickness of the tibial insert was determined to obtain 0° extension with no medial instability. When full extension was not obtained, we added bone resection of the proximal tibia. As we believed that avoiding elevation of the femorotibial joint line would be one of the most important determinants of the successful TKA applied to the measured resection technique, we did not add a distal femoral bone resection even if the flexion gap was larger than the extension gap. Although the bone resection of proximal tibia does not reduce the gap between flexion and extension, we gave priority to maintain the height of the femorotibial joint line during study period.
Measurement of soft tissue balance
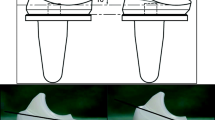
After manually confirming acceptable soft tissue balance, the soft tissue balance was measured at both 0° extension and 90° flexion using an offset-type TKA tensor (Offset Repo-Tensor; Zimmer-Biomet) (Fig. 1). The joint center gap and varus ligament balance at 0° extension and 90° flexion were recorded using the tensor with a distraction force of 30 lb.
Offset-type tensor for measurement of soft tissue balance during total knee arthroplasty. The tensor has upper and lower plates. The central scale indicates the distance between two plates, which is the bone gap. Another scale (arrowhead) indicates the tilting angle of the two plates, which is varus/valgus imbalance. We quantified the bone gap and varus/valgus imbalance with a distraction force of 30 lb using the torque driver attached to the tensor (arrow)
The Offset Repo-Tensor has an offset arm allowing the surgeon to measure the soft tissue balance with the patella reduced. The Offset Repo-Tensor has upper seesaw and lower platform plates. The surgeon lays these two plates on the surfaces of the resected tibia and femur. When these two plates distract the resected surface of the femur from that of the tibia, the distance between the two plates is the joint gap. The tilting angle between the two plates is the varus/valgus imbalance. When the tilting angle shows that medial soft tissue tension is tighter than that on the lateral side, the deviation is defined as varus and is given a negative value [6]. In the case of tighter lateral soft tissue tension compared with the medial soft tissue, the deviation is defined as valgus and given a positive value [6].
Statistical analysis
Firstly, we evaluated the strengths of the relationships between knee flexion angle 1 year after TKA and multiple parameters, including the difference between flexion and extension gaps, preoperative flexion angle, age, sex, body mass index, diagnosis, and history of diabetes mellitus using the Pearson’s product-moment correlation. Secondly, we performed multiple regression analyses to assess the association of knee flexion angle 1 year after TKA with the abovementioned parameters. We presented standardized coefficients (β) and p values. All statistical analyses were performed with R software version 3.4.1. (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Participants
During the study period, a total of 107 PS-TKAs were performed using Persona in our division. Table 1 summarizes the demographic characteristics of the patients. Of the 107 patients, one was lost to follow-up before 1 year after TKA. The remaining 106 TKAs were included in the analysis. The mean knee flexion and extension angles 1 year after TKA were 120° ± 13° and − 3° ± 3°, respectively.
Pearson’s product-moment correlation
Table 2 summarizes the strengths of relationships between knee flexion angle 1 year after TKA and each parameter. The value of the difference between flexion and extension gaps showed a slight negative correlation with postoperative knee flexion angle in univariate analysis (r = − 0.20, 95% confidence interval [CI], − 0.38 to − 0.01, p = 0.04) (Fig. 2). Preoperative flexion angle was the best predictor of postoperative knee flexion angle (r = 0.51, 95% CI, 0.35–0.64, p < 0.01).
Correlation between the values of the difference between flexion and extension gaps showed a slight negative correlation with postoperative knee flexion angle using Pearson’s product-moment correlation. The numerical difference of flexion gap minus extension gap was slightly negatively correlated with postoperative knee flexion angle 1 year after total knee arthroplasty (r = − 0.20, 95% confidence interval [CI], − 0.38 to − 0.01, p = 0.04)
Multiple regression analysis
Table 3 summarizes the impact on knee flexion angle 1 year after TKA calculated by multiple linear regression analysis. The multiple linear regression model included age, sex, body mass index, diagnosis, history of diabetes mellitus, preoperative flexion angle, and difference between flexion and extension gaps (F-statistic = 7.9, p < 0.01, adjusted R2 = 0.33). The difference between flexion and extension gaps was negatively correlated with postoperative knee flexion angle (β = − 0.89, 95% CI, − 1.60 to −0.18, p = 0.01).
Discussion
We found a negative correlation between knee flexion angle 1 year after TKA using a J-curve PS prosthesis and the difference in soft tissue tension between 90° flexion and 0° extension.
Equal width of flexion and extension gaps has been still one ideal soft tissue balance during TKA [6]. However, surgeons recognize that strict quantification of soft tissue balance has prohibited obtaining perfect soft tissue balance. It would be important to determine how the degree of the soft tissue imbalance affects clinical outcome. Matsumoto et al. [5] reported that the difference in flexion and extension gaps measured with the femoral component was negatively correlated with postoperative knee flexion angle in 25 consecutive J-curve PS-TKAs (PFC Sigma; DePuy Synthes, Warsaw, IN). The study had important limitations regarding the small sample size, which disallowed multivariate analysis, including preoperative flexion angle, the best predictor of postoperative knee flexion angle [5]. We sized up the relationship between the difference in flexion and extension gaps and postoperative knee flexion angle and found a negative correlation. The results of the study of Matsumoto et al. and our findings support each other. Although the reason for the paradoxical decrease in the postoperative knee flexion angle due to the large flexion gap was unclear, Matsumoto et al. [5] deduced that large flexion gap was associated with the small posterior condylar offset caused by excess resection of posterior condyle.
This study had several limitations. This study only assessed the relationship between postoperative knee flexion angle and intraoperative bone gap. Recent studies indicated that the intraoperative soft tissue tension could affect general outcome, such as 2011 Knee Society score [12, 13]. However, the results of this study have important implications for both patients and knee surgeons as knee flexion angle is an important concern associated with TKA.
We measured bone gap to quantify the soft tissue tension. The bone gap is the width between resected surfaces of the femur and tibia. Several investigators measured the width between femoral component and resected surface of the tibia as the soft tissue tension [5, 14, 15]. Such measurements can reflect the soft tissue balance after TKA implantation more strictly than the bone gap. However, the impact of bone gap on postoperative outcome would be important as many current surgical techniques to obtain appropriate soft tissue balance are based on bone gap measurements [16].
In conclusion, this study showed a slight negative correlation between the difference between flexion and extension gaps and postoperative knee flexion angle after J-curve design PS-TKA in both univariate and multivariate analyses.
References
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y (2001) Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res 391:210–217
Takayama K, Matsumoto T, Kubo S, Muratsu H, Ishida K, Matsushita T, Kurosaka M, Kuroda R (2012) Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:532–537
Higuchi H, Hatayama K, Shimizu M, Kobayashi A, Kobayashi T, Takagishi K (2009) Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. Int Orthop 33:997–1000
Matsumoto T, Mizuno K, Muratsu H, Tsumura N, Fukase N, Kubo S, Yoshiya S, Kurosaka M, Kuroda R (2007) Influence of intra-operative joint gap on post-operative flexion angle in osteoarthritis patients undergoing posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 15:1013–1018
Tsukada S, Fujii T, Wakui M (2017) Impact of soft tissue imbalance on knee flexion angle after posterior stabilized total knee arthroplasty. J Arthroplasty 32:2399–2403
Tamaki M, Tomita T, Yamazaki T, Yoshikawa H, Sugamoto K (2013) Factors in high-flex posterior stabilized fixed-bearing total knee arthroplasty affecting in vivo kinematics and anterior tibial post impingement during gait. J Arthroplasty 28:1722–1727
Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ (2013) The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46:1351–1357
Tsukada S, Kurosaka K, Nishino M, Hirasawa N (2018) Cutaneous hypesthesia and kneeling ability after total knee arthroplasty: a randomized controlled trial comparing anterolateral and anteromedial skin incision. J Arthroplasty 33:3174–3180
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Baldini A, Scuderi GR, Aglietti P, Chalnick D, Insall JN (2004) Flexion-extension gap changes during total knee arthroplasty: effect of posterior cruciate ligament and posterior osteophytes removal. J Knee Surg 17:69–72
Matsumoto T, Takayama K, Muratsu H, Ishida K, Hashimoto S, Hayashi S, Kuroda R (2018) Relatively loose flexion gap improves patient-reported clinical scores in cruciate-retaining total knee arthroplasty. J Knee Surg 31:573–579
Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y, Furu M, Ito H, Matsuda S (2018) Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138:1143–1150
Matsui Y, Nakagawa S, Minoda Y, Mizokawa S, Tokuhara Y, Kadoya Y (2014) Joint gap measurement in total knee arthroplasty using a tensor device with the same articulating surface as the prosthesis. Arch Orthop Trauma Surg 134:699–705
Minoda Y, Nakagawa S, Sugama R, Ikawa T, Noguchi T, Hirakawa M, Nakamura H (2014) Intraoperative assessment of midflexion laxity in total knee prosthesis. Knee 21:810–814
Sheth NP, Husain A, Nelson CL (2017) Surgical techniques for total knee arthroplasty: measured resection, gap balancing, and hybrid. J Am Acad Orthop Surg 25:499–508
Funding
The authors declare that they did not receive and will not receive any benefits or funding from any commercial party related directly or indirectly to the subject of this article
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsukada, S., Kurosaka, K., Nishino, M. et al. Intraoperative loose flexion gap may restrict postoperative knee flexion after J-curve design posterior-stabilized total knee arthroplasty. Eur J Orthop Surg Traumatol 30, 147–151 (2020). https://doi.org/10.1007/s00590-019-02538-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02538-9