Abstract
Rationale
Despite decades of research, tardive dyskinesia (TD) remains a poorly understood iatrogenic movement disorder with few effective treatments and no known cure. Accordingly, the development of an innocuous strategy to prevent or mitigate antipsychotic (AP)-associated TD would represent an important clinical advance. Supporting evidence for antioxidant (AX)-based treatment regimens can be found in the preclinical literature, where AP-induced vacuous chewing movements (VCMs) in rats are attenuated by the concurrent administration of direct and indirect AXs.
Objectives
Our aim was to review the preclinical literature examining the role of AX-promoting treatments in the prevention of AP-induced VCMs in rats.
Methods
A literature search using Google Scholar and PubMed was performed. Relevant results were qualitatively reviewed.
Results
Studies featuring a variety of naturally occurring and synthetic AX treatments were identified and included in the review. The majority of studies used haloperidol (HAL), a typical AP, to induce VCMs. Studies revealed reduced VCMs in co-treated rats, with favorable changes seen in markers of oxidative stress (OS) and AX status, but were limited by their short durations.
Conclusions
Some preclinical evidence suggests that the inclusion of a naturally occurring and benign AX compound as an adjunct to AP treatment may help guard patients against TD, but additional long-duration studies are needed. This AX-based strategy is further substantiated by accumulating evidence of preexisting OS abnormalities in schizophrenia (SZ).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tardive dyskinesia (TD) is an enduring, potentially irreversible disorder associated with chronic antipsychotic (AP) exposure and characterized by involuntary, stereotyped, and repetitive movements in different body parts (American Psychiatric Association 2013). While it has been suggested that the newer “atypical” APs carry a diminished risk of TD, the magnitude of improvement has been called into question and it remains the case that all APs carry a risk of TD (Remington 2007; Correll and Schenk 2008). Moreover, APs are being used increasingly in other diagnostic categories, such as depression and disruptive behavior disorders (Olfson et al. 2012). Accordingly, developing strategies to reduce AP-related TD remains a priority.
While theories of TD etiology and pathophysiology have been posited, none are considered definitive. Striatal dopamine receptor supersensitivity, γ-aminobutyric acid (GABA) insufficiency, and structural brain abnormalities have long been implicated in TD (Fibiger and Lloyd 1984; Casey 2000; Sarró et al. 2013). Likewise, the potential contributions of AP-induced glutamatergic excitotoxicity, disruption of mitochondrial function, free radical generation, oxidative stress (OS), and neurodegeneration have all been recognized (Cadet and Lohr 1989; Elkashef and Wyatt 1999; Andreassen and Jørgensen 2000). Interestingly, the OS hypothesis can simultaneously accommodate these previously reported dopaminergic, GABAergic, and structural abnormalities in TD (Sachdev 2000). As well, several risk factors for TD (e.g., advanced age, diabetes, drug abuse) are associated with elevated OS (Sohal and Weindruch 1996; West 2000; Yamamoto and Raudensky 2008).
The role(s) of free radicals and OS in TD have been reviewed in detail elsewhere (Elkashef and Wyatt 1999; Sachdev 2000; Lohr et al. 2003). Briefly, APs are thought to increase OS and thereby contribute to neurodegeneration and ultimately the development of TD by the following mechanisms: (1) AP blockade of dopamine receptors leads to a compensatory increase in dopamine synthesis, release, and breakdown; (2) superoxide anions, dopamine quinones, and hydrogen peroxide, all of which are known to promote OS, are produced when excess dopamine undergoes auto-oxidation (forming superoxide anions and quinones) or catabolism by monoamine oxidase B (forming hydrogen peroxide); (3) these events occur in the dopamine-rich striatum, a metabolically active brain region involved in motor function, in the presence of abundant polyunsaturated membrane lipids, oxygen, and transition metal ions such as iron (which can interact with hydrogen peroxide to form the reactive hydroxyl radical); (4) the endogenous antioxidant (AX) system, a collection of enzymes and molecules including superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase/reductase, reduced glutathione (GSH), and vitamins C and E, may become saturated and overpowered by free radicals, leading to neural membrane lipid peroxidation and protein carbonylation; and (5) uncurbed lipid peroxidation cascades may ensue, which could result in neural membrane destabilization, impaired cellular signal transduction, and ultimately cell death. This situation is compounded by the direct neurotoxic effects of some APs and their tendency to further promote transition metal accumulation in the basal ganglia with chronic use (Elkashef and Wyatt 1999; Lohr et al. 2003). Additionally, accumulating evidence of preexisting OS and endogenous AX abnormalities in schizophrenia (SZ) that precede and are independent of AP effects may contribute to the heightened susceptibility of these patients to AP-related OS and TD (Flatow et al. 2013; Merrill et al. 2013).
There is evidence suggesting that AXs such as vitamin E (Cadet and Lohr 1989; Soares-Weiser et al. 2011), melatonin (Nelson et al. 2003), and ginkgo biloba (Bhidayasiri et al. 2013) may be beneficial in the treatment of TD, but their efficacy as preventative agents has not yet been evaluated in clinical trials. Additional support for the early application of AXs in combination with APs in the treatment of SZ can be derived from evidence implicating robust and interrelated OS (Flatow et al. 2013) and inflammatory (Kirkpatrick and Miller 2013) abnormalities in SZ that may be central to the disorder itself. Accordingly, the provision of adjunctive AX support in SZ for the purpose of preventing TD may yield additional positive effects on other symptom domains. For the purposes of this review, the term AX will encompass agents that directly or indirectly reduce oxidative stress (e.g., by scavenging free radicals or strengthening the endogenous AX system).
Various animal models of TD have been developed and used to test hypotheses concerning its underlying mechanisms (Casey 2000; Blanchet et al. 2012). One such model involves administering APs to rodents continuously for a period of weeks and documenting the emergence of purposeless mouth openings referred to as vacuous chewing movements (VCMs; Turrone et al. 2002). These VCMs are considered to be analogous to the involuntary orofacial movements of TD (Casey 2000), setting the stage for this line of investigation to be used in examining the role of various factors in the development of AP-related TD. Similarly, it can be used to examine possible TD prevention strategies.
Recent experiments in rats reveal that AP-induced VCMs and OS can be attenuated by the coadministration of AX compounds such as curcumin, a substance derived from turmeric (Bishnoi et al. 2008b, 2011; Sookram et al. 2011). However, questions remain as to whether similar effects are seen across studies testing different AX-promoting treatments in this preclinical model. Thus, the present review was undertaken to establish whether consensus exists in the preclinical literature on the protective effect of such treatments against AP-induced VCMs and OS. As TD can be irreversible, developing a better understanding of the role of OS in its pathogenesis has important clinical implications, as does establishing whether AX-promoting treatments could potentially delay or prevent the onset of TD.
Methods
A literature search using Google Scholar and PubMed was performed in September 2013 with the search terms “vacuous chewing” and “antioxidant.” Publication date limits were not imposed on search results, and additional reports were identified in the reference lists of relevant articles.
Studies were included if they met the following criteria: (a) written in English, (b) published in a peer-reviewed journal (verified using Ulrichsweb), (c) examined AP-induced VCMs in rats, and (d) evaluated the effect of an AX-promoting treatment on VCM behavior, while providing an in vivo measure of OS and/or AX levels. Studies evaluating VCMs or dyskinetic behaviors induced by other drugs (e.g., reserpine, tacrine, 3-nitropropionic acid) or in other species (e.g., mice, non-human primates) were excluded.
Studies meeting the above criteria were examined for the following information: AP(s) and dose(s) used for VCM induction, route of AP administration and dosing schedule, AX treatment(s) and dose(s) evaluated, route of AX delivery and treatment schedule, study and treatment duration, in vivo measure(s) of OS and/or AX levels used, and relevant results from the study.
Results
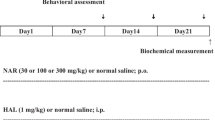
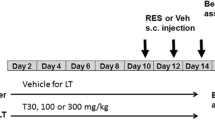
A total of 38 publications reporting results from 44 experiments were identified and included. Haloperidol (HAL; n = 36), fluphenazine (FLU; n = 3), chlorpromazine (CPZ; n = 3), and clozapine (CLZ; n = 2) were used in these experiments. Figure 1 provides a detailed overview of the article search and inclusion process.
Many agents and treatments with known direct or indirect AX potential have been evaluated for preventative effects against AP-induced VCMs. The specific measures of OS and AX levels used and reported by investigators vary across studies, but most commonly include levels of brain thiobarbituric acid reactive substances (TBARS; end-stage products of lipid peroxidation), GSH, SOD, and/or CAT. Tables 1 and 2 provide summaries of these reports and their main findings.
Taken together, the findings can be summarized as follows: (1) daily dosing with HAL (0.2–5.0 mg/kg/day), FLU (1.0–1.7 mg/kg/day), and CPZ (5 mg/kg/day) for as little as 2 weeks induces VCMs in rats; (2) AP-induced VCMs are reliably accompanied by elevations in brain TBARS and/or reductions in endogenous AX enzymes and molecules including GSH, SOD, and CAT, all of which is indicative of elevated OS in AP-treated rats; (3) an array of naturally occurring and synthetic compounds coadministered enterally and parenterally appear to effectively attenuate the manifestation of these AP-induced behavioral and biochemical alterations, thereby implicating OS in the development of AP-induced VCMs; and (4) the known pharmacological actions of these various compounds are diverse, and thus, the OS-reducing mechanisms implicated in the preventative effects of one agent may be different from those operating in another. Notably, with the exception of three studies (Naidu et al. 2003d; Thaakur and Jyothi 2007; Thaakur and Himabindhu 2009), the initiation of the AX-promoting treatment always preceded or coincided with the beginning of AP administration.
Discussion
The rat VCM model
The rat VCM model has been used extensively in preclinical efforts to elucidate the pathophysiology of TD (Casey 2000; Turrone et al. 2002; Blanchet et al. 2012). This model is an analog of the human disorder, as it captures several important aspects of TD but falls short of the more faithful representations obtained in long-term studies conducted with non-human primates (Casey 2000; Blanchet et al. 2012). In addition to orofacial movements, affected patients and certain non-human primates exposed to APs may also present with involuntary movements of the neck, trunk, and upper limbs (Blanchet et al. 2012). The VCM model fails to capture these features, as movements reportedly only occur in the orofacial region in AP-treated rats (Turrone et al. 2002; Blanchet et al. 2012).
Nonetheless, many other features of human TD translate to the rat VCM model. The use of typical APs, higher dosages, longer-treatment durations, and older rats have all been shown to result in more reliable or pronounced VCMs; similarly, withdrawal from long-term AP treatment and stress further aggravates VCMs in rodents that have developed the behavior (Turrone et al. 2002). Interestingly, structural and neurochemical changes have been observed in the striata and substantia nigra of AP-exposed rats exhibiting VCMs (Blanchet et al. 2012)—both of which are known to be involved in motor function.
However, caution must be applied when interpreting results obtained from short-duration VCM studies. Egan and colleagues (1996) demonstrated important pharmacological and neurochemical differences between HAL-induced VCMs occurring in groups of rats treated 1–3 weeks with daily intraperitoneal (IP) injections versus those emerging in rats treated with HAL decanoate for 30 weeks, where challenge doses of HAL did not reduce VCMs in the former groups but suppressed them in the latter. Critically, VCMs were late-emergent (beginning in week 12) in the HAL decanoate-treated group and persisted for an additional 24 weeks after the cessation of HAL treatment at week 30. The authors concluded that AP-induced VCMs occurring in short-term studies (1–21 days) may better reflect acute extrapyramidal or Parkinsonian side effects whereas longer-term studies (>12 weeks) are required to effectively model TD.
Long-term studies
Although the majority of the studies summarized in this review offer encouraging results, only five applied long-acting injectable AP treatment protocols that continued for 12 weeks or longer (see Table 1). This is critical, given the rapid metabolism of APs in rodents (Chiu and Franklin 1996; Kapur et al. 2003). For example, the half-life of HAL in rodents approximates 1.5 h, while it is in the range of 12–36 h in humans (Cheng and Paalzow 1992; Bezchlibnyk-Butler and Jeffries 2005). Thus, routes of administration such as IP or subcutaneous (SC) injection do not mirror the pattern of exposure observed in humans being administered APs on an ongoing basis, where steady state plasma levels are achieved within approximately 4–7 days (Dahl 1986). Administration of depot formulations in animals circumvents this problem, as does the use of osmotic minipumps where APs can be continuously infused over an extended interval as long as 1 month (Turrone et al. 2003).
An examination of the evidence presented here appears to reflect this. Findings from the five long-term studies involving depot antipsychotic administration are mixed; notably, the only negative findings encountered among all of the studies surveyed are found in three of these five publications (Andreassen et al. 1999; Sachdev et al. 1999; Fachinetto et al. 2007a). Andreassen et al. (1999) found no protective effect of coenzyme Q10 (CoQ10)-enhanced food against VCMs induced by 16 weeks of HAL decanoate treatment, speculating that the lack of effect might have been attributable to species differences in the pharmacokinetics and AX roles of CoQ10 and CoQ9 or to a predominance of oxidized versus reduced CoQ10 in the treated group. The failure to detect increased brain CoQ10 levels despite the reported rise in serum levels may also explain the negative findings, but because these biochemical measures were obtained from a separate group of rats that received only 10 days of CoQ10 treatment, their relevance to the interpretation of the behavioral data is unclear. However, other work has also shown minimal brain uptake of CoQ10 in rats (Bentinger et al. 2003).
Likewise, Sachdev and colleagues (1999) provided groups of rats with vitamin E-enhanced, vitamin E-depleted, and standard food beginning 2 weeks prior to a 12-week FLU decanoate treatment period and also failed to demonstrate differences in VCM behavior between these groups. Though changes in serum vitamin E levels were detected, the authors suggest that methodological shortcomings (small groups, vitamin E content of injectable oils) or the short-term resistance of the brain to vitamin E depletion may have partly accounted for these negative findings. Recent work has shown that feeding rats a vitamin E-enhanced diet (750 mg/kg/day) for 2 weeks yields a substantial increase in brain vitamin E levels (Betti et al. 2011), suggesting that a similar increase may have been seen if brain samples had been analyzed. Sachdev et al. (1999) simultaneously reported on a protective effect of selegiline, a MAO-B inhibitor with putative AX effects, but failed to accompany these behavioral data with any biochemical measure of OS or AX levels.
Fachinetto et al. (2005) evaluated the effects of low- versus high-fat diets (16 vs 63 % energy from fat) in a prolonged study, where diets remained altered from 6 months prior to the beginning of a 7-month HAL decanoate treatment period, and thereby provide some evidence for VCM prevention accompanied by brain TBARS reduction in months 3–5 in the low-fat diet group while implicating high-fat diets as an additional source of OS. These investigators subsequently failed to show a protective effect of Valeriana officinalis root extract against HAL decanoate-induced VCMs and associated changes in several markers of brain OS in a 14-week study, with AP treatment commencing in the third week, suggesting that this plant extract may offer little in vivo AX support (Fachinetto et al. 2007a). Although the pharmacokinetic profile of valerenic acid—a single bioactive constituent of V. officinalis—has been established in rats, whether this compound or any other derived from the plant can access the brain in vivo has yet to be determined (Sampath et al. 2012).
Finally, in a 24-week study examining the effect of diphenyl diselenide against FLU enanthate, Fachinetto and colleagues (2007b) observed a reduced prevalence of VCM behavior associated with increased striatal SOD levels in the group receiving FLU and diphenyl diselenide. These findings suggest that this compound protected some rats from developing VCMs, but it failed to attenuate VCM severity among treated rats that did develop the behavior. Others have reported that diphenyl diselenide can reach the brain following oral administration in rats (Prigol et al. 2010), but certain methodological discrepancies between these studies—e.g., the use of rat pups versus adults and much higher doses—must be emphasized.
It should also be noted that Rogoza and colleagues (2004) alluded to results from a 6-month study examining the protective effect of the free radical trapper α-phenyl-N-tert-butylnitrone as being similar to those from their 4-week study summarized in Table 2. However, these data were absent from their report and the VCMs were not induced by depot AP treatment.
Short-term studies
Nearly all of the short-term studies in Table 2 administered APs via daily IP or SC injections, with two notable exceptions. Barcelos and colleagues (2010) demonstrated the protective effect of ω-3 fatty acids against depot HAL- and FLU-induced VCMs and associated TBARS elevations in the hippocampus, substantia nigra, and periphery. Here, ω-3 fatty acids were introduced to rats’ drinking water beginning 4 weeks prior to a 4-week AP treatment period. Polyunsaturated membrane lipids are particularly susceptible to peroxidation by free radicals in the brain (Elkashef and Wyatt 1999; Flatow et al. 2013), and the authors proposed that the beneficial effect of supplemental ω-3 fatty acids may have been due to their direct AX or membrane lipid-sparing properties. Subsequently, this group reported intriguing results from a study where rats were subjected to 16 weeks of swimming exercise with HAL decanoate treatment occurring during the final 4 weeks (Teixeira et al. 2011). Swimming exercise sessions occurred 5 times a week and entailed three 15-min supervised swim intervals separated by 5-min rest periods where rats remained on a semi-submerged platform. Protective effects on both behavioral and biochemical parameters were seen in the exercised group. Notably, VCM behavior was correlated with cortical and subcortical TBARS levels and inversely correlated with subcortical CAT, thereby further implicating increased OS and compromised AX defenses in AP-induced VCM behavior.
Daily IP or SC injections of APs were used to induce VCMs in the remaining 31 studies (see Table 2). These varied in duration and include a 7-week study, three 4-week studies, twenty-five 3-week studies, and a 2-week study. The protective properties of a variety of compounds and formulations were evaluated, and results were largely unanimous. Short-term (2–7 weeks) daily AP treatment induced VCMs and produced elevations in markers of OS, such as TBARS, and reductions in endogenous AXs, such as GSH, SOD, and CAT. These behavioral and biochemical changes were consistently attenuated by the coadministration of numerous naturally occurring compounds: plant-derived substances such as quercetin (Naidu et al. 2003b, 2003d), rutin (Bishnoi et al. 2007c), and curcumin (Bishnoi et al. 2008b, 2011; Sookram et al. 2011); extracts derived from Withania somnifera root (Naidu et al. 2003c), Spirulina maxima (Thaakur and Jyothi 2007), Morus alba leaf (Nade et al. 2010), Mucuna pruriens (Pathan et al. 2011), and Murraya koenigii leaf (Patil et al. 2012); vitamins B1, B6, B12 (Macêdo et al. 2011), and E (Pathan et al. 2011; Patil et al. 2012); and other agents such as melatonin (Naidu et al. 2003a), xanthines (Bishnoi et al. 2006, 2007d), neurosteroids (Bishnoi et al. 2008a, 2008c), l-arginine (Bishnoi et al. 2009), alpha lipoic acid (Thaakur and Himabindhu 2009), and HAL-loaded polysorbate-coated nanocapsules containing fish oil-based cores (Benvegnú et al. 2012).
A collection of drugs were also reported to be effective in these short-duration studies, including the following: the sympatholytic carvedilol (Naidu et al. 2002); the immunosupressant tacrolimus (Singh et al. 2003); the selenium-containing compound ebselen (Burger et al. 2005); N-acetylcysteine amide (Sadan et al. 2005); the synthetic steroid U-74500A; the hypnotic zolpidem; the adenosine-modulating dipyridamole and nimodipine; the calcium channel-blocking verapamil, diltiazem, and nifedipine; the NO donor molsidomine (Bishnoi et al. 2007a, 2007b, 2007e, 2008d, 2009); the free radical-trapping α-phenyl-N-tert-butylnitrone (Daya et al. 2011); and the peroxisome proliferator-activated receptor agonists pioglitazone and fenofibrate (Grover et al. 2013).
As mentioned previously, the applicability of findings obtained from such short-duration VCM studies to human TD may be limited because early-onset VCMs more closely resemble acute extrapyramidal symptom (EPS)-like responses to APs (Egan et al. 1996). This differentiation of early- versus late-onset VCMs is supported by the discrepancy in findings from the aforementioned vitamin E studies, where a protective effect was seen against 3 weeks of daily IP HAL (Pathan et al. 2011; Patil et al. 2012) but not 12 weeks of depot FLU treatment (Sachdev et al. 1999), although other methodological differences aside from study duration may also have affected these outcomes. Because early EPS is a known harbinger of TD in susceptible patients treated with AP (Saltz et al. 1991), the findings from these studies are worthy of some consideration. At the very least, not only do they implicate elevated OS in acute EPS-like responses to AP but they also suggest that these responses may be amenable to disruption via numerous pharmacological mechanisms. That such a variety of agents can apparently attenuate VCMs induced by short-term daily AP treatments further demonstrates that early-onset VCMs lack the robust qualities of late-onset VCMs (Egan et al. 1996), and the discrepancy between the vitamin E studies mentioned above also supports this conclusion (Sachdev et al. 1999; Pathan et al. 2011; Patil et al. 2012). Additional studies of sufficient duration applying depot APs to induce VCMs will clarify these matters. Nonetheless, these reports indicate that a variety of agents possess in vivo OS-attenuating or AX-potentiating properties in rats, yet whether these are attributable to direct (e.g., free radical-scavenging) or indirect (e.g., AX-replenishing) effects remains open to question, as does their relevance to TD prevention in humans.
Summary and future directions
Summarizing, evidence from long-term studies (>12 weeks; Table 1) suggests that the consumption of a reduced-fat diet (Fachinetto et al. 2005) and the coadministration of diphenyl diselenide (Fachinetto et al. 2007b) can attenuate depot HAL- and FLU-induced VCMs and mitigate brain OS while reducing TBARS and elevating striatal SOD, respectively. However, enhancing food with CoQ10 (Andreassen et al. 1999), vitamin E (Sachdev et al. 1999, but see Pathan et al. 2011; Patil et al. 2012), or coadministering V. officinalis root extract (Fachinetto et al. 2007a) confers no protection against depot AP-induced VCMs and OS. Notably, two 4-week depot studies also demonstrated the protective effects of ω-3 fatty acid supplementation (Barcelos et al. 2010) and exercise (Teixeira et al. 2011) against AP-induced VCMs; these effects were associated with favorable reductions in peripheral and brain TBARS and increases in brain CAT. Likewise, short-term studies (<12 weeks; Table 2) applying daily AP injections indicate that early-onset VCMs, OS, and AX reductions can be attenuated by a multitude of agents.
While these results offer some support to the OS hypothesis of TD, there is a shortage of studies of sufficient duration applying long-acting injectable APs. Additional studies are needed to evaluate whether the promising results seen with a variety of compounds in the short term (<12 weeks) can be obtained in longer-duration studies with depot APs. Likewise, there is a need for replication: vitamin E (Sachdev et al. 1999; Pathan et al. 2011; Patil et al. 2012), quercetin (Naidu et al. 2003b, 2003d), curcumin (Bishnoi et al. 2008b, 2011; Sookram et al. 2011), progesterone (Bishnoi et al. 2008a, 2008c), ω-3 fatty acids (Barcelos et al. 2010; Benvegnú et al. 2012), and α-phenyl-N-tert-butylnitrone (Rogoza et al. 2004; Daya et al. 2011) were the only AX treatments assessed in more than a single study. Surprisingly, although vitamin E and several B vitamins (Macêdo et al. 2011) were evaluated in these preclinical studies, none examined vitamin C.
It is also noteworthy that none of the studies captured in this review examined depot atypical APs. Although Bishnoi and colleagues (2011) included a CLZ group in their second curcumin study and report effects on striatal OS and AX measures similar to those seen with HAL, though much less pronounced, this atypical AP was administered by daily injection for only 3 weeks. Interestingly, this finding contrasts with that of an earlier report where no effect of CLZ was seen on similar measures in the forebrain (Naidu et al. 2002). The discrepancy could be accounted for by differences in the doses of CLZ used (10 vs 2 mg/kg) and/or in the brain regions assayed in these studies (striatum vs forebrain). Nonetheless, long-term studies evaluating the potential of depot atypical APs —such as risperidone, paliperidone, olanzapine, or aripiprazole —to produce VCMs and in vivo OS would be informative.
In conclusion, it would appear that there is insufficient preclinical evidence to strongly advocate for preventative AX-based treatments to guard patients receiving APs against TD, at least at this point. While limited evidence from clinical trials suggests that vitamin E and melatonin may hold some promise as treatments for established TD (Cadet and Lohr 1989; Nelson et al. 2003; Soares-Weiser et al. 2011), more preclinical work is needed to determine whether such compounds can effectively prevent the onset of AP-induced VCMs and accompanying in vivo changes in OS and AX measures in studies of sufficient duration. From a clinical perspective, the ideal preventative AX compound would be readily accessible, naturally occurring (if not endogenous), potent, nontoxic, and capable of crossing the blood-brain barrier. Melatonin (Naidu et al. 2003a) and curcumin (Bishnoi et al. 2008b, 2011; Sookram et al. 2011) both appear to be candidate AXs that fit this profile, and although some preclinical evidence suggests their protective properties, experiments were of short duration (2–3 weeks) and used daily IP injections of HAL (1–5 mg/kg) to induce VCMs. Future studies should be longer in duration (>12 weeks) and incorporate a range of long-acting injectable AP doses that better correspond to those used in the clinic (Egan et al. 1996; Kapur et al. 2003). Such work would likely have higher translational value with greater relevance to human TD. As the pathophysiology of TD remains obscure and no single treatment has been proven to effectively manage this iatrogenic condition, there is a strong rationale for further assessing the efficacy of AX-based prevention strategies in well-designed rat VCM studies. Furthermore, given the accumulating evidence implicating OS and AX abnormalities in SZ (Flatow et al. 2013) and the heightened susceptibility of these patients to TD (Merrill et al. 2013), the early application of AX-promoting treatments alongside APs may prove to be a promising strategy for simultaneously mitigating TD risk and providing adjunctive AX support to the patients who need it the most.
Conflict of interest
Dr. Remington has received research support from Novartis, Medicure, and Neurocrine Bioscience, consultant fees from Roche, and speaker’s fees from Novartis. He holds no commercial investments in any pharmaceutical company within the past 5 years. All other authors report no conflicts of interest.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders- 5. APA Press, Arlington
Andreassen OA, Jørgensen HA (2000) Neurotoxicity associated with neuroleptic-induced oral dyskinesias in rats: implications for tardive dyskinesia? Prog Neurobiol 61:525–541
Andreassen OA, Weber C, Jørgensen HA (1999) Coenzyme Q10 does not prevent oral dyskinesias induced by long-term haloperidol treatment of rats. Pharmacol Biochem Behav 64:637–642
Barcelos RCS, Benvegnú DM, Boufleur N, Reckziegel P, Müller LG, Pase C, Emanuelli T, Bürger ME (2010) Effects of ω-3 essential fatty acids (ω-3 EFAs) on motor disorders and memory dysfunction typical neuroleptic-induced: behavioral and biochemical parameter. Neurotox Res 17:228–237
Bentinger M, Dallner G, Chojnacki T, Swiezewska E (2003) Distribution and breakdown of labeled coenzyme Q10 in rat. Free Radical Bio Med 34:563–575
Benvegnú DM, Barcelos RCS, Boufleur N, Pase CS, Reckziegel P, Flores FC, Ourique AF, Nora MD, da Silva CDB, Beck RCR, Bürger ME (2012) Haloperidol-loaded polysorbate-coated polymeric nanocapsules decrease its adverse motor side effects and oxidative stress markers in rats. Neurochem Int 61:623–631
Betti M, Minelli A, Ambrogini P, Ciuffoli S, Viola V, Galli F, Canonico B, Lattanzi D, Colombo E, Sestili P, Cuppini R (2011) Dietary supplementation with α-tocopherol reduces neuroinflammation and neuronal degeneration in the rat brain after kainic acid-induced status epilepticus. Free Radical Res 45:1136–1142
Bezchlibnyk-Butler KZ, Jeffries JJ (2005) Clinical handbook of psychotropic drugs. Hogrefe and Huber Publishers, Toronto
Bhidayasiri R, Fahn S, Weiner WJ, Gronseth GS, Sullivan KL, Zesiewicz TA (2013) Evidence-based guideline: treatment of tardive syndromes. Neurology 81:463–469
Bishnoi M, Chopra K, Kulkarni SK (2006) Involvement of adenosinergic receptor system in an animal model of tardive dyskinesia and associated behavioural, biochemical and neurochemical changes. Eur J Pharmacol 552:55–66
Bishnoi M, Chopra K, Kulkarni SK (2007a) U-74500A (Lazaroid), a 21-aminosteroid attenuates neuroleptic-induced orofacial dyskinesia. Method Find Exp Clin 29:601–605
Bishnoi M, Chopra K, Kulkarni SK (2007b) Possible anti-oxidant and neuroprotective mechanisms of zolpidem in attenuating typical anti-psychotic-induced orofacial dyskinesia—a biochemical and neurochemical study. Prog Neuro-Psychoph 31:1130–1138
Bishnoi M, Chopra K, Kulkarni SK (2007c) Protective effect of rutin, a polyphenolic flavonoid against haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes. Fund Clin Pharmacol 21:521–529
Bishnoi M, Chopra K, Kulkarni SK (2007d) Theophylline, adenosine receptor antagonist prevents behavioral, biochemical and neurochemical changes associated with an animal model of tardive dyskinesia. Pharmacol Rep 59:181–191
Bishnoi M, Chopra K, Kulkarni SK (2007e) Protective effect of adenosine reuptake inhibitors in haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes. Pharmacology 79:171–183
Bishnoi M, Chopra K, Kulkarni SK (2008a) Modulatory effect of neurosteroids in haloperidol-induced vacuous chewing movements and related behaviors. Psychopharmacology 196:243–254
Bishnoi M, Chopra K, Kulkarni SK (2008b) Protective effect of curcumin, the active principle of turmeric (Curcuma longa) in haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes in rat brain. Pharmacol Biochem Behav 88:511–522
Bishnoi M, Chopra K, Kulkarni SK (2008c) Progesterone attenuates neuroleptic-induced orofacial dyskinesia via the activity of its metabolite, allopregnanolone, a positive GABAA modulating neurosteroid. Prog Neuro-Psychoph 32:451–461
Bishnoi M, Chopra K, Kulkarni SK (2008d) Protective effect of L-type calcium channel blockers against haloperidol-induced orofacial dyskinesia: a behavioural, biochemical and neurochemical study. Neurochem Res 33:1869–1880
Bishnoi M, Chopra K, Kulkarni SK (2009) Co-administration of nitric oxide (NO) donors prevents haloperidol-induced orofacial dyskinesia, oxidative damage and change in striatal dopamine levels. Pharmacol Biochem Behav 91:423–429
Bishnoi M, Chopra K, Rongzhu L, Kulkarni SK (2011) Protective effect of curcumin and its combination with piperine (bioavailability enhancer) against haloperidol-associated neurotoxicity: cellular and neurochemical evidence. Neurotox Res 20:215–225
Blanchet PJ, Parent M, Rompré PH, Lévesque D (2012) Relevance of animal models to human tardive dyskinesia. Behav Brain Funct 8:1–9
Burger ME, Fachinetto R, Zeni G, Rocha JBT (2005) Ebselen attenuates haloperidol-induced orofacial dyskinesia and oxidative stress in rat brain. Pharmacol Biochem Behav 81:608–615
Cadet JL, Lohr JB (1989) Possible involvement of free radicals in neuroleptic-induced movement disorders: evidence from treatment of tardive dyskinesia with vitamin E. Ann NY Acad Sci 570:176–185
Casey DE (2000) Tardive dyskinesia: pathophysiology and animal models. J Clin Psychiat 61(suppl 4):5–9
Cheng YF, Paalzow LK (1992) Linear pharmacokinetics of haloperidol in the rat. Biopharm Drug Dispos 13:69–76
Chiu JA, Franklin RB (1996) Analysis and pharmacokinetics of olanzapine (LY170053) and two metabolites in rat plasma using reversed-phase HPLC with electrochemical detection. J Pharmaceut Biomed 14:609–615
Correll CU, Schenk EM (2008) Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatr 21:151–156
Dahl SG (1986) Plasma level monitoring of antipsychotic drugs clinical utility. Clin Pharmacokinet 11:36–61
Daya RP, Tan ML, Sookram CD, Skoblenick K, Mishra RK (2011) Alpha-phenyl-N-tert-butylnitrone prevents oxidative stress in a haloperidol-induced animal model of tardive dyskinesia: investigating the behavioural and biochemical changes. Brain Res 1412:28–36
Egan MF, Hurd Y, Ferguson J, Bachus SE, Hamid EH, Hyde TM (1996) Pharmacological and neurochemical differences between acute and tardive vacuous chewing movements induced by haloperidol. Psychopharmacology 127:337–345
Elkashef AM, Wyatt RJ (1999) Tardive dyskinesia: possible involvement of free radicals and treatment with vitamin E. Schizophrenia Bull 25:731–740
Fachinetto R, Burger ME, Wagner C, Wondracek DC, Brito VB, Nogueira CW, Ferreira J, Rocha JBT (2005) High fat diet increases the incidence of orofacial dyskinesia and oxidative stress in specific brain regions of rats. Pharmacol Biochem Behav 81:585–592
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Ávila DS, Burger ME, Calixto JB, Rocha JBT, Ferreira J (2007a) Valeriana officinalis does not alter the orofacial dyskinesia induced by haloperidol in rats: role of dopamine transporter. Prog Neuro-Psychoph 31:1478–1486
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Puntel RL, Paixão MW, Braga AL, Calixto JB, Rocha JBT, Ferreira J (2007b) Diphenyl diselenide decreases the prevalence of vacuous chewing movements induced by fluphenazine in rats. Psychopharmacology 194:423–432
Fibiger HC, Lloyd KG (1984) Neurobiological substrates of tardive dyskinesia: the GABA hypothesis. Trends Neurosci 7:462–464
Flatow J, Buckley P, Miller BJ (2013) Meta-analysis of oxidative stress in schizophrenia. Biol Psychiat 74:400–409
Grover S, Kumar P, Singh K, Vikram V, Budhiraja RD (2013) Possible beneficial effect of peroxisome proliferator-activated receptor (PPAR)—α and γ agonist against a rat model of oral dyskinesia. Pharmacol Biochem Behav 111:17–23
Kapur S, VanderSpek SC, Brownlee BA, Nobrega JN (2003) Antipsychotic dosing in preclinical models is often unrepresentative of the clinical condition: a suggested solution based on in vivo occupancy. J Pharmacol Exp Ther 305:625–631
Kirkpatrick B, Miller BJ (2013) Inflammation and schizophrenia. Schizophrenia Bull 39:1174–1179
Lohr JB, Kuczenski R, Niculescu AB (2003) Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17:47–62
Macêdo DS, de Oliveira GV, Gomes PXL, de Araújo FYR, de Souza CM, Vasconcelos SMM, de Barros Viana GS, de Sousa FCF, Carvalho AF (2011) B vitamins attenuate haloperidol-induced orofacial dyskinesia in rats: possible involvement of antioxidant mechanisms. Behav Pharmacol 22:674–680
Merrill RM, Lyon JL, Matiaco PM (2013) Tardive and spontaneous dyskinesia in the general population. BMC Psychiatry 13:152
Nade VS, Kawale LA, Yadav AV (2010) Protective effect of Morus alba leaves on haloperidol-induced orofacial dyskinesia and oxidative stress. Pharm Biol 48:17–22
Naidu PS, Singh A, Kulkarni SK (2002) Carvedilol attenuates neuroleptic-induced orofacial dyskinesia: possible antioxidant mechanisms. Brit J Pharmacol 136:193–200
Naidu PS, Singh A, Kaur P, Sandhir R, Kulkarni SK (2003a) Possible mechanism of action in melatonin attenuation of haloperidol-induced orofacial dyskinesia. Pharmacol Biochem Behav 74:641–648
Naidu PS, Singh A, Kulkarni SK (2003b) Quercetin, a bioflavinoid, attenuates haloperidol-induced orofacial dyskinesia. Neuropharmacology 44:1100–1106
Naidu PS, Singh A, Kulkarni SK (2003c) Effect of Withania somnifera root extract on haloperidol-induced orofacial dyskinesia: possible mechanisms of action. J Med Food 6:107–114
Naidu PS, Singh A, Kulkarni SK (2003d) Reversal of haloperidol-induced orofacial dyskinesia by quercetin, a bioflavinoid. Psychopharmacology 167:418–423
Nelson LA, McGuire JM, Hausafus SN (2003) Melatonin for the treatment of tardive dyskinesia. Ann Pharmacother 37:1128–1131
Olfson M, Blanco C, Liu S, Wang S, Correll CU (2012) National trends in the office-based treatment of children, adolescents, and adults with antipsychotics. Arch Gen Psychiat 69:1247–1256
Pathan AA, Mohan M, Kasture AS, Kasture SB (2011) Mucuna pruriens attenuates haloperidol-induced orofacial dyskinesia in rats. Nat Prod Res 25:764–771
Patil R, Hiray Y, Shinde S, Langade P (2012) Reversal of haloperidol-induced orofacial dyskinesia by Murraya koenigii leaves in experimental animals. Pharm Biol 50:691–697
Prigol M, Pinton S, Schumacher R, Nogueira CW, Zeni G (2010) Convulsant action of diphenyl diselenide in rat pups: measurement and correlation with plasma, liver and brain levels of compound. Arch Toxicol 84:373–378
Remington G (2007) Tardive dyskinesia: eliminated, forgotten, or overshadowed? Curr Opin Psychiatr 20:131–137
Rogoza RM, Fairfax DF, Henry P, N-Marandi S, Khan RF, Gupta SK, Mishra RK (2004) Electron spin resonance spectroscopy reveals alpha-phenyl-N-tert-butylnitrone spin-traps free radicals in rat striatum and prevents haloperidol-induced vacuous chewing movements in the rat model of human tardive dyskinesia. Synapse 54:156–163
Sachdev PS (2000) The current status of tardive dyskinesia. Aust Nz J Psychiat 34:355–369
Sachdev P, Saharov T, Cathcart S (1999) The preventative role of antioxidants (selegiline and vitamin E) in a rat model of tardive dyskinesia. Biol Psychiat 46:1672–1681
Sadan O, Bahat-Stromza M, Gilgun-Sherki Y, Atlas D, Melamed E, Offen D (2005) A novel brain-targeted antioxidant (AD4) attenuates haloperidol-induced abnormal movement in rats: implications for tardive dyskinesia. Clin Neuropharmacol 28:285–288
Saltz BL, Woerner MG, Kane JM, Lieberman JA, Alvir JMJ, Bergmann KJ, Blank K, Koblenzer J, Kahaner K (1991) Prospective study of tardive dyskinesia incidence in the elderly. J Amer Med Assoc 266:2402–2406
Sampath C, Haug K, Thanei S, Hamburger M, Derendorf H, Frye R, Butterweck V (2012) Pharmacokinetics of valerenic acid in rats after intravenous and oral administrations. Planta Med 78:575–581
Sarró S, Pomarol-Clotet E, Canales-Rodriguez EJ, Salvador R, Gomar JJ, Oritz-Gil J, Landin-Romero R, Vila-Rodriguez F, Blanch J, McKenna PJ (2013) Structural brain changes associated with tardive dyskinesia in schizophrenia. Brit J Psychiat 203:51–57
Singh A, Naidu PS, Kulkarni SK (2003) Possible antioxidant and neuroprotective mechanisms of FK506 in attenuating haloperidol-induced orofacial dyskinesia. Eur J Pharmacol 477:87–94
Soares-Weiser K, Maayan N, McGrath J (2011) Vitamin E for neuroleptic-induced tardive dyskinesia. Cochrane DB Syst Rev. doi:10.1002/14651858.CD000209.pub2
Sohal RS, Weindruch R (1996) Oxidative stress, caloric restriction, and aging. Science 273:59–63
Sookram C, Tan M, Daya R, Heffernan S, Mishra RK (2011) Curcumin prevents haloperidol-induced development of abnormal oro-facial movements: possible implications of Bcl-XL in its mechanism of action. Synapse 65:788–794
Teixeira A, Müller LG, Reckziegel P, Boufleur N, Pase CS, Villarinho JG, Fachinetto R, Ferreira J, Rocha JBT, Bürger ME (2011) Beneficial effects of an innovative exercise model on motor and oxidative disorders induced by haloperidol in rats. Neuropharmacology 60:432–438
Thaakur S, Himabindhu G (2009) Effect of alpha lipoic acid on the tardive dyskinesia and oxidative stress induced by haloperidol in rats. J Neural Transm 116:807–814
Thaakur SR, Jyothi B (2007) Effect of spirulina maxima on the haloperidol induced tardive dyskinesia and oxidative stress in rats. J Neural Transm 114:1217–1225
Turrone P, Remington G, Nobrega JN (2002) The vacuous chewing movement (VCM) model of tardive dyskinesia revisited: is there a relationship to dopamine D2 receptor occupancy? Neurosci Biobehav R 26:361–380
Turrone P, Remington G, Kapur S, Nobrega JN (2003) Differential effects of within-day continuous vs transient dopamine D2 receptor occupancy in the development of vacuous chewing movements (VCMs) in rats. Neuropsychopharmacol 28:1433–1439
West IC (2000) Radicals and oxidative stress in diabetes. Diabetic Med 17:171–180
Yamamoto BK, Raudensky J (2008) The role of oxidative stress, metabolic compromise, and inflammation in neuronal injury produced by amphetamine-related drugs of abuse. J Neuroimmune Pharm 3:203–217
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lister, J., Nobrega, J.N., Fletcher, P.J. et al. Oxidative stress and the antipsychotic-induced vacuous chewing movement model of tardive dyskinesia: evidence for antioxidant-based prevention strategies. Psychopharmacology 231, 2237–2249 (2014). https://doi.org/10.1007/s00213-014-3582-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3582-6