Abstract
Reserpine (RES)-induced orofacial dyskinesia (OD) has been used as an animal model for human tardive dyskinesia (TD) for decades, due to its strong pathophysiological association with striatal oxidative stress and neural cytoarchitecture alteration. L-Theanine (LT), one of the major amino acid components in green tea, has potent antioxidative, anti-inflammatory, and neuroprotective effects. In this study, we examined the potential protective effects of LT on RES-induced behavioral and neurochemical dysfunction in rats. RES treatment (1 mg/kg s.c., 3 injections 1 day apart) induced significant increases (p < 0.001) in the frequency of vacuous chewing movements (VCM), tongue protrusion (TP), as well as the duration of facial twitching (FT). LT treatment (100, 300 mg/kg orally for 14 days, starting 10 days before RES injection) was able to prevent most of the RES-induced OD. Moreover, LT treatment reduced the RES-induced lipid peroxidation (LPO) production, increased the antioxidation power and catecholamines in the striatum, and significantly reduced the levels of neuroinflammatory and apoptotic markers. Our results indicated that LT was able to counteract the increased oxidative damage, neurotransmitter deficiency, neuroinflammation, and apoptosis induced by RES, and these results have demonstrated the possible neuroprotective effects of LT against RES-induced OD, including antioxidation, neurochemical deficiency prevention, antineuroinflammation, and antiapoptosis. These findings, therefore, suggest a potential role for LT to have a clinically relevant therapeutic effect in delaying or treating human TD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tardive dyskinesia (TD), caused by long-term administration of neuroleptic drugs, has become an evident clinical problem during schizophrenia treatment due to its duration—from months to years—after ceasing to take the drug. In some patients, the symptoms are irreversible (Huang et al. 1997; Kostrzewa et al. 2007). Reserpine (RES) is an indole alkaloid and had been used for decades as an antipsychotic and antihypertensive reagent to relieve psychotic symptoms and control blood pressure, respectively (Davies and Shepherd 1955; Durlach 1956). Previous reports have linked RES with the development of TD and behavioral symptoms of Parkinson disease (PD) by depleting catecholamines (Neisewander et al. 1994; Ishibashi and Ohno 2004; Fernandes et al. 2012; Santos et al. 2013). RES-treated rats develop orofacial dyskinesia (OD), which is characterized by increased vacuous chewing movements, tongue protrusion, orofacial bursts, and cataleptic behavior (Neisewander et al. 1994; Patil et al. 2012a, b; Wang et al. 2015). Similar to the clinical findings, these symptoms, oxidative stress, neuroinflammation, neurotransmitter deficiency, and serious neurodegeneration, seem to be related to OD; the development of RES-induced OD has been linked to an increased production in striatal lipid peroxidation (LPO) by-product and increased levels of inflammatory mediators. The combination of these two factors would cause a rapid reduction in antioxidative enzyme activity and catecholamine levels, resulting in motor dysfunction, resembling the symptoms of PD (Hanff et al. 2010; de Freitas et al. 2016). These previous reports suggested that antioxidant or anti-inflammatory agent treatment may be beneficial in treating TD in animal models (Burger et al. 2003; Patil et al. 2012a, b; Nade et al. 2013; Wang et al. 2015; Cunha et al. 2016; Datta et al. 2016).
L-Theanine (LT), γ-glutamylethylamide, is one of the main amino acid components in green tea, and it is synthesized from ethylamine and glutamate in green tea leaves (Terashima et al. 1999). LT is mostly absorbed in the small intestine and is then further redistributed to other organs, including the brain (Kakuda 2011). Many reports have shown that LT has numerous pharmacological properties: sedative, hypotensive, anti-obesity, anti-inflammatory, and antitumorigenesis effects (Yokogoshi et al. 1995; Zhang et al. 2002; Zheng et al. 2004; Yin et al. 2011; Pérez-Vargas et al. 2016). Furthermore, LT can scavenge reactive radicals and decrease the peroxidative condition (Kakuda 2011; Thangarajan et al. 2014; Sumathi et al. 2015). It has also been predicted to have neuroprotective properties to treat behavioral impairments induced by ischemia, toxins, and stress (Kakuda 2011; Yin et al. 2011; Zukhurova et al. 2013; Thangarajan et al. 2014; Sumathi et al. 2015; Jamwal and Kumar 2017). However, the reports regarding its protective effects on RES-induced OD are still limited. Given its antioxidative, anti-inflammatory, and neurotransmitter-normalizing properties, we hypothesized that LT counteracts the increased oxidative damage, neurotransmitter deficiency, neuroinflammation, and apoptosis induced by RES, and sequentially disrupts the OD development. In this study, we examined the possible therapeutic effects of LT to prevent the RES-induced OD in rats, as well as monitoring the oxidative status, antioxidation power, neurotransmitter levels, neuroinflammation, and apoptotic markers in the striatum: (1) the levels of LPO by-products; (2) enzyme activities for glutathione (GSH), superoxide dismutase (SOD), and catalase (CAT); (3) catecholamine levels including dopamine (DA), norepinephrine (NE), serotonin (5-HT), and their metabolites 3,4-dihydroxyphenylacetic acid (DOPAC), homovanillic acid (HVA), and 5-hydroxyindoleacetic acid (5-HIAA); and also (4) tumor necrosis factor α (TNF-α), interleukin-6 (IL-6), and caspase-3 were measured in both the control and RES treatment groups with or without LT treatment. The groups were also monitored for characteristics of OD: increases of the frequency in vacuous chewing movements (VCM), tongue protrusion (TP), and the duration of facial twitching (FT).
Materials and Methods
Animals
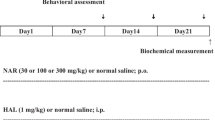
All the experiments followed the “Guidelines for the Care and Use of Laboratory Animals” published by the U.S. National Institutes of Health and were approved by the Institutional Animal Care and Use Committee (IACUC) of the National Taipei University of Technology (IACUC Approval No: 20150217). Male Wistar rats weighing 270–320 g (about 3 months old) were used for our study. Rats were housed in groups of three, each in Plexiglas cages with free access to food and water in a room with a controlled temperature (22 ± 3 °C) and in 12/12-h light/dark cycle with lights on at 7:00 a.m. The rats were randomly assigned to eight groups (Table 1): control group (C), reserpine (RES) treatment group (R), LT 30 mg/kg treatment group (T30), LT 100 mg/kg treatment group (T100), LT 300 mg/kg treatment group (T300), LT 30 mg/kg + RES treatment group (T30 + R), LT 100 mg/kg + RES treatment group (T100 + R), and LT 300 mg/kg + RES treatment group (T300 + R). Figure 1 illustrates the experimental paradigm. The C group received distilled water orally for 14 days and a 0.1% acetic acid solution (vehicle for reserpine) subcutaneously (s.c.) 3 times, once on each of days 10, 12, and 14. The first injection of acetic acid was given on the tenth day, after the administration of distilled water. The R group received distilled water orally for 14 days and 1 mg/kg RES s.c. 3 times, on days 10, 12, and 14. The T30, T100, and T300 groups received accordingly 30, 100, or 300 mg/kg LT orally for 14 days and 0.1% acetic acid solution s.c. 3 times, on days 10, 12, and 14. T30 + R, T100 + R, and T300 + R groups received 30, 100, or 300 mg/kg, respectively, of LT orally for 14 days and 1 mg/kg RES s.c. 3 times, on days 10, 12, and 14. On the tenth, 12th, and 14th day, the administration of LT or distilled water preceded the RES or acetic acid solution injection by 60 min. On the 15th day, 24 h after the third injection of RES or acetic acid solution, all animals were examined and quantified for their OD behavior. Animals were sacrificed about 1 h after behavioral assessments. During this study, three rats died naturally for unknown reasons.
Experimental design and drug treatment paradigm: 24 h after the third injection of RES or its vehicle acetic acid solution, all animals were examined for their OD behavior, and animals were sacrificed to do the biochemical assessments 1 h after behavioral assessments. (RES: reserpine, 1 mg/kg; LT: L-theanine; s.c.: subcutaneous; vehicle for RES: 0.1% acetic acid)
Drugs
Reserpine (methyl reserpate 3,4,5-trimethoxybenzoic acid ester; Sigma) was dissolved in glacial acetic acid, then diluted to a final concentration of 0.1% acetic acid with distilled water; the vehicle consisted of a 0.1% acetic acid solution. The above solutions were subcutaneously injected. However, LT (N-ethyl-l-glutamine ≥ 98%; Sigma), prepared with distilled water, was orally administrated during the period of housekeeping and animal nursing. All the drug dosages were adapted from the previous publications (Thangarajan et al. 2014; Wang et al. 2015) and administrated in the volume of 1.0 mL/kg body weight.
Behavioral Testing
On the 15th day, 24 h after the third injection of RES or the acetic acid solution, animals were examined for OD behavior (Burger et al. 2003). Animals were placed in separate cages (20 × 20 × 19 cm), equipped with mirrors underneath the floors to allow for behavioral quantification even when the animal was facing away from the observer. To quantify the occurrences of OD, the events of VCM and TP and the duration of FT were recorded 15 min in each section after a period of 2 min adaptation. All behavioral experiments were conducted between 09:00 and 11:00 a.m.
Dissection and Homogenization
Rats were sacrificed about 1 h after behavioral examination. The brain was quickly removed and the striatum was isolated. The dissected-out striatum tissue was rinsed with isotonic saline and weighed, and then it was homogenized with 0.1 N HCl. A 10% (w/v) tissue homogenate was prepared in a 0.1-M phosphate buffer (pH 7.4); the pos nuclear fraction for catalase assay was obtained by centrifugation of the homogenate at 1000g for 20 min at 4 °C. For the other enzyme assays, centrifuging was done at 12,000g for 60 min at 4 °C.
Measurement of Oxidative Stress Parameters
Assessment of Lipid Peroxidative Indices
Lipid peroxide concentration was measured by the thiobarbituric acid-reactive substance (TBARS) assay, adapted from Ohkawa et al. (1979), per the procedures described by Hashimoto et al. (2005). The concentration was measured in nanomoles of malondialdehyde/milligram of protein. Malondialdehyde levels were then further normalized to a standard preparation of 1,1,3,3-tetraethoxypropane.
Measurement of Glutathione
GSH was measured using the methods described by Ellman (1959). Into the homogenate, 10% trichloroacetic acid was added, as well as 1.0 mL of Ellman’s reagent [19.8 mg of 5,5-0-dithiobisnitro benzoic acid in 100 mL of 1.0% sodium citrate and 3 mL of phosphate buffer (pH 8.0)], then centrifuged. The finished developed product was measured at 412 nm. The results were expressed in units of nanomoles of GSH/milligram of tissue.
Measurement of Superoxide Dismutase Activity
The assay to determine SOD activity was based on the ability of SOD to inhibit the spontaneous oxidation of adrenaline to adrenochrome (Misra and Fridovich 1972). Supernatant of 0.05 mL was added into 2.0 mL of carbonate buffer, together with 0.5 mL of ethylenediamine tetraacetic acid (EDTA). The reaction was initiated by adding 0.5 mL of epinephrine. The auto-oxidation of adrenaline (3 × 10−4 M) to adrenochrome at pH 10.2 was measured at an optical density at 480 nm. The changes in optical density were measured at 480 nm, normalized to a blank reagent, every minute. The results are expressed as units of SOD activity (milligram per protein). One unit of SOD activity caused about 50% inhibition of adrenaline. The results were expressed using nanomoles of SOD per unit/milligram of tissue.
Measurement of Catalase Activity
The CAT activity assay was adapted from Beers and Sizer (1952). The reaction mixture consisted of 2 mL phosphate buffer (pH 7.0), 0.95 mL hydrogen peroxide (0.019 M), and 0.05 mL supernatant, resulting in a total volume of 3 mL. Absorbance was recorded at 240 nm every 10 s for 1 min. One unit of CAT was defined as the quantity of enzymes required to decompose 1 mmol of peroxide per min, at 25 °C with pH 7.0. The results were expressed as units of CAT activity (mg/protein). Units of activity were calculated from the standard graph of H2O2. The results were expressed as catalase per unit/milligram of tissue.
Neurochemical Analysis
The levels of catecholamines—including DA, NE, 5-HT, and their metabolites, DOPAC, HVA, and 5-HIAA—were measured by high-performance liquid chromatography (HPLC) using an electrochemical detector (Patel et al. 2005). Waters standard system was used in the study; the system includes a high pressure isocratic pump, a 20-μL manual sample injector valve, a C18 reverse phase column, and an electrochemical detector. The mobile phase was sodium citrate buffer (pH 4.5)-acetonitrile (87:13, v/v), which consists of 10 mM citric acid, 25 mM NaH2PO4, 25 mM EDTA, and 2 mM 1-heptane sulfonic acid. Electrochemical conditions for the experiment were set at + 0.75 V with sensitivity range from 5 to 50 nA. Separation was achieved at a flow rate of 0.8 mL/min and samples of 20 μL each time were injected manually. On the day of the experiment, frozen brain samples were thawed and homogenized in a homogenizing solution containing 0.2 M perchloric acid. The homogenized samples were further centrifuged at 12,000g for 10 min. The supernatant was filtered through 0.22 μm nylon filters before being injected into the HPLC sample injector. Data were recorded and analyzed, and concentrations of neurotransmitters and their metabolites were calculated from the standard curve generated by using standard in a concentration range of 10–100 ng/mL (Patel et al. 2005).
Measurement of Neuroinflammatory Markers
Estimation of Tumor Necrosis Factor α
The TNF-α level was assessed using a rat TNF-α kit (R&D Systems, Minneapolis, MN, USA). The reagents and standard dilutions were prepared following the manufacturer’s suggestions. In brief, 50 μL of assay diluents were added to each well of the precoated microtiter plate, and 50 μL of standard or sample was then added in each well and gently mixed. The plate was covered with an adhesive strip and incubated for 2 h at room temperature; each well was then aspirated and washed with buffer, which was repeated a total of five times. The plate was then inverted and blotted against a clean paper towel; 100 μL of rat TNF conjugate was then added to each well and covered with a new adhesive strip: the plate was again incubated for 2 h at room temperature. Aspirations and washes were repeated as previously mentioned; 100 μL of substrate solution was then added to each well and incubated for 30 min at room temperature, protected from light; and 100 μL of stop solution was finally added to each well and the absorbance of each well was measured in an ELISA reader (Bio-Rad xMark) under 450 nm.
Estimation of Interleukin-6
IL-6 level was assessed using a quantikine rat IL-6 immunoassay kit (R&D Systems, Minneapolis, MN, USA). Reagents, standard solutions, controls, and samples were prepared following the kit’s instructions. Fifty microliters of assay diluents RD1–54 were added to each well, and 50 μL of standard, control, or sample was added in each well. It was gently mixed by tapping the plate frame for 1 min. Plates were covered with adhesive tape and incubated at room temperature for 2 h. Each well was aspirated and washed with buffer (400 μL) five times. Complete removal of liquid at each step was crucial. After the last wash, any residual washing buffer was removed by aspirating or decanting. Plates were inverted and blotted against clean paper towels; 100 μL of rat IL-6 conjugate was added to each well, covered with a new adhesive tape and incubated for 2 h at room temperature. Aspirations and washes were repeated as previously described. One hundred microliters of substrate solution was added to each well and incubated for 30 min at room temperature, protected from light, and 100 μL of stop solution was added to each well. Plates were mixed gently by tapping. Optical density was measured within 30 min using a microplate reader (Bio-Rad xMark) at 450 nm.
Measurement of Apoptotic Marker
Caspase-3 Colorimetric Assay
Caspase-3, also known as CPP-32, Yama, or apopain, is an intracellular cysteine protease. Normally, caspase-3 exists as a proenzyme; however, it is activated during the cascade of the events linked to apoptosis. The protease activity of the tissue lysates/homogenates can be evaluated by adding a caspase-specific peptide that is conjugated to the color reporter molecule p-nitroanaline (pNA). Caspase is able to cleave the peptide, resulting in the release of the chromophore pNA that can be measured spectrophotometrically at 405 nm. The caspase enzyme activity in the cell lysate/homogenate is directly related to the color reaction. The enzymatic reaction for caspase activity was accomplished by using R&D systems caspase-3 colorimetric kit.
Statistical Analysis
The data were presented as mean ± SEM. There are two experimental groups with different dosages of drug treatment. Therefore, the data were analyzed using a mixed repeated ANOVA to assess the differences between groups (control vs. RES) as well as among different dosage treatments. If the assumption of sphericity was not violated, evidenced by a nonsignificant Mauchly’s test (p > 0.05), we reported the output without adjustment. On the other hand, if the assumption of sphericity was violated, evidenced by a significant Mauchly’s test (p < 0.05), we reported the output using the Greenhouse-Geisser adjustment. Also, one-way ANOVA together with Tukey pairwise tests was used for post hoc comparison to examine the differences for both control and RES groups at various drug dosage treatments. p < 0.05 was considered as statistically significant.
Results
LT Treatment Reduced the RES-Induced Increases in Vacuous Chewing Movement Frequency
The effects of RES on VCM frequency are presented in Fig. 2a. RES treatment (1 mg/kg, every other day injection, in a total of three times) induced a significant increase in the VCM frequency (t test, C vs. R; p < 0.001). A mixed repeated ANOVA was conducted to assess the differences between groups (control vs. RES) and different dosage treatments in VCM frequency. The assumption of sphericity was not violated, evidenced by a nonsignificant Mauchly’s test (p = 0.71); therefore, we reported the output without adjustment. Our results indicated a significant interaction between groups (control vs. RES) and different dosages (no T, T30, T100, and T300), F(3, 36) = 71.02, p < 0.001. Results also indicated a significant main effect of dosage differences, F(3, 36) = 64.39, p < 0.001. There is also a significant difference between groups (control vs. RES, p < 0.001). Polynominal contrasts further indicated there was a significant linear trend, F(1, 12) = 259.19, p < 0.001. Examination of these means suggests that LT was effective in treating the increased VCM frequency induced by RES treatment; the higher the dosage of LT, the stronger the effect in decreasing VCM frequency. LT 30 mg/kg treatment reduced VCM frequency by 16.3% from 140.9 to 117.9 (times/15 min); LT 100 mg/kg treatment reduced VCM frequency by 52.2% from 140.9 to 67.3 (times/15 min), and LT 300 mg/kg treatment reduced VCM frequency by 65.3% from 140.9 to 48.9 (times/15 min). However, LT treatment was not able to completely block the increased frequency of VCM induced by RES; dosages of 300 mg/kg LT treatments still had significant higher VCM frequency (p < 0.001) compared to the C group. On the other hand, LT treatment was not able to alter VCM frequency in the control group.
LT dose-dependently blocked most of the increased orofacial dyskinesia (OD) behaviors in R-treated rats. The frequencies of a vacuous chewing movement (VCM), b tongue protrusion (TP), and c the duration of facial twitching (FT) were used as the output measurements to assess RES-induced OD behavioral characteristics. Data were presented as mean ± SEM (n = 7). C: control; R: reserpine-treated (3 injections of 1 mg/kg); T30: 30 mg/kg LT without reserpine; T100: 100 mg/kg LT without reserpine; T300: 300 mg/kg LT without reserpine; T30 + R: T 30 mg/kg + reserpine treatment; T100 + R: T 100 mg/kg + reserpine treatment; T300 + R: T 300 mg/kg + reserpine treatment. ***p < 0.001 as compared with C; ###p < 0.001 as compared with R. The data were analyzed using a mixed repeated ANOVA and post hoc with one-way ANOVA together with Tukey pairwise tests
LT Treatment Prevented the RES-Induced Increases in Tongue Protrusion Frequency
The effects of RES on TP frequency are shown in Fig. 2b. RES treatment induced a significant increase in the TP frequency (t test, C vs. R; p < 0.001). A mixed repeated ANOVA was conducted to assess whether there were group (control vs. RES) and dosage differences in TP frequency. The assumption of sphericity was violated, evidenced by a significant Mauchly’s test (p = 0.01); therefore, we reported the output adjusted with Greenhouse-Geisser epsilons. Our results indicated a significant interaction between groups (control vs. RES) and different dosages (no T, T30, T100, and T300), F(1.78, 21.59) = 42.97, p < 0.001. Results also indicated a significant main effect of dosage differences, F(1.78, 21.59) = 51.07, p < 0.001. There is also a significant difference between groups (control vs. RES, p < 0.001). Polynominal contrasts further indicated there was a significant linear trend, F(1, 12) = 76.47, p < 0.001. Examination of these means suggests LT was effective in reducing TP frequency; the higher the dosage of LT, the stronger the effects in treating TP frequency. However, it reached its plateau at T100, as there was no difference between T100 and T300. We used one-way ANOVA to examine the differences between the control and RES at various LT dosages, and we found LT had no effect on TP frequency in the control group; however, the increased frequency of TP induced by RES was significantly reduced 42.0% from 21.4 to 12.4 (times/15 min) by LT 30 mg/kg treatment and completely blocked by LT 100 and LT 300 mg/kg treatment, resulting in no significant difference between the control group and the groups of T100 + R and T300 + R (p = 0.078 and 0.394, respectively).
LT Treatment Blocked the RES-Induced Increases in the Duration of Facial Twitching
The effects of RES on the duration of FT are shown in Fig. 2c. RES treatment induced a significant increase in the duration of FT (t test, C vs. R; p < 0.001). A mixed repeated ANOVA analysis indicated a significant interaction between group (control vs. RES) and dosage (no T, T30, T100, and T300), F(3, 36) = 72.74, p < 0.001. Results also indicated a significant main effect of dosage differences, F(3, 36) = 77.09, p < 0.001. There is also a significant difference between groups (control vs. RES, p < 0.001). Polynominal contrasts further indicated there was a significant linear trend, F(1, 12) = 158.74, p < 0.001. Examination of these means suggests LT was effective in treating increased FT; the higher the dosage of LT, the better the effects in reducing FT, and it reached a plateau at T100. We further used one-way ANOVA as the post hoc test to examine the difference between the control and RES at various LT dosages, and we found LT had no effect on FT duration in control rats; however, the increased duration of FT induced by RES was significantly decreased 26.8% from 81.4 to 59.6 (s) by T 30 mg/kg treatment (p < 0.001) and completely prevented by LT 100 and LT 300 mg/kg treatment (p < 0.001), resulting in no significant differences between the control group and the groups of T100 + R and T300 + R (p = 0.1 and 0.442, respectively).
LT Treatment Inhibited the RES-Induced Increases in Striatal Lipid Peroxide Production
The effects of RES on the TBARS production in rat striatum are shown in Fig. 3. RES treatment induced a significant increase in the TBARS level in rat striatum from 31.0 ± 3.5 to 54.4 ± 3.6 (nmol/mg protein, t test, C vs. R; p < 0.001). A mixed repeated ANOVA analysis indicated a significant interaction between group (control vs. RES) and dosage (no T, T30, T100, and T300), F(3, 36) = 15.22, p < 0.001. Results also indicated a significant main effect of dosage differences, F(3, 36) = 20.84, p < 0.001. There is also a significant difference between groups (control vs. RES, p < 0.001). Polynominal contrasts further indicated there was a significant linear trend, F(1, 12) = 42.35, p < 0.001. Examination of these means suggests LT was effective in reducing TBARS levels; the higher the dosage of LT, the better the effects in reducing TBARS levels, and it reached a plateau at T100. One-way ANOVA post hoc tests indicated the increased TBARS level, induced by RES in rat striatum, was partially but significantly inhibited by LT 30 mg/kg treatment to the level of 43.7 ± 6.9 (nmol/mg protein) (p < 0.001) and completely inhibited by LT 100 and 300 mg/kg treatment (p < 0.001), resulting in no significant difference between the control group and the groups of T100 + R and T300 + R with the TBARS levels of 32.0 ± 7.5 and 29.9 ± 6.8 (nmol/mg protein), respectively (p = 0.067 and 0.183, respectively).
LT dose-dependently reduced the R-induced striatal oxidative stress. TBARS level in rat striatum was used as an output measurement to assess RES-induced dysfunctions. Data were presented as mean ± SEM (n = 7). C: control; R: reserpine-treated; T30: 30 mg/kg LT without reserpine; T100: 100 mg/kg LT without reserpine; T300: 300 mg/kg LT without reserpine; T30 + R: T 30 mg/kg + reserpine treatment; T100 + R: T 100 mg/kg + reserpine treatment; T300 + R: T 300 mg/kg + reserpine treatment. ***p < 0.001 as compared with C; ###p < 0.001 as compared with R. The data were analyzed using a mixed repeated ANOVA, and post hoc with one-way ANOVA together with Tukey pairwise tests
LT Treatment Prevented the RES-Induced Decreases in Striatal Antioxidation Power
The effects of RES on the levels of GSH and protective enzymes such as SOD and CAT in rat striatum are shown in Fig. 4a–c. RES treatment induced a significant decrease in the levels of GSH, SOD, and CAT in rat striatum (t test in each subfigure; C vs. R, p < 0.001). A mixed repeated ANOVA was conducted to assess whether there were group (control vs. RES) and dosage differences in GSH, SOD, and CAT levels. Our results indicated a significant interaction between group (control vs. RES) and dosage (no T, T30, T100, and T300); F(3, 36) = 66.09, p < 0.001 for GSH experiment; F(3, 36) = 28.39, p < 0.001 for SOD experiment; F(3, 36) = 50.32, p < 0.001 for CAT experiment. Results also indicated a significant main effect of dosage differences [GSH: F(3, 36) = 103.4, p < 0.001; SOD: F(3, 36) = 30.30, p < 0.001; CAT: F(3, 36) = 43.86, p < 0.001]. There is also a significant difference between groups (control vs. RES, p < 0.001). Polynominal contrasts further indicated there was a significant linear trend [GSH: F(1, 12) = 166.34, p < 0.001; SOD: F(1, 12) = 74.07, p < 0.001; CAT: F(1, 12) = 96.65, p < 0.001]. One-way ANOVA post hoc tests indicated that these reduced levels of GSH, SOD, and CAT in rat striatum caused by RES treatment were partially recovered by LT 30 mg/kg treatment (p < 0.001) and completely returned to control level by LT 100 and 300 mg/kg treatments, resulting in no statistical difference to the control group. The p values for the control group versus T300 + R in GSH, SOD, and CAT levels were 0.943, 0.151, and 0.914 respectively.
LT dose-dependently prevented the decreased striatal antioxidation power in R-treated rats. The levels of a GSH, b SOD, and c CAT in rat striatum were used as output measurements to assess RES-induced dysfunctions. Data were presented as mean ± SEM (n = 7). C: control; R: reserpine-treated; T30: 30 mg/kg LT without reserpine; T100: 100 mg/kg LT without reserpine; T300: 300 mg/kg LT without reserpine; T30 + R: T 30 mg/kg + reserpine treatment; T100 + R: T 100 mg/kg + reserpine treatment; T300 + R: T 300 mg/kg + reserpine treatment. ***p < 0.001 as compared with C; ###p < 0.001 as compared with R. The data were analyzed using a mixed repeated ANOVA and post hoc with one-way ANOVA together with Tukey pairwise tests
LT Treatment Prevented the RES-Induced Alterations in Striatal Catecholamine Levels
The effects of RES on the levels of catecholamines including DA, NE, 5-HT, and their metabolites, DOPAC, HVA, and 5-HIAA, in rat striatum were measured by HPLC (Patel et al. 2005), and their results are shown in Fig. 5a–f. RES treatment induced significant decreases in the levels for DA, NE, 5-HT, and 5-HIAA in rat striatum (t test, C vs. R, p < 0.001), and it also induced significant increases in the levels for DOPAC and HVA (t test, C vs. R, p < 0.001). A mixed repeated ANOVA was conducted to assess whether there were group (control vs. RES) and dosage differences in the levels of these catecholamines. Our results indicated a significant interaction between groups (C vs. R) and different LT dosages (no T, T30, T100, and T300) [DA: F(3, 36) = 21.19, p < 0.001; NE: F(3, 36) = 43.27, p < 0.001; 5-HT: F(3, 36) = 25.69, p < 0.001; DOPAC: F(2.05, 24.56) = 9.40, p = 0.001; HVA: F(3, 36) = 14.70, p < 0.001; 5-HIAA: F(3, 36) = 13.56, p < 0.001]. Results also indicated a significant main effect of dosage differences [DA: F(3, 36) = 27.39, p < 0.001; NE: F(3, 36) = 56.38, p < 0.001; 5-HT: F(3, 36) = 33.67, p < 0.001; DOPAC: F(2.05, 24.56) = 10.51, p < 0.001; HVA: F(3, 36) = 14.25, p < 0.001; 5-HIAA: F(3, 36) = 12.34, p < 0.001]. Polynominal contrasts further indicated there was a significant linear trend for DA, NE, 5-HT, and 5-HIAA [DA: F(1, 12) = 48.57, p < 0.001; NE: F(1, 12) = 137.14, p < 0.001; 5-HT: F(1, 12) = 71.74, p < 0.001; 5-HIAA: F(1, 12) = 45.34, p < 0.001] but not for DOPAC and HVA [DOPAC: F(1, 12) = 2.34, p = 0.152; HVA: F(1, 12) = 1.52, p = 0.241]. Examination of these means suggests LT was effective in enhancing the levels of DA, NE, 5-HT, and 5-HIAA in rat striatum. One-way ANOVA post hoc tests indicated the decreased DA, NE, 5-HT, and 5-HIAA levels caused by RES in rat striatum were dose-dependent but only partially enhanced, by LT 30 and 100 mg/kg treatments (p < 0.001). The LT treatment reached its plateau to enhance these catecholamine neurotransmitter markers at LT 100 mg/kg as the LT 300-mg/kg treatment was not able to further increase their levels in rat striatum. The data also indicated that LT treatment, even at the highest dosage of LT 300 mg/kg, was not able to completely block the decreased levels of catecholamine from RES treatment (C vs. T300 + R, p < 0.001).
LT restored the striatal catecholamine levels in R-treated rats. The levels of a DA, b NE, c 5-HT, d DOPAC, e HVA, and f 5-HIAA in rat striatum were used as output measurements to assess RES-induced dysfunctions. Data were presented as mean ± SEM (n = 7). C: control; R: reserpine-treated; T30: 30 mg/kg LT without reserpine; T100: 100 mg/kg LT without reserpine; T300: 300 mg/kg LT without reserpine; T30 + R: T 30 mg/kg + reserpine treatment; T100 + R: T 100 mg/kg + reserpine treatment; T300 + R: T 300 mg/kg + reserpine treatment. ***p < 0.001 as compared with C; ###p < 0.001 as compared with R. The data were analyzed using a mixed repeated ANOVA and post hoc with one-way ANOVA together with Tukey pairwise tests
LT Treatment Inhibited the RES-Induced Increases in Striatal Neuroinflammatory and Apoptotic Markers
The effects of RES on the levels of neuroinflammatory (TNF-α and IL-6) and apoptotic (caspase-3) markers in rat striatum are shown in Fig. 6a–c. RES treatment induced significant increases in the levels for TNF-α, IL-6, and caspase-3 in rat striatum (t test in each subfigure, C vs. R, p < 0.001). A mixed repeated ANOVA was conducted to assess whether there were group (control vs. RES) and dosage differences in the levels of TNF-α, IL-6, and caspase-3. Our results indicated a significant interaction between groups (C vs. R) and different LT dosages (no T, T30, T100, and T300) [TNF-α: F(3, 36) = 36.84, p < 0.001; IL-6: F(3, 36) = 24.04, p < 0.001; caspase-3: F(3, 36) = 19.12, p < 0.001]. Results also indicated a significant main effect of dosage differences [TNF-α: F(3, 36) = 29.43, p < 0.001; IL-6: F(3, 36) = 23.27, p < 0.001; caspase-3: F(3, 36) = 17.25, p < 0.001]. Polynominal contrasts further indicated there was a significant linear trend [TNF-α: F(1, 12) = 74.76, p < 0.001; IL-6: F(1, 12) = 44.99, p < 0.001; caspase-3: F(1, 12) = 26.05, p < 0.001]. Examination of these means suggests LT was effective in reducing the levels of TNF-α, IL-6, and caspase-3 in rat striatum. One-way ANOVA post hoc tests indicated the increased TNF-α, IL-6, and caspase-3 levels caused by RES in rat striatum were dose-dependent but only partially inhibited, by LT 30 and 100 mg/kg treatments (p < 0.001). The LT treatment reached its plateau to inhibit these neuroinflammatory and apoptotic markers at LT 100 mg/kg as the LT 300-mg/kg treatment was not able to further reduce these neuroinflammatory and apoptotic markers in rat striatum. The data also indicated that LT treatment, even at the highest dosage of LT 300 mg/kg, was not able to completely block the increased levels of neuroinflammatory and apoptotic markers resulting from RES treatment (C vs. T300 + R, p < 0.001).
LT dose-dependently blocked the increased striatal neuroinflammatory and apoptotic markers in R-treated rats. The levels of a TNF-α, b IL-6, and c caspase-3 in rat striatum were used as output measurements to assess RES-induced dysfunctions. Data were transformed into percentage changes from the control and they were presented as mean ± SEM (n = 7). C: control; R: reserpine-treated; T30: 30 mg/kg LT without reserpine; T100: 100 mg/kg LT without reserpine; T300: 300 mg/kg LT without reserpine; T30 + R: T 30 mg/kg + reserpine treatment; T100 + R: T 100 mg/kg + reserpine treatment; T300 + R: T 300 mg/kg + reserpine treatment. ***p < 0.001 as compared with C; ###p < 0.001 as compared with R. The data were analyzed using a mixed repeated ANOVA and post hoc with one-way ANOVA together with Tukey pairwise tests
Discussion
In this study, we have shown that RES treatment induced OD behaviors in rats, as well as elevating the levels for LPO, TNF-α, IL-6, and caspase-3, as well as diminishing the antioxidation power and catecholamines in rat striatum. However, the goal of this study was to highlight the protective effects of LT against RES-induced behavioral dysfunction, oxidative stress, neurochemical deficiency, neuroinflammation (IL-6 and TNF-α), and apoptotic pathway (caspase-3) activation. Our results indicated that LT has strong protective effects against RES-induced pathophysiological dysfunction; therefore, it would be beneficial to treat OD or clinical human TD.
Not only do the RES-induced OD characteristics strongly resemble the symptoms of TD, but RES has also been linked to human TD development (Burger et al. 2003; Nade et al. 2013; Kronbauer et al. 2015; Wang et al. 2015; de Freitas et al. 2016). Consistent with previous studies, we found that RES treatment significantly increased the frequency of VCM and T, and the duration of FT, suggesting a neurotoxic effect caused by RES (Calvente et al. 2002; Wang et al. 2015). Our data also showed that RES increased LPO status—as indicated by the increased TBARS level in the striatum—suggesting that free radicals may partially underlie the mechanisms of OD development. Moreover, RES treatment decreased the levels of GSH (an endogenous antioxidant), SOD, and catalase (cellular antioxidant enzymes), further supporting the possible free radical toxicity in RES-induced OD. Many reports have shown that RES-induced OD is tightly associated with the striatal oxidative stress state (Teixeira et al. 2009; Kronbauer et al. 2015; Wang et al. 2015).
RES also causes disruption in neurotransmission by affecting the vesicular monoamine transporter (VMAT) to restrict the storage of DA in synaptic vesicles, resulting in an accelerated rate of cytosolic DA oxidative metabolism by monoamine oxidase (MAO) (Fuentes et al. 2007; Kronbauer et al. 2015; de Freitas et al. 2016). With DA metabolism accelerated, the formation of reactive metabolites and hydrogen peroxide was augmented, resulting in an increased oxidative stress in dopaminergic neurons (Burger et al. 2003; Bilska et al. 2007; Teixeira et al. 2009; Nade et al. 2013). Furthermore, the O-quinone aminochrome formed by the autoxidation of DA could lose one more electron to become a leukoaminochrome O-semiquinone radical. This free radical has been considered one of the major sources of endogenous reactive species involved with many neurodegenerative diseases (Paris et al. 2005; Fuentes et al. 2007; Teixeira et al. 2009). Since monoamines are plentiful in the basal ganglia including the striatum, higher susceptibility to free radical damage to increase oxidative stress would be anticipated (Lohr et al. 2003). Moreover, the increased DA turnover along with increased glutamatergic transmission after RES treatment further enhanced the free radical generation to add more oxidative stress. The increased oxidative stress was closely related to RES treatment and OD development as well as neurobiological alteration within the basal ganglia (Kronbauer et al. 2015; Cunha et al. 2016; de Freitas et al. 2016). In addition, alteration in striatal neurochemistry, such as insufficiencies in monoamines, including DA, NE, and 5-HT, has also been reported to occur in OD (Cunha et al. 2016; Jamwal and Kumar 2017): this is consistent with our results of reduced levels of DA, NE, 5-HT, and 5-HIAA catecholamines, whereas their metabolite levels of DOPAC and HVA in the striatum increased after RES treatment. These results were consistent with previous reports, suggesting the implication of neurochemical deficiency in rat striatum in RES-induced striatal damage, resulting in the development of OD (Cunha et al. 2016; de Freitas et al. 2016). DA, together with other neurotransmitters, is crucial in managing coordinated body movements—the altered DA level induced by RES treatment was associated with the disruption of the balance with other neurotransmitters, e.g., NE and 5-HT, especially affecting the basal ganglia neuronal circuitry (Jamwal and Kumar 2017). These results agreed with our observed behavioral impairment after RES treatment.
Excess oxidative stress frequently activates the inflammatory process and releases inflammatory mediators, such as TNF-α and IL-6, to initiate the apoptotic pathway, which has been suggested as the key mechanism for neuronal cell death (Selvakumar et al. 2012; Datta et al. 2016). In this study, we observed increased levels for TNF-α and IL-6 in the striatum from RES-treated rats. This result was consistent with a previous report (Hanff et al. 2010), suggesting the implication of neuroinflammatory cascades in RES-induced neurotoxicity, such as striatal damage and leading to the development of OD (Datta et al. 2016). Additionally, caspase-3 has been linked to many biological and morphological features of apoptosis (Túnez et al. 2006; Kumar et al. 2011). The finding of increased levels of caspase-3 after RES treatment in this study, therefore, supports the involvement of apoptotic cascade in the OD pathology in rat striatum, and this result is also consistent with the previous reports that animal models with OD development have an increased apoptosis and a reduced number of neural cell in brains (Andreassen et al. 1998; Kelley and Roberts 2004; Santos et al. 2013). In the current RES treatment OD animal model, we are the first group to report the increased levels for both TNF-α and IL-6, markers of neuroinflammation, and associated with the increased caspase-3 level, markers of apoptosis, in rat striatum.
Our results in the current study suggested that RES-treated rats had a high oxidative stress state, catecholamine deficiency, and increased levels of neuroinflammation and apoptosis in the striatum, providing us a practical therapeutic target. Therefore, decreasing excessive free radicals, increasing antioxidative factors, preventing neurochemical deficiency, or stopping inflammatory and apoptotic cascades may be possible to disrupt the development of the OD caused by RES-induced oxidative injury (Burger et al. 2003; Faria et al. 2005; Wang et al. 2015; Cunha et al. 2016).
LT has been reported to have strong antioxidative and anti-inflammatory effects and to also be able to prevent neurotransmitter deficiency (Kakuda 2011; Thangarajan et al. 2014; Sumathi et al. 2015; Pérez-Vargas et al. 2016; Jamwal and Kumar 2017). Therefore, LT would be anticipated to have the properties to reduce oxidative damage, neurotransmitter deficiency, and neuroinflammation in the striatum. In our findings, LT was able to dose-dependently reduce the levels of TBARS, TNF-α, IL-6, and caspase-3 that were observed to be increased in RES-treated rat striatum, and LT was able to dose-dependently increase the levels of GSH, SOD, CAT, DA, NE, and 5-HT. Those were observed to be decreased in the rat striatum after RES treatment, suggesting LT’s multifunctions are linked with many pathophysiological pathways. These properties may underlie the mechanisms of LT in preventing RES-induced OD as indicated by our behavioral examination. Other reports have shown a protective role of GSH and protective enzymes such as SOD and CAT, as well as catecholamine level normalization to inhibit the development of OD (Burger et al. 2003; Abílio et al. 2004; Naidu et al. 2004; Faria et al. 2005; Patil et al. 2012a, b; Wang et al. 2015; Jamwal and Kumar 2017). Thus, at least in part, the results of the antidyskinetic properties of LT in RES-treated rats were attributed to its ability to clear excessive free radicals, enhance antioxidative factors, normalize neurotransmitters, and inhibit inflammation and apoptotic cascades in the striatum of RES-treated rats.
In this study, however, our data indicated that LT was not able to completely block the increased levels of TNF-α, IL-6, caspase-3, and catecholamines as well as the behavioral alterations induced by RES. In contrast, LT was able to completely prevent the increased TBARS level induced by RES. These results suggest that neuroinflammation, apoptosis, neurotransmitter deficiency, and behavioral alterations induced by RES are not entirely caused by free radical production. It could also be affected by other mechanisms, such as the many different classes of behavioral manifestations induced by RES like different modulations by the NMDA receptor blocker, MK-801 (Dutra et al. 2002; Cunha et al. 2016). It would also be possible that OD was caused primarily by free radicals formed during catecholamine metabolism, including dopamine quinones and hydrogen peroxide produced by MAO (Paris et al. 2005; Fuentes et al. 2007), and sequentially, these reactive species promote lipoperoxidation.
Conclusions
In summary, our findings suggest the potential involvement of antioxidation, neurochemical deficiency prevention, antineuroinflammatory, and apoptotic cascades underlying the neuroprotective effects of LT and provide evidence of LT’s therapeutic value in treating OD in an animal model, presumably also to a beneficial effect in treating clinically relevant human TD.
Abbreviations
- CAT:
-
catalase
- DA:
-
dopamine
- FT:
-
facial twitching
- GSH:
-
glutathione
- IL-6:
-
interleukin-6
- LPO:
-
lipid peroxidation
- MAO:
-
monoamine oxidase
- NE:
-
norepinephrine
- OD:
-
orofacial dyskinesia
- PD:
-
Parkinson disease
- RES:
-
reserpine
- SOD:
-
superoxide dismutase
- LT:
-
L-theanine
- TBARS:
-
thiobarbituric acid-reactive substance
- TD:
-
tardive dyskinesia
- TNF-α:
-
tumor necrosis factor α
- TP:
-
tongue protrusion
- VCM:
-
vacuous chewing movements
- VMAT:
-
vesicular monoamine transporter
- 5-HT:
-
serotonin
References
Abílio VC, Silva RH, Carvalho RC, Grassl C, Calzavara MB, Registro S, D’Almeida V, Ribeiro Rde A, Frussa-Filho R (2004) Important role of striatal catalase in aging- and reserpine-induced oral dyskinesia. Neuropharmacology 47(2):263–272
Andreassen OA, Ferrante RJ, Beal MF, Jørgensen HA (1998) Oral dyskinesias and striatal lesions in rats after long-term co-treatment with haloperidol and 3-nitropropionic acid. Neuroscience 87(3):639–648
Beers RF Jr, Sizer IW (1952) A spectrophotometric method for measuring the breakdown of hydrogen peroxide by catalase. J Biol Chem 195(1):133–140
Bilska A, Dubiel M, Sokołowska-Jezewicz M, Lorenc-Koci E, Włodek L (2007) Alpha-lipoic acid differently affects the reserpine-induced oxidative stress in the striatum and prefrontal cortex of rat brain. Neuroscience 146(4):1758–1771
Burger ME, Alves A, Callegari L, Athayde FR, Nogueira CW, Zeni G, Rocha JB (2003) Ebselen attenuates reserpine-induced orofacial dyskinesia and oxidative stress in rat striatum. Prog Neuro-Psychopharmacol Biol Psychiatry 27(1):135–140
Calvente PR, Araujo CC, Bergamo M, Abilio VC, D’Almeida V, Ribeiro Rde A, Frussa FR (2002) The mitochondrial toxin 3-nitropropionic acid aggravates reserpine-induced oral dyskinesia in rats. Prog Neuro-Psychopharmacol Biol Psychiatry 26(2):401–405
Cunha AS, Matheus FC, Moretti M, Sampaio TB, Poli A, Santos DB, Colle D, Cunha MP, Blum-Silva CH, Sandjo LP, Reginatto FH, Rodrigues AL, Farina M, Prediger RD (2016) Agmatine attenuates reserpine-induced oral dyskinesia in mice: role of oxidative stress, nitric oxide and glutamate NMDA receptors. Behav Brain Res 312:64–76
Datta S, Jamwal S, Deshmukh R, Kumar P (2016) Beneficial effects of lycopene against haloperidol induced orofacial dyskinesia in rats: possible neurotransmitters and neuroinflammation modulation. Eur J Pharmacol 771:229–235
Davies DL, Shepherd M (1955) Reserpine in the treatment of anxious and depressed patients. Lancet 269(6881):117–120
de Freitas CM, Busanello A, Schaffer LF, Peroza LR, Krum BN, Leal CQ, Ceretta AP, da Rocha JB, Fachinetto R (2016) Behavioral and neurochemical effects induced by reserpine in mice. Psychopharmacology 233(3):457–467
Durlach J (1956) Treatment of emaciation with reserpine. Concours Med 78(7):725–728
Dutra RC, Andreazza AP, Andreatini R, Tufik S, Vital MA (2002) Behavioral effects of MK-801 on reserpine-treated mice. Prog Neuro-Psychopharmacol Biol Psychiatry 26(3):487–495
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77
Faria RR, Abílio VC, Grassl C, Chinen CC, Negrão LT, de Castro JP, Fukushiro DF, Rodrigues MS, Gomes PH, Registro S, de Carvalho Rde C, D’Almeida V, Silva RH, Ribeiro Rde A, Frussa-Filho R (2005) Beneficial effects of vitamin C and vitamin E on reserpine-induced oral dyskinesia in rats: critical role of striatal catalase activity. Neuropharmacology 48(7):993–1001
Fernandes VS, Santos JR, Leão AH, Medeiros AM, Melo TG, Izídio GS, Cabral A, Ribeiro RA, Abílio VC, Ribeiro AM, Silva RH (2012) Repeated treatment with a low dose of reserpine as a progressive model of Parkinson’s disease. Behav Brain Res 231(1):154–163
Fuentes P, Paris I, Nassif M, Caviedes P, Segura-Aguilar J (2007) Inhibition of VMAT- 2 and DT-diaphorase induced cell death in a substantia nigra-derived cell line—an experimental cell model for dopamine toxicity studies. Chem Res Toxicol 20(5):776–783
Hanff TC, Furst SJ, Minor TR (2010) Biochemical and anatomical substrates of depression and sickness behavior. J Psychiatry Relat Sci 47(1):64–71
Hashimoto M, Tanabe Y, Fujii Y, Kikuta T, Shibata H, Shido O (2005) Chronic administration of docosahexaenoic acid ameliorates the impairment of spatial cognition learning ability in amyloid beta-infused rats. J Nutr 135(3):549–555
Huang NY, Kostrzewa RM, Li C, Perry KW, Fuller RW (1997) Persistent spontaneous oral dyskinesias in haloperidol-withdrawn rats neonatally lesioned with 6-hydroxydopamine: absence of an association with the Bmax for [3H]raclopride binding to neostriatal homogenates. J Pharmacol Exp Ther 280(1):268–276
Ishibashi T, Ohno Y (2004) Antiparkinsonian actions of a selective 5-HT1A agonist, tandospirone, in rats. Biogen Amines 18:329–338
Jamwal S, Kumar P (2017) L-theanine, a component of green tea prevents 3-nitropropionic acid (3-NP)-induced striatal toxicity by modulating nitric oxide pathway. Mol Neurobiol 54(3):2327–2337
Kakuda T (2011) Neuroprotective effects of theanine and its preventive effects on cognitive dysfunction. Pharmacol Res 64(2):162–168
Kelley JJ, Roberts RC (2004) Effects of haloperidol on cholinergic striatal interneurons: relationship to oral dyskinesias. J Neural Transm 111(8):1075–1091
Kostrzewa RM, Huang NY, Kostrzewa JP, Nowak P, Brus R (2007) Modeling tardive dyskinesia: predictive 5-HT2C receptor antagonist treatment. Neurotox Res 11(1):41–50
Kronbauer M, Segat HJ, De David Antoniazzi CT, Roversi K, Roversi K, Pase CS, Barcelos RC, Burger ME (2015) Magnesium supplementation prevents and reverses experimentally induced movement disturbances in rats: biochemical and behavioral parameters. Biol Trace Elem Res 166(2):163–172
Kumar P, Kalonia H, Kumar A (2011) Role of LOX/COX pathways in 3-nitropropionic acid-induced Huntington’s disease-like symptoms in rats: protective effect of licofelone. Br J Pharmacol 164(2b):644–654
Lohr JB, Kuczenski R, Niculescu AB (2003) Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17(1):47–62
Misra HP, Fridovich I (1972) The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247(10):3170–3175
Nade VS, Shendye NV, Kawale LA, Patil NR, Khatri ML (2013) Protective effect of nebivolol on reserpine-induced neurobehavioral and biochemical alterations in rats. Neurochem Int 63(4):316–321
Naidu PS, Singh A, Kulkarni SK (2004) Reversal of reserpine-induced orofacial dyskinesia and cognitive dysfunction by quercetin. Pharmacology 70(2):59–67
Neisewander JL, Castañeda E, Davis DA (1994) Dose-dependent differences in the development of reserpine-induced oral dyskinesia in rats: support for a model of tardive dyskinesia. Psychopharmacology 116(1):79–84
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358
Paris I, Martinez-Alvarado P, Cárdenas S, Perez-Pastene C, Graumann R, Fuentes P, Olea-Azar C, Caviedes P, Segura-Aguilar J (2005) Dopamine-dependent iron toxicity in cells derived from rat hypothalamus. Chem Res Toxicol 18(3):415–419
Patel BA, Arundell M, Parker KH, Yeoman MS, O’Hare D (2005) Simple and rapid determination of serotonin and catecholamines in biological tissue using high-performance liquid chromatography with electrochemical detection. J Chromatogr B Analyt Technol Biomed Life Sci 818(2):269–276
Patil R, Dhawale K, Gound H, Gadakh R (2012a) Protective effect of leaves of Murraya koenigii on reserpine-induced orofacial dyskinesia. Iran J Pharm Res 11(2):635–641
Patil RA, Hiray YA, Kasture SB (2012b) Reversal of reserpine-induced orofacial dyskinesia and catalepsy by Nardostachys jatamansi. Indian J Pharmacol 44(3):340–344
Pérez-Vargas JE, Zarco N, Vergara P, Shibayama M, Segovia J, Tsutsumi V, Muriel P (2016) l-Theanine prevents carbon tetrachloride-induced liver fibrosis via inhibition of nuclear factor κB and down-regulation of transforming growth factor β and connective tissue growth factor. Hum Exp Toxicol 35(2):135–146
Santos JR, Cunha JA, Dierschnabel AL, Campêlo CL, Leão AH, Silva AF, Engelberth RC, Izídio GS, Cavalcante JS, Abílio VC, Ribeiro AM, Silva RH (2013) Cognitive, motor and tyrosine hydroxylase temporal impairment in a model of parkinsonism induced by reserpine. Behav Brain Res 253:68–77
Selvakumar G, Vijayraja D, Krishnamoorthy D, Manivasagam T (2012) Morin attenuates haloperidol induced tardive dyskinesia and oxidative stress in mice. J Nat Sci Res 8(2):153–165
Sumathi T, Shobana C, Thangarajeswari M, Usha R (2015) Protective effect of L-theanine against aluminium induced neurotoxicity in cerebral cortex, hippocampus and cerebellum of rat brain—histopathological, and biochemical approach. Drug Chem Toxicol 38(1):22–231
Teixeira AM, Reckziegel P, Müller L, Pereira RP, Roos DH, Rocha JB, Bürger ME (2009) Intense exercise potentiates oxidative stress in striatum of reserpine-treated animals. Pharmacol Biochem Behav 92(2):231–235
Terashima T, Takido J, Yokogoshi H (1999) Time-dependent changes of amino acids in the serum, liver, brain and urine of rats administered with theanine. Biosci Biotechnol Biochem 63(4):615–618
Thangarajan S, Deivasigamani A, Natarajan SS, Krishnan P, Mohanan SK (2014) Neuroprotective activity of L-theanine on 3-nitropropionic acid-induced neurotoxicity in rat striatum. Int J Neurosci 124(9):673–684
Túnez I, Collado JA, Medina FJ, Peña J, Del C, Muñoz M, Jimena I, Franco F, Rueda I, Feijóo M, Muntané J, Montilla P (2006) 17 eta-Estradiol may affect vulnerability of striatum in a 3-nitropropionic acid-induced experimental model of Huntington’s disease in ovariectomized rats. Neurochem Int 48(5):367–373
Wang MH, Lin RF, Tseng HC, Soung HS, Chang KC, Tsai CC (2015) (−)Epigallocatechin-3-gallate attenuates reserpine-induced orofacial dyskinesia and oxidative stress in rat striatum. Pharmacol Biochem Behav 131:71–76
Yin C, Gou L, Liu Y, Yin X, Zhang L, Jia G, Zhuang X (2011) Antidepressant-like effects of L-theanine in the forced swim and tail suspension tests in mice. Phytother Res 25(11):1636–1639
Yokogoshi H, Kato Y, Sagesaka YM, Takihara-Matsuura T, Kakuda T, Takeuchi N (1995) Reduction effect of theanine on blood pressure and brain 5-hydroxyindoles in spontaneously hypertensive rats. Biosci Biotechnol Biochem 59(4):615–618
Zhang G, Miura Y, Yagasaki K (2002) Effects of dietary powdered green tea and theanine on tumor growth and endogenous hyperlipidemia in hepatoma-bearing rats. Biosci Biotechnol Biochem 66(4):711–716
Zheng G, Sayama K, Okubo T, Juneja LR, Oguni I (2004) Anti-obesity effects of three major components of green tea, catechins, caffeine and theanine, in mice. In Vivo 18(1):55–62
Zukhurova M, Prosvirnina M, Daineko A, Simanenkova A, Petrishchev N, Sonin D, Galagudza M, Shamtsyan M, Juneja LR, Vlasov T (2013) L-theanine administration results in neuroprotection and prevents glutamate receptor agonist-mediated injury in the rat model of cerebral ischemia-reperfusion. Phytother Res 27(9):1282–1287
Acknowledgements
The authors thank Persistent BioMed Editing services located in Philadelphia, USA, for their valuable editing and proofreading of the current manuscript.
Funding
This study was supported by the Yuan-Shan Br. of Taipei Veteran General Hospital (YSVH-10505), Mackay Memorial Hospital (MMH-105-69), and Shin Kong Wu Ho-Su Memorial Hospital (SKH-8302-104-DR-24).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Soung, HS., Wang, MH., Chang, KC. et al. L-Theanine Decreases Orofacial Dyskinesia Induced by Reserpine in Rats. Neurotox Res 34, 375–387 (2018). https://doi.org/10.1007/s12640-018-9897-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-018-9897-z