Abstract
Introduction and hypothesis
Pelvic floor disorders (PFD), including urinary incontinence, anal incontinence, and pelvic organ prolapse, are common and have a negative effect on the quality of life of women. Treatment is associated with morbidity and may not be totally satisfactory. Prevention of PFDs, when possible, should be a primary goal. The purpose of this paper is to summarise the current literature and give an evidence-based review of the prevention of PFDs
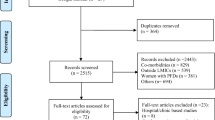
Methods
A working subcommittee from the International Urogynecological Association (IUGA) Research and Development (R&D) Committee was formed. An initial document addressing the prevention of PFDs was drafted, based on a review of the English-language literature. After evaluation by the entire IUGA R&D Committee, revisions were made. The final document represents the IUGA R&D Committee Opinion on the prevention of PFDs.
Results
This R&D Committee Opinion reviews the literature on the prevention of PFDs and summarises the findings with evidence-based recommendations.
Conclusions
Pelvic floor disorders have a long latency, and may go through periods of remission, thus making causality difficult to confirm. Nevertheless, prevention strategies targeting modifiable risk factors should be incorporated into clinical practice before the absence of symptomatology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
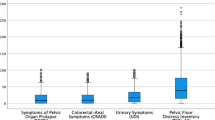
Pelvic floor disorders (PFDs) include urinary incontinence (UI), anal incontinence (AI), and pelvic organ prolapse (POP). PFDs are common, affecting at least one quarter of women, with a significant impact on the quality of life [1]. The differential prevalence of PFD in various populations and cultures around the world has not been determined when using the same definition and time framework. Nevertheless, the morbidity and economic impact of UI is a well-recognised worldwide health problem [2]. Although conservative therapy is available, many women undergo surgical treatment for PFD. Based on a recent claims and encounters database in the USA, the estimated lifetime risk of undergoing surgery to treat POP or stress urinary incontinence (SUI) is 20 % [3]. Even though the surgical treatment of SUI is fairly successful and durable, a significant proportion or women who undergo POP repair experience symptomatic recurrence. Surgical and nonsurgical treatment of AI remains far from satisfactory, especially in the long term. Overactive bladder syndrome (OAB) continues to cause significant morbidity, especially in the elderly, and to be resistant to effective management [4].
Since the treatment of PFD is less than optimal, strategies for the prevention of PFD are imperative. Retrospective cohort studies have found that the strongest contributor to PFD is vaginal birth [5–8]. However, as the majority of women who give birth vaginally do not develop PFD, a strategy of only caesarean delivery (CD) would expose most women to unnecessary surgical risks. The identification of women at highest risk of developing symptomatic PFD following vaginal delivery (VD) is a key strategy in the field of urogynecology. A recent publication outlined a potential scoring system (“UR-CHOICE”) that could potentially be utilised to predict the risk of future PFD associated with vaginal birth, and therefore be decreased by CD [9].
Besides childbirth, biological factors, such as ethnicity and a family history of PFD [9], and possibly environmental factors, as detailed below, contribute to the development of PFD. Population-based studies have reported that only 33 % of cases of UI are attributable to VD. [10]. Although operative vaginal birth is the strongest risk factor for AI, CD is not deemed protective, especially when AI is remote from delivery [6]. Increasing parity is strongly associated with the development of POP [11], but again, CD is not protective [6]. Clearly, childbirth is not the only contributor to the development of PFD.
The purpose of this International Urogynecological Association (IUGA) Research and Development Committee Opinion is to review the current literature regarding the prevention of PFD and provide an evidence-based summary of current knowledge. In this article, PFDs to be discussed under preventive strategies include: all types of UI, symptoms of OAB, AI, and POP. Prevention will include primary prevention and the prevention of progression to a more symptomatic condition.
Materials and methods
During the 39th annual IUGA meeting in 2014, a subcommittee in the R&D Committee of IUGA was formed and assigned the task to perform a review addressing the prevention of PFD, specifically UI, AI, and POP. Members of this subcommittee (the authors of this article) individually reviewed separate aspects related to the topic of the prevention of PFDs: pregnancy and delivery, pelvic floor muscle training (PFMT), medical conditions and comorbidities, lifestyle factors, and medications, in addition to basic science relevant to available clinical data. A review of the English-language literature was performed by searching the electronic databases of MEDLINE, PubMed, and Google Scholar until 1 November 2015, using relevant key words. Pertinent English-language publications, including abstracts presented in meetings, referred to by articles identified using this search strategy, were also reviewed. Where appropriate, publications with the highest level of evidence were included. Initially, each aspect was addressed by two subcommittee members, always including the corresponding author (T.B). At a later stage, the manuscript was circulated among all members, and comments were solicited and taken into account until a consensus was reached. As preventive strategies are diverse, and affect different aspects of PFDs in different populations, the outcome of the task is best defined as an integrative review.
Pregnancy and delivery
Since VD is the most common cause of pelvic floor dysfunction in women, it is vital that obstetric care is optimised to reduce the negative consequences of this event for the pelvic floor.
Anal incontinence in women is multifactorial. However, the link between obstetric anal sphincter injuries (OASIS) and the persistence of AI many years later is well established [12]. Consequently, preventing OASIS, or at least, its recognition and early repair, are crucial in the prevention of AI.
Over the last decade, there has been accumulating evidence about levator avulsion (LA) as a significant etiological factor in the development of POP [13]. LA occurs when the pubovisceral (commonly referred to as pubococcygeus and puborectalis) muscle is detached—partially or completely—from the inner surface of the pubic bone during VD. Although it can be appreciated by finger palpation of the trained individual, such injury is occult, is not screened for, and is best quantified by MRI or three-dimensional ultrasound. Contrary to an established role of LA in the development of POP, the link between LA and SUI or AI remains inconclusive [13]. Advanced maternal age at first birth is now acknowledged as a major risk factor for LA, the odds of which increase 10 % per year of age. [14].
Maternal age is an independent risk factor for postpartum SUI [15]. Furthermore, the link of advanced maternal age to long-term UI was demonstrated in a 20-year national cohort of primiparous women where the estimated increased risk was 3 % per year of childbirth delay [7]. Women older than 30 years at the time of first delivery are twice as likely to undergo subsequent SUI or POP surgery as their younger counterparts, irrespective of the mode of delivery [16]. Finally, advanced maternal age is also an established risk factor for OASIS [17].
Antenatal care
Massage and stretching
A 2013 Cochrane review concluded that although antenatal perineal massage reduces the overall incidence of “perineal trauma” (including episiotomy) in primiparous women, it did not affect the incidence of OASIS [18]. An inflatable silicon balloon designed to stretch the vagina and perineum in late pregnancy (Epi-No®) was claimed to decrease the incidence of perineal trauma. The results of a systematic review, however, failed to demonstrate protection against OASIS [19].
Antepartum PFMT
Two systematic reviews concluded that continent pregnant women who were randomised to intensive antenatal PFMT had an approximately 30 % decrease in reports of UI up to 6 months post-partum (risk ratio 0.71, 95 % CI: 0.54 to 0.95) compared with women randomised to no PFMT or usual antenatal care [20, 21]. This was based on the combined results of five trials.
A recent RCT demonstrated that exercise, which included 10 min of PFMT for 22 weeks antenatally, resulted in significant improvement in both UI and amount of leakage at 36–40 weeks’ pregnancy, compared with usual care, with only information on PFMT by a midwife [22]. Importantly, PFMT was taught by trained sport instructors without former assessment of the ability to contract the pelvic floor muscles (PFMs). This was the first study to demonstrate that effective PFMT can be provided without previous palpation or other clinical assessment of PFM function.
Weight of mother and infant
A higher BMI at term is the best predictor for the persistence of UI symptoms at 2 years postpartum, when these symptoms start during pregnancy [23]. This finding was also confirmed in two cohorts of nulliparous women at 12 years and 20 years after delivery [7, 24]. Although the effect of birth weight on the incidence of POP and UI is not consistent among studies [7, 11, 24], macrosomia continues to be an independent risk factor for the occurrence of OASIS [17, 25].
Intra-partum care
Warm compresses
Application of warm compresses to the perineum during the second stage of labour is associated with a significant reduction in OASIS (RR 0.48, 95 % CI 0.28 to 0.84) [26]. A protective effect of similar magnitude was observed with introital massage during the second stage [26]. Furthermore, the application of warm packs was found in one RCT involving 717 primiparas, associated with a significantly lower incidence of UI at 3 months postpartum [27]. No long-term data are available regarding this intervention.
Epidural
Studies evaluating the effect of intrapartum epidural analgesia on OASIS rates had conflicting results. However, when multiple regression analysis was performed in a large retrospective cohort study, thus eliminating confounding variables, a net protective effect of epidural was observed (adjusted OR 0.84) [25]. Epidural use was also found to be associated with a lower risk of LA when 4D ultrasound findings at 3–4 months postpartum were compared with those in late pregnancy [28].
Duration of the second stage of labour
The maximum pressures received by the PFMs during the second stage of labour are higher than the increased intra-vaginal pressures for coughing and straining [29]. In fact, by the end of the second stage, the pelvic floor levator muscles should be able to stretch 3.5 times their original length without rupturing. Although the duration of the second stage is positively correlated with the risk of levator muscle avulsion [30], the link to PFD has not been consistently proven. The higher incidence of operative vaginal deliveries following a longer second stage may present a confounding variable [31]. No long-term data are available regarding the effect of interventions aimed at shortening the second stage. Fundal pressure, including the use of an “obstetric belt,” has not shown any definite protective effect regarding OASIS [32]. Similarly, no conclusive evidence was reached when analysing the results of heterogeneous studies addressing pushing methods or the absence of bearing during the second stage [33].
Posture during vaginal birth
The risk of OASIS in relation to posture during delivery has not been studied in a randomised fashion. Based on the Obstetric Database in Sweden, including more than 113,000 singleton spontaneous vaginal births with no episiotomy, the rate of OASIS was evaluated in the following positions: sitting, lithotomy, lateral, on knees, birth seat, supine, squatting, and standing [34]. The rate of OASIS was highest in the lithotomy position, and lowest when birth took place while standing. Lateral position during delivery had a slightly protective effect in primiparas [34].
Assisted delivery
Manual perineal support during delivery of the head, frequently referred to as the “hands on” technique, comprises a wide variety of manoeuvres, including Ritgen’s. Although a meta-analysis of five RCTs demonstrated no protective effect from the “hands on” policy, evaluation of seven non-randomised trials (including two large interventional programmes in Norway) showed a clear benefit, as the incidence of OASIS was cut in half [35]. Although perineal support techniques vary, a common goal is a slow, controlled delivery of the head.
Episiotomy
A 2012 Cochrane review concluded that, compared with routine episiotomy, “restrictive” episiotomy results in less severe perineal trauma, including OASIS (RR 0.67, 95 % CI 0.49 to 0.91), at the cost of almost doubling the anterior perineal trauma rate, but with no difference in dyspareunia or UI [36]. The key issue in interpreting these findings is to question whether the “restrictions” or factors favouring episiotomy constitute confounding variables. This was arguably clarified by Räisänen et al. in a retrospective study evaluating a total of 64,000 women [37]. When well-established OASIS risk factors such as birth weight, instrumental delivery, previous caesarean delivery, length of second stage, age and parity were accounted for in a matched pair analysis, episiotomy actually prevented 23 % of OASIS in primiparous women, but a 61 % increased incidence was observed in second or subsequent vaginal births [37]. A potentially protective role for episiotomy was further suggested in a retrospective study evaluating 214,256 primiparous women. Multiple regression analysis revealed that episiotomy lowered the risk of OASIS during vacuum delivery (OR, 0.60; 95 % CI, 0.56–0.65) [25]. It is noteworthy that these two studies took place in Finland and Denmark, where episiotomies are almost exclusively mediolateral or lateral, as acknowledged by the authors. Finally, in a 20-year national cohort of primiparous women in Sweden, the prevalence of faecal incontinence following VD with episiotomy was the same as that following CD, but doubled with the presence of a perineal tear [38].
There is level I evidence that midline episiotomy is associated with a higher rate of OASIS, compared with mediolateral episiotomy, in spite of quicker resumption of sexual activity and better cosmetic appearance of the scar [39]. Studies that addressed the “optimal angle” of episiotomy to avoid OASIS were plagued with several limitations [40]. First, the length of episiotomy was rarely accounted for. Second, the “planned for” angle of episiotomy at the time of incision has a poor correlation with the actual angle after delivery, mostly because of “perineal deformity” during crowning. Such deformity is also affected by the timing of the episiotomy. Despite these limitations, there seems to be a consensus that episiotomies close to the midline carry a higher risk of OASIS than lateral ones [41]. This relationship is not linear, as the most lateral of episiotomies—the horizontal—actually carries the highest risk of OASIS [41].
Instrumental delivery
A 2010 Cochrane review concluded that forceps use carries at least twice the risk of causing OASIS compared with vacuum-assisted delivery [42]. In addition, forceps use was consistently found to increase the odds of LA compared with non-instrumental or vacuum-assisted delivery, with an odds ratio ranging between 3 and 32 in 16 different studies [43]. When women were evaluated 16–24 years after the first delivery, forceps delivery was associated with a higher incidence of POP, LA and larger hiatal areas compared with vacuum-assisted and non-instrumental deliveries [44]. In another study, forceps use, not vacuum-assisted delivery, was linked to a higher prevalence of faecal incontinence, compared with CD 12 years after birth [45].
OASIS repair
There has been an ongoing debate regarding the ideal method for the repair of OASIS. A Cochrane review analysing six trials involving 588 women concluded that the overlap technique was superior to the end-to-end method with regard to faecal urgency and AI at 1 year. These benefits do not seem to persist at 3 years, although the number of subjects at follow-up was small [46].
Structured training in OASIS repair, including workshops conducted during and outside professional society meetings, is believed to potentially decrease the incidence of the sequelae of OASIS. In a survey involving 311 obstetricians (most were from the UK) attending a structured training course in OASIS repair, 87 % felt that their training was not satisfactory when performing their first unsupervised repair. Following the course, there was a significant improvement in the identification and repair techniques of OASIS [47]. Whether this will lead to decreased AI in the long term remains to be determined.
Obstructed labour
Avoidance of obstructed labour helps reduce the incidence of obstetric fistula, among other advanced PFDs. In low-resource countries, improving obstetric care is a long-term goal that requires substantial socio-economic development and attention to the status of women. In the meantime, establishing birthing centres where women at risk are admitted before labour, and the use of simple tools such as the fistula index (multiplying the height in centimetres by the number of knuckles that can be accommodated between the ischial tuberosities) may help to identify patients at risk of obstructed labour who can be offered Caesarean delivery from the outset [48].
The role of Caesarean delivery in the prevention of PFD
Although UI, and even POP, may be encountered in nulliparous women [10], birth is clearly the most important risk factor for the presence of PFD. The critical question is whether CD significantly decreases the prevalence of PFD, compared with VD. Longitudinal studies evaluating the effect of mode of delivery should ideally be conducted over a long time span. PFDs, as complex multifactorial conditions, not only have a long latency from the “time of insult”, such as birth, but may also have various remission rates.
Two large longitudinal studies, based on a symptom questionnaire, were instrumental in clarifying the possible protective role of CD. The first, a 12-year longitudinal study, surveyed 3,763 women in the UK and New Zealand, and concluded that only exclusive CD was protective of UI, compared with VD, or a combination of vaginal and Caesarean birth [45]. This protection was of equal magnitude whether the CD was pre-labour or post-labour. The prevalence of AI, on the other hand, did not change with the mode of delivery, although it increased with forceps use, but not with vacuum-assisted delivery. The second study, a 20-year national cohort in Sweden, surveyed 5,236 women with only one singleton birth (1985–1988), thus eliminating the cumulative effects of obstetric events along with their confounding variables [7, 8, 38, 49]. When self-reported symptoms in a questionnaire (returned by 65 % of the cohort, 20 years postpartum) were evaluated, the prevalence of all types of UI was higher after VD compared with CD (OR 1.42 for SUI, 1.66 for urgency UI, 1.46 for MUI), with no difference between pre-labour and post-labour CD [49]. Importantly, CD was no more protective when the infant’s weight was <3,000 g. Again, advanced maternal age and BMI, in addition to current BMI, were independent contributing factors. In addition, symptoms of POP were two and a half times more prevalent following VD compared with CD [8]. The combination of short stature (<160 cm) and macrosomia (>4,000 g) was particularly detrimental. As for faecal incontinence, the prevalence was higher with VD (OR 1.43), but episiotomy performance was protective as it rendered the risk equal to that following CD [38]. Finally, when 1,011 women were recruited for evaluation 5–10 years following their first delivery, spontaneous vaginal birth was found to be associated with a much increased prevalence of POP to or beyond the hymen, compared with CD (OR 5.6, 95 % CI 2.2–14.7), although 75 % were still asymptomatic at the time of recruitment [5]. Operative vaginal birth was associated with an even worse outcome regarding all PFD.
The strongest level of evidence regarding the incidence of UI as related to the mode of delivery comes from an international trial that randomised 1,940 pregnant women with Breech singletons (estimated fetal weight <4,000 g) to vaginal or Caesarean birth [50, 51]. Evaluation at 3 months postpartum revealed a lower UI prevalence in women with CD (RR 0.62; 95 % CI 0.41–0.93) [50]. However, there was no statistically significant difference at 2 years postpartum [51]. This finding is in agreement with the results of a longitudinal study that surveyed 1,481 primiparous women annually for 1 to 5 years, starting at least 5 years postpartum. Although SUI and OAB symptoms were more common and more severe after VD compared with CD, the differences between the two groups narrowed over time. This was mostly due to a progressively increasing incidence of symptoms with the Caesarean group over time [52].
It follows that although CD—before or after labour—confers some protection, it does not totally prevent the incidence of PFD later in life.
Identification of established PFD risk factors before counselling an individual pregnant woman regarding the benefit/risk analysis of CD, is a wise strategy [9, 53]. These risk factors are: race, family history of PFD, maternal age, height, BMI, UI before or during pregnancy, and estimated fetal weight. Although the quantification of this score is a very ambitious goal, the evaluation of these factors represents an excellent introduction to the discussion and counselling of mothers-to-be. The other variable in the equation is the number of children desired [9]. Assuming comparable perinatal outcome, maternal morbidity following > 2 Caesarean births is well recognised, and could even be life-threatening in cases of placenta praevia, percreta, or uterine rupture [54]. Global estimates for 2015 reveal that the total fertility rate continues to vary widely in different regions of the world (0.81 to 6.76), with the highest estimates encountered in the underdeveloped countries [55]. Consequently, recommendations cannot be made globally, even when resources are accounted for.
PFMT in the context of prevention
There is Level 1a evidence that PFMT is effective in treating SUI, MUI, and POP in the general female population [21, 56]. However, the role of PFMT in the primary prevention of UI and POP is less clear. Primary prevention studies are sparse and difficult to conduct as they should ideally last for decades.
Systematic reviews conclude that nulliparous continent women who participated in an intensive and supervised PFMT programme were less likely to experience UI from late pregnancy up to 6 months postpartum [21]. However, studies in women with and without UI following delivery show less clear results, and the long-term effect of PFMT in the postpartum period is not yet established. In one study, the absence of benefits of PFMT was found to be unrelated to the status of levator defect following delivery [57]. As these studies combined continent and incontinent women, the role of postpartum PFMT in the primary prevention of UI is difficult to ascertain.
There are no preventive studies on PFMT in UI in the general population of premenopausal women. Only one study evaluated the effect of a diverse “behavioural modification programme” combined with PFMT in asymptomatic continent menopausal women aged > 55 years (n = 359). One year after randomisation, the intervention group had a better continence status (p = 0.01), pelvic muscle strength and voiding frequency [58].
Systematic reviews found no studies on the primary prevention of PFDs in POP [21, 56]. An abstract was presented at the International Continence Society Annual Meeting in 2014 showing that in 407 women with and without POP, those randomised to five sessions of PFMT per week had significantly lower POP scores after 2 years compared with the control group [59]. The authors concluded that PFMT can be effective in reducing prolapse symptoms in a non-clinical population of women who had not sought treatment for prolapse.
Some epidemiological studies have found that women who participate in regular exercise are less likely to experience UI [21]. However, it is difficult to conclude whether women are active because they do not leak or vice versa. On the other hand, there is solid evidence that physically active women and elite athletes have a higher prevalence of UI [60, 61]. To date no RCT has been performed on the effect of general physical activity or exercise training on PFM strength or UI or POP [21].
Medical conditions and comorbidity
Studying the impact of diabetes, obesity, constipation, and chronic obstructive pulmonary disease on the development of PFD is limited by two obstacles. First, longitudinal studies evaluating the incidence of PFD before and after the onset of these conditions are sparse. Second, women often suffer from more than one condition, and interventions may be combined and individualised, making it difficult to identify the outcome of the exact preventive measure.
Diabetes mellitus
One study showed no correlation between the earlier intensive treatment of type 1 diabetes mellitus and the prevalence of UI in later life versus conventional treatment [62]. Preventive effects of early diabetes treatment on POP remain unclear [11].
Obesity
Obesity is now a global pandemic, as the prevalence in the developing world has been escalating over the last few decades. Possible factors include urbanisation and allegedly adoption of the “industrialised diet”, with refined oils and carbohydrates [63]. Obesity has been identified as a risk factor for UI in many epidemiological studies [7], and the prevalence of both UUI and SUI increases proportionately with rising BMI. There is evidence that weight loss in obese women, whether achieved through non-surgical interventions or with bariatric surgery, leads to the improvement of UI, OAB symptoms and, although to a lesser extent, AI symptoms [64].
In the context of prevention, the question is whether weight gain per se leads to the development of symptoms of PFD. Evidence from the SWAN study suggests that weight gain in women who were continent at baseline might be a significant risk factor for developing incontinence [65]. In another cohort of middle-aged women over an 18-year period, weight gain was associated with the development of UI [66]. The shorter the time span over which weight gain takes place, the higher the risk of developing UI [67]. Although increased intra-abdominal pressure (IAP) as a precipitating factor is a simple and attractive concept, the scientific evidence is lacking; higher BMI is not synonymous with “central adiposity”. Interestingly, a 5-year longitudinal study concluded that specifically waist circumference gains were associated with new onset UI [68].
Pre-pregnant BMI is not an independent risk factor for OASIS [17, 25]. Nevertheless, the prevalence of faecal incontinence increases with BMI [45, 69]. The odds of faecal incontinence increase by 6 % for each unit increase in BMI [38].
Obesity is also a significant risk factor for POP [11]. A secondary analysis that included women aged 50–79, enrolled in the WHI study, concluded that being overweight or obese is associated with faster progression of POP, compared with women with lower BMI [70]. Weight loss was not associated with the regression of POP [70].
Asthma and chronic obstructive pulmonary disease
A prospective cohort of middle-aged and older women has shown that the participants with chronic obstructive pulmonary disorder at baseline were more likely to report UI progression [71]. Asthma was found to be associated with “incident” or new onset UI in a cohort of women followed over 5 years [68]. In contrast, pulmonary disease does not appear to be a risk factor for POP [11].
Constipation
The intra-abdominal peak pressure values during straining are not as high as for a cough [72], but the pressure is more sustained. This underlies the importance of constipation as a mechanically challenging condition to the integrity of pelvic supporting structures, especially after changes in mechanical properties secondary to aging, repetitive trauma, or childbirth [73]. Straining during defecation is reported to increase the risk of SUI and urinary urgency [74, 75]. However, there is no evidence that treating constipation prevents the incidence or progression of UI, although both constipation and UI appear to be improved by certain behavioural interventions.
As for POP, a meta-analysis did not confirm an association between POP and constipation [11].
Lifestyle
Fluid intake
Manipulation of fluid intake is commonly undertaken in conjunction with other behavioural approaches, and mostly in symptomatic subjects. Furthermore, the instructions on modifying the amount of intake are generally individualised. No data exist regarding fluid intake and the onset of UI or OAB.
Caffeine
Theoretically, caffeine consumption may affect storage and voiding functions through several mechanisms: by increasing fluid intake when consumed in coffee or caffeinated beverages, through diuresis and possibly through the modulation of bladder sensation and detrusor activity. However, a cross-sectional population survey found no statistically significant association between caffeine intake and UI [76]. Furthermore, in a cohort of 21,564 women with moderate UI enrolled in the Nurse’s Health Study, long-term caffeine intake did not affect the risk of progression of UI over 2 years [77].
The exclusive contribution of caffeine to urinary symptoms is difficult to assess. First, the amount of caffeine in cups of coffee or tea is variable. Second, caffeine is present in different beverages and edibles, and is therefore difficult to quantify.
Randomised controlled trials mostly evaluated the effect of caffeine intake modulation in symptomatic women, hindering the extrapolation to preventive effects. Data from a prospective cohort study involving 65,176 women without incontinence (Nurse’s Health Study and Nurse’s Health Study II) were suggestive of a link between heavy caffeine consumption (in all consumables, not only coffee drinks) and the frequency of urgency UI episodes [78]. In another study where multivariate models tested associations in a 5-year cohort, women who increased coffee or caffeinated diet soda intake had higher odds of progression of urgency [68].
Alcohol
A large prospective cohort study from the UK reported that beer consumption was not associated with the onset of OAB and SUI in women [79]. The lack of association was also observed in two population-based studies carried out in Norway and Italy [76, 80]. On the other hand, in a 5-year longitudinal study in the Boston (USA) area, alcohol consumption was associated with the persistence of UI, but not its new onset [68]. Therefore, no firm conclusions can be drawn regarding the avoidance of alcohol as a preventive strategy for PFD.
Carbonated beverages
In a prospective 1-year cohort study of women older than 40 years, carbonated beverage consumption was associated with the new onset of OAB and SUI as well [79]. In another cohort of 2,000 women over a period of 5 years, increasing carbonated beverage consumption by >2 servings/day was found to double the incidence of new onset UI [68]. The main limitation in the interpretation of these observations is the fact that carbonated beverages contain many additives, and the underlying mechanism behind its effect is not clear. Artificial sweeteners could elicit OAB symptoms. This was suggested in a four-way cross-over study of 20 asymptomatic volunteers, where the diet variety of “Coke” lead to the highest increase in frequency and urgency compared with the other varieties [81].
Physical activity
There is consistent evidence that physically active women and elite athletes experience higher levels of SUI than control populations [60, 61]. Interestingly, these symptoms are not only experienced during activity performance, but also during daily life chores [82]. However, a history of strenuous physical activity does not seem to be a risk factor for the development of UI later in life [83].
For a long time, expert opinion has suggested that repetitive straining and heavy lifting do increase IAP and are therefore potential risk factors for POP. Theoretically important factors, difficult to quantitatively account for, include the sustainability (duration) of the increase in IAP and the repetition of the manoeuvre. Using arithmetical models (such as maximal area under the curve), a study involving 57 women concluded that there was significant variability in intra-abdominal pressure amongst individuals doing the same activity, especially when the regulation of effort is required [84]. Besides genetic and other variables affecting the pelvic support structures, the differential in the increase in IAP secondary to various life tasks is not well understood. One study questioning the routine postoperative activity restrictions concluded that lifting 20 lb (9 kg) from a counter, climbing stairs or doing abdominal crunches do not involve a larger increase in IAP than simply getting out of a chair [85].
Clinically, in one cross-sectional study where 1,004 women underwent POP quantification on examination, subjects who were labourers/factory workers were found to have significantly more advanced prolapse than those in other job categories (p < 0.001). Differences persisted after controlling for age, race, parity, BMI, and smoking status [86]. This finding, however, has not been consistently replicated, as a recent systematic review did not confirm a relationship between current or past heavy work and the development of primary POP [11].
Smoking
Data from large epidemiological studies using logistic regression analysis revealed a strong association among UI, AI and smoking [69, 76, 87]. Furthermore, smoking was independently linked to the onset of OAB in a 1-year longitudinal study [88]. Although smoking cessation may decrease the risk of bladder cancer, there are no studies evaluating a beneficial effect on the progression of UI, OAB symptoms or AI.
The results of studies evaluating the association between smoking and POP, or the recurrence of POP after surgery, were inconsistent [11]. Interestingly, statistical analyses in some studies were suggestive of a possible protective effect [11].
Vitamin D
A possible role for elocalcitol (a vitamin D analogue) in the treatment of OAB symptoms was suggested in one international RCT involving 308 women [89]. However, longitudinal studies evaluating the effect of vitamin D supplementation on the new incidence of PFD are lacking. The National Health and Nutrition Examination Survey data revealed that vitamin D levels lower than 30 ng/ml were associated with a higher prevalence of UI, but not AI [90]. Vaginal bulge symptoms were surprisingly more prevalent among women with a higher vitamin D level [90]. In another study, urinary symptoms of nearly 6,000 women aged > 40 years over the course of 1 year correlated with different nutrients using a food frequency questionnaire [88]. Higher intake of vitamin D, protein and potassium were significantly associated with decreased risks of onset of OAB [88]. Finally, lower vitamin D levels in the third trimester were associated with decreased postpartum PFM strength assessed using a perineometer [91]. Clinical correlation regarding symptoms postpartum was not evaluated.
Oestrogen replacement
Data from large epidemiological studies linked systemic oestrogen replacement, oral or transdermal (with or without progestin), to the development of UI. This risk, albeit small, is reversible upon discontinuation of therapy [92]. There are no data addressing the effect of vaginal oestrogens on the onset or prevention of PFD. Dietary intake of phytoestrogens has no significant effect on urinary symptoms [93].
Conclusions
The promotion of prevention strategies for PFD in the absence of symptomatology should be incorporated in clinical practice. However, PFDs are multifactorial, and affected women may have more than one predisposing risk factor. In addition, women often suffer from more than one PFD at a given time, although with a different impact on quality of life. PFDs have a long latency, and may go through periods of remission. Although associations can be suggested from statistical models, causality is difficult to establish. Consequently, only limited data exist where conclusions with regard to the prevention of PFD can be inferred. The following statements are assigned levels of evidence and grades of recommendation according to the Oxford Centre for Evidence-based Medicine—Levels of Evidence (March 2009) [94].
-
PFMT during pregnancy can prevent UI in the short term (level 1a), but more long-term follow-up studies are desirable.
-
Although there is some limited evidence to support the recommendation for PFMT to prevent UI and the progression of POP in the general population (grade B recommendation), more long-term prospective studies are needed.
-
OASIS predisposes to the development of AI; consequently, efforts should be directed towards the prevention of OASIS. Interventions that probably decrease the incidence of OASIS include the application of warm compresses (level 1a), and a slow controlled delivery of the head (level 2b). Modifiable risk factors strongly associated with OASIS include the infant’s weight (level 3a), and forceps delivery (level 1a). Current evidence suggests that episiotomy should be subject to the discretion of the obstetrician; when performed, direction of the episiotomy away from the midline would decrease the risk of OASIS (level 1b).
-
Compared with vacuum-assisted delivery, forceps use carries a higher risk of OASIS (level 1a), and LA (level 2b).
-
To date, there has been a preponderance of evidence linking advanced maternal age at first delivery to measurable increased risks of PFD (level 2b).
-
The role of CD in modifying the risks of PFD should be discussed with pregnant women after reviewing individual risk factors for PFD, while taking into consideration the number of future pregnancies (grade B recommendation).
-
Weight gain, especially with an increase in waist circumference, increases the incidence of UI (level 2b). Obesity is associated with AI (level 3b), and with the faster progression of POP (level 2b).
-
It is likely that high caffeine intake is a modifiable risk factor for urinary urgency (level 2c).
-
Alcohol consumption may decrease the chance of remission of UI (level 2c).
-
Increasing the consumption of non-alcoholic beverages is associated with the new onset of all types of UI, and with OAB symptoms as well (level 2c).
-
The evidence linking smoking, pulmonary disease and excessive physical activity to PFD is more preponderant in UI than in POP. Smoking is linked to the new onset of OAB symptoms (level 2c).
-
There is a mildly negative, yet measurable, effect of systemic oestrogen replacement during menopause on UI (level 1a). This has to be balanced against the benefits in the relief of vasomotor symptoms.
Abbreviations
- AI:
-
Anal incontinence
- CD:
-
Caesarean delivery
- LA:
-
Levator avulsion
- OAB:
-
Overactive bladder
- OASIS:
-
Obstetric anal sphincter injuries
- PFD:
-
Pelvic floor disorder
- PFM:
-
Pelvic floor muscle
- PFMT:
-
Pelvic floor muscle training
- POP:
-
Pelvic organ prolapse
- SUI:
-
Stress urinary incontinence
- UI:
-
Urinary incontinence
- VD:
-
Vaginal delivery
References
Dieter AA, Wilkins MF, Wu JM (2015) Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol 275:380–384
Minassian VA, Drutz HP, Al-Badr A (2003) Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet 82:327–338
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
American Urological Association; Society of Urodynamics, Female Pelvic Medicine, Gormley EA, Lightner DJ, Faraday M, Vasavada SP (2015) Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol 193:1572–1580
Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A (2011) Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol 118:777–784
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG 107:1460–1470
Gyhagen M, Bullarbo M, Nielsen T, Milsom I (2013) The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:144–151
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:152–160
Wilson D, Dornan J, Milsom I, Freeman R (2014) UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J 25:1449–1452
Norwegian EPINCONT Study, Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S (2003) Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348:900–907
Vergeldt Tineke FM, Weemhoff M, IntHout J, Kluivers KB (2015) Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J J26:1559–1573
Mous M, Muller SA, de Leeuw JW (2008) Long-term effects of anal sphincter rupture during vaginal delivery: faecal incontinence and sexual complaints. BJOG 115:234–8
Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R (2012) Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol 39:372–383
Dietz HP, Simpson JM (2007) Does delayed child-bearing increase the risk of levator injury in labour? Aust N Z J Obstet Gynaecol 47:491–495
Hijaz A, Sadeghi Z, Byrne L, Hou JC, Daneshgari F (2012) Advanced maternal age as a risk factor for stress urinary incontinence : a review of the literature. Int Urogynecol J 23:395–401
Leijonhufvud A, Lundholm C, Cnattingius S, Granath F, Andolf E, Altman D (2012) Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery. Am J Obstet Gynecol 207:303.e1–303.e7
Jander C, Lyrenas S (2001) Third and fourth degree perineal tears. Predictor factors in a referral hospital. Acta Obstet Gynecol Scand 80:229–234
Beckmann, Michael M, Stock, Owen M (2013) Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst Rev 4
Brito LG, Ferreira CH, Duarte G, Nogueira AA, Marcolin AC (2015) Antepartum use of Epi-No birth trainer for preventing perineal trauma: systematic review. Int Urogynecol J 26:1429–1436
Boyle R, Hay-Smith JE, Cody JD, Morkved S (2012) Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 10:CD007471
Moore K, Dumoulin C, Bradley C, Burgio K, Chambers T, Hagen S, Hunter K, Imamaura M, Thakar R, Williams K, Vale L (2013) Adult conservative management. In: Abrams P, Cardozo L. Khouy S, Wein A (eds) Incontinence, 5th edn. IUCD, 5th International Consultation on Incontinence, Paris, pp 1101–1227
Pelaez M, Gonzalez-Cerron S, Montejo R, Barakat R (2014) Pelvic floor muscle training included in a pregnancy exercise program is effective in primary prevention of urinary incontinence: a randomized controlled trial. Neurourol Urodyn 33:67–71
Arrue M, Diez-Itza I, Ibañez L, Paredes J, Murgiondo A, Sarasqueta C (2011) Factors involved in the persistence of stress urinary incontinence from pregnancy to 2 years post partum. Int J Gynaecol Obstet 115:256–259
Pizzoferrato AC, Fauconnier A, Quiboeuf E et al (2014) Urinary incontinence 4 and 12 years after first delivery: risk factors associated with prevalence, incidence, remission, and persistence in a cohort of 236 women. Neurourol Urodyn 338:1229–1234
Jango H, Langhoff-Roos J, Rosthoj S, Sakse A (2014) Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol 210:59.e1–59.e6
Aasheim V, Nilsen BA, Lukasse M, Reinar ML (2011) Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 12:CD006672
Dahlen HG, Homer CS, Cooke M, Upton AM, Nunn R, Brodrick B (2007) Perineal outcomes and maternal comfort related to the application of perineal warm packs in the second stage of labor: a randomized controlled trial. Birth 34:282–290
Shek KL, Dietz HP (2010) Intrapartum risk factors for levator trauma. BJOG 117:1485–1492
Ashton-Miller JA, DeLancey JO (2009) On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng 11:163–176
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO (2006) Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107:144–149
Gartland D, Donath S, MacArthur C, Brown SJ (2012) The onset, recurrence and associated obstetric risk factors for urinary incontinence in the first 18 months after a first birth: an Australian nulliparous cohort study. BJOG 119:1361–1369
Verheijen EC, Raven JH, Hofmeyr GJ (2009) Fundal pressure during the second stage of labour. Cochrane Database Syst Rev 4:CD00606
Lemos A, Amorim MM, Dornelas de Andrade A, de Souza AI, Cabral Filho JE, Correia JB (2015) Pushing/bearing down methods for the second stage of labour. Cochrane Database Syst Rev 10:CD009124
Elvander C, Ahlberg M, Thies-Lagergren L, Cnattingius S, Stephansson O (2015) Birth position and obstetric anal sphincter injury: a population-based study of 113 000 spontaneous births. BMC Pregnancy Childbirth 15:252
Bulchandani S, Watts E, Sucharitha A, Yates D, Ismail KM (2015) Manual perineal support at the time of childbirth: a systematic review and meta-analysis. BJOG 122:1157–1165
Carroli G, Mignini L (2009) Episiotomy for vaginal birth. Cochrane Database Syst Rev 1:CD000081
Räisänen S, Selander T, Cartwright R, Gissler M, Kramer MR, Laine K, Heinonen S (2014) The association of episiotomy with obstetric anal sphincter injury—a population based matched cohort study. PLoS One 9:e107053. doi:10.1371/journal.pone.0107053
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2014) Faecal incontinence 20 years after one birth: a comparison between vaginal delivery and caesarean section. Int Urogynecol J 25:1411–1418
Coats PM, Chan KK, Wilkins M, Beard RJ (1980) A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol 87:408–412
Kalis V, Laine K, de Leeuw JW, Ismail KM, Tincello DG (2012) Classification of episiotomy: towards a standardisation of terminology. BJOG 119:522–526
Stedenfeldt M, Pirhonen J, Blix E, Wilsgaard T, Vonen B, Oian P (2012) Episiotomy characteristics and risks for obstetric anal sphincter injuries: a case–control study. BJOG 119:724–730
O’Mahony F, Hofmeyr GJ, Menon V (2010) Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev 11:CD005455
Dietz HP (2015) Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand 94:347–351
Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ (2015) Forceps delivery is associated with increased risk of pelvic organ prolapse and muscle trauma: a cross-sectional study 16–24 years after first delivery. Ultrasound Obstet Gynecol 46:487–495
MacArthur C, Glazener C, Lancashire R, Herbison P, Wilson D (2011) Exclusive caesarean delivery and subsequent urinary and faecal incontinence: a 12 year longitudinal study. BJOG 118:1000–1007
Fernando RJ, Sultan AH, Kettle C, Thakar R (2013) Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst Rev 2:CD002866
Andrews V, Thakar R, Sultan AH (2009) Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 20:193–199
Browning A, Lewis A, Whiteside S (2014) Predicting women at risk for developing obstetric fistula: a fistula index?: an observational study comparison of two cohorts. BJOG 121:604–609
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) A comparison of the long-term consequences of vaginal delivery versus caesarean section on the prevalence, severity and bothersomeness of urinary incontinence subtypes: a national cohort study in primiparous women. BJOG 120:1548–1555
Term Breech Trial 3-Month Follow-up Collaborative Group, Hannah ME, Hannah WJ, Hodnett ED, Chalmers B, Kung R, Willan A, Amankwah K, Cheng M, Helewa M, Hewson S, Saigal S, Whyte H, Gafni A (2002) Outcomes at 3 months after planned cesarean vs planned vaginal delivery for breech presentation at term: the international randomized Term Breech Trial. JAMA 287:1822–1831
Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M, Gafni A, Guselle P, Helewa M, Hodnett ED, Hutton E, Kung R, McKay D, Ross S, Saigal S, Willan A (2004) Term breech trial collaborative group maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized term breech trial. Am J Obstet Gynecol 191:917–927
Handa VL, Pierce CB, Muñoz A, Blomquist JL (2015) Longitudinal changes in overactive bladder and stress incontinence among parous women. Neurourol Urodyn 34:356–361
Jelovsek JE, Piccorelli A, Barber MD, Tunitsky-Bitton E, Kattan MW (2013) Prediction models for postpartum urinary and fecal incontinence in primiparous women. Female Pelvic Med Reconstr Surg 19:110–118
Silver RM (2012) Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol 36:315–323
https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html. Accessed 18 November 2015
Hagen S, Stark D (2011) Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev 12:CD003882. 10.1002/14651858
Hilde G, Stær-Jensen J, Siafarikas F, Ellström Engh M, Bø K (2013) Postpartum pelvic floor muscle training and urinary incontinence: a randomized controlled trial. Obstet Gynecol 122:1231–1238
Diokno AC, Sampselle CM, Herzog AR, Raghunathan TE, Hines S, Messer K, Karl C, Leite MC (2004) Prevention of urinary incontinence by behavioral modification program: a randomized, controlled trial among older women in the community. J Urol 171:1165–1171
Hagen S, Glazener C, McClurg D, Macarthus C, HerbisonP WD, Tooz-Hobson P, Bain C, Hay-Smith J, Collins M, Elders A (2014) A multicenter randomised controlled trial of a pelvic floor muscle training intervention for the prevention of pelvic organ prolapse (PREVPOL). Neurourol Urodyn 33:852–853
Bø K (2004) Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med 34(7):451–464
Bø K (2015) Pelvic floor dysfunction, prevention and treatment in elite athletes. In: Bø K, Berghmans B, Mørkved S, van Kampen M (eds) Evidence based physical therapy for the pelvic floor—bridging science and clinical practice, 2nd edn. Elsevier, Amsterdam, pp 387–407
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group, Sarma AV, Kanaya A, Nyberg LM, Kusek JW, Vittinghoff E, Rutledge B, Cleary PA, Gatcomb P, Brown JS (2009) Risk factors for urinary incontinence among women with type 1 diabetes: findings from the epidemiology of diabetes interventions and complications study. Urology 73:1203–1209
Prentice AM (2006) The emerging epidemic of obesity in developing countries. Int J Epidemiol 35:93–99
Vissers D, Neels H, Vermandel A, De Wachter S, Tjalma WA, Wyndaele JJ, Taeymans J (2014) The effect of non-surgical weight loss interventions on urinary incontinence in overweight women: a systematic review and meta-analysis. Obes Rev 15:610–617
Waetjen LE, Leung K, Crawford SL, Huang MH, Gold EB, Greendale GA (2013) Study of women’s health across the nation. Menopause 20:428–436
Legendre G, Ringa V, Panjo H, Zins M, Fritel X (2015) Incidence and remission of urinary incontinence at midlife: a cohort study. BJOG 122:816–824
Townsend MK, Danforth KN, Lifford KL, Rosner B, Curhan GC, Resnick NM, Grodstein F (2007) Incidence and remission of urinary incontinence in middle-aged women. Am J Obstet Gynecol 197:167.e1–167.e5
Maserejian NN, Minassian VA, Chen S, Hall SA, McKinlay JB, Tennstedt SL (2014) Treatment status and risk factors for incidence and persistence of urinary incontinence in women. Int Urogynecol J 25:775–782
Townsend MK, Matthews CA, Whitehead WE, Grodstein F (2013) Risk factors for fecal incontinence in older women. Am J Gastroenterol 108:113–119
Kudish BI, Iglesia CB, Sokol RJ, Cochrane B, Richter HE, Larson J, Hendrix SL, Howard BV (2009) Effect of weight change on natural history of pelvic organ prolapse. Obstet Gynecol 113:81–88
Thom DH, Brown JS, Schembri M, Ragins AI, Subak LL, Van Den Eeden SK (2010) Incidence of and risk factors for change in urinary incontinence status in a prospective cohort of middle-aged and older women: the reproductive risk of incontinence study in Kaiser. J Urol 184:1394–1401
Kruger J (2014) Intra-abdominal pressure changes during activities of daily living. How much is too much? IUGA Annual Meeting Abstract Video https://www.youtube.com/watch?v=ccieeVvTCNs. Accessed 17 November 2015
Chantereau P, Brieu M, Kammal M, Farthmann J, Gabriel B, Cosson M (2014) Mechanical properties of pelvic soft tissue of young women and impact of aging. Int Urogynecol J 25:1547–1553
Møller L, Lose G, Jørgensen T (2000) Risk factors for lower urinary tract symptoms in women 40 to 60 years of age. Obstet Gynecol 96:446–451
Byles J, Millar CJ, Sibbritt DW, Chiarelli P (2009) Living with urinary incontinence: a longitudinal study of older women. Age Ageing 38:333–338
Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S (2003) Are smoking and other lifestyle factors associated with female urinary incontinence? the Norwegian EPINCONT study. BJOG 2003(110):247–254
Townsend MK, Resnick NM, Grodstein F (2012) Caffeine intake and risk of urinary incontinence progression among women. Obstet Gynecol 119:950–957
Jura YH, Townsend MK, Curhan GC, Resnick NM, Grodstein F (2011) Caffeine intake, and the risk of stress, urgency and mixed urinary incontinence. J Urol 185:1775–1780
The Leicestershire MRC Incontinence Study Group; Dallosso HM, McGrother CW, Matthews RJ, Donaldson MMK (2003) The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int 92:69–77
Bortolotti A, Bernardini B, Colli E, Di Benedetto P, Giocoli Nacci G, Landoni M et al (2000) Prevalence and risk factors for urinary incontinence in Italy. Eur Urol 37:30–35
Cartwright R, Srikrishna S, Cardozo L, Gonzalez J (2007) Does diet coke cause overactive bladder? a 4-way cross over trial investigating the effect of carbonated soft drinks on overactive bladder symptoms in normal volunteers. 37th Annual Meeting of the International Continence Society. Neurourol Urodyn 26:626–627
Thyssen HH, Clevin L, Olesen S, Lose G (2002) Urinary incontinence in elite female athletes and dancers. Int Urogynecol J Pelvic Floor Dysfunct 13:15–17
Nygaard IE (1997) Does prolonged high-impact activity contribute to later urinary incontinence? a retrospective cohort study of female Olympians. Obstet Gynecol 90:718–722
Shaw JM, Hamad NM, Coleman TJ, Egger MJ, Hsu Y, Hitchcock R, Nygaard IE (2014) Intra-abdominal pressures during activity in women using an intra-vaginal pressure transducer. J Sports Sci 32:1176–1185
Weir LF, Nygaard IE, Wilken J, Brandt D, Janz KF (2006) Postoperative activity restrictions: any evidence? Obstet Gynecol 107:305–309
Woodman PJ, Swift SE, O’Boyle AL, Valley MT, Bland DR, Kahn MA, Schaffer JI (2006) Prevalence of severe pelvic organ prolapse in relation to job description and socioeconomic status: a multicenter cross-sectional study. Int Urogynecol J Pelvic Floor Dysfunct 17:340–345
Sampselle CM, Harlow SD, Skurnick J, Brubaker L, Bondarenko I (2002) Urinary incontinence predictors and life impact in ethnically diverse perimenopausal women. Obstet Gynecol 100:1230–1238
Leicestershire MRC Incontinence Study Group, Dallosso HM, McGrother CW, Matthews RJ, Donaldson MM (2004) Nutrient composition of the diet and the development of overactive bladder: a longitudinal study in women. Neurourol Urodyn 23:204–210
Digesu GA, Verdi E, Cardozo L, Olivieri L, Khullar V, Colli E (2012) Phase IIb, multicenter, double-blind, randomized, placebo-controlled, parallel-group study to determine effects of elocalcitol in women with overactive bladder and idiopathic detrusor overactivity. Urology 80:48–54
Badalian SS, Rosenbaum PF (2010) Vitamin D and pelvic floor disorders in women: results from the national health and nutrition examination survey. Obstet Gynecol 115:795–803
Aydogmus S, Kelekci S, Aydogmus H, Demir M, Yilmaz B, Sutcu R (2015) Association of antepartum vitamin D levels with postpartum pelvic floor muscle strength and symptoms. Int Urogynecol J 26:1179–1184
Robinson D, Cardozo L, Milsom I, Pons ME, Kirby M, Koelbl H, Vierhout M (2014) Oestrogens and overactive bladder. Neurourol Urodyn 33:1086–1091
Gold EB, Waetjen LE, Ye J, Feng WY, Johnson WO, Greendale GA, Sampselle CM, Sternfield B, Harlow SD, Study of Women’s Health Across the Nation (SWAN) (2009) Association between menopausal transition stages and developing urinary incontinence. Obstet Gynecol 114:989–998
http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/retrieved. Accessed 26 January 2016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Tony Bazi: none; Satoru Takahashi: research funding from Astellas; Sharif Ismail: none; Kari Bø: none; Alejandra M. Ruiz-Zapata: none; Jonathan Duckett: paid travel expenses, honoraria, research funding by AMS, Astellas, Ethicon, Pfizer, EliLilly and was a consultant for Astellas and Ethicon; Dorothy Kammerer-Doak: none.
Rights and permissions
About this article
Cite this article
Bazi, T., Takahashi, S., Ismail, S. et al. Prevention of pelvic floor disorders: international urogynecological association research and development committee opinion. Int Urogynecol J 27, 1785–1795 (2016). https://doi.org/10.1007/s00192-016-2993-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-2993-9