Abstract
Introduction and hypothesis
The objective of this analysis was to describe urinary incontinence (UI) incidence and persistence over 5 years in association with treatment status, sociodemographic, medical, and lifestyle factors, in a racially/ethnically diverse population-based female sample.
Methods
The Boston Area Community Health Survey enrolled 3,201 women aged 30-79 years of black, Hispanic, and white race/ethnicity. Five-year follow-up was completed by 2,534 women (conditional response rate 83.4 %), allowing population-weighted estimates of UI incidence and persistence rates. Predictors of UI were determined using multivariate logistic regression models.
Results
Incidence of UI at least monthly was 14.1 % and weekly 8.9 %. Waist circumference at baseline and increasing waist circumference over 5-year follow-up were the most robust predictors of UI incidence in multivariate models (P ≤ 0.01). Among 475 women with UI at baseline, persistence was associated with depression symptoms [monthly UI, odds ratio (OR) = 2.39, 95 % confidence interval (CI) 1.14–5.02] and alcohol consumption (weekly UI, OR = 3.51, 95 % CI 1.11–11.1). Among women with weekly UI at baseline, 41.7 % continued to report weekly UI at follow-up, 14.1 % reported monthly UI, and 44.2 % had complete remission. Persistence of UI was not significantly higher (58.2 % vs. 48.0 %, chi-square P = 0.3) among untreated women. Surgical or drug treatment for UI had little impact on estimates for other risk factors or for overall population rates of persistence or remission.
Conclusions
Women with higher gains in waist circumference over time were more likely to develop UI, but waist circumference was not predictive of UI persistence. UI treatments did not affect associations for other risk factors. Additional research on the role of alcohol intake in UI persistence is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) affects millions of adult women and has a substantial negative impact on quality of life (QoL) [1–3]. Prevalence estimates range from 10 % for weekly urine leakage [4] to 47 % for occasional (monthly) leakage [5]. Numerous epidemiological studies have identified risk factors for prevalent UI, with prominent associations for increasing age, body mass index (BMI) and vaginal child delivery. Data from longitudinal studies provide more compelling evidence by measuring development of UI over time [5]. For example, the Nurses’ Health Study found that lower physical activity levels, higher waist circumference, and postmenopausal hormone use were associated with not only incidence but persistence over an 8-year follow-up [6–8].
Prior epidemiological studies of UI incidence and persistence are limited in two major respects: lack of data on UI treatment and on racially/ethnically diverse populations. Missing UI treatment data could result in biased estimates of the natural history of UI (i.e. progression or remission) and confound associations with risk factors for persistence or incidence. This is particularly of concern if treatments occurred between baseline and follow-up study visits. In a prior analysis, women with persistent UI were compared with women never reporting UI [8]. Thus, the question of which factors might predict persistence vs. remission among women with UI remains unexamined. Furthermore, no study has included a population-based random sample balanced by race/ethnicity to allow more generalizable results.
The objectives of this analysis were to examine the incidence and persistence of UI among women aged ≥30 years from a population-based random stratified sample survey. Furthermore, we aimed to identify predictors of UI status after 5 years of follow-up, particularly focusing on treatment and various lifestyle, medical, and sociodemographic factors.
Methods
Study design and population
The Boston Area Community Health (BACH) Survey is an observational cohort study designed to assess the epidemiology of urologic symptoms in a racially/ethnically diverse population-based sample. Using a stratified two-stage cluster design, BACH recruited a random sample of 5,502 residents (2,301 men, 3,201 women) aged 30–79 years from three racial/ethnic groups in Boston, MA, USA. Participants completed an in-person interview at baseline (occurring between 2002 and 2005) and approximately 5 years later (2006–2010). Completed follow-up interviews were obtained for 2,534 women from the 3,037 eligible for follow-up (not deceased, incarcerated, on active military duty; or those medically incompetent), resulting in a conditional response rate of 83.4 %. Further details on the BACH study design have been published [9]. All participants provided written informed consent. The study was approved by the New England Research Institute Institutional Review Board.
Measurement of urinary incontinence and treatment status
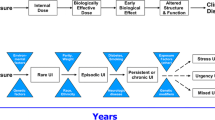
During in-person interviews at baseline and follow-up, UI was assessed by the question, “Many people complain that they leak urine (wet themselves) or have accidents. In the last 12 months, have you leaked even a small amount of urine?” Women who responded positively were then classified by the frequency of their urine leakage. The analysis examined two outcome classifications: (i) monthly, defined as urine leakage occurring at least once per month in the past 12 months, and (ii) weekly, defined as occurring at least once per week in the past 12 months. To describe UI type, women were further classified as having stress UI if they experienced involuntary loss of urine on effort or physical exertion, urgency UI if they experienced involuntary loss of urine associated with urgency, mixed UI if they had both, and other if they had neither [4, 5, 10].
At both study visits, medication use in the previous 4 weeks was collected by recording medication container labels and by self-report using prompts for indication. Medication labels and/or responses were coded using the Slone Drug Dictionary [11], which classifies medications using a modification of the American Hospital Formulary Service Pharmacologic–Therapeutic Classification System. Drug treatment for UI was defined as current use of any of the following: oxybutynin chloride (Ditropan®), transdermal oxybutynin chloride (Ditropan Transdermal®), tolterodine tartrate (Detrol®), darifenacin hydrobromide (Enablex®); solifenacin succinate (Vesicare®); trospium chloride (Sanctura®); fesoterodine fumarate (Toviaz®); propantheline bromide (Pro-Banthine®); hyoscyamine (Levsin®). Medications for overactive bladder (OAB) were included, as these are also prescribed for UI. Surgical intervention was assessed by asking participants if they ever had “surgery for incontinence (urine leakage).” Participants self-reported use of pelvic floor strengthening exercises, urination timing, and other treatments (pessary, biofeedback, electric stimulation, acupuncture, and homeopathy).
Statistical analysis
Descriptive analyses examined the change in UI frequency between baseline and follow-up and prevalence at follow-up among all women. To identify relevant predictors, separate multivariate logistic regression models were created for incidence and persistence. Analysis of incidence (UI present at follow-up among women without UI at baseline) included the 2,059 women with no or rare (less often than monthly) UI at baseline. Analyses of persistence (UI present at follow-up among women with UI monthly or more often at baseline) included the 475 participants with UI at baseline.
We examined various sociodemographic, medical, and lifestyle factors (Table 3 footnote) plausibly related to UI based on previous evidence. Initially, age-adjusted estimates were obtained for each possible predictor. Variables associated with UI outcome at P < 0.20 in the age-adjusted model were then included in a multivariate model to obtain adjusted OR and 95 % CI for the association between variable and outcome. Treatment indicators were then added to this model to examine its influence at baseline or follow-up. Interactions between race/ethnicity and other factors were tested in the multivariate models, and exploratory analyses were stratified by race/ethnicity to examine possible differences in predictors. To account for missing data (<1 % of urological data), multiple imputation was performed in IVEware, generating 15 complete data sets, based on multivariate sequential regression [12]. To account for the multistage sampling design and obtain population-generalizable estimates, data observations were weighted inversely to their probability of selection at baseline, adjusted for nonresponse bias at follow-up, and then poststratified to the Boston census population in 2000. Analyses were conducted in SAS v.9.3 (SAS Institute, Cary, NC, USA) and SUDAAN v.11.0 (Research Triangle Park, NC, USA).
Results
Mean ± standard deviation (SD) time between baseline and follow-up assessments was 4.8 (0.6) years. Table 1 presents changes in UI frequency between baseline and follow-up. Prevalence of at least monthly or weekly UI increased slightly over follow-up, from 19.7 % to 21.4 % for monthly and from 11.0 % to 13.4 % for weekly UI. Among women with weekly UI at baseline, 41.7 % continued to report weekly UI at follow-up, whereas 44.2 % had complete UI remission. Overall, remission was most common among women with leakage two to three times a month (55.2 %). Although Hispanic women less frequently reported urgency UI and more commonly reported stress UI (Table 2), racial/ethnic differences in UI prevalence were not statistically significant.
Incidence of UI
Among the 2,059 women reporting no UI at baseline, incidence of at least monthly was 14.1 % and of at least weekly was 8.9 %. Table 3 presents select factors that were considered in predictive models for UI incidence based on prior studies and their associations in age-adjusted models (P < 0.20). Factors associated with increased incidence of monthly or more frequently UI were higher waist circumference, smoking, having increased carbonated beverage intake by 2+ servings/day over follow-up, depression symptoms, asthma, and arthritis/rheumatism (age-adjusted P < 0.05). In addition, for more frequent (weekly or more often), low physical activity and allergies were predictive. Race/ethnicity was not statistically associated with UI incidence in age-adjusted models; however, upon adjustment for waist circumference and age, black women had a lower odds of frequent UI compared with white women (OR = 0.54, 95 % CI 0.30–0.99, P = 0.048).
In full multivariate models, waist circumference at baseline was the most robust predictor (weekly UI, OR = 1.03 per cm increase, 95 % CI 1.01–1.05, P = 0.01) and alone explained the greatest variation in UI incidence. From the baseline mean ([standard error (SE)] of 89.6 (0.7) cm, mean change in waist circumference was an increase of 6.7 (0.6) cm over the follow-up period and was higher for women with smaller waist circumferences at baseline and for white compared with black and Hispanic women. A larger increase in waist circumference over follow-up was predictive of developing weekly UI (OR = 1.03 per cm increase, 95 % CI 1.01–1.06, P = 0.01) and had strong positive associations with other factors, particularly lower physical activity, increased carbonated beverage intake, and presence of depression symptoms, asthma, or arthritis/rheumatism; adjustment for waist circumference accounted for associations between UI and most of these other factors. Because mean waist circumference was higher among blacks vs. whites, the inverse association between black race and incidence of weekly UI was strengthened upon adjustment for waist circumference. Age, smoking status, and allergies remained marginally significant as predictors of weekly UI.
Interactions between race/ethnicity and other factors in the multivariate model were not statistically significant. In exploratory analysis stratified by racial/ethnic groups (data not shown), the most significant predictors of weekly UI incidence among white women were waist circumference (P = 0.003) and change in waist circumference (P = 0.01). For black and Hispanic women, current cigarette smoking, as well as depression symptoms among Hispanic women, were most statistically significant (P = 0.01).
Persistence and regression of UI
Among the 475 women with UI at baseline, approximately half reported UI persistence at follow-up: 51.0 % of women with monthly or more frequent UI, 55.8 % with weekly or more frequent UI. Excluding women (n = 82) ever having surgical or pharmaceutical UI treatment, the proportion with monthly persistence was unchanged, but weekly persistence was not significantly higher among untreated vs. treated women (58.2 % vs. 48.0 %, chi-square P = 0.3).
Few factors were statistically significant predictors of persistence (alternatively, regression, Table 4). Women with depression symptoms or from the middle socioeconomic level (vs. lowest) had approximately twice the odds monthly persistence. Alcohol drinking (1+ vs. no drinks/day) was associated with two to three times the odds of persistence, although CI were wide, e.g., for weekly or more frequent, OR = 3.51, 95 % CI: 1.11–11.1. Similarly, marginally significant associations were observed for use of tricyclic antidepressants. No associations between waist circumference, smoking status, or race/ethnicity and persistence were found.
Treatment status
Figure 1 presents percentages for treatment and management strategies among women with UI at baseline. Rates of prior surgical intervention and current pharmaceutical treatment were similar in patients reporting monthly (surgical 6.5 %, medication 6.4 %) and weekly (surgery 10.6 %, medication 9.9 %) UI, with few patients having had both interventions. Treatments at baseline were not strongly predictive of persistence or remission. Results were similar for treatment reported at follow-up (data not shown). Adjusting for treatment status did not appreciably change results for factors associated with persistence in the multivariate models shown in Table 3.
Only ten women with UI at baseline newly reported having had surgery between baseline and follow-up; eight had complete remission, whereas reported monthly UI. Meanwhile, new use of UI medications between baseline and follow-up occurred for 4 % of women (n = 22 with monthly or more frequent UI, n = 16 with weekly or more frequent UI). Compared with nonusers of medication at follow-up, new users had the highest rates of remission of weekly UI (59.2 % vs 43.7 % who used medication at neither time point, 46.9 % who used medication at baseline only, and 38.6 % who were repeat users). Treatments other than medication, surgery, timing, or pelvic floor strengthening exercises were rare (<3 %) and were most commonly used at follow-up among women with persistent UI. Of the women without UI at baseline, 34 (1.3 %) reported previously receiving surgery; ten reported UI at follow-up (six at least weekly). A total of 17 women without UI at baseline reported having had surgery between baseline and follow-up; most (12 of 17) reported no UI at follow-up.
Discussion
This longitudinal, population-based study of women confirms certain results from prior studies of UI incidence and persistence and provides novel findings regarding treatment status and waist circumference gains over time. In general, risk factors for newly developing UI (incidence) differed from those for having persistent UI over 5 years of follow-up. Higher baseline and greater increases in waist circumference over follow-up were robust predictors of UI incidence. Persistence was most strongly associated with alcohol intake and marginally with depression symptoms or midsocioeconomic level. Of note, UI treatments had little impact on overall rates persistence or remission and did not affect associations for other risk factors.
This is the first generalizable population-based study using a racially/ethnically balanced design to examine changes in UI status and persistence over time. Compared with other epidemiological investigations, a unique strength of this study is its detailed data on medications and other treatments. This addresses the criticism of most previous epidemiological studies in which the potential effects of treatment status were unknown. Our results show that the rate persistence was only marginally higher among women who had not received surgical or pharmaceutical treatment compared to the total sample. This was likely due to the low overall rate of treatment, which made a relatively small impact on population level rates of persistence and remission, despite treatment efficacy in some patients. Given relatively low rates of surgery and medication in the general population [13, 14], these findings reinforce epidemiological studies lacking treatment data.
In addition, among the subgroup of women who had received treatment at baseline, the proportion with persistent UI at 5-year follow-up was similar to that with remission. It is possible that a lack of treatment benefit was due to more severe UI among these patients, who were concurrently using medications and experiencing UI at baseline. For women who previously underwent surgical treatment, efficacy may have decreased over time, resulting in recurrence [15]. Alternatively, one subtype (e.g., stress UI) may have resolved and another (e.g., urgency UI) developed or persisted.
The importance of waist circumference for UI incidence is consistent with prior studies, which identified weight, weight gain, BMI, and central adiposity as risk factors [16–19]. However, to our knowledge, this is the first study to report that greater increases in waist circumference over time are positively associated with newly developing UI, particularly frequent UI. It is biologically plausible that increased waist circumference increases the weight load on the abdomen and pelvic floor, which increases bladder pressure and urethral mobility, thereby facilitating leakage. Data from a randomized trial of a behavioral weight-loss program among overweight/obese women with UI showed that women in the intervention arm (with mean 8.0 % weight loss) had a significant reduction in both stress and urgency UI at 6-months follow-up [20]. However, the study did not examine waist circumference changes or the relative contributions of increased physical activity and reduced caloric intake. Although a role for physical activity or diet in the development of UI is plausible [21–23], the evidence to date suggests that weight, particularly central adiposity, is more relevant.
An interesting finding from our exploratory analyses was that although waist circumference was relevant for all racial/ethnic subgroups, it was a highly significant predictor of UI incidence for white women only. This may be related to the fact that there was more variation in both baseline and change in waist circumference among white women compared with black and Hispanic women, and the mean increase over follow-up was largest among white women. Among black and Hispanic women, current smoking, and among Hispanics, depression symptoms, were more statistically significant for developing weekly UI. Further research is needed to understand mechanisms in which smoking and depression may contribute to development of UI and whether these associations are causal. Of note, predictors of persistent UI were similar across the racial/ethnic subgroups.
For women with UI, our results indicate that alcohol intake may contribute to its persistence. This finding is consistent with results from the Nurses’ Health Study [8], though a precise mechanism of action remains to be identified. Numerous studies indicate that UI is associated with decreased QoL [2, 3, 24], but few studies have focused specifically on depression [24]. We found depression symptoms were predictive of persistence of occasional but not weekly UI. Tricyclic antidepressants have been used to treat UI; therefore, the association with persistence may reflect treatment rather than a risk factor. Further research is also needed to understand mechanisms behind the finding that women of midlevel socioeconomic status had the highest odds of persistent UI. This was an unexpected finding, because previous analyses of baseline BACH data showed no socioeconomic status differences in prevalence [4] or treatment seeking for UI [13], and the Reproductive Risks for Incontinence Study in Kaiser found no associations between education or income and progression or persistence of UI [18]. Furthermore, although black women were at lower odds of developing weekly UI, there were no racial/ethnic differences in persistence of UI.
A limitation of this study is that the 5-year duration between baseline and follow-up may have missed brief episodes of UI, interim changes in severity, and interim changes in medication use. Although the study was sufficiently powered to analyze incidence, analysis of persistence of weekly UI had fewer women, which may be why few significant predictors were observed. For accurate assessments of medication efficacy and outcomes, multiple assessments of UI shortly before and after starting treatment would be helpful. Also, data on surgical treatment were self-reported and lacking detailed information on type of surgery, e.g., sacral neuromodulation or other techniques. Lastly, three new treatments for urgency incontinence have recently been approved: mirabegron, percutaneous tibial nerve stimulation, and botulinum toxin A (Botox®) intradetrusor injections; it is unclear whether these results apply to new medications.
In conclusion, this population-based observational study of women of Hispanic, black, and non-Hispanic white race/ethnicity found that the most robust predictor of newly developing UI among all women was increasing waist circumference over time. However, among women with UI at baseline, waist circumference was not predictive of persistence. UI treatments had little impact on overall rates of persistence or remission and did not affect associations for other risk factors. Finding that risk factors for incidence differed from those for persistence suggests a need to establish distinct public health messages for UI prevention, particularly regarding avoiding abdominal weight gain.
Abbreviations
- BACH:
-
Boston area community health
- UI:
-
Urinary incontinence
References
Minassian VA, Drutz HP, Al-Badr A (2003) Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet: Off Organ Int Fed Gynaecol Obstet 82:327–38
Tennstedt SL, Chiu GR, Link CL, Litman HJ, Kusek J, McKinlay JB (2009) The effects of severity of urine leakage on quality of life in hispanic, white and black men and women: The Boston Area Community Health Survey. Urology 75:27–33. doi:10.1016/j.urology.2009.08.019
Minassian VA, Devore E, Hagan K, Grodstein F (2013) Severity of urinary incontinence and effect on quality of life in women by incontinence type. Obstet Gynecol 121:1083–90. doi:10.1097/AOG.0b013e31828ca761
Tennstedt SL, Link CL, Steers WD, McKinlay JB (2008) Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol 167:390–9
Waetjen LE, Liao S, Johnson WO, Sampselle CM, Sternfield B, Harlow SD, Gold EB (2007) Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data: study of women’s health across the nation. Am J Epidemiol 165:309–18. doi:10.1093/aje/kwk018
Townsend MK, Curhan GC, Resnick NM, Grodstein F (2009) Postmenopausal hormone therapy and incident urinary incontinence in middle-aged women. Am J Obstet Gynecol 200(86):e1–5
Townsend MK, Danforth KN, Rosner B, Curhan GC, Resnick NM, Grodstein F (2008) Physical activity and incident urinary incontinence in middle-aged women. J Urol 179:1012–6, discussion 6-7
Devore EE, Minassian VA, Grodstein F (2013) Factors associated with persistent urinary incontinence. Am J Obstet Gynecol. doi:10.1016/j.ajog.2013.05.002
McKinlay JB, Link CL (2007) Measuring the Urologic Iceberg: Design and Implementation of the Boston Area Community Health (BACH) Survey. Eur Urol 52:389–96
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20
Kelley KE, Kelley TP, Kaufman DW, Mitchell AA (2003) The Slone Drug Dictionary: A research driven pharmacoepidemiology tool. Pharmacoepidemiol Drug Safety 12:168–9
Raghunathan TE, Solenberger P, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software User Guide. Survey Research Center, Institute for Social Research, University of Michigan. http://www.isr.umich.edu/src/smp/ive; 2002
Harris SS, Link CL, Tennstedt SL, Kusek JW, McKinlay JB (2007) Care seeking and treatment for urinary incontinence in a diverse population. J Urol 177:680–4
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF (2012) The iceberg of health care utilization in women with urinary incontinence. Int Urogynecol J 23:1087–93. doi:10.1007/s00192-012-1743-x
Svenningsen R, Staff AC, Schiotz HA, Western K, Kulseng-Hanssen S (2013) Long-term follow-up of the retropubic tension-free vaginal tape procedure. Int Urogynecol J 24:1271–8. doi:10.1007/s00192-013-2058-2
Townsend MK, Danforth KN, Rosner B, Curhan GC, Resnick NM, Grodstein F (2007) Body mass index, weight gain, and incident urinary incontinence in middle-aged women. Obstet Gynecol 110:346–53
Minassian VA, Stewart WF, Wood GC (2008) Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol 111:324–31. doi:10.1097/01.AOG.0000267220.48987.17
Thom DH, Brown JS, Schembri M, Ragins AI, Subak LL, Van Den Eeden SK (2010) Incidence of and risk factors for change in urinary incontinence status in a prospective cohort of middle-aged and older women: the reproductive risk of incontinence study in Kaiser. J Urol 184:1394–401. doi:10.1016/j.juro.2010.05.095
Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS (2013) Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urol 13:27. doi:10.1186/1471-2490-13-27
Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, Richter HE, Myers D, Burgio KL, Gorin AA, Macer J, Kusek JW, Grady D (2009) Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med 360:481–90
Maserejian NN, Kupelian V, Miyasato G, McVary KT, McKinlay JB (2012) Are physical activity, smoking and alcohol consumption associated with lower urinary tract symptoms in men or women? Results from a population based observational study. J Urol 188:490–5. doi:10.1016/j.juro.2012.03.128
Maserejian NN, Giovannucci EL, McVary KT, McGrother C, McKinlay JB (2010) Dietary macronutrient and energy intake and urinary incontinence in women. Am J Epidemiol 171:1116–25
Maserejian NN, Giovannucci EL, McVary KT, McKinlay JB (2011) Intakes of vitamins and minerals in relation to urinary incontinence, voiding, and storage symptoms in women: a cross-sectional analysis from the Boston Area Community Health survey. Eur Urol 59:1039–47. doi:10.1016/j.eururo.2011.03.008
Sung VW, West DS, Hernandez AL, Wheeler TL 2nd, Myers DL, Subak LL (2009) Association between urinary incontinence and depressive symptoms in overweight and obese women. Am J Obstet Gynecol 200(557):e1–5
Acknowledgments
The authors thank Gretchen Chiu and Teresa Curto for their contributions to data set preparation and statistical analysis.
Funding
This project was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, Grant No. U01DK56842. The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maserejian, N.N., Minassian, V.A., Chen, S. et al. Treatment status and risk factors for incidence and persistence of urinary incontinence in women. Int Urogynecol J 25, 775–782 (2014). https://doi.org/10.1007/s00192-013-2288-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2288-3