Abstract
The pathophysiology of stress urinary incontinence (SUI) is multifactorial and evidence supports a critical role of pregnancy and vaginal delivery. This review dissects epidemiologic literature to determine the weight of evidence on the role of advanced maternal age (AMA) as a risk factor for the development of subsequent or persistent SUI. We conducted a Medline search using the keywords postpartum, SUI, maternal age, pregnancy, and incontinence. The published literature was critically analyzed. Evidence supports that childbirth trauma contributes to the development and severity of SUI. Yet, there is contradicting evidence as to whether AMA increases the risk. AMA clearly represents an independent risk factor for postpartum SUI. However, long-term studies did not confirm this observation. Whether this finding is suggestive of a true biologic signal that is lost with competing risk factors over time warrants further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is a prevalent condition that affects the quality of life of women as early as their postpartum years [12]. Over half of women with postpartum urinary incontinence reported being moderately to greatly bothered by the incontinence [13]. Significant evidence supports a critical role of pregnancy and vaginal delivery in the development of SUI [5, 9–11]. Clinical epidemiology reveals that postpartum SUI recovers in the majority of patients within a few months or up to 1 year after delivery. Partial recovery, or the lack of recovery, sets the stage for development of SUI 5–12 years later [22, 23]. Patient characteristics such as advanced maternal age (AMA) at the time of pregnancy and delivery are considered potential risk factors that may increase a patient’s susceptibility to the pregnancy—and delivery-induced injury and decreased recovery.
Recent evidence suggests that an increasing proportion of women are having their first deliveries at an advanced age [14]. With a large and increasing population of women in this risk category, the clinical significance of the role of maternal age on the development of SUI becomes increasingly important. Because of the social and medical significance, we were interested in gaining a deeper understanding of the current data available about the association between AMA and SUI. In this review, we examine the epidemiologic literature to determine the weight of evidence on the role of AMA as a risk factor for the development of postpartum and persistent SUI.
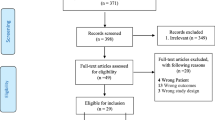
We conducted a Medline search for citations between 1960 and 2010 using the keywords of “postpartum,” “stress urinary incontinence,” “maternal age,” “pregnancy,” and “incontinence.” We indentified a total of 169 that aimed primarily at discussion of risk factor of SUI from an epidemiologic stand point. All these articles were reviewed, and only a total of 21 looked at AMA in postpartum/persistent SUI. We excluded studies that only evaluated risk factors of SUI during pregnancy including AMA. The results of the published data were categorized based on the type of epidemiologic study (i.e., retrospective vs. prospective and short vs. long term). Short-term studies were classified as studies shorter than 12 months. The search identified a total of 21 articles, including eight retrospective or case studies, seven short-term prospective studies, and six long-term prospective studies (Table 1). Figure 1 also demonstrates the odds ratio (OR) and confidential intervals (CI) of urinary incontinence prevalence according to the age at first delivery or maternal age reported in 14 of these reviewed articles.
Evidence from retrospective studies and case series
Glazener et al. [10] recently reported a large epidemiologic study where all women who delivered over the course of 1 year in three maternity units were asked to complete a mailed questionnaire 3 months postpartum. Of 10,989 eligible women, 7,879 (72%) completed the questionnaire and 3,405 of whom were primiparas with singleton births. The prevalence of incontinence among 3,405 primiparas was 29%. The study demonstrates that the mode of delivery and older maternal age were significantly related to the chance of developing new urinary incontinence 3 months after delivery. The likelihood increased most (OR, 2.21 (1.47–3.33)) for the oldest women (35 years and older). However, if a women’s incontinence first occurred during pregnancy prior to delivery, AMA was not a significant factor.
In a study conducted by Pregazzi et al. [17], 537 consecutive primiparas were questioned about their urinary symptoms 3 months after their vaginal delivery. They reported that maternal age at >35 years is associated with a greater prevalence of frequency while there was not a statistically significant association between maternal age and the other urinary symptoms (for SUI, p > 0.05, χ 2 = 5.4522).
In a retrospective study (N = 186) to examine the prevalence of postpartum SUI, Groutz et al. [12] reported a fourfold increase in SUI prevalence 1 to 2 years after spontaneous delivery in older (maternal age, 40 ± 1.8 years) compared with younger (maternal age, 26.2 ± 2.5 years) primiparas (38.5% vs. 9.8%, respectively; p < 0.001). In addition, older primiparas who underwent elective cesarean section had a significantly lower prevalence of postpartum SUI than those who delivered vaginally (p = 0.02). A weaker association was however described by Chin et al. who evaluated risk factor for SUI 1 year postpartum in review of the records of 529 primiparas women [4]. They concluded that an older maternal age and higher BMI prior to pregnancy increase slightly the risk of urinary incontinence (ORs = 1.081 and 1.097, with p values 0.040 and 0.049, respectively).
In a retrospective survey, Fritel et al. [8] reported that 4 years after first delivery the prevalence of SUI was 32% (99/307). AMA was identified as an independent risk factor of SUI on multiple logistic regression analysis with an odds ratio (OR) 2.4 (95% CI, 1.4–4.2) for women older than 30 years at their first delivery. As with Glazner, this study identified that incontinence status prior (OR, 18.7; 95% CI, 3.6–96.4) and during (OR, 2.5; 95% CI, 1.3–4.8) first pregnancy to be the other significant risk factors.
A retrospective case control study done by Carley et al. [3] on 480 women (age, 51.4 + 13.0 years) who underwent corrective surgery for urinary incontinence, pelvic organ prolapse, or both, and whose obstetric history was obtainable through chart review. The control group was composed of 150 women (age, 50.7 + 9.6 years) having routine screening mammography who completed a questionnaire regarding obstetric, gynecologic, and urologic history. They found that compared with controls, patients were older by 4 years at the time of their first delivery (28.9 + 4.9 vs. 24.9 + 4.9 years, p < 0.001).
Foldspang et al. [7] studied the possible association between parity and prevalence of urinary incontinence in a random sample of 2,631 women aged 30–59 years from the population of Aarhus, Denmark. Questionnaire screened for all incontinence, stress, mixed, and urge urinary incontinence. Multiple logistic regression did not reveal any association between urinary incontinence and time or age specification of parity including age at first and last childbirth. However, in a separate analysis of the two major age groups at the time of survey (30–44 and >45 years), women aged 30–44 years showed an increased risk for all types of urinary incontinence with increasing age at last childbirth. In women >45 years, SUI decreased with increasing age at first childhood (OR, 0.9; 95% CI, 0.9–1.0).
In another cross-sectional study, Fritel [9] examined the prevalence of severe SUI among 2,625 perimenopausal women and potential obstetric risk factors; 15% of the population had severe SUI defined as “often” and “all the time” on the questionnaire in the 4 weeks prior to completing the questionnaire. Among those perimenopausal women with severe SUI, this study demonstrated that women younger than 22 years at first delivery had a higher risk of severe SUI (OR 1.4 (CI, 1.1–1.9)) compared with older women (22–27 and >27). Except for parity, no other obstetrical factor was associated with severe SUI including mode of delivery. The risk of severe SUI increased with increasing body mass index (BMI), diabetes, and previous urinary incontinence surgery.
The above mentioned studies differ from one another in that the latter reports on severe incontinence and more importantly, examines the risk factors at a later time frame from the time of delivery. Review of retrospective studies and case series reveal that advanced maternal age increases the risk of any SUI when examined in the postpartum period (3 month). When researchers examined severe/frequent SUI in post-menopausal women, then advanced maternal age had no effect. Young maternal age and presence of incontinence during pregnancy were risk factors for severe/frequent SUI in menopausal years. These retrospective studies suggest that risk factors for SUI vary depending on the time frame examined (postpartum vs. perimenopausal) and degree of severity of SUI.
Evidence from prospective short-term studies
Maternal age was found to be an independent risk factor in five prospective short-term studies of postpartum SUI. Two prospective short-term studies did not confirm the finding. Schytt et al. [19] investigated SUI 1 year after childbirth in 2,390 Swedish women (average age, 29.5 years); 44% of the population were primiparas and 56% were multiparas; 79.2% of the women had a vaginal delivery. Study showed that women >35 years reported stress urinary incontinence to a greater extent than younger women (RR, 1.5; CI 95%, 1.0–2.1). Van Brummen et al. [21] demonstrated that the predictive factors for presence of bothersome SUI were older maternal age (32.5 vs. 30.3 years old at delivery) and the presence of bothersome SUI at 12 weeks of gestation when assessed 1 year after first pregnancy. None of the women aged 25 years, 2.8% aged 26 to 30 years, 4.3% aged 31 to 35 years, and 10.3% aged ≥36 years had bothersome SUI. Using those aged <26 years as the reference group, there was a trend for women >30 years of age to have more bothersome SUI (p < 0.098).
Recently, Baydock et al. [2] reported on the risks of urinary incontinence 4 months after vaginal delivery in 632 patients. Twenty-nine percent of women had any urinary incontinence. In univariate analysis, SUI was found to be increased in patients >30 years of age (26.2%) compared with patients <30 years of age (19.3%; RR, 1.4; CI 95%, 1.0–1.8; p = 0.05). In multivariate analysis, the two variables that remained significant for any urinary incontinence were maternal age at least 30 years (p < 0.01) and forceps delivery (p < 0.01).
Yang et al. [24] recently evaluated fecal and urinary incontinence status in 1889 primiparas women 6 months after delivery. AMA among other risks was determined to be an independent risk of urinary incontinence (OR, 1.08; 95% CI, 1.04–1.12).
In a large UK hospital, a total of 435 women who sustained an obstetric anal sphincter injury (OASIS) were followed up by Marsh et al. [16] over a 5-year period. Details of bowel, urinary, and sexual function were documented using a structured questionnaire. The outcome measures included the incidence of symptoms following OASIS and factors which modify the risk of developing symptoms. In this study, significantly more women >35 years old reported SUI than those <35 (27.5% (n = 14/51) vs. 13.6% (n = 48/354); p = 0.012). They concluded that older maternal age and the use of forceps significantly increase the risk of developing urinary symptoms.
On the other hand, Diez-Itza et al. [6] investigated the risk factors associated with SUI 1 year after delivery in 352 primiaras women with no prior history of SUI. On univariate analysis, maternal age was marginally significant with the mean age of continent women being less than incontinent women (31.0 ± 3.4 vs. 32.3 ± 4.5, p value 0.09). When included in the multivariate analysis with other marginally significant variables, the only factor that was independently associated with SUI 1 year after delivery was the new onset of SUI during pregnancy.
Stainton et al. [20] analyzed the risk factors for 1 year postpartum SUI in a convenient sample of 124 women. They did not select the patients as in the former study; 24/124 (19.3%) were >36 years and only 63.7% of the population were primiparas. Maternal age was not a significant predictor of SUI yet the authors report that 37.5% of the expected cell counts were <5 which questions the results of the maternal age impact. Incontinence status prior to first pregnancy emerged as the key factor for predicting those women most at risk for developing postnatal urine leakage (RR, 4.14; 95% CI, 1.23–13.92).
The first five prospective short-term studies reviewed support the theory that likelihood of developing postpartum incontinence increases with older maternal age. The relative risk however for AMA ranged from 1.1 to 1.5. The last two studies either showed a marginal significance for maternal age as a risk (Diez-Itza) or lacked sample size (stainton).
Evidence from long-term prospective studies
In a 6-year follow-up study of the cohort reported by Glazener described above, women older than 35 years at first birth had 2.36 higher odds of developing SUI 6 years after the index delivery compared to women younger than 25 years [15]. Of the original cohort of 10,989 eligible women, 4,214 (38%) completed a follow-up questionnaire 6 years later. Older maternal age at first birth (older than 30 years), parity, and vaginal delivery were found to be significant risk factors for persistent (defined as incontinence at 3 months and 6 years) and long-term (defined as incontinence at 6 years but not 3 months) urinary incontinence. The prevalence of persistent urinary incontinence at both 3 months and 6 years was 24%. Point prevalence increased from 33% at 3 months to 45% at 6 years. Among symptomatic women at 3 months, the proportion who still had symptoms at 6 years was 73%. Among the women without symptoms at 3 months, symptoms at 6 years were reported by 33% of those who had a subsequent birth(s) and 30% of those who did not [10]. A logistic regression model restricted to primiparas at index birth showed that inclusion of the additional obstetric variables did not alter the associations with mode of first delivery, maternal age, number of births, or ethnic group. It is important to note that the 38% response rate in this study might introduce a bias that affect the generalization of the results.
Viktrup et al. [23] conducted a longitudinal cohort study to examine the impact of onset of SUI in first pregnancy or the postpartum period on the risk of symptoms 12 years after the first delivery. The study demonstrated that the presence of SUI 3 months after first delivery predicted a very high risk of SUI after 5 and 12 years. The study confirms the finding that onset of SUI during first pregnancy or puerperal period carries a risk of inducing instant or delayed SUI that may become chronic and be present 5 and 12 years later. There was no statistically significant difference in the prevalence of SUI at 12 years in women younger or older than 25 years at first delivery. In the cohort (241 women), 46.1% were <25 and 53.9% were >25 at the time of first delivery with a prevalence of SUI of 38.7% and 45.5%, respectively (p = 0.3). The authors did not report the percentage of women at higher age groups and their SUI prevalence. Thus for the purpose of our review, we cannot conclude if this study produce evidence with or against the association between advanced maternal age and SUI at 12 years following first delivery.
Rortveit studied the effect of maternal age at first and last pregnancy on urinary incontinence and found that women age 25 years or older at the first delivery had increased risk for urinary incontinence, and specifically stress urinary incontinence, compared with younger women [18].The prevalence of any urinary incontinence was significantly higher among women who had their first delivery after the age of 25 years compared with women who had their first delivery at the age of 25 years and younger (27.7% vs. 23.2%; P < 0.01). However, the effect attenuates with increasing actual age and it disappears in the age group 50 to 64 years. The age at the last delivery seems to be of less importance [18].
In a prospective, 10-year observational study, Altman assessed the long-term effects of childbirth on urinary incontinence after first delivery. They demonstrated a significant increase in prevalence of SUI, as well as urinary urgency at a 10-year follow-up. The RR (adjusted for maternal age and parity) of moderate to severe urinary incontinence increased significantly 10 years after first delivery (RR, 5.8; 95% CI, 1.2–33.7). Multivariable regression analysis on obstetric covariates at first or subsequent deliveries found no significant association with the development of SUI or urinary urgency at 10-year follow-up. Multivariable analysis (adjusted for age and parity) found that SUI symptoms at 9-month and 5-year follow-up were independently associated with the presence of symptoms at 10 years (RR, 13.3; 95% CI, 3.9–33.1 and RR, 14.1; 95% CI, 2.5–18.8, respectively). Altman could not confirm that maternal age at the time of first delivery was associated with an increased risk for urinary incontinence [1].
First delivery at a young age was also found to be a risk factor by Grodstein [11] and colleagues when obstetric history was assessed through the use of biennial mailed questionnaires from 1976 to 1996 among participants of the Nurses’ Health Study. In 1996, 83,168 women aged 50 to 75 years reported their frequency of leaking urine and quantity of leakage. Overall, 34.1% of the women reported leaking urine at least once per month during the previous 12 months and 17.7% reported frequent urine leak defined as once per week or daily leakage of urine. After controlling for potential confounders, there were strong trends of increasing prevalence of occasional and frequent leaking with increasing age (p < 0.0001). There was also increasing prevalence of leaking urine with increasing parity. Age at first delivery older than 35 years was associated with a slight elevation in frequent leakage compared with women with age at first delivery from 21 to 25 years (OR, 1.13; 95% CI, 0.94–1.36). Interestingly, greater elevated risks of incontinence were observed among women who gave birth at the youngest ages compared with those women who first gave birth at 21 to 25 years. For those women younger than 21 years of age at their first births, the risk of frequent leaking was 1.27 (95% CI, 1.13–1.42). When they examined the effect of current age on the OR for age at first birth, there was no clear suggestion that the OR of leaking urine differed among the younger women and older women. Women with younger or older age at first birth who had ≥3 childbirths were at particularly high risk of frequent leaking, with a 70% to 80% greater prevalence than women with one child who had given birth between the ages of 21 and 25 years (OR, 1.78, 95% CI, 1.47–2.14 for younger age at birth and ≥3 births; OR, 1.70, 95% CI, 1.08–2.66 for older age at first birth and ≥3 births).
Long-term prospective studies (6 years or more) either suggested a relationship between AMA and persistent SUI (Glazner, Rortveit and Gordstein) or failed to confirm a relationship (Viktrup and Altman). Nevertheless, a relationship when observed was either marginal or attenuated with age.
Overall interpretation
Despite the presence of significant variation in definitions of incontinence and methodology used, it seems that the timing and stage of a woman’s life when risk factors are examined play a key role in the final determination of the significance of each factor. Studies that examined risk factors in young women a few years after delivery (Groutz, Fritel, etc.) demonstrated a significant role for vaginal delivery as an inciting factor with advanced maternal age, maternal pre-pregnancy BMI, incontinence in early pregnancy, and persistent incontinence 3 months after delivery as independent risk factors. So when we analyze pelvic floor trauma after vaginal delivery in women during their reproductive years for risk factors, there are certain risk factors that consistently present themselves.
To simplify the complexity of the multifactorial nature of SUI development, we propose that pathophysiologically, SUI results from an imbalance of injury to the pelvic floor with vaginal delivery and recovery mechanisms. The different risk factors that are described could be classified into two major categories: contributory and decompensating. Thus, maternal age, obesity, diabetes, and continence status before or during first pregnancy are contributing factors that affect either the degree of injury to the pelvic floor or the recovery mechanisms. Post-delivery incontinence status is an indicator of this balance. All other factors that could subsequently occur during the life of the women including aging would be considered decompensating to the overall balance. Menopause, chronic cough, development of diabetes, BMI increase, and smoking contribute to the imbalance that occurred in early years after the trauma. Therefore, when we look in retrospectively at the risk factors of SUI in elderly women or perimenopausal women we would not be able to see the same factors that we see when we examine women during their reproductive age.
Surgery for incontinence or pelvic organ prolapse is a modifier. It modifies, and in some situations changes, the nature of the disease. When Fritel examined the risk factors for severe SUI in perimenopausal women, he found that the risk of severe SUI increased with BMI, diabetes, and previous urinary incontinence surgery [9]. Neither the mode of first delivery nor the mode of all deliveries was associated with severe SUI in contrast to other studies which found that cesarean delivery had a protective effect against SUI. This is an example of how the time of evaluation can identify decompensating and modifying factors as important risks.
Summary and conclusions
The data on the role of maternal age in the development of SUI are inconclusive. Evidence for an independent risk factor is more often observed in short-term prospective studies. This effect might be attenuated by time from the index delivery and the severity of incontinence. The biological explanation for this observation is extremely intriguing. Does advanced age affect tissue susceptibility to trauma and tissue recovery? Current studies to further investigate the effects of AMA on development of SUI are being undertaken as the clinical relevance is increasing with more and more women having their first child at an advanced age.
References
Altman D, Ekstrom A, Gustafsson C, Lopez A, Falconer C, Zetterstrom J (2006) Risk of urinary incontinence after childbirth: a 10-year prospective cohort study. Obstet Gynecol 108:873–878
Baydock SA, Flood C, Schulz JA, MacDonald D, Esau D, Jones S, Hiltz CB (2009) Prevalence and risk factors for urinary and fecal incontinence four months after vaginal delivery. J Obstet Gynaecol Can 31:36–41
Carley ME, Turner RJ, Scott DE, Alexander JM (1999) Obstetric history in women with surgically corrected adult urinary incontinence or pelvic organ prolapse. J Am Assoc Gynecol Laparosc 6:85–89
Chin HY, Chen MC, Liu YH, Wang KH (2006) Postpartum urinary incontinence: a comparison of vaginal delivery, elective, and emergent cesarean section. Int Urogynecol J Pelvic Floor Dysfunct 17:631–635
Dietz HP, Simpson JM (2007) Does delayed child-bearing increase the risk of levator injury in labour? Aust N Z J Obstet Gynaecol 47:491–495
Diez-Itza I, Arrue M, Ibanez L, Murgiondo A, Paredes J, Sarasqueta C (2010) Factors involved in stress urinary incontinence 1 year after first delivery. Int Urogynecol J 21:439–45
Foldspang A, Mommsen S, Lam GW, Elving L (1992) Parity as a correlate of adult female urinary incontinence prevalence. J Epidemiol Community Health 46:595–600
Fritel X, Fauconnier A, Levet C, Benifla JL (2004) Stress urinary incontinence 4 years after the first delivery: a retrospective cohort survey. Acta Obstet Gynecol Scand 83:941–945
Fritel X, Ringa V, Varnoux N, Fauconnier A, Piault S, Breart G (2005) Mode of delivery and severe stress incontinence. A cross-sectional study among 2,625 perimenopausal women. BJOG 112:1646–1651
Glazener CM, Herbison GP, MacArthur C, Lancashire R, McGee MA, Grant AM, Wilson PD (2006) New postnatal urinary incontinence: obstetric and other risk factors in primiparae. BJOG 113:208–217
Grodstein F, Fretts R, Lifford K, Resnick N, Curhan G (2003) Association of age, race, and obstetric history with urinary symptoms among women in the Nurses’ Health Study. Am J Obstet Gynecol 189:428–434
Groutz A, Helpman L, Gold R, Pauzner D, Lessing JB, Gordon D (2007) First vaginal delivery at an older age: does it carry an extra risk for the development of stress urinary incontinence? Neurourol Urodyn 26:779–782
Hermansen IL, O’Connell BO, Gaskin CJ (2010) Women’s explanations for urinary incontinence, their management strategies, and their quality of life during the postpartum period. J Wound Ostomy Continence Nurs 37:187–192
Huang L, Sauve R, Birkett N, Fergusson D, van Walraven C (2008) Maternal age and risk of stillbirth: a systematic review. CMAJ 178:165–172
MacArthur C, Glazener CM, Wilson PD, Lancashire RJ, Herbison GP, Grant AM (2006) Persistent urinary incontinence and delivery mode history: a six-year longitudinal study. BJOG 113:218–224
Marsh F, Lynne R, Christine L, Alison W (2011) Obstetric anal sphincter injury in the UK and its effect on bowel, bladder and sexual function. Eur J Obstet Gynecol Reprod Biol 154:223–227
Pregazzi R, Sartore A, Troiano L, Grimaldi E, Bortoli P, Siracusano S, Guaschino S (2002) Postpartum urinary symptoms: prevalence and risk factors. Eur J Obstet Gynecol Reprod Biol 103:179–182
Rortveit G, Hunskaar S (2006) Urinary incontinence and age at the first and last delivery: the Norwegian HUNT/EPINCONT study. Am J Obstet Gynecol 195:433–438
Schytt E, Lindmark G, Waldenstrom U (2004) Symptoms of stress incontinence 1 year after childbirth: prevalence and predictors in a national Swedish sample. Acta Obstet Gynecol Scand 83:928–936
Stainton MC, Strahle A, Fethney J (2005) Leaking urine prior to pregnancy: a risk factor for postnatal incontinence. Aust N Z J Obstet Gynaecol 45:295–299
van Brummen HJ, Bruinse HW, van de Pol G, Heintz AP, van der Vaart CH (2006) Bothersome lower urinary tract symptoms 1 year after first delivery: prevalence and the effect of childbirth. BJU Int 98:89–95
Viktrup L (2002) The risk of lower urinary tract symptoms five years after the first delivery. Neurourol Urodyn 21:2–29
Viktrup L, Rortveit G, Lose G (2006) Risk of stress urinary incontinence twelve years after the first pregnancy and delivery. Obstet Gynecol 108:248–254
Yang X, Zhang HX, Yu HY, Gao XL, Yang HX, Dong Y (2010) The prevalence of fecal incontinence and urinary incontinence in primiparous postpartum Chinese women. Eur J Obstet Gynecol Reprod Biol 152:214–217
Acknowledgments
The authors thank Kerry O. Grimberg, Ph.D. for her medical editorial assistance.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hijaz, A., Sadeghi, Z., Byrne, L. et al. Advanced maternal age as a risk factor for stress urinary incontinence: a review of the literature. Int Urogynecol J 23, 395–401 (2012). https://doi.org/10.1007/s00192-011-1562-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1562-5