Abstract
Purpose
It was the aim to assess all published original research dealing with dynamic repair of the anterior cruciate ligament (ACL) and to provide a semi-quantitative analysis of clinical outcome reports.
Methods
Both OVIS and MEDLINE databases were utilized for allocation of articles. All preclinical and clinical studies related to dynamic intraligamentary stabilization (DIS) were identified. Results were tabulated and semi-quantitative analysis performed.
Results
Twenty-three articles related to DIS were identified. The predominant level of evidence ranged between II and IV, with only one level I study. Reported failure rates ranged between 4% and 13.6%. Most clinical studies only reported revision rates without referring to failure of restoring stability. Highest success was achieved with proximal ACL ruptures. Both the level of physical activity and patient age have been found to influence the risk of failure.
Conclusion
There is sufficient evidence to support that DIS repair may be an effective modality for the treatment of acute proximal tears of the ACL. However, comparative studies are lacking. Upcoming studies should compare the technique to ACL reconstruction with failure as an endpoint. Comparison to rigid methods of proximal fixation is also necessary to justify the need for dynamic fixation. Overall, there is evidence to suggest the potential space for ACL repair in the decision tree for individualized treatment planning. The best outcome will be in the hands of the best patient selectors.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A renewed interest in the repair of the anterior cruciate ligament (ACL) emerged during the recent years [32]. The principle of preserving the native ACL in an attempt to potentially preserve maximum proprioceptive tissue alongside the reduced drawback of donor site morbidity allowed for a continuous effort and research activity in ACL preserving research in the background of the thriving clinical expansion of ACL reconstruction [4, 29].
A technique that gained particular attention is dynamic fixation of the ACL. The idea is purely biomechanical and based on the principle that rigid fixation of sutures fail upon cyclic loading, resultant to natural motion of the knee [22]. The authors of the first reports of this technique stated that this is likely to explain the historically high failure rates of simple repair and that the only way to overcome the problem would be by providing some form of dynamic augmentation to withstand cyclic forces acting on the repair construct.
In the meanwhile, numerous reports were published in conjunction with this idea. Most reports referred to dynamic intraligamentary stabilization (DIS) using an augmentation system [24]. The device is commercially available under the name LigamysTM (Mathys AG, Bettlach, Switzerland).
Given that there has been much discussion around this technique in the orthopaedic community, the aim of this study was to: (1) identify all published original research on dynamic repair of the ACL. (2) Provide a semi-quantitative of reported failure rates and revision rates.
It was hypothesized that short-term failure rates of the procedure are less than 20% allowing for the assumption that the procedure may have a potential as a treatment option.
Materials and methods
Search strategy
A literature search was conducted in April of 2018. Two databases MEDLINE (PubMed) and OVID (Embase) were utilized for the search process without time restrictions. The following MeSH term combination was applied: [ligamys OR (dynamic AND intraligamentary AND (stabilization OR stabilisation)) OR (dynamic AND (stabilization OR stabilisation))] AND [acl OR (anterior AND cruciate AND ligament)]. After removal of duplicates, two reviewers screened titles for potentially relevant articles. Reference lists were also reviewed to capture any potentially missed articles.
Final inclusion of articles was based on the following criteria:
Inclusion criteria
-
Biomechanical studies related to dynamic ACL repair
-
Animal studies related to dynamic ACL repair
-
Biology and cell based studies related to response to dynamic ACL repair
-
Clinical studies of all types with primary focus on dynamic ACL repair
Exclusion criteria
-
Narrative reviews or systematic reviews
-
Reports of only one case
-
Articles with focus on multi-ligament injuries Schenk grade KD I or higher [33].
Quality assessment
Two epidemiologically trained investigators rated each clinical article. Level of evidence was given to each article based on the oxford centre of evidence-based medicine criteria. Furthermore, critical appraisal of study designs was performed using checklists of the Joanna Briggs institute. Disagreement between investigators was solved by consensus.
Data extraction
Data extraction from clinical studies included all parameters primarily related to failure: laxity as determined by instrumented measurement, pivots shift and revision ACL surgery. Further extracted outcome measures included subjective assessment scores.
Synthesis of results
Articles were arranged into categories based on study design. Descriptive presentation was provided for results and conclusions from basic research articles. Outcomes from clinical studies were tabulated and graphical illustrations provided. In case of heterogeneity of data reporting, means were calculated from medians with the following formula [21]:
Using the values of the median (m), low and high end of the range (a and b, respectively). This was not necessary for a sample size > 25 [21].
Results
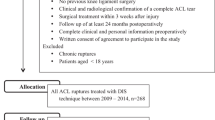
A total of 23 articles were identified. All were published between 2013 April 2018. A flow-chart presenting the article allocation process is shown in Fig. 1.
Study characteristics
The characteristics and critical appraisal of the included clinical research articles fulfilling the Oxford Center for Evidence Based Medicine (CEBM) criteria are illustrated in Table 1. There was one randomized trial, three case–control studies, two cohort studies and nine case series. The primary research questions varied.
Preclinical research
The first article was published in 2013 [23]. The authors of the study transected the ACL in 11 sheep, treating eight with DIS repair alongside microfracturing of the femoral footprint. The remaining three sheep received no ACL treatment and served as a control group. It was possible to demonstrate macroscopic healing of the ACL as well as microscopic scar tissue formation is the repair junction. The repair junction exhibited a high proportion of fibroblasts and increased vascularity at 3 months. The results of the animal study were later substantiated in a biomechanical cadaver study demonstrating that ACL DIS repair results in significantly less anterior posterior (ap) translation after 50 ROM cycles, with a 0.2 mm mean increase in laxity, compared to 8.1 mm increase in the group with rigid suture fixation [22]. The findings provided a potential explanation for historic failure rates associated with rigid suture repair. A later article published in 2016 confirmed these findings demonstrating a non significant increase in ap-translation [13]. Robotic measurements of both ap-translation and pivot shift at varying degrees of flexion were performed comparing DIS repair tensioned at either 60N or 80N, alongside ACL intact and deficient controls. Both 80N and 60N tensioning provided resemblance to native joint kinematics. However, an 80N pretension load provided a slightly enhanced natural kinematic resemblance in all degrees of flexion [31]. A further recent study published by Hoogeslag et al. [20] underlined prior findings, noting that anterior translation after DIS repair was maintained after 300 ROM cycles and did not significantly differ from the intact ACL. The study also demonstrated that static tape augmentation failed to maintain stabilizing properties after 300 ROM cycles [20]. The angle at with maximum tension is transferred to the system and ultimately the spring, was determined to be 0° of flexion (full extension) in a cadaveric study with optical spring motion capture [15]. Given that the spring loosens in flexion and tightens in extension, the recommendation to apply a preload of 80N in 0° of flexion to prevent overloading of the system, was made [15].
Finally, It was also shown that the maximum wear of the DIS implant in its functional lifetime would be 1.7 mg [27].
Clinical studies
Outcome studies scores
Eight articles reported on postoperative scores [3, 6, 9, 10, 19, 24, 25, 28]. The commonly reported scores were Tegner, International Knee Documentation Committee (IKDC) score, Lysholm score and subjective visual analogue scale (VAS) for satisfaction.
Pre-injury Tegner scores were frequently reported, in fact one inclusion criterion was a high level of activity exposing the knee to pivoting motions, constituting a Tegner score > 4. Most studies reported a median pre-injury Tegner score of six with varying ranges [3, 6, 9, 10, 24, 25, 28], indicating that a rather active population group was studied. One study reported on a group of very active patients with a Tegner score of eight prior to injury [28]. One study reported means instead of a medians, with a mean pre-injury Tegner score of 5.1 [19].
Only early follow-up was available from studies reporting postoperative outcome scores, ranging from a minimum of 1 year (n = 4 articles) to 2 or 3 years (n = 3 articles) and only article reported the 5-year follow-up of the first series of treated patients [10].
The lowest and highest reported medians and means from the studies above are illustrated in Fig. 2.
Anterior posterior translation
Eight articles reported anterior posterior translation upon early follow-up [3, 6, 9, 10, 24, 25, 28, 30]. Delta anterior posterior translation to the contralateral was the most commonly reported measure, with means ranging from 1.4 to 2.1 mm for the vast majority of studies (Fig. 3).
Revision rate
Twelve reported the rate revision to ACL reconstruction [3, 5, 6, 9, 10, 14, 17,18,19, 24, 25, 28] as seen in Fig. 4. Only short-term follow-up is present, although one article of the first 10 patients provided 5-year outcome results [10]. First year follow-up reports showed slightly lower revision rates than reports published later. One-year follow-up studies reported the following rates of ACL revision: 2.1%, 2.9% 3.8%, 6.6%, 15% [3, 6, 19, 25, 28]. Reports with 2-year follow-up or more reported the following ACL revision rates: 7.9% 8%, 8.7%, 9.4%, 10%, 11% [5, 9, 10, 14, 17, 18, 24]. One case series of the first 10 patients undergoing this procedure with 5-year follow-up demonstrated a failure rate of 20% (two patients) at 5 years [10].
Failure rate
Five articles reported failure of ACL repair with the DIS repair [3, 18, 19, 24, 26]. The definition of failure was not only ACL revision but also insufficient restoration of stability, which was variably defined as persisting laxity/instability based on clinical exam, or confirmed upon follow-up arthroscopy performed during implant removal. Given that the reported failure rates were higher than the corresponding revision rates, not all patients undergo revision. The reported failure rates of the studies were as follows: 4.0%, 8.5%, 10.0%, 11.0%, 13.6% [3, 18, 19, 24, 26] (Fig. 5).
Multivariate analysis
Several regression analyses were performed to identify potential factors likely to influence the likelihood of revision or failure of the procedure. Henle et al. [17] proposed age < 24 years, a high pre-injury level of physical activity (Tegner score > 5) and residual knee joint laxity as risk factors for ACL revision. Krismer et al. [26] proposed two factors influencing failure, namely a mid-substance location of the rupture and a pre-injury Tegner score of > 7. A further study showed that surgeon experience does not influence the risk of ACL revision [18]. It was suggested that with narrowing of indications, considering the above factors, failure rates could be reduced to 3.9% [26].
Comparative studies
A comparative study by Bieri et al. [5] compared DIS repair of the ACL in 53 patients to a matched group of patients undergoing ACL reconstruction. The two groups did not differ regarding the rates of secondary surgery or ACL revision [5]. Treatment costs and time of absence from work were found to be similar between both groups. The course of postoperative work incapacity was also very similar between the two groups [5].
A study by Evangelopoulos et al. [11] compared two groups with mid-substance ACL ruptures treated with DIS, one with collagen a membrane coverage, the other without. It was noted in that study that the complication rate was significantly reduced, which was defined as the incidence of failure or loss of motion due to hypertrophic scar tissue formation.
One prospective comparative study examined postoperative gait and functional outcome after either DIS repair or ACL reconstruction in a two-armed trial [30]. The study proved that patients undergoing DIS repair showed a significantly higher level of postoperative activity, measured with an accelerometric step counter. However, functional scores did not differ between groups [30].
A further non-clinical, comparative study looking into cost-effectiveness of DIS repair, noted that quality adjusted life years (QUALY) were slightly higher in patients undergoing DIS, compared to reconstruction (2.34 versus 2.26). This was associated with an increased incremental cost-effectiveness ratio of DIS at the time of article publication in 2014. The results are to be interpreted with caution, given the variations in implant costs and time-related changes.
Discussion
The most important finding of this underlines the fact that there is Level IV, III, II and I evidence to support that ACL repair and dynamic stabilization is a safe and potentially effective procedure for the treatment of acute ACL tears in a select group of patients.
It was noticeable that all research related to ACL repair and dynamic stabilization was published within a short time frame following the first published article in 2013. The fact that level I evidence was rapidly reached denotes good reporting and satisfying academic scrutiny. This may have been resultant to the initial skeptical reception by the orthopedic community. Historic reports of unsuccessful repair alongside complete replacement of repair techniques by graft reconstruction all contributed to the prevailing orthodoxy that the ACL does not heal [8, 12]. ACL reconstruction, therefore, captured the clinical spotlight during the last decades [1, 2]. There is now sufficient evidence to allow for the statement that the ACL does have a healing potential. The art in the current era of individualized treatment is in the selection of the correct candidate for primary repair.
Furthermore, it is clear that the majority of articles actually report revision rates or re-ruptures after DIS repair, but only a minority report actual failure rates. The difference between the two is that a failure is not necessarily a traumatic re-rupture or a revision, but could also be insufficient restoration of stability identified upon clinical exam. It is true, as seen in the studies above, that not every patient with insufficient restoration of stability would require ACL revision surgery, since studies illustrating both demonstrated failure rates that were higher than revision rates [3, 24]. Still, the procedure relies on ACL healing, which should lead to elimination of laxity, and its success should be defined as such. Authors of upcoming articles should be urged to include failure rates as an outcome measure, defined as insufficient restoration of stability based on criteria of the international knee documentation committee (IKDC) [16]. The overall failure rates in the short-term were reported to reach 15%, though patient selection with regard to rupture location showed a marked reduction in that rate. High level athletes are more prone to suffer failure, but this is also the case after reconstructive procedures. Given the fact that no clinical study with failure as an endpoint, compared DIS repair to reconstruction, it is also difficult to deduce a sound conclusion from the results above, regarding superiority or inferiority of the procedure. This is underlined by the fact that failure and revision rates after ACL reconstruction have broad reported ranges (3.2–27%) in the long term [7]. Only true comparative studies would provide a definitive answer.
Multivariate analyses highlighted important aspects regarding the potency of this technique and the potential large success that may be associated with narrowing of indications. It was agreed upon that proximal ruptures are associated with the lowest failure rates. Young age and high level of physical activity were postulated as further possible factors likely to influencing failure. Therefore, given the adequate evidence, the procedure should be limited to proximal ruptures, and caution is necessary when treating highly active sporty patients.
It is fair to mention that proximal ruptures have also recently been shown to respond well to rigid fixation forms [32]. This ultimately allows the true value of dynamic fixation to be questioned. Given the implant associated costs and invasiveness of dynamic fixation, dynamic repair would have to prove itself superior to rigid proximal ACL repair with comparative studies in the near future.
The limitations of the current study are associated with the heterogeneity of included studies. This is due to the rather small number of studies included and the novelty of the area of research, which should justify the conduction of the current review. The second weakness is the lack of pooling and meta-analysis of results, which is also attributed to the heterogeneity.
The strength of this study is to be seen in its clinical impact. It was shown here that ACL repair is likely to provide good outcome in a select group of patients and predictive factors of failure were highlighted. The best outcome will, therefore, be in the hands of best patient selectors.
Conclusion
There are numerous clinical studies of levels IV, III, II and I evidence indicating a potential role for ACL DIS repair and possible space for it in the decision tree for ACL treatment. It is clear that indications have been narrowed and limited to proximal ruptures. Highly active physically demanding patients are also at higher risk of failure. The art, therefore, remains in good patient selection.
References
Ahmad SS, Evangelopoulos DS, Abbasian M, Roder C, Kohl S (2014) The hundred most-cited publications in orthopaedic knee research. J Bone Joint Surg Am 96:e190
Ahmad SS, Meyer JC, Krismer AM, Ahmad SS, Evangelopoulos DS, Hoppe S et al (2017) Outcome measures in clinical ACL studies: an analysis of highly cited level I trials. Knee Surg Sports Traumatol Arthrosc 25:1517–1527
Ateschrang A, Ahmad SS, Stockle U, Schroeter S, Schenk W, Ahrend MD (2018) Recovery of ACL function after dynamic intraligamentary stabilization is resultant to restoration of ACL integrity and scar tissue formation. Knee Surg Sports Traumatol Arthrosc 26:589–595
Barrett DS (1991) Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br 73:833–837
Bieri KS, Scholz SM, Kohl S, Aghayev E, Staub LP (2017) Dynamic intraligamentary stabilization versus conventional ACL reconstruction: a matched study on return to work. Injury 48:1243–1248
Buchler L, Regli D, Evangelopoulos DS, Bieri K, Ahmad SS, Krismer A et al (2016) Functional recovery following primary ACL repair with dynamic intraligamentary stabilization. Knee 23:549–553
Crawford SN, Waterman BR, Lubowitz JH (2013) Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy 29:1566–1571
Drogset JO, Grøntvedt T, Robak OR, Mølster A, Viset AT, Engebretsen L (2006) A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. JBJS 88:944–952
Eggli S, Kohlhof H, Zumstein M, Henle P, Hartel M, Evangelopoulos DS et al (2015) Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. Knee Surg Sports Traumatol Arthrosc 23:1215–1221
Eggli S, Roder C, Perler G, Henle P (2016) 5 years results of the first ten ACL patients treated with dynamic intraligamentary stabilisation. BMC Musculoskelet Disord 17:105
Evangelopoulos DS, Kohl S, Schwienbacher S, Gantenbein B, Exadaktylos A, Ahmad SS (2017) Collagen application reduces complication rates of mid-substance ACL tears treated with dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc 25:2414–2419
Feagin JA Jr, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4:95–100
Haberli J, Henle P, Acklin YP, Zderic I, Gueorguiev B (2016) Knee joint kinematics with dynamic augmentation of primary anterior cruciate ligament repair—a biomechanical study. J Exp Orthop 3:29
Haberli J, Jaberg L, Bieri K, Eggli S, Henle P (2018) Reinterventions after dynamic intraligamentary stabilization in primary anterior cruciate ligament repair. Knee 25:271–278
Häberli J, Voumard B, Kösters C, Delfosse D, Henle P, Eggli S et al (2018) Implant preloading in extension reduces spring length change in dynamic intraligamentary stabilization: a biomechanical study on passive kinematics of the knee. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5002-7
Hefti E, Müller W, Jakob RP, Stäubli H-U (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surgery, Sports Traumatology. Arthroscopy 1:226–234
Henle P, Bieri KS, Brand M, Aghayev E, Bettfuehr J, Haeberli J et al (2018) Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 26:1182–1189
Henle P, Bieri KS, Haeberli J, Arnout N, Victor J, Herbort M et al (2018) Surgeon experience with dynamic intraligamentary stabilization does not influence risk of failure. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4847-0
Henle P, Röder C, Perler G, Heitkemper S, Eggli S (2015) Dynamic intraligamentary stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: case series experience of the first three years. BMC Musculoskelet Disord 16:27
Hoogeslag RAG, Brouwer RW, Huis In ‘t Veld R, Stephen JM, Amis AA (2018) Dynamic augmentation restores anterior tibial translation in ACL suture repair: a biomechanical comparison of non-, static and dynamic augmentation techniques. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4848-z
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 5:13
Kohl S, Evangelopoulos DS, Ahmad SS, Kohlhof H, Herrmann G, Bonel H et al (2014) A novel technique, dynamic intraligamentary stabilization creates optimal conditions for primary ACL healing: a preliminary biomechanical study. Knee 21:477–480
Kohl S, Evangelopoulos DS, Kohlhof H, Hartel M, Bonel H, Henle P et al (2013) Anterior crucial ligament rupture: self-healing through dynamic intraligamentary stabilization technique. Knee Surg Sports Traumatol Arthrosc. 21:599–605
Kohl S, Evangelopoulos DS, Schär MO, Bieri K, Müller T, Ahmad SS (2016) Dynamic intraligamentary stabilisation: initial experience with treatment of acute ACL ruptures. Bone Joint J. 98-B:793–798
Kosters C, Herbort M, Schliemann B, Raschke MJ, Lenschow S (2015) Dynamic intraligamentary stabilization of the anterior cruciate ligament. Operative technique and short-term clinical results. Unfallchirurg. 118:364–371
Krismer AM, Gousopoulos L, Kohl S, Ateschrang A, Kohlhof H, Ahmad SS (2017) Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilisation. Knee Surg Sports Traumatol Arthrosc 25:3923–3928
May C, Gueorguiev B, Heuberger R, Sague J, Gross C, Henle P et al (2017) Low metallic wear of dynamic intraligamentary stabilization. Tribol Int. 109:217–221
Meister M, Koch J, Amsler F, Arnold MP, Hirschmann MT (2018) ACL suturing using dynamic intraligamentary stabilisation showing good clinical outcome but a high reoperation rate: a retrospective independent study. Knee Surg Sports Traumatol Arthrosc 26:655–659
Relph N, Herrington L, Tyson S (2014) The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy 100:187–195
Schliemann B, Glasbrenner J, Rosenbaum D, Lammers K, Herbort M, Domnick C et al (2018) Changes in gait pattern and early functional results after ACL repair are comparable to those of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 26:374–380
Schliemann B, Lenschow S, Domnick C, Herbort M, Haberli J, Schulze M et al (2017) Knee joint kinematics after dynamic intraligamentary stabilization: cadaveric study on a novel anterior cruciate ligament repair technique. Knee Surg Sports Traumatol Arthrosc 25:1184–1190
van Eck CF, Limpisvasti O, ElAttrache NS (2018) Is there a role for internal bracing and repair of the anterior cruciate ligament? a systematic literature review. Am J Sports Med 46:2291–2298
Walker D, Hardison R, Schenck R (1994) A baker’s dozen of knee dislocations. Am J Knee Surg 7:117–124
Funding
The authors received no funding for the conduction of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
Given the type of study, an ethical approval was not necessary for the conduction of this study.
Rights and permissions
About this article
Cite this article
Ahmad, S.S., Schreiner, A.J., Hirschmann, M.T. et al. Dynamic intraligamentary stabilization for ACL repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 27, 13–20 (2019). https://doi.org/10.1007/s00167-018-5301-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5301-z