Abstract
Purpose
Dynamic intraligamentary stabilization (DIS) has been introduced as a new technique to repair the torn anterior cruciate ligament (ACL) and to restore knee joint kinematics after an acute ACL tear. Aim of the present study was to compare the early post-operative activity, restoration of gait pattern and functional results after DIS in comparison with primary ACL reconstruction (ACLR) for acute ACL tears. It was hypothesized that functional results, post-operative activity and changes in gait pattern after DIS are comparable to those after ACLR.
Methods
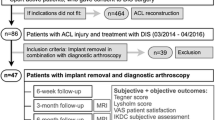
Sixty patients with acute ACL tears were included in this study and underwent either DIS or ACLR with an anatomic semitendinosus autograft in a randomized manner. Patients were equipped with an accelerometric step counter for the first 6 weeks after surgery in order to monitor their early post-operative activity. 3D gait analysis was performed at 6 weeks and 6 months after surgery. Temporal-spatial, kinematic and kinetic parameters were extracted and averaged for each subject. Functional results were recorded at 6 weeks, 6 months and 12 months after surgery using the Tegner activity scale, International Knee Documentation Committee score and Lysholm score.
Results
Patients who underwent DIS showed an increased early post-operative activity with significant differences at week 2 and 3 (p = 0.0241 and 0.0220). No significant differences between groups were found for knee kinematic and kinetic parameters or the functional scores at any time of the follow-up. Furthermore, the difference in anterior tibial translation was not significantly different between the two groups (n.s.).
Conclusion
Early functional results and changes in gait pattern after DIS are comparable to those of primary ACLR. Therefore, ACL repair may be an alternative to ACLR in this cohort of patients.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dynamic intraligamentary stabilization (DIS) has been introduced as a new technique to repair the torn anterior cruciate ligament (ACL) and to restore knee joint kinematics after an acute ACL tear. The torn ACL is reattached to its femoral insertion site and the knee is held continuously in a posterior drawer position during the healing period by a dynamic spring fixed in the proximal tibia. Early biomechanical and clinical results after this procedure were promising. Henle et al. [10] published clinical results of 278 patients treated with DIS and found excellent functional scores and a high patient satisfaction. However, primary ACL reconstruction (ACLR) using tendon autografts or allografts is still the standard procedure to treat these injuries. Although good functional results can be achieved, ACLR is associated with complications such as re-tears, particularly in young and active patients, and the perioperative morbidity is increased if a tendon has to be harvested [2, 21, 23]. Therefore, ACL-preserving restoration of knee joint stability has always been attempted.
Furthermore, it is well known that ACL tears and reconstructions lead to abnormal knee joint biomechanics during gait. In particular, in the sagittal plane, changes in knee kinematics and moments have to be expected and may be associated with early development of posttraumatic arthritis [7]. Surgical intervention therefore must aim to restore physiologic knee kinematics.
So far, there are only case series reporting results of DIS. Aim of the present study was therefore to compare the early functional results after DIS with those after ACL reconstruction in a prospective randomized study. It was hypothesized that functional results, knee joint stability, early post-operative activity measured by a step counter and changes in gait pattern after DIS are comparable to those after ACLR.
Materials and methods
In 2014 and 2015, 62 patients with acute ACL tears were included in this study. Only those patients were included who presented with an acute (<3 weeks) isolated ACL tear. Patients with concomitant lesions of the menisci and collateral ligaments were excluded due to its influence on the post-operative rehabilitation protocol. Similarly, those patients with previous knee injuries on both the affected and contralateral knee were also excluded. Two patients had to be excluded after a previously undetected meniscus lesion that had to be fixed during surgery. Therefore, 60 patients were finally followed.
Patients were allocated to undergo either DIS (Ligamys, Mathys Medical, Bettlach, Switzerland) or ACLR with an anatomic semitendinosus autograft by block randomization. A sealed envelope prepared by an assistant who was not involved in the study was opened in theatre just before surgery (for sample size calculation see “statistical analysis). The demographics of the two groups are illustrated in Table 1.
Surgical technique
All operations were performed within 21 days after the injury (Table 1). Under general anaesthesia and with perioperative antibiotic prophylaxis, patients were placed in a supine position. The DIS procedure was performed according to the technique described by Kösters al. [11]. Anatomic single-bundle ACL reconstruction was performed using a four-stranded semitendinosus autograft [18].
After both procedures, the knee was placed in a knee immobilizer for 4 days. Afterwards, patients underwent a brace-free rehabilitation programme. Full weight bearing was allowed after 2 weeks, and range of motion was not limited. Quadriceps and hamstrings strength training was started using closed chain knee exercises. Intensive proprioceptive exercises were initiated after 3 weeks. Running was allowed after 6 weeks. Pivoting and competitive sports were allowed after at least 5 months but only after prior clinical examination and return-to-sports testing.
Follow-up examinations
Patients were evaluated clinically at the date of primary presentation and inclusion in the study and at 6 weeks, 6 months and 12 months after surgery. At every time point, the Tegner activity scale, International Knee Documentation Committee (IKDC) score and Lysholm score were recorded. Patients’ satisfaction with the surgical outcome was evaluated using a visual analogue scale with 10 points indicating a complete satisfaction.
Anterior tibial translation of the affected and the non-injured contralateral knees was assessed at 30 degrees flexion using a Rolimeter (Aircast, Neubeuern, Germany) at 6 months and 12 months after surgery.
Furthermore, patients were equipped with a light-weight accelerometric step counter (StepWatch Activity Monitor, Modus Health, Washington DC, USA) for the first 6 weeks after surgery in order to monitor the early post-operative activity of the patients. The number of gait cycles was recorded continuously in 1-min intervals during the waking hours. The weekly mean was determined for each of the 6 weeks and compared between the two intervention groups.
3D gait analysis
3D gait analysis was performed at 6 weeks and 6 months after surgery. A six-camera system (60 Hz, Cohu cameras, Motion Analysis Corporation, Santa Rosa, CA, USA) and two strain-gauge force plates (600 Hz, AMTI, Watertown, MA, USA) were used for three-dimensional movement analysis. Twenty-five reflective markers were fixed to every patient according to the Helen Hayes marker set. Patients walked at self-selected speed across the force plates and repeated trials were stored for further analyses (EVA 5.2, Expert Vision and Orthotrak 4.1, Motion Analysis Corporation). Temporal-spatial, kinematic and kinetic parameters were extracted and averaged for each subject. The results were statistically analysed for significant differences between the affected limb and the healthy contralateral limb, between groups and between the two time points.
IRB approval was obtained prior the study by the ethics board of the University of Münster (2013-414-f-S).
Statistical analysis
A power analysis was performed prior to the study. 28 patients were to be included per group based on an expected mean difference in anterior tibial translation of 3 mm (regarded as clinically significant), a standard deviation of ±2 mm and an estimated loss to follow-up of 15% (α = 0.05, β = 0.8). The difference in anterior tibial translation measured with the Lachman/Rolimeter test was chosen for the power analysis because of its high sensitivity and diagnostic accuracy [12, 16].
In case of multiple testing, the Bonferroni correction was used to adjust the level of significance. The Friedman test was used to analyse differences in score results within one group at the four different time points during follow-up (prior to the injury, 6 weeks, 6 months, 1 year). Differences in gait parameters within the group were assessed using the Wilcoxon-signed-rank test whereas the Mann–Whitney U test was used to evaluate differences between the two intervention groups.
Results
Functional results
The mean Tegner activity scale prior to the injury was 6 (range 4–10) in both groups (Table 1). The results for the Lysholm and IKDC scores are summarized in Table 2. Whereas there were significant differences within the two groups between the 6-week, 6-month and 1-year follow-up, no significant differences could be found between the two groups (for exact p values see supplemental material).
The difference in anterior tibial translation between the injured and the contralateral knee was 7.6 mm in the DIS group and 8.4 mm in the ACLR group prior to the intervention. At the 12-month follow-up, this difference decreased to 1.7 mm in the DIS group and 1.4 mm in the ACLR group. Again, this difference was not significant (n.s.).
Patient satisfaction at the final follow-up was 8.8/10 (SD 1.4) in the DIS group and 9.1/10 (SD 1.5) in the ACLR group.
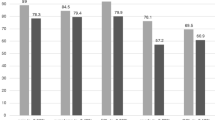
Step counter
The number of gait cycles increased continuously from week 1 to week 6 in both groups. Early post-operative activity was slightly higher in the DIS group at every week (Fig. 1). However, a statistically significant difference was only found for week 2 and 3 (p = 0.0241 and p = 0.0220).
Number of gait cycles (weekly mean) within the first 6 post-operative weeks. Although the number of gait cycles was higher in the DIS group throughout the 6 weeks, a significant difference was only found for weeks 2 and 3. DIS dynamic intraligamentary stabilization, ACLR anterior cruciate ligament reconstruction
Gait analysis
The results of the gait analysis are illustrated in Figs. 2, 3 and Table 3. In general, a persisting limitation of gait performance could be seen at the 6-week follow-up and an improvement could be observed in most of the knee-related parameters in both groups from the 6-week to the 6-month follow-up.
Knee kinematics in the sagittal plane at 6 weeks and 6 months. Again, no significant differences were found between the two groups (see also Table 2). DIS dynamic intraligamentary stabilization, ACLR anterior cruciate ligament reconstruction, max1_KneeFlx maximum knee flexion during stance, min_KneeFlx minimum knee flexion during stance, max2_KneeFlx maximum knee flexion during swing
Vertical ground reaction force at 6 weeks and 6 months (see also Table 2). DIS dynamic intraligamentary stabilization, ACLR anterior cruciate ligament reconstruction, max1_grf ground reaction force peak at weight acceptance, min_gfr ground reaction force at mid-stance, max2_grf ground reaction force peak at pre-swing, BW body weight
With respect to the temporal-spatial parameters, a significant improvement was seen in both groups with an increased gait velocity (DIS +5%, p = 0.002; ACLR +6%, p = 0.017) and step length (DIS +4%, p = 0.003; ACLR +3%, p = 0.042).
For the knee kinematics, a significant improvement of both groups was seen most clearly in an increased range of motion during the stance phase and swing phase (Knee ROM1: DIS +48%, p = 0.002; ACLR +23%, p < 0.001. Knee ROM2: DIS +27%, p < 0.001; ACLR +19%, p < 0.001).
The kinetic parameters also revealed an improved function with more dynamic vertical ground reaction forces as indicated in higher force peaks during weight acceptance and push-off and a lower minimum during mid-stance (Max1: DIS +5%, p < 0.001; ACLR +5%, p = 0.002. Min: DIS −7%, p < 0.001; ACLR −3%, p < 0.022. Max2: DIS +5%, p < 0.001; ACLR +4%, p < 0.001).
However, statistically significant differences between the DIS and the ACLR group could not be observed for any parameter at any time.
Discussion
The most important finding of the present study is that no significant differences could be observed between the DIS and ACLR group with regard to all parameters assessed during gait analysis and to the outcome scores as well as to the anterior tibial translation. Analysis of the data collected with the step counter even revealed a higher early post-operative activity in the DIS group. Thus, DIS can provide results that are comparable to ACLR within a short post-operative follow-up period.
The DIS represents an innovative technique for ACL-preserving restoration of anterior knee stability after an acute ACL tear. In the past, several efforts have been made in order to suture and reattached the torn ACL [14, 15, 17, 20]. However, functional results of suture repair were not very satisfying. In 1992, Pässler et al. described a technique of augmented suture repair. After repair of the torn ACL using sutures as described by Marshall, they used a synthetic device in order to augment the repaired ACL and to provide biomechanical stability during the healing process [17]. Although patients’ satisfaction was high, only 51% of the patients returned to their pre-injury activity level. Furthermore, a mean difference in anterior tibial translation of 2.4 mm between the injured and the contralateral side remained. A similar technique, ligament bracing, was introduced recently for operative treatment of knee dislocations and has also been used for acute ACL repair [8, 9, 26]. So far, no reports on functional results after internal bracing of acute ACL tears exist.
One major disadvantage of the augmented repair techniques described above is the rigid fixation that does not take the length change of the ACL during knee flexion–extension into account. Lubowitz found an intraarticular length change of the graft after anatomic ACLR of 6.7 mm between 120° and 0° degrees of flexion [13]. The DIS implant, that is equipped with a spring within the tibial monobloc, allows for an 8-mm elongation of the intraarticular polyethylene suture and therefore incorporates the non-isometric kinematic behaviour of the ACL. Thus, with the DIS, the knee pulled into a posterior drawer position with a constant preload during full range of motion. In a previous biomechanical study, we demonstrated that knee joint kinematics after DIS were comparable to those of the ACL-intact knee under simulation of Lachman- and Pivot-shift tests [22].
The first clinical results of the DIS technique were promising and could be confirmed with additional studies with larger cohorts of patients and longer follow-up times [3, 4, 10, 11]. However, no study compared the functional results of this relatively new technique to ACLR so far. The present study demonstrated similar results in a short-term follow-up period when compared to ACLR using autologous hamstring grafts. Although the results are comparable, a longer follow-up is required in order to allow for evident conclusions with regard to functional results, knee joint stability and rate of recurrence. Henle et al. [10] reported a recurrence rate of approximately 4% in 197 patients treated with DIS who were followed for at least 6 months. Re-ruptures occurred between 106 and 740 days post-operatively. In addition, three patients of the same cohort presented with a subjective giving way as a sign of insufficient healing but did not undergo revision surgery. Thus, the rate of recurrence seems to be slightly increased when compared to ACLR. Andernord et al. [1] analysed data from the Swedish national knee ligament register and found a 2-year revision rate of 1.8% in a cohort of 16,930 patients. Fältström et al. [5] reported of a 4.3% revision rate within 5 years after the index procedure. It has yet to be investigated in further studies whether DIS can maintain its good results over a long-term follow-up period or will be associated with an increased failure rate over time.
With regard to the gait analysis, similar changes in gait patterns could be found for the two intervention groups. It is well known from other studies, that ACL reconstruction leads to changes in knee joint kinematics and moments [6, 7, 24, 25].
As shown in this study, gait patterns normalize over time. While patients in both group showed limited knee flexion angles and lower ground reaction forces 6 weeks after the surgery, these parameters return to almost physiologic values at the 6-month follow-up. However, some deficits still persist at that time. This is in accordance with results of a study of Roewer et al. [19] who found still asymmetric knee angles, knee moments, and knee power profiles during gait analysis performed 6 months after ACLR in non-copers after an ACL tear. Similarly, Gokeler et al. [6] concluded from a systematic review that return to normal gait after ACLR can take up to 5 years after the surgical intervention if it fully recovers at all. Although persistent alterations in gait patterns are suspected to be a risk factor for the development of posttraumatic osteoarthritis, no study confirmed this causality yet.
Conclusion
In this prospective randomized trial, patients who underwent DIS for an acute ACL tear showed comparable functional results and knee joint stability in the short-term follow-up when compared to patients who had primary ACLR. Changes in gait patterns were also similar in both group and normalized over time. The only significant difference was a higher early post-operative activity level in the DIS group as recorded by a step counter. It has yet to be determined whether the results after DIS remain comparable to those of primary ACL after longer follow-up periods.
References
Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K (2015) Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med 43(1):121–127
Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA (2012) Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med 40(9):1985–1992
Eggli S, Kohlhof H, Zumstein M, Henle P, Hartel M, Evangelopoulos DS, Bonel H, Kohl S (2014) Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. Knee Surg Sports Traumatol Arthrosc 23(4):1215–1221
Eggli S, Roder C, Perler G, Henle P (2016) Five year results of the first ten ACL patients treated with dynamic intraligamentary stabilisation. BMC Musculoskelet Disord 17:105
Fältström A, Hagglund M, Magnusson H, Forssblad M, Kvist J (2016) Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc 24(3):885–894
Gokeler A, Benjaminse A, van Eck CF, Webster KE, Schot L, Otten E (2013) Return of normal gait as an outcome measurement in acl reconstructed patients. A systematic review. Int J Sports. Phys Ther 8(4):441–451
Hart HF, Culvenor AG, Collins NJ, Ackland DC, Cowan SM, Machotka Z, Crossley KM (2016) Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med 50(10):597–612
Heitmann M, Dratzidis A, Jagodzinski M, Wohlmuth P, Hurschler C, Puschel K, Giannakos A, Preiss A, Frosch KH (2014) Ligament bracing–augmented cruciate ligament sutures: biomechanical studies of a new treatment concept. Unfallchirurg 117(7):650–657
Heitmann M, Gerau M, Hotzel J, Giannakos A, Frosch KH, Preiss A (2014) Ligament bracing–augmented primary suture repair in multiligamentous knee injuries. Oper Orthop Traumatol 26(1):19–29
Henle P, Roder C, Perler G, Heitkemper S, Eggli S (2015) Dynamic intraligamentary stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: case series experience of the first three years. BMC Musculoskelet Disord 16:27
Kösters C, Herbort M, Schliemann B, Raschke MJ, Lenschow S (2015) Dynamic intraligamentary stabilization of the anterior cruciate ligament. Operative technique and short-term clinical results. Unfallchirurg 118(4):364–371
Leblanc MC, Kowalczuk M, Andruszkiewicz N, Simunovic N, Farrokhyar F, Turnbull TL, Debski RE, Ayeni OR (2015) Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 23(10):2805–2813
Lubowitz JH (2014) Anatomic ACL reconstruction produces greater graft length change during knee range-of-motion than transtibial technique. Knee Surg Sports Traumatol Arthrosc 22(5):1190–1195
Marshall JL, Warren RF, Wickiewicz TL (1982) Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med 10(2):103–107
Marshall JL, Warren RF, Wickiewicz TL, Reider B (1979) The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop Relat Res 143:97–106
Mulligan EP, McGuffie DQ, Coyner K, Khazzam M (2015) The reliability and diagnostic accuracy of assessing the translation endpoint during the lachman test. Int J Sports Phys Ther 10(1):52–61
Paessler HH, Deneke J, Dahners LE (1992) Augmented repair and early mobilization of acute anterior cruciate ligament injuries. Am J Sports Med 20(6):667–674
Petersen W, Forkel P, Achtnich A, Metzlaff S, Zantop T (2013) Anatomic reconstruction of the anterior cruciate ligament in single bundle technique. Oper Orthop Traumatol 25(2):185–204
Roewer BD, Di Stasi SL, Snyder-Mackler L (2011) Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech 44(10):1948–1953
Sandberg R, Balkfors B, Nilsson B, Westlin N (1987) Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg Am 69(8):1120–1126
Sanders TL, Pareek A, Hewett TE, Levy BA, Dahm DL, Stuart MJ, Krych AJ (2017) Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc 25(1):222–228
Schliemann B, Lenschow S, Domnick C, Herbort M, Haberli J, Schulze M, Wahnert D, Raschke MJ, Kösters C (2015) Knee joint kinematics after dynamic intraligamentary stabilization: cadaveric study on a novel anterior cruciate ligament repair technique. Knee Surg Sports Traumatol Arthrosc 25(4):1184–1190
Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr (2004) Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med 32(8):1986–1995
Webster KE, Feller JA (2011) Alterations in joint kinematics during walking following hamstring and patellar tendon anterior cruciate ligament reconstruction surgery. Clin Biomech 26(2):175–180
Webster KE, Wittwer JE, O'Brien J, Feller JA (2005) Gait patterns after anterior cruciate ligament reconstruction are related to graft type. Am J Sports Med 33(2):247–254
Wilson WT, Hopper GP, Byrne PA, MacKay GM (2016) Anterior cruciate ligament repair with internal brace ligament augmentation. Surg Technol Int XXIX:273–278
Acknowledgements
A native speaker prior to submission edited the manuscript. We thank MAD for their help with the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
BS, MH and CK are consultants for the Mathys Medical AG. MH is a consultant for Medacta and Karl Storz. All other authors declare that they have no conflict of interest.
Funding
No funding was received.
Ethical approval
IRB approval was obtained prior to the study by the Ethics Board of the University of Münster (2013-414-f-S).
Informed consent
Informed consent was obtained from all patients included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schliemann, B., Glasbrenner, J., Rosenbaum, D. et al. Changes in gait pattern and early functional results after ACL repair are comparable to those of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26, 374–380 (2018). https://doi.org/10.1007/s00167-017-4618-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4618-3