Abstract
Purpose
Dynamic intraligamentary stabilization (DIS) is recognized as a ligament preserving technique for the treatment of acute anterior cruciate ligament (ACL) injuries. The aim of this study was to assess the integrity and morphology of the recovered ACL after DIS repair.
Methods
The cohort comprised 47 patients with an acute proximal ACL rupture undergoing DIS repair. All patients underwent diagnostic arthroscopy after a minimum postoperative interval of 6 months for semi-quantitative evaluation of ACL integrity, function and scar tissue formation. Tegner, Lysholm and International Knee Documentation Committee (IKDC) scores as well as objective anteroposterior (ap) translation were assessed at 6 weeks, 3-, 6- and 12 months postoperatively.
Results
Full restoration of the ACL volume was affirmed in 30 (63.8%) patients and two-third restoration in 13 (27.7%). Hypertrophic scar formation was observed in 23 (48.9%) patients. Forty-four patients (93.6%) demonstrated sufficient ACL tensioning intraoperatively upon anterior stress. At final follow-up, the median Tegner activity level was 5.5 (3–10), Lysholm and IKDC scores were 100 (64–100) and 94 (55–100) points, respectively. The mean ap-translation differed from the normal knee by 2.1 ± 2.2 mm. Deficient ACL recovery was noted in four patients (8.5%), none of which required secondary reconstructive surgery.
Conclusion
The results demonstrate that clinical recovery of ACL function after DIS repair is resultant to both restoration of ACL volume and scar tissue formation. Factors influencing the degree of scar tissue formation need further investigation to enable future attempts of guiding a balanced biological healing response.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoration of the functional anatomy of a torn anterior cruciate ligament (ACL) defines the primary goal of surgical treatment [3, 4].
Historic reports of primary fixation techniques demonstrated high failure rates, subsequently leading to the shift of principle towards ACL reconstruction. The concept of ACL reconstruction gained recognition as an effective surgical procedure, allowing it to occupy a spotlight position as the surgical gold standard till our current time [1, 6, 15].
However, renewed interest in preserving the native ACL was recently perceived in the field of sports traumatology, in an attempt to eliminate donor site morbidity and preserve maximum proprioceptive tissue [11, 13, 17]. One proposed technique named dynamic intraligamentary stabilization (DIS) was introduced in the year 2013, based on the theory that failure of earlier reported historic primary repair, was resultant to the rigid form of applied suture fixation, which based on recent findings, is expected to fail under cyclic loading during natural knee motion [12, 13]. Therefore, a dynamic form of fixation was proposed and developed [12]. Initial reports of the concept of DIS are promising, though these were all based on clinical assessment of ACL function [5, 7, 8, 13, 14]. Macroscopic assessment of the recovered ACL after this procedure was not performed.
The aim of this study was to objectify integrity and assess morphology of the ACL after DIS repair.
It was hypothesized that functional recovery of the ACL is resultant to scar tissue formation.
Materials and methods
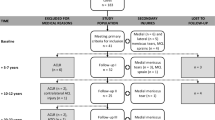
Patients presenting with an acute ACL rupture between March 2014 and April 2016 underwent DIS repair based on previously recommended indications (Fig. 1) [13, 14]:
-
Clinical and radiological confirmation of an ACL rupture.
-
Acute rupture within a 21-day post-injury time period.
-
Rupture location within the proximal third of the ACL.
-
Active patients with a pre-injury Tegner score of >4.
-
Age > 18 years.
Study inclusion criteria were:
-
Informed written consent.
-
Hardware removal and re-arthroscopy at a minimum of 6 months from the DIS repair procedure.
-
Follow-up of 12 months from the index procedure.
Patient demographics
The study group consisted of 47 knees in 47 patients. There were 27 male and 20 female patients with a mean age of 27.7 ± 9.0 years. Mean time from injury to surgery was 16.5 ± 6.5 days. ACL disruption patterns included: 17 single bundle, 27 double bundle, 2 triple bundle and 1 multilacerated (≥4 strands) injuries. Concomitant injuries were present in 22 patients: 13 sustained a lesion of one meniscus and 1 patient of both menisci, 2 presented a combined lesion of one meniscus and a chondral lesion of the femoral condyle, 3 sustained a medial collateral ligament (MCL) injury and 3 patients demonstrated combined injuries of the meniscus and MCL. All 6 lesions of the MCL were augmented during surgery, as previously described by Ateschrang et al. [2]. Meniscal lesions were either sutured or partially resected. The mean surgical time was 62 ± 16 min.
Surgical DIS technique—index procedure
All DIS repair procedures were performed by a single surgeon (AA), as previously described [13]. The Ligamys™ (Mathys Ltd Bettlach, Switzerland) fixation device was applied in all patients and tension chosen between 60 and 80 N (Fig. 2) [16].
Postoperative treatment
In the case of no concomitant injury, the knee was immobilized in full extension for 4 days after surgery. Active physiotherapy and controlled muscle strengthening exercise were begun at the fifth postoperative day with no restriction of range of motion (ROM). Cycling and jogging were permitted at 6 and 10 weeks, respectively. Return to sport was permitted 6 months after surgery.
Functional and clinical assessment
Knee function was evaluated at 6 weeks, 3-, 6- and 12 months postoperatively. Outcome assessment encompassed the following measures: Tegner-, Lysholm-, subjective International Knee Documentation Committee (IKDC) assessment scores, visual analogue scale for patient satisfaction (0 = completely dissatisfied, 10 = completely satisfied) and objective IKDC evaluation. Anterior laxity was measured using the KT-1000 arthrometer (MEDmetric, San Diego, CA, USA) at 30° of flexion and 30 lb (133 N) anterior force. The injured and the uninjured knee were both measured three times, and a mean difference was calculated (ap-translation).
Radiographic assessment
MRI was performed using a 1.5 T system (Achieva, Philips, Best, Netherlands) with a dedicated extremity knee coil (8 channel). The MRI sequences included a coronal T1-weighted spin echo, a coronal STIR, a sagittal intermediate-weighted fast-spin echo with fat suppression, an axial intermediate-weighted fast-spin echo with fat suppression and a sagittal 3D T1-weighted fast-field echo with water excitation (WATS). MRI investigations were conducted 3-, 6- and 12 months postoperatively. Evaluation included assessment of ACL reattachment, integrity and secondary meniscal or cartilaginous damage.
Arthroscopic evaluation and implant removal
Removal of the implant (Ligamys™) and arthroscopic evaluation of the joint were performed after having obtained written consent and in conjunction with either a clinical indication (n = 1, late-onset surgical site infection) or patient request (n = 46). The volume, consistency, tension-building ability and stability of the ACL were evaluated arthroscopically. The volume of the ACL was semi-quantitatively evaluated by one surgeon (AA) with respect to the percentage of its original volume: 100%, 75%, 50% or less than 25%. The consistency of the ACL was semi-quantitatively graded based on the extend of scar tissue formation: grade 0 = no scar tissue formation, grade 1 = small scar tissue formation (≤25% scare tissue of the original ACL), grade 2 = medium scar tissue formation (>25–75% scare tissue of the original ACL) and grade 3 = pronounced scarification of the ACL with only marginal ACL ligament structure (≥75% scar tissue of the original ACL). Scarification of the notch was also graded for demonstrative purposes (Fig. 3): grade 0 = no scarification, grade 1 = occupying one-third of the notch, grade 2 = occupying two-thirds of the notch and grade 3 = hypertrophic scarification of the entire notch.
The tibial bone defect after device removal was filled with an allogenic cancellous bone graft.
Definition of failure
Failure was defined as the presence of any of the following: (1) a side-to-side ap-translation of more than 5 mm [10] and (2) restoration of ≤50% of the native ACL volume upon arthroscopy.
This study was approved by the institutional review board of the Eberhard Karls University of Tübingen and was given the ID number 431/2013BO1.
Statistics analysis
Skewed data were presented as median (range). Normally distributed data were presented as mean ± standard deviation (minimum to maximum). Calculations were performed using JMP® (SAS Institute Inc., JMP®, Version 13.0.0, Cary, NC, USA).
Results
Functional and clinical assessment
Subjective outcome measures are illustrated in Table 1, demonstrating a continuous improvement of scores throughout the follow-up interval.
Objective outcome measures are illustrated in Table 2, showing clinical recovery of joint stability, as well as the expected loss of device tension with subsequent increase in ap-translation throughout follow-up.
Arthroscopic evaluation of ACL consistence and integrity
Results of the semi-quantitative arthroscopic grading are illustrated in Fig. 4. Full volume restoration of the ACL with little scar tissue formation and no scarification of the notch was present in >50% of patients. Intraoperative anterior stress testing demonstrated sufficient ACL tensioning in 93.6% (n = 44) of patients with 2.5 ± 1.2 mm (0–5 mm) ap-translation. Three patients showed an insufficient tension build-up as well as increased ap-translation during arthroscopy (Table 3).
Arthroscopic semi-quantitative morphological grading of the recovered ACL. The consistency of the ACL: grade 0 = no scar tissue, grade 1 = small scar tissue formation (≤25% scare tissue of the original ACL), grade 2 = medium scar tissue formation (>25–75% scare tissue of the original ACL), grade 3 = pronounced scarification of the ACL with only marginal ACL ligament structure (≥75% scar tissue of the original ACL). Scarification of the notch: grade 0 = no scarification of the notch, grade 1 = one-third, grade 2 = two-third and grade 3 = hypertrophic scarification of the entire notch. # Windshield wiper effect of the polyethylene cord acting as a healing obstacle
Secondary intra-articular findings upon re-arthroscopy included one fraying and one bucket handle tear of the posteromedial meniscal horn. The bucket handle tear was a concomitant primary injury, showing no signs of healing after primary meniscal repair.
The polyethylene cord was free of tension in all patients. Stability after implant removal was not compromised.
Radiographic assessment
MRI exams showed corresponding findings to arthroscopy regarding secondary joint injuries and ACL integrity, showing one new onset posteromedial meniscal fraying. The supplementary material provides MRI captions of the recovered ACL with corresponding arthroscopic images in a series of patients.
Failures and complications
No intraoperative complications were encountered. Postoperative complications included 1 hemarthrosis, 1 lung embolism, 1 late-onset infection, 1 traumatic re-rupture occurring 9 months after surgery during play, and 4 cases of insufficient ACL recovery. Two of the patients with insufficient ACL recovery were clinically detected upon 6-month follow-up (ap-translation > 5 mm) and 2 patients were only detected upon arthroscopic evaluation showing less than 50% restoration of ACL volume. Despite insufficient ACL recovery, all 4 patients reported high subjective knee functional scores as seen in Table 3.
Discussion
The most important finding of this study was that the clinical stability achieved after DIS repair of the ACL was associated with recovery of ligament integrity with various degrees of scarification.
The temporary function of the DIS fixation system has been noted in previous reports referring to the return of natural anterior posterior play after gradual loss of device tension [13]. This could be substantiated by results from this study, confirming macroscopic integrity of the ACL and proving that device removal does not compromise ACL function. The recovered tension-building ability of the ACL should compensate for the progressive loss of device function. Any case of non-healing would therefore gradually become apparent while loss of tension takes place. Therefore, it would be reasonable to assume that failures would be expected as the device loosens within the first 6 postoperative months.
A frequent finding abundant in one third of patients undergoing DIS repair is partial loss of ACL volume. This did not necessarily result in clinical instability. A likely explanation for this observation is the windshield wiper effect of the polyethylene cord, which could have acted as a healing obstacle, reducing the capacity of the ACL remnant to re attach to its femoral footprint (Fig. 4). A two-canal fixation method could address this issue in the future.
Intra-articular scar tissue formation in the notch region also represents a common finding, which may hypothetically be associated with the mandatory step of femoral footprint microfracturing during the DIS procedure. Based on the arthroscopic joint evaluation performed in this study, the degree of scar tissue formation in the notch could vary from minor to complete. Although scar tissue volume did not result in clinical symptoms in any of the patients in this series, previous studies demonstrated association with impingement and loss of the arc of motion, necessitating a second arthroscopic procedure for scar tissue reduction [9, 13].
Considering the results of this study and the increasing evidence from prior studies dealing with ACL preservation, excessive biology leads to hypertrophic scar formation, whereas lack of biology leads to failure of the procedure. This in terms underlines the significance of tissue engineering approaches that could guide the biological healing response. Primary promising reports of collagen membrane application alongside DIS repair have been recently published, demonstrating improvement of outcome [9]. Only a combined approach appreciating both biomechanics and biology would lead to higher success rates in ligament preserving surgery.
The limitations of this study include the semi-quantitative nature of the analysis, which despite allowing for comparison of qualitative data remains investigator dependent. A further limitation is the short follow-up, which does not influence the primary research question regarding ACL scarification and recovery, but would provide further valuable knowledge regarding secondary joint degeneration and stability in case of longer follow-up. Furthermore, it can be assumed that early arthroscopic evaluation involving reduction of visible hypertrophic scar tissue and screw removal could have both prevented complications and improved clinical results beyond the true effects of the primary index procedure.
Conclusion
The results of this study indicate that the clinical stability achieved with DIS repair of the ACL was associated with true recovery of the ligament integrity with various degrees of scar tissue formation. Removal of the device did not compromise ACL function. Further tissue engineering approaches to help guide the biological healing response.
Supplementary material
A sample of 16 intraoperative arthroscopic captures taken during the index procedure as well as during follow-up re-arthroscopy, with corresponding follow-up MRI scans, are available as supplementary material alongside the online version of this article. * A patient in which two-canal fixation method was applied, to prevent the windshield wiper effect of the polyethylene cord.
References
Ahmad SS, Meyer JC, Krismer AM, Ahmad SS, Evangelopoulos DS, Hoppe S et al (2017) Outcome measures in clinical ACL studies: an analysis of highly cited level I trials. Knee Surg Sports Traumatol Arthrosc 25(5):1517–1527
Ateschrang A, Döbele S, Freude T, Stöckle U, Schröter S, Kraus TM (2016) Acute MCL and ACL injuries: first results of minimal-invasive MCL ligament bracing with combined ACL single-bundle reconstruction. Arch Orthop Trauma Surg 136:1265–1272
Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE (2005) Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med 33:1751–1767
Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE (2005) Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med 33:1579–1602
Bierbaum M, Schoffski O, Schliemann B, Kosters C (2017) Cost-utility analysis of dynamic intraligamentary stabilization versus early reconstruction after rupture of the anterior cruciate ligament. Health Econ Rev 7(1):8
Drogset JO, Grontvedt T, Robak OR, Molster A, Viset AT, Engebretsen L (2006) A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am 88:944–952
Eggli S, Kohlhof H, Zumstein M, Henle P, Hartel M, Evangelopoulos DS et al (2015) Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. Knee Surg Sports Traumatol Arthrosc 23:1215–1221
Eggli S, Roder C, Perler G, Henle P (2016) Five year results of the first ten ACL patients treated with dynamic intraligamentary stabilisation. BMC Musculoskelet Disord 17:105
Evangelopoulos DS, Kohl S, Schwienbacher S, Gantenbein B, Exadaktylos A, Ahmad SS (2015) Collagen application reduces complication rates of mid-substance ACL tears treated with dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3838-7
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17:971–980
Kohl S, Evangelopoulos D, Kohlhof H, Hartel M, Bonel H, Henle P et al (2013) Anterior crucial ligament rupture: self-healing through dynamic intraligamentary stabilization technique. Knee Surg Sports Traumatol Arthrosc 21:599–605
Kohl S, Evangelopoulos D, Schär M, Bieri K, Müller T, Ahmad S (2016) Dynamic intraligamentary stabilisation. Bone Jt J 98:793–798
Krismer AM, Gousopoulos L, Kohl S, Ateschrang A, Kohlhof H, Ahmad SS (2017) Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilisation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-017-4445-6
Louboutin H, Debarge R, Richou J, Selmi TAS, Donell ST, Neyret P et al (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16:239–244
Schliemann B, Lenschow S, Domnick C, Herbort M, Häberli J, Schulze M et al (2017) Knee joint kinematics after dynamic intraligamentary stabilization: cadaveric study on a novel anterior cruciate ligament repair technique. Knee Surg Sports Traumatol Arthrosc 25(4):1184–1190
Steadman JR, Matheny LM, Briggs KK, Rodkey WG, Carreira DS (2012) Outcomes following healing response in older, active patients: a primary anterior cruciate ligament repair technique. J Knee Surg 25:255–260
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was received for the conduction of this study.
Ethical approval
The study was approved by the institutional ethical review board of the Eberhard Karls University of Tübingen in accordance to the Declaration of Helsinki and was given the ID number 431/2013BO1.
Informed consent
Informed consent was received by each study participant.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ateschrang, A., Ahmad, S.S., Stöckle, U. et al. Recovery of ACL function after dynamic intraligamentary stabilization is resultant to restoration of ACL integrity and scar tissue formation. Knee Surg Sports Traumatol Arthrosc 26, 589–595 (2018). https://doi.org/10.1007/s00167-017-4656-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4656-x