Abstract
Purpose
Because distance between the knee ACL femoral and tibial footprint centrums changes during knee range-of-motion, surgeons must understand the effect of ACL socket position on graft length, in order to avoid graft rupture which may occur when tensioning and fixation is performed at the incorrect knee flexion angle. The purpose of this study is to evaluate change in intra-articular length of a reconstructed ACL during knee range-of-motion comparing anatomic versus transtibial techniques.
Methods
After power analysis, seven matched pair cadaveric knees were tested. The ACL was debrided, and femoral and tibial footprint centrums for anatomic versus transtibial techniques were identified and marked. A suture anchor was placed at the femoral centrum and a custom, cannulated suture-centring device at the tibial centrum, and excursion of the suture, representing length change of an ACL graft during knee range-of-motion, was measured in millimeters and recorded using a digital transducer.
Results
Mean increase in length as the knee was ranged 120°–0° (full extension) was 4.5 mm (±2.0 mm) for transtibial versus 6.7 mm (±0.9 mm) for anatomic ACL technique. A significant difference in length change occurs during knee range-of-motion both within groups and between the two groups.
Conclusions
Change in length of the ACL intra-articular distance during knee range-of-motion is greater for anatomic socket position compared to transtibial position. Surgeons performing anatomic single-bundle ACL reconstruction may tension and fix grafts with the knee in full extension to minimize risk of graft stretch or rupture or knee capture during full extension. This technique may also result in knee anterior–posterior laxity in knee flexion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1995, Morgan et al. [9] published that anatomic ACL footprint positioning using endoscopic, transtibial technique should result in minimal graft elongation during knee range-of-motion, a nearly isometric state. However, while the goal of transtibial ACL was to minimize graft length change [1, 5, 6, 9, 11, 14, 15], anatomic ACL reconstruction is associated with graft length change during knee range-of-motion [4, 9]. Because there is a strong basis for anatomic ACL reconstruction [7], it is vital that surgeons understand the effect of ACL socket position on graft length, in order to avoid graft rupture which may occur when tensioning and fixation is performed at the incorrect knee flexion angle.
The purpose of this study is to evaluate change in length of the ACL single-bundle centrums intra-articular distance during knee range-of-motion comparing anatomic socket position versus transtibial.
The hypothesis is that anatomic ACL reconstruction has larger length change during range-of-motion, and distance between the femoral and tibial footprints increases during knee range-of-motion.
Materials and methods
Seven matched pairs of cadaveric knees (average age = 68 ± 5 years, six males, one female) were used for this testing. All knees had ACL present, and no history or examination signs of instability, previous arthrotomy, or ACL reconstruction. The native ACL was arthroscopically debrided, sparing fibers of the tibial stump as an anatomic reference.
Anatomic footprint technique
The anatomic centrums of the ACL femoral and tibial footprint were identified using arthroscopic rulers (Flipcutter guide, Arthrex, Inc., Naples, FL), and a radiofrequency device was used to mark the positions (OPES, Arthrex). First, the center of the femoral footprint was marked via the anteromedial arthroscopic portal at a position 43 % of the distance from the proximal cartilage border to the distal cartilage border, and 7.5 mm anterior to the posterior cartilage border on the lateral wall of the femoral intercondylar notch [12]. Then, the tibial centrum was marked 15 mm anterior to the PCL (adjusting for patient size by referencing the actual tibial ACL footprint stump appearance), and 40 % the interspinous distance from the medial to the lateral intercondylar eminence [2].
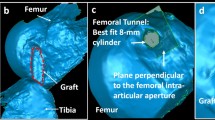
Transtibial footprint technique
The anatomic centrums of the ACL femoral and tibial footprint were identified using femoral and tibial aimers for endoscopic (transtibial, one-incision) ACL technique (Arthrex). First, the tibial aimer was used to centera 2.4-mm drill-tipped guide pin 7 mm anterior to the PCL [8]. After over-drilling using a 10-mm cannulated drill, a transtibial femoral guide (Arthrex) was used to center a beath pin 7 mm distal to the proximal cartilage border of the femoral lateral intercondylar notch wall at the 10:00 (right knee) or 2:00 clock-face position with the knee at 90° [3].
Experimental technique
The outcome measure is change in length of the ACL during knee range-of-motion while changing ACL femoral and tibial footprint centrums positions (anatomic vs. transtibial technique).
The technique involved a cadaveric knee model where a suture is attached to the femur in the positions for the techniques described above. For both techniques, the suture is attached to the femur with a 2.4-mm self-tapping, metal suture anchor (FasTak, Arthrex). To measure change in length of the ACL, on the tibia side, the suture is free to slide through a tibial interosseous tunnel, while the knee is brought through its range-of-motion. On the tibia side, the suture position is controlled using a centring device described below where the device positions the suture in the positions for the techniques described above. For both techniques, on the tibia, a custom (cut-off) tip of a 10-mm ACL tunnel dilator (Arthrex) was used as a suture-centring device to keep the sutures centred in the footprint after over-drilling with a 10-mm cannulated drill. The suture was held distally, under tension, using a 2-lb weight.
A Differential Variable Reluctance Transducer (DVRT; MicroStrain, Inc. Williston, VT) is an instrument that measures displacement of the head of a pin when connected to a signal processor, which in turn relays data to a laptop computer to be read by MicroStrain software at 10 Hz. The transducer was attached to the tibia with screws (Fig. 1). The head of the DVRT pin is placed through the tails of a suture (Fiberwire, Arthrex). When the knee moves through a range-of-motion, the suture moves, which moves the pin a variable distance that is equal to the change in length of the ACL during knee range-of-motion. In summary, during knee range-of-motion, the suture moves relative to the tibial tunnel (via the suture-centring device) and moves the head of the pin, and movement of the head of the pin is measured in millimetre using the DVRT (Figs. 1, 2).
Differential Variable Reluctance Transducer (DVRT; MicroStrain, Inc. Williston, VT) is an instrument that measures displacement of the head of a pin. The head of the pin is placed through the tails of a blue suture (Fiberwire, Arthrex), where suture excursion represents ACL graft length change in millimeters. The DVRT is screwed to the proximal, anteromedial tibia (left knee), just distal to the suture exit point from the tibia (top center)
Differential Variable Reluctance Transducer (silver, DVRT, MicroStrain, Inc. Williston, VT) is screwed to the proximal, anteromedial tibia (left knee), just distal to the suture exit point from the tibia. The tails of a blue suture (Fiberwire, Arthrex, where suture excursion represents ACL graft length change in millimetre) are affixed by the head of the DVRT pin (see Fig. 1), and the DVRT measures suture excursion in millimeters. Distally, the suture is held under tension using a 2-lb weight. Proximal to the DVRT, the suture passes through the proximal, anteromedial tibial metaphysis via a custom suture-centring device, which allows suture excursion (representing ACL graft length change in millimeters) during knee range-of-motion
The DVRT was positioned at 0 mm with the knee at 90° flexion using a bubble-meter goniometer as a guide (Arthrex). Next, change in length of the distance between the ACL femoral and tibial centrums during knee range-of-motion (anisometry) was measured at 15° increments, using the goniometer as a reference, as the knee was ranged through 120°. Figure 3 illustrates knee samples at 0°, 30°, 60°, and 120°. The clinically important outcome measure is maximum length change for each group, and the range-of-motion increment resulting in maximum length change is primarily analysed in the results.
Differential Variable Reluctance Transducer (silver, DVRT, MicroStrain, Inc. Williston, VT) is screwed to the proximal, anteromedial tibia (left knee), just distal to suture (blue, Fiberwire, Arthrex) tibial exit point. The DVRT measures suture excursion (representing ACL graft length change in millimeters) during knee range-of-motion. A bubble-meter goniometer (Arthrex) guides knee position for measurement from 0° through 120° at 15° increments. Knee samples at 0° (a), 30° (b), 60° (c), and 120 (d) are illustrated
Statistical analysis
Four cadaveric pairs were originally evaluated (pilot analysis details below) to determine the number of samples required. We determined that seven matched pairs (sample size) would result in power >0.8, assuming standard deviation of 1.5 mm and paired mean difference of 2.0 mm and α = 0.05 based upon pilot analysis of four matched pairs measured at 0 and 90 only, PASS 11 software (version 11.0.7, NCSS, LLC; Kaysville, UT). Data were analysed using OriginPro 8.0 software (OriginLab Corp., Northampton, MA). A two-way repeated-measures ANOVA (α = 0.05) was performed to compare differences in anisometry between anatomic and transtibial technique, and between the various flexion angles. The statistical analysis was performed using SigmaPlot 11.0 software (Systat Software, Inc.).
Results
The data are summarized in detail in Tables 1 and 2 and illustrated in Fig. 4. Both techniques result in significantly longer intra-articular distance in full extension versus any other position, and maximum increase in length occurs when the knee is extended from 90° to 0° knee flexion for both techniques.
Differential Variable Reluctance Transducer (DVRT) excursion in millimeters by knee flexion angle for anatomic versus transtibial techniques, where excursion represents change in length of ACL relative to the 90° position (zero point). The distance between the ACL femoral and tibial footprint centrums increases during knee extension, and maximum ACL graft length occurs at 0° (full extension) for both groups, and the difference between techniques is significant (Table 2) at 0°, 15°, 30°, and 45°. Graft stretch or graft rupture could occur if surgeons tension and fix ACL reconstruction grafts at >0° knee flexion using the femoral centrum and tibial footprint centrums positions investigated
Anatomic ACL results in significantly longer intra-articular distance in full extension (0°) versus 15°, 30°, 45°, 60°, 75°, 90°, 105°, and 120°, where p < 0.001 for each comparison. Mean maximum increase in length at 0° was 6.7 mm (±0.9 mm).
Transtibial ACL also results in significantly longer intra-articular distance in full extension (0°) versus 15°, 30°, 45°, 60°, 75°, 90°, 105°, and 120°, where p < 0.001 for each comparison. Mean maximum increase in length at 0° was 4.5 mm (±2.0 mm).
Comparing the two techniques, anatomic ACL results in significantly longer intra-articular distance compared to transtibial technique at full extension: 0° (p < 0.001), 15° (p < 0.001), 30° (p = 0.006), and 45° (p = 0.035).
Discussion
The results show that ACL graft length (the distance between the ACL femoral and tibial footprint centrums) increases significantly for both groups during knee extension, and the increase is significantly greater for anatomic ACL technique than for transtibial technique. Maximum length change occurs when the knee is extended from 90° to 0° knee flexion for both techniques. The results are similar to other recent literature reporting that the functional length of the ACL becomes longer in the extended position and shorter in the flexed position [5, 6, 11, 14, 15], and topical as surgeons make the transition from transtibial to anatomic technique [7].
The results may be clinically relevant because ACL graft length change of >4 % will result in irreversible graft stretch or graft failure [16], and considering ACL maximum intra-articular distance = 35 mm [13], a mean = 4.5 mm increase in graft length for transtibial technique, and a mean 6.7 mm increase in graft length for anatomic technique (Table 1), the results show length change of >4 % for all specimens in both groups when the knee is extended from 90° to 0° knee flexion (full extension).
A clinical conundrum is that ACL reconstruction graft fixation in 0° knee flexion (full extension) will result in knee laxity increase in flexion. Future research is required to determine whether cadaveric findings correlate in actual surgical patients. In the experience of the author, the ACL laxity during flexion is better tolerated by patients than irreversible graft stretch and graft rupture or extension loss after ACL reconstructive surgery.
Study limitations include knee joint motion in vivo is controlled by muscle forces that are not present using our model. This may result in forces on the ACL graft that do not represent in vivo forces. Vertical position has been reported to result in less change in graft length during knee range-of-motion than the transtibial position tested [10, 15]. The data are specific to the footprint centrum positions described in the methods. In addition, other methods for measuring cadaveric knee range-of-motion may be more precise than goniometer. Finally, hyperextension requires future evaluation.
The results are clinically relevant because to prevent graft stretch or graft rupture or knee capture during full extension, surgeons performing anatomic or transtibial single-bundle ACL reconstruction could tension and fix ACL reconstruction grafts in 0° knee flexion (full extension). This is of significantly greater importance for anatomic technique.
Conclusion
Change in length of the ACL intra-articular distance during knee range-of-motion is greater for anatomic socket position compared to transtibial position.
References
Giron F, Cuomo P, Aglietti P, Bull AM, Amis AA (2006) Femoral attachment of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14:250–256
Hwang MD, Piefer JW, Lubowitz JH (2012) Anterior cruciate ligament tibial footprint anatomy: systematic review of the 21st century literature. Arthroscopy 28:728–734
Howell SM (1998) Principles for placing the tibial tunnel and avoiding roof impingement during reconstruction of a torn anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 6(Suppl 1):S49–S55
Iriuchishima T, Shirakura K, Fu F (2013) Graft impingement in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21:664–670
Iwahashi T, Shino K, Nakata K et al (2008) Assessment of the “functional length” of the three bundles of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 16:167–174
Li G, DeFrate LE, Sun H, Gill TJ (2004) In vivo elongation of the anterior cruciate ligament and posterior cruciate ligament during knee flexion. Am J Sports Med 32:1415–1420
Lubowitz J, Poehling G (2009) Watch your footprint: anatomic ACL reconstruction. Arthroscopy 25:1059–1060
Morgan CD, Kalman VR, Grawl DM (1995) Definitive landmarks for reproducible tibial tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy 11:275–288
Morgan CD, Kalmam VR, Grawl DM (1995) Isometry testing for anterior cruciate ligament reconstruction revisited. Arthroscopy 11:647–659
Musahl V, Plakseychuk A, VanScyoc A, Sasaki T, Debski R, McMahon P, Fu F (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med 33:712–718
Pearle AD, Shannon FJ, Granchi C, Wickiewicz TL, Warren RF (2008) Comparison of 3-dimensional obliquity and anisometric characteristics of anterior cruciate ligament graft positions using surgical navigation. Am J Sports Med 36:1534–1541
Piefer J, Pflugner T, Hwang M, Lubowitz J (2012) Anterior cruciate ligament femoral footprint anatomy: systematic review of the 21st century literature. Arthroscopy 28:872–881
Samuelsson K (2012) Anatomic anterior cruciate ligament reconstruction. Current evidence and future directions. The Sahlgrenska Academy, University of Gothenberg Press 1:19. ISBN: 978-91-628-8422-2
Wang J, Kato Y, Ingham S, Maeyama A, Linde-Rosen M, Smolinski P, Fu F (2012) Measurement of the end-to-end distances between the femoral and tibial insertion sites of the anterior cruciate ligament during knee flexion and with rotational torque. Arthroscopy 28:1524–1532
Yoo YS, Jeong WS, Shetty NS, Ingham SJ, Smolinski P, Fu F (2010) Changes in ACL length at different knee flexion angles: an in vivo biomechanical study. Knee Surg Sports Traumatol Arthrosc 18:292–297
Zavras T, Race A, Bull A, Amis A (2001) A comparative study of “isometric” points for anterior cruciate ligament graft attachment. Knee Surg Sports Traumatol Arthrosc 9:28–33
Acknowledgments
John Konicek, BS, is a bioengineer in Arthrex, Inc., Naples, FL.
Conflict of interest
James H. Lubowitz receives consulting and royalties from Arthrex. James H. Lubowitz Item 1. Board member/owner/officer/committee appointments: Committee member: AANA, AOSSM, ISAKOS, Item 2. Royalties: Arthrex, Item 3. Speakers bureau/paid presentations: N/A, Item 4A. Paid consultant or employee: AANA, Arthrex, Item 4B. Unpaid consultant: N/A, Item 5. Research or institutional support from publishers: N/A, Item 6. Research or institutional support from companies or suppliers (data generated from such studies must be unrestricted): Arthrex, Breg, Donjoy, S+N, Item 7. Stock or stock options: Ivivi.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubowitz, J.H. Anatomic ACL reconstruction produces greater graft length change during knee range-of-motion than transtibial technique. Knee Surg Sports Traumatol Arthrosc 22, 1190–1195 (2014). https://doi.org/10.1007/s00167-013-2694-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2694-6