Abstract
Purpose
A comparison of clinical outcomes between double-bundle (DB) and single-bundle (SB) anterior cruciate ligament (ACL) reconstruction for patients with ACL injury.
Methods
Sixty patients were treated with either SB (n = 30) or DB (n = 30) ACL reconstruction between 2011 and 2012. The hamstring tendons were autografted with suspensory fixation on the femoral side, while a bio-absorbable interference screw was used for fixation on the tibial side. These patients were evaluated using Lysholm score, International Knee Documentation Committee (IKDC) forms (both objective and subjective), Lachman test, pivot shift test, and KT 1000 arthrometer.
Results
After a median follow-up duration of 35.5 months (ranging between 30 and 42 months), the frequency of patients who had high objective IKDC scores was significantly higher in the DB group than those in the SB group. In terms of DB, the Lachman test was normal in 26 patients (86.7%), nearly normal in three patients (10%), and abnormal in one patient (3.3%); comparatively, in terms of SB, the Lachman test was normal in 20 patients (66.7%), nearly normal in eight patients (26.7%) and abnormal in two patients (6.6%). The pivot shift test was negative in 29 patients (96.7%) and 21 patients (70%) for DB and SB, respectively. The average KT-1000 side-to-side difference was 1.0 mm for DB and 1.5 mm for SB. The subjective IKDC and Lysholm score showed non-significant differences between both techniques.
Conclusion
Double-bundle ACL reconstruction was found to have a significant advantage in anterior and rotational stability as well as objective IKDC than that of SB reconstruction. However, subjective measurements showed no statistical differences between the techniques.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injury is one of the most common knee sports injuries, which may result in recurrent knee instability, meniscal tears, and articular cartilage degeneration [5]. Currently, the most common treatment strategy for the injured ACL is either single-bundle (SB) or double-bundle (DB) ACL reconstruction [30]: both treatments are effective in virtually restoring native joint anatomy and kinematics [32].
The ACL is a double-bundled ligament containing the anteromedial (AM) bundle and the posterolateral (PL) bundle, which together provide anterior and rotational stability of the knee [20]. Arthroscopic SB technique was performed by creating one single femoral tunnel and one single tibial tunnel [34]. Such a technique may have good clinical outcomes to the extent that it restores anterior stability following an ACL injury [23], yet it is, perhaps, suboptimal for rotational function.
Biomechanical studies have revealed that DB reconstruction restores both the AM and PL bundles, and thus results in closer to normal anterior and rotational stability than does conventional SB, which restores the ACL as only one bundle [9].
The reconstruction of PL bundle has significantly increased rotational laxity when compared with SB ACL reconstruction [11]. Anatomical and biomechanical studies have also given support to the operative anatomical DB concept. This DB concept is perhaps attributed to the recreation of the native footprint and restoration of biomechanical functions [2]. Such anatomical and biomechanical considerations have triggered an interest in the clinical application of more anatomical reconstruction techniques [33].
The technique of replicating the complex anatomy of the ACL in DB was first described by Mott [22] in 1983 and Müller [23] in 1982, and many technical variations of the procedure were added thereafter [1, 28, 29].
A considerable number of prospective comparative clinical studies with either level I or II evidence have reported superior results of anatomical DB reconstruction than those of SB [12, 16, 28, 29, 34]. However, there are some studies that report no differences between SB and DB ACL reconstruction [20].
The current study hypothesized that a four-tunnel DB ACL reconstruction might be advantageous in restoring anterior and rotational laxity; furthermore, objective clinical results were superior in DB than those of SB ACL reconstruction surgery.
Materials and methods
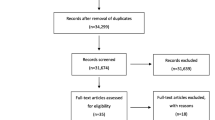
The study involved patients who have had complete ACL rupture with closed growth plates and were admitted by our institute from 2011 to 2012. The patients were divided into two groups according to the surgical procedure: the single-bundle (SB) group (n = 45) and the double-bundle (DB) group (n = 40). The patients who suffered from multi-ligamentous injuries, severe arthritic changes, total or subtotal meniscectomy, revisional ACL reconstruction, contralateral ACL-deficient knee, or a partial ACL rupture were excluded. Furthermore, patients with intraoperative findings other than complete ACL rupture and those who have failed to maintain contact during the follow-up were excluded from the study. A total of 60 patients (70.6%) met the inclusion criteria (30 patients per group). The remaining 25 patients (29.4%) did not meet the inclusion criteria and were excluded from the study. Causes for exclusion included need for revision of ACL reconstruction (n = 4), presence of contralateral ACL injury and reconstruction (n = 5), subtotal meniscectomy (n = 2), severe arthritic changes (n = 2), intraoperative diagnosis of partial ACL injury (n = 6) and patient’s absence during follow-up (n = 6).
Preoperative data of the 60 patients are demonstrated in Table 1. On the day of the surgery, patients were randomly assigned to one of the two groups.
Operative techniques
Double-bundle reconstruction
Double-stranded hamstring autograft was used for DB reconstruction through the application of Pascal et al.’s four-tunnel technique [26] with slight modifications while performing femoral tunnels. These modifications were a contribution of the current study: for the anteromedial tunnel, the passing pin was placed in the center of the AM insertion site, posteriorly to the bifurcate ridge and inferiorly to the lateral intercondylar ridge, and drilled to perforate the lateral cortex of the femur during knee flexion at approximately 120°. For the posterolateral tunnel, a specific posterolateral femoral drill guide was introduced via the accessory medial portal in the AM tunnel; the PL tunnel was drilled with a cannulated drill bit, which was placed inferiorly to the lateral intercondylar ridge and anteriorly to the bifurcate ridge. On the tibial side, the AM bundle was fixed in between 45° and 60° knee flexion and the PL bundle was fixed in between 0° and 15° knee flexion, both utilizing a bio-absorbable interference screw that is larger than their respective tunnels by 1 mm.
Single-bundle reconstruction
Similar to DB reconstruction, a femoral tunnel was performed below the lateral intercondylar ridge and at the lateral bifurcate ridge; then, tibial tunnels were performed. An ACL tibial aimer was placed in the center of the ACL tibial insertion site, based on anatomical landmarks between the AM and PL insertion sites. The position of the aimer on the tibial cortex was 3 cm medial to the tibial tubercle. The graft was then passed through both the tibial and femoral tunnels; then, the endobutton was flipped in standard fashion for femoral fixation and a bio-absorbable interference screw (one that is larger than the tunnel by 1 mm) was used for tibial fixation.
During patient follow-ups, one of the authors, who was not aware of the randomization and procedure, was responsible for subjective and objective assessment; additionally, at the time of the patient’s most recent visit, anteroposterior and lateral views were taken for assessment.
Ethical approval was obtained from the Institutional Review Board (IRB) from Al-Azhar University: No. 429.
Statistical analysis
Data collected was analyzed descriptively and inferentially using the SPSS program (Statistical Package of Social Science; SPSS Inc., Chicago, IL, USA) version 16 for Microsoft Windows. In effect, mean and median scores were calculated to measure the central tendency of parametric and non-parametric data, respectively. A comparison of groups was done using Mann–Whitney U test to determine the significance in difference between two medians and Chi-square test (χ2) for comparison of qualitative data. The level of significance was taken at p value of < 0.05. The results are represented in the tables. During the predetermined period of the study, all those who met the inclusion and exclusion criteria and agreed to participate were included in the study. Also, post hoc power analysis was done with 0.81 statistical power.
Results
Intraoperative findings as outlined in Table 2 revealed no significant (n.s.) differences between the groups. At end of the follow-up, the negative pivot shift test and normal Lachman test were significantly higher (p < 0.05) in patients who had DB than those who had SB. Average KT-1000 side-to-side difference in an anterior tibial displacement was significantly less (p < 0.05) in DB than in SB groups [1.0 (± 0.74) vs. 1.5 (± 1.92) mm, respectively]. The outcome of objective IKDC 2000 evaluation showed a significant difference (p < 0.05) in favor of DB reconstruction, while subjective IKDC 2000 evaluation and Lysholm score did not show any difference (n.s.) (Table 3). Postoperative complications were encountered in three patients (5%); one patient developed moderate effusion that required aspiration and application of cold fomentation, and the other two patients suffered donor site superficial wound infections relieved by intensive antibiotic therapy and daily dressings 2 days for the former and 3 days for the latter.
Discussion
The most important finding of the present study is the significantly less anteroposterior translation (APT) as measured by the KT-1000 with significant improvement of rotational stability according to the pivot shift test in patients who had DB than in those who had SB.
The results verified the hypothesis of the study and indicated that DB is clinically advantageous when compared with SB. ACL injury represents one of the most common diagnoses in orthopedic sports medicine [18] and its reconstruction is one of the most commonly performed orthopedic surgeries [19] to restore the function of the native ACL [27]. For ACLR using the semitendinosus and gracilis tendons, endobuttons were used for femoral fixation and a bio-absorbable interference screw for tibial fixation. The rationale for the study concerning the hypothesis and mode of graft fixation coincided with multiple recent studies [3, 4, 13, 17].
The results of this study go in line with the results obtained by Komzák et al. [16] who reported that the ADB technique results in better knee stability in both APT and rotation than that of the central ASB technique. By the same token, Zhang et al. [35] underscored that postoperative (PO) knee stability and joint functions were better after ADB or ASB with anterolateral ligament reconstruction than after ASB reconstruction alone. More recently, Mutsuzaki et al. [25] experimentally verified that, 6 months postoperatively, the in situ forces under anterior tibial load (ATL) and internal tibial torque (ITT) in the DB group were greater than those of SB group.
The reported anterior laxity is perhaps attributed to the additional reconstruction of the PL bundle. In support of such an assumption, Komzák et al. [15] highlighted increased knee stability in APT and internal/external rotation when PL bundle is added to DB reconstruction.
The results of the current study showed significantly better objective IKDC results with DB than with SB, and this could be influenced by the laxity of both groups. However, there were no significant differences in the subjective results and failure rates. In a similar study performed at a follow-up average of 35 months, Devgan et al. [6] detected no statistically significant difference concerning knee laxity, knee scores, subjective evaluations, and MRI evaluation of graft inclination angles between SB- and DB-ACL reconstruction. Similarly, Torkaman et al. [32] found that the average side-to-side differences using KT-1000 showed no significant differences between SB and DB groups and Lysholm score improved significantly in both groups, but there was no significant difference between groups. In line with the reported non-significant different subjective outcome, Koga et al. [14] reported during the 2-year follow-up: in DB ACL reconstruction, when the anteromedial bundle was fixed at 20° flexion, fixation of the posterolateral bundle (PLB) at 45° was worse than fixation at 0° and 20° regarding anterior and rotational laxity; however, there were no significant differences in range of motion or other subjective parameters. Tian et al. [31] found no significant differences in postoperative activity levels and functional outcomes of arthroscopic anatomical DB ACLR using a hamstring tendon autograft versus irradiated allograft. Moreover, over a 7-year follow-up, Liu et al. [17] reported that both SB and DB ACL reconstruction using 6- to 8-stranded hamstring autograft showed satisfactory results in subjective scores and anteroposterior and rotational stability with no significant differences between groups in functional scores.
The present study reported significant improvement of rotational stability as judged by negative pivot shift test: 96.7% of DB patients and 70% of SB patients. Such figures for negative pivot shift test are in line with Devgan et al. [6, 7] who pointed out negative pivot shift test results in 100% of patients who had DB [10, 11] and 93.3% of patients who had SB [11]. Similarly, Morey et al. [21] found graded stability as judged by the results of the Lachman, anterior drawer, and pivot shift tests in patients who underwent DB ACR was almost near to that in normal knee. Figueroa et al. [10] found anatomical outside-in SB ACL reconstruction using a retrodrill results in negative pivot shift test in 90% of patients. The current study coincided with Devgan et al. [7] in attributing the reported knee laxity to PL reconstruction and the high rate of negative pivot shift test to the four-tunnel technique, which utilizes the whole area of the footprint of the reconstruction.
Throughout the 36-month follow-up, no patient in either group required revision surgery; similarly, during a mean follow-up of 4.2 years, Dugas et al. [8] documented that among the 42 baseball players who underwent ACL reconstruction none required revision ACL surgery.
The clinical relevance of this study lies in the fact that four-tunnel DB ACL reconstruction provides anteroposterior laxity (as measured by KT 1000) and rotational laxity (as measured by the pivot shift test) than those who had SB. Based on the present results, this study can be useful in daily clinical practice. Dealing with athletes such as football players, judo practitioners and wrestlers, a clear proposal of DB ACL reconstruction is recommended.
The current study has a number of limitations which need to be addressed by future research. One of these limitations, which is the cornerstone of anatomical ACL reconstruction, is the concept of individualizing the procedure to suit the patient’s activity levels, expectations, and knee anatomy. However this is contradictory to the rationale of blinded randomization. The current study illustrate the experience of single center; however, multi-center comparative studies are mandatory to establish the outcomes. Also, comparisons with the outcome of other procedures could help establish the clinical utility of the anatomical double-bundle ACL reconstruction.
Conclusion
Four-tunnel DB ACL reconstruction was found to have significant advantages in anterior and rotational laxity as well as objective IKDC when compared to SB ACL reconstruction. However, no statistical differences were found between the subjective scorings after both technique.
References
Ahn JH, Lee SH (2007) Anterior cruciate ligament double-bundle reconstruction with hamstring tendon autografts. Arthroscopy; 23:109.e1–109.e4
Buoncristiani AM, Tjoumakaris PF, Starman JS, Ferretti BSM, Fu FH. (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy; 22:1000–1006
Browning WM 3rd, Kluczynski MA, Curatolo C, Marzo JM (2017) Suspensory versus aperture fixation of a quadrupled hamstring tendon autograft in anterior cruciate ligament reconstruction. Am J Sports Med. https://doi.org/10.1177/0363546516680995
Debieux P, Franciozi CE, Lenza M, Tamaoki MJ, Magnussen RA, Faloppa F, Belloti JC. (2016) Bioabsorbable versus metallic interference screws for graft fixation in anterior cruciate ligament reconstruction. Cochrane Database Syst Rev 7:CD009772
Desai N, Bjornsson H, Musahl V, Bhandari M, Petzold M, Fu FH, Samuelsson K (2014) Anatomic single- versus double-bundle acl reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22:1009–1023
Devgan A, Rohilla R, Singh A, Tanwar M, Devgan R, Siwach K (2016) A prospective study to evaluate the clinico-radiological outcomes of arthroscopic single bundle versus double bundle anterior cruciate ligament reconstruction. J Clin Orthop Trauma 7(Suppl 2):236–242
Devgan A, Singh A, Gogna P, Singla R, Magu NK, Mukhopadhyay R (2015) Arthroscopic anatomical double bundle anterior cruciate ligament reconstruction: a prospective longitudinal study. Indian J Orthop 49(2):136–142
Dugas JR, Bedford BB, Andrachuk JS, Scillia AJ, Aune KT, Cain EL, Andrews JR, Fleisig GS (2016) Anterior cruciate ligament injuries. Baseb Play Arthrosc 32(11):2278–2284
Edwards A, Bull AM, Amis AA (2008) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament, part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc 16:29–36
Figueroa D, Calvo R, Figueroa F, Paccot D, Izquierdo G, Morales N (2016) Clinical and arthrometric outcomes of an anatomic outside-in single-bundle anterior cruciate ligament reconstruction using a retrodrill. Knee 23(6):1098–1105
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22:85–89
Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring graft compared with procedures. J Bone Joint Surg Br 91(10):1310–1315
Karikis I, Desai N, Sernert N, Rostgard-Christensen L, Kartus J (2016) Comparison of anatomic double- and single-bundle techniques for anterior cruciate ligament reconstruction using hamstring tendon autografts: a prospective randomized study with 5-year clinical and radiographic follow-up. Am J Sports Med 44(5):1225–1236
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M, Nakamura T, Otabe K, Sekiya I (2015) Effect of posterolateral bundle graft fixation angles on clinical outcomes in double-bundle anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med 43(5):1157–1164
Komzák M, Hart R, Smíd P, Puskeiler M (2014) The effect of central anatomical single-bundle versus anatomical double-bundle reconstruction of the anterior cruciate ligament on knee stability. A clinical study. Acta Chir Orthop Traumatol Cech 81(4):276–280
Kopf S, Pombo MW, Szczodry M, Irrgang JJ, Fu FH (2011) Size variability of the human anterior cruciate ligament insertion sites. Am J Sports Med 39:108–113
Liu Y, Cui G, Yan H, Yang Y, Ao Y (2016) Comparison between single- and double-bundle anterior cruciate ligament reconstruction with 6- to 8-stranded hamstring autograft: a prospective, randomized clinical trial. Am J Sports Med 44(9):2314–2322
Lorenz S, Ahrens P, Kirchhoff S, Wolf P, Hinterwimmer S, Obermeier A, Beirer M, Kirchhoff C (2015) Dynamic quantification of tibio-femoral rotation in postero-lateral bundle insufficiency of the anterior cruciate ligament: a cadaver study. Int Orthop 39(5):865–870
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr, Paletta GA Jr (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42(10):2363–2370
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421
Morey VM, Nag HL, Chowdhury B, Pannu CD, Meena S, Kumar K, Palaniswamy A (2016) Arthroscopic anatomic double bundle anterior cruciate ligament reconstruction: our experience with follow-up of 4 years. J Clin Orthop Trauma 7(1):17–22
Mott W (1983) Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop Relat Res 172:90–92
Müller W (1982) Das Knie. Form, Funktion Und Ligamentäre Wiederherstellungschirurgie. Springer, New York
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double bundle techniques. Arthroscopy 23:618–628
Mutsuzaki H, Fujie H, Nakajima H, Fukagawa M, Nomura S, Sakane M (2017) Comparison of postoperative biomechanical function between anatomic double-bundle and single-bundle ACL reconstructions using calcium phosphate-hybridized tendon grafts in goats. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.ostr.2016.11.013
Pascal C, Franceschi JP, Sbihi A, Colombet P, Djian P, Belier G (2005) Anatomic anterior cruciate ligament reconstruction: the French experience. Oper Tech Orthop 15:103–110
Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu FH (2016) Anatomical individualized ACL reconstruction. Arch Bone Joint Surg 4:291–297
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16:232–238
Sun R, Chen BC, Wang F, Wang XF, Chen JQ (2015) Prospective randomized comparison of knee stability and joint degeneration for double-and single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 23:1171–1178
Tian S, Wang B, Liu L, Wang Y, Ha C, Li Q, Yang X, Sun K (2016) Irradiated hamstring tendon allograft versus autograft for anatomic double-bundle anterior cruciate ligament reconstruction: midterm clinical outcomes. Am J Sports Med 44(10):2579–2588
Torkaman A, Yazdi H, Hosseini MG (2016) The results of single bundle versus double bundle ACL reconstruction surgery, a retrospective study and review of literature. Med Arch 70(5):351–353
Van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Xu M, Gao S, Zeng C, Han R, Sun J, Li H, Xiong Y, Lei G (2013) Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy 29:357–365
Zhang H, Qiu M, Zhou A, Zhang J, Jiang D (2016) Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med 15(4):688–696
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Ethical approval
Ethical approval was obtained from the Institutional Review Board (IRB) from Al-Azhar University: No.429 and agreement.
Informed consent
Patients were informed, and they consented to conduct the study. All the patients agreement to conduct the study.
Rights and permissions
About this article
Cite this article
El-Sherief, F.A.H., Aldahshan, W.A., Wahd, Y.E. et al. Double-bundle anterior cruciate ligament reconstruction is better than single-bundle reconstruction in terms of objective assessment but not in terms of subjective score. Knee Surg Sports Traumatol Arthrosc 26, 2395–2400 (2018). https://doi.org/10.1007/s00167-017-4804-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4804-3