Abstract
The objective of this article is to describe the clinical outcome of the transitional double-bundle procedure for anatomical ACL reconstruction. Subjects included 78 patients (average age 25 years) who had undergone ACL reconstruction with the transitional double-bundle procedure with multi-stranded hamstring tendons. The femoral socket for the anteromedial (AM) graft was created at 5–6 mm from the mid-sagittal line of the intercondylar notch at 2:00 or 10:00, and that for the posterolateral (PL) graft was drilled adjacent to the AM socket at 3:00 or 9:00. For the tibial side, two tunnels were made at the center of the footprint of the AM and PL bundles of the normal ACL. Patients were evaluated at 24 months or longer postoperatively based on the IKDC Knee Examination Form. Subjectively, 32 knees (41%) were graded as normal; 41 (53%), as nearly normal; 4 (5%), as abnormal; and 1 (1%) as graft rupture by re-injury. The average side-to-side difference in anterior laxity at manual maximum force with the KT-2000 arthrometer was 0.9 mm ± 1.2. Seventy patients (93%) had a range between −1 mm and 2 mm. In conclusion the transitional double-bundle ACL reconstruction provided a satisfactory outcome after a short-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Double-bundle anterior cruciate ligament (ACL) reconstructions with multi-stranded hamstring tendons have been performed recently based on the obtained biomechanical data from newly-developed robotic technology [7, 13–16, 29] aiming at better clinical results than those after the single-bundle procedures [1, 4, 5, 9, 11, 12, 17–19, 21, 26, 27, 30–32]. However, there has been concern that these procedures may lead to a larger graft-length change during the range of knee motion, thus leading to compromised graft healing or excessive stretch during postoperative rehabilitation [8, 20]. Thus, we have been trying to perform a step-by-step transition of procedures leading up to our use of the anatomical double-bundle reconstruction to safely achieve clinical success of ACL reconstruction (Fig. 1). First, we used the bi-socket procedure with two femoral sockets near the high noon position and one tibial tunnel (high socket-one tunnel procedure; HS-1T procedure) [9, 21, 28]. Next, we changed the femoral socket location created at a position lower to the near high noon location (low socket-one tunnel procedure; LS-1T procedure) [28]. Then, we made two tunnels in the tibial side, beginning the transitional procedure (low socket-two tunnel procedure; LS-2T procedure) to the anatomical double-bundle reconstruction described in this study. Finally, we have recently achieved the anatomical double/triple bundle ACL reconstruction in which the graft mimics normal orientation of the native ACL bundles by creating tunnels within the femoral and tibial anatomical footprints [23, 25].
Transition of the ACL reconstruction in our hospital (left knee). a High socket-one tunnel procedure (HS-1T procedure), b low socket-one tunnel procedure (LS-1T procedure), c low socket-two tunnel procedure (LS-2T procedure), d anatomical double-bundle procedure. AMS the socket for the anteromedial graft, PLS the socket for the posterolateral graft, AMT the tunnel for the anteromedial graft, PLS the tunnel for the posterolateral graft. The arrow shows the top of the intercondylar notch and each black oval express each location of femoral socket or tibial tunnel
Previously, we discussed the effect of femoral socket location by comparison of the HS-1T and the LS-1T procedures, and reported that the latter was more favorable with regard to subjective results without complications [28]. In this study, we focused on the LS-2T procedure. We could then elucidate the effect of two tibial tunnels by comparing the LS-2T procedure with the outcome of the LS-1T procedure, which had the same femoral socket location with one tibial tunnel. Thus, the purpose of this study was to describe the short-term clinical outcome of this LS-2T procedure.
Patients and methods
Inclusion criteria
Inclusion criteria in this study were as follows: (1) no prior intra- or extra-articular ligament reconstruction, (2) absence of posterior drawer sign, abnormal varus/valgus laxity, excessive external tibial rotation compared with the contralateral normal knee, (3) a healthy contralateral knee as determined by the patient’s history and physical examination, (4) no severe osteoarthritic changes (more than 50% of joint space narrowing in any compartment detected by radiography), (5) no acute cases of patients who sustained their injury within 3 weeks (those who did visit our hospital during the acute phase underwent rehabilitation to regain a normal range of motion) and (6) the grafts were composed either of two double-looped semitendinosus (ST) tendons, or of one double-looped ST and one double-looped gracilis (Gr) tendons.
Patients
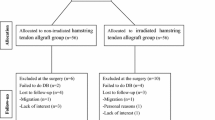
Of the 128 patients with chronic ACL insufficiency who received the double-bundle ACL reconstruction by the LS-2T procedure with between July 2003 and March 2005 in Kansai Rosai Hospital, 119 patients met the criteria for inclusion in the study. Among these patients, 78 patients were available for direct follow-up at more than 24 months after the operation while 41 patients were lost to follow-up (follow-up rate 66%). The patients included 37 females and 41 males (46 right, 32 left) with an average age of 25 years ± 10 (range 13–49). According to activity level defined by the IKDC Knee Ligament Evaluation Form 1999, they were classified as follows: 56 patients (72%), level I; 15 (19%), level II; 1 (1%), level III; and 6 (8%), level IV. The average follow-up period was 27 months with a range from 24 to 55 months (Table 1).
Operative procedure
ACL reconstruction was arthroscopically performed by a single surgeon (YT) using the drill hole technique with the Protrac/Director tibial guide® (Smith & Nephew Endoscopy, Andover, MA, USA) and Endobutton® (Smith & Nephew Endoscopy) femoral fixation.
Femoral sockets
Two 2.4-mm guide-wires were inserted to the ACL femoral attachment through the additional portal (“far antero-medial portal”) 2–2.5 cm posterior to the anteromedial portal [23]. The anteromedial (AM) socket was created 5–6 mm down from the mid-sagittal line of the intercondylar notch adjacent to the posterior edge of the intercondylar notch. The posterolateral (PL) socket was drilled just adjacent to the AM socket, also just anterior to the posterior edge of the intercondylar notch (Fig. 1). We arthroscopically identified the superior border of the medial margin of the articular cartilage of the lateral femoral condyle, and created the AM and PL sockets just above or below the border, respectively (Fig. 2). When the conventional clock expression was used, which was popular to express the socket locations at that period, the AM socket was located at 2:00 or 10:00 and the PL socket was at 3:00 or 9:00 [28]. These sockets were created using a 4.5- to 7-mm-diameter cannulated reamer according to the diameter of the AM graft and the PL graft. Notchplasty was not performed in any of the cases.
Tibial tunnels
Two 2.4-mm guide-wires were inserted into the center of the tibial attachment sites of both the AM and the PL bundles of the ACL from the anteromedial aspect of the tibia using the Director Drill Guide System® (Smith & Nephew Endoscopy) (Fig. 1). The guide wires were over-drilled using a 4.5- to 7-mm-diameter cannulated reamer according to the diameter of the grafts. As great care was taken to keep the two tunnels inside the native ACL stump, the bone bridge between them was not always preserved in this series.
Graft preparation
When the ST tendon was 24 cm or longer, it was transversely cut in two and each portion was folded over. When the ST tendon was less than 24 cm, the Gr tendon was also harvested. The ST tendon was folded over to make a thicker AM graft and the Gr tendon was folded over to create a thinner PL graft. Endobutton CL® (Smith & Nephew Endoscopy) was used for each loop end on the femoral side and two No. 3 polyester braided sutures were sewn on to each free end at the tibial side of the folded grafts by Krackow suture.
Graft fixation
The grafts were passed from the tibial tunnel to the femoral sockets and fixed with Endobuttons®. Grafts were inserted more than 13 mm of their length into both the femoral sockets and the tibial tunnels to facilitate sufficient bone-tendon healing. The tibial sides of the two grafts were fixed at 20 degrees of knee flexion with Double Spike Plates® (Smith & Nephew Endoscopy) with 30 N in each graft using the ligament tensioners® (Smith & Nephew Endoscopy) (Table 1) [24].
Associated meniscal surgeries
Regarding the intra-articular pathology for all subjects, 50 (64%) cases had associated injuries to the medial meniscus (MM) and 27 (35%) to the lateral meniscus (LM). The treatments for these lesions as well the articular cartilage lesions in each compartment based on Outerbridge’s classification are summarized in Table 1.
Postoperative regimen
The knee was immobilized for a week with a brace followed by CPM exercise. Active and assisted ROM exercise was started at 2 weeks. Partial weight bearing was allowed at 3 weeks and full weight bearing was started at 5 weeks. Running was allowed at 4 months followed by return to previous sports activity at 9–12 months.
Evaluation
All of these patients were evaluated qualitatively and quantitatively using the IKDC Knee Examination Form 1999 in addition to assessment of isokinetic thigh muscle strength. In the subjective assessment, patients who graded their knees as “nearly normal” or “abnormal” were asked the reason for their response. Answers were categorized as follows: unstable knee, severe pain, mild pain, occasional slight pain, muscle weakness, difficulty in Japanese sitting style, feeling different than the normal side and anxiety over re-injury. Objectively, Lachman sign was graded as negative (<2 mm), trace (3–5 mm) and positive (>6 mm). Also the pivot shift test was graded as equal, glide, gross and marked. For ligament laxity evaluation, the anterior knee laxity was measured using the KT-2000 arthrometer® (MEDmetric Corp. San Diego, CA). Injured and contralateral normal knees were measured with a maximum manual anterior force applied to the proximal tibia at 20° of knee flexion. The side-to-side difference (injured minus normal) in anterior laxity was used as a representative indicator of restored knee laxity. To analyze thigh strength, the peak extension and flexion torques were isokinetically measured using Biodex system 3® (Biodex Medical Systems, Shirley, NY, USA) at 60 deg/s. The side-to-side ratio (ratio of peak muscle torque of operated knee/peak muscle torque of contralateral knee × 100) in peak muscle torque was used as the representative parameter for thigh muscle strength. Plain radiographs in this study included the weight-bearing view during flexion [22], a non-weight-bearing lateral view and the skyline view at 45 degrees of knee flexion. Joint space narrowing was elucidated by these radiographs at the final follow-up in comparison with pre-operative radiographs.
Statistical analysis
Statistical analyses were conducted using the SPSS 11.5 J (SPSS Japan, Inc., Tokyo, Japan) software package. A difference of P < 0.05 was considered significant.
Results
Subjective evaluation
According to the IKDC subjective assessment by patients, 32 knees (41%) were graded as “normal”, 41 (53%) as “nearly normal” and 4 (5%) as “abnormal” with 1 (1%) recurrent abnormal laxity following a traumatic episode or re-injury (R/R) (Table 2). The reasons for grades of “nearly normal” or “abnormal” were as follows: 19 patients complained of occasional slight pain; 12 of feeling different than the normal side; 7 of muscle weakness; 4 of difficulty in sitting Japanese style; 1 of an unstable knee; 1 of mild pain and 1 of anxiety over a re-injury.
Objective evaluation
Three of the patients were excluded from the objective evaluation: one, re-injury during the pre-injury sports activity followed by the revision surgery; two, ACL injury to the contralateral knee before the final follow-up examination. Loss of knee extension less than 5 degrees was observed in 2 patients (3%) and loss of flexion less than 5 degrees in 2 patients (3%). Lachman sign was negative in 71 patients (95%) and trace in 4 patient (5%). The pivot shift test was negative or equivalent to the contralateral healthy knee in 73 patients (97%) and glide in 2 patients (3%)(Table 3). The KT side-to-side difference in anterior laxity at manual maximum force was 0.9 mm ± 1.2 (range: −3 to 5 mm). Seventy patients (93%) had a value between −1 mm and 2 mm (Fig. 3).
Thigh muscle strength
Thigh muscle strength evaluation was performed on 62 out of 75 patients. The percentage of isokinetic peak torque of knee extension and flexion for the operated knee compared to the contralateral normal knee was 90% ± 16 and 95% ± 21 (Table 3).
Radiographic evaluation
Joint space narrowing in each compartment is shown in Table 3. Patellofemoral joint space narrowing was not observed in any patients. Medial joint space narrowing less than 50% was found in 8 patients (11%). Lateral joint space narrowing less than 50% was noted in 21 patients (28%).
Discussion
Recently, great progress has been made in ACL reconstruction due to a combination of increased understanding of the precise anatomy [2, 3, 6, 10], innovative biomechanics with newly-developed robotic technology [7, 13–16, 29], and improved operative instrumentation [21, 23–25]. We have also made a great effort to develop more anatomically-oriented reconstruction procedures accompanied by the above-mentioned improvements as shown in Fig. 1. First, we started to use a double-bundle ACL reconstruction of the bi-socket ACL procedure advocated by T. D. Rosenberg, in which two separate double-looped grafts were fixed via two femoral sockets and one tibial tunnel (HS-1T procedure) [9, 21, 28]. This was followed by implementation of the LS-1T procedure to avoid graft impingement to the intercondylar notch or the PCL, which also had two femoral sockets and one tibial tunnel [28]. After these series, we attempted to make two separate tibial tunnels to improve remodeling of the central part of the graft by widening the graft-bone interface in the tibial side with the same location of the femoral sockets. Because of technical difficulty in making the PL tunnel long enough to securely fix the graft with an Endo-button® on the lateral femoral cortex through the far antero-medial portal [23], we were obliged to create the tunnels a little bit higher than each anatomical footprint of the AM and the PL bundles of the native ACL [10]. Therefore, we are now performing an anatomical double-bundle ACL reconstruction in which two femoral and two tibial tunnels are created at the anatomical footprints. Thus, the present procedure described here could be regarded as a transitional procedure from the Rosenberg’s bi-socket ACL reconstruction to the anatomical double-bundle ACL reconstruction. While we have performed several procedures for ACL reconstruction, we firmly believe that it is very important to summarize the clinical results of each procedure in order to better understand the improvements made in ACL reconstructions. Here, we have compared the short-term clinical outcome of the LS-2T procedure, the transitional double-bundle reconstruction, with that of the previously-reported LS-1T procedure that characterized by two femoral sockets in the same location as in this series, and by the single tibial tunnel in the center of the attachment area [28]. Thus, this presents an opportunity to compare the outcome of the two procedures to scrutinize the effect of doubling the tibial tunnels. Previously-reported data for the patients who had had a follow-up of 24 months or longer after receiving ACL reconstruction by the LS-1T procedure are summarized in Table 4. The subjects of these groups were not totally comparative because we found significant difference in activity level (Mann–Whitney U test; P = 0.02), treatment for the lateral meniscal lesion (Mann–Whitney U test; P = 0.005) and the chondral lesion in the lateral tibial plateau (Mann–Whitney U test; P = 0.023) between the groups. However, we still believe it important to compare the clinical outcomes despite of these biases.
Subjectively, 73 out of 78 knees (94%) with the present procedure were graded as “normal” or “nearly normal”, while 40 out of 43 knees (94%) with the LS-1T procedure were also graded as “normal” or “nearly normal” (Table 4). This suggests that this transitional reconstruction approach could produce subjectively satisfactory outcomes. However, a significantly greater percentage of patients in this series was categorized into the nearly-normal group compared to patients after the LS-1T procedure (53 vs. 16%)(Mann–Whitney U test; P ≤ 0.001). Answers of “nearly normal” were considered to represent subtle complaints with no disabilities involving sports activities while answers of “abnormal” indicated unstable knees or mild pain. Taking this into account, this greater percentage of nearly-normal knees may be due to increased patients’ demand for ACL reconstruction.
The rate of R/R was 1% with the LS-2T procedure and 7% with the LS-1T procedure, a difference was not statistically significant (Fisher’s exact test; P = 0.128). As the R/R rate was influenced by patients’ activity levels and/or frequency of participation in sports activities, we could not easily conclude that the LS-2T procedure has a low R/R rate. However, findings suggested that the two tibial tunnels did not adversely affect this rate.
As for objective findings, satisfactory results for ROMs, Lachman sign, pivot shift test and isokinetic peak torque of thigh muscle were shown for both the LS-2T and LS-IT groups, however, no significant difference was found between these two procedures (loss of extension and flexion: P = 0.300, 0.958, Lachman sign: P = 0.228, pivot shift test: P = 0.160; Mann–Whitney U test and isokinetic peak torque of thigh muscle: P = 0.501, 0.318; Student’s t test). The side-to-side difference in KT value was 0.9 mm ± 1.2 for the LS-2T procedure and was 1.0 mm ± 1.6 for the LS-1T procedure, showing no statistically significant difference (Student’s t test; P = 0.719). In previous studies, the average residual anterior laxity measured with KT 2000 ranged from 1.1 to 2.2 mm [18, 19, 26, 32]. Hence, our results were no less favorable despite differences in surgical techniques and post-operative rehabilitation regimens. When KT values of −1 to 2 mm were considered to be successful, 93% of the patients were regarded as successful cases. As 80% of the patients in the LS-1T procedure were included in this range, there was no statistically significant difference between the success rates of the two procedures (Fisher’s exact test; P = 0.059). A high success rate and small residual anterior laxity suggested that favorable antero-posterior and rotatory laxity could be gained by the LS-2T procedure without any harmful effects by the two tibial tunnels.
Radiologically results for the LS-2T procedure were similar to the LS-1T procedure regarding joint space narrowing. Joint space narrowing was affected by the condition of both meniscal and chondral lesions; therefore, we considered that much more subjects are needed to statistically evaluate the effect of the meniscal and chondral lesions on the joint space narrowing. Unfortunately we considered our series was too small to evaluate it.
In summary, this LS-2T procedure, the transitional procedure to the anatomical double-bundle ACL reconstruction, produced results as satisfactory as the LS-1T procedure without severe complications. This suggests that doubling tibial tunnels does not adversely affect the clinical outcome of ACL reconstruction.
Finally, it is with regret that the follow-up rate was not very high despite our tremendous efforts. A higher follow-up rate is very difficult to achieve in the geographical location of our urban area where patients move so frequently. However, we believe that our data provide basic information on the clinical outcome of the transitional technique to the anatomical double-bundle ACL reconstruction.
Conclusion
The LS-2T double-bundle ACL reconstruction with multi-stranded hamstring tendons provided subjectively and objectively satisfactory outcomes over a short-term follow-up period.
References
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single-and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 454:108–113
Amis AA, Dawkins GPC (1991) Functional anatomy of the anterior cruciate ligament. J Bone Joint Surg Br 73:260–267
Arnold MP, Kooloos J, Kampen AV (2001) Single incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Artrosc 9:194–199
Bellier G, Christel P, Colombet P, Djian P, Franceschi JP, Sbihi A (2004) Double-stranded hamstring graft for anterior cruciate ligament reconstruction. Arthroscopy 20:890–894
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:1000–1006
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23:1218–1225
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22:85–89
Graf B (1987) Isometric placement of substitutes for the anterior cruciate ligament. In: Jackson DW (ed) The anterior cruciate deficient knee. Mosby, St. Louis, pp 102–113
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T (2001) Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy 17:801–807
Iwahashi T, Shino K, Nakata K, Nakamura N, Yamada Y, Yoshikawa H, Sugamoto K (2008) Qantitative determination of ACL femoral footprint: superimposition technique of microscopic measurement on three-dimensional volume rendering (3-DVR) CT image. In: 13th ESSKA 2000 congress, Porto
Kim SJ, Jung KA, Song DH (2006) Arthroscopic double-bundle anterior cruciate ligament reconstruction using autogenous quadriceps tendon. Arthroscopy 22:797.e1–797.e5
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med [Epub ahead of print]
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement. Arthroscopy 19:297–304
Mae T, Shino K, Miyama T, Shinjo H, Ochi T, Yoshikawa H, Fujie H (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy 17:708–716
Mae T, Shino K, Nakata K, Toritsuka Y, Otsubo H, Fujie H (2008) Optimization of graft fixation at the time of anterior cruciate ligament reconstruction. Part I: effect of initial tension. Am J Sports Med 36:1087–1093 Epub 2008 Feb 29
Mae T, Shino K, Nakata K, Toritsuka Y, Otsubo H, Fujie H (2008) Optimization of graft fixation at the time of anterior cruciate ligament reconstruction. Part II: effect of knee flexion angle. Am J Sports Med 36:1094–1100 Epub 2008 May 9
Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15:618–624
Muneta T, Koga H, Morito T, Yagishita K, Sekiya I (2006) A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy 22:252–258
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
O’Meara PM, O’Brien WR, Henning CE (1992) Anterior cruciate ligament reconstruction stability with continuous passive motion. The role of isometric graft placement. Clin Orthop 277:201–209
Rosenberg TD, Graf B (1994) Techniques for ACL reconstruction with Multi-Trac drill guide. Acufex Microsurgical, Mansfield
Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM (1988) The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am 70:1479–1483
Shino K, Horibe S, Hamada M, Nakamura N, Nakata K, Toritsuka Y, Mae T (2002) Allograft anterior cruciate ligament reconstruction. Tech Knee Surg 1:78–85
Shino K, Mae T, Maeda A, Miyama T, Shinjo H, Kawakami H (2002) Graft fixation under predetermined tension using a new device “Double Spike Plate (DSP)”. Arthroscopy 18:908–991
Shino K, Nakata K, Nakamura N et al (2005) Anatomic anterior cruciate ligament reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop 15:130–134
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16:232–238 Epub 2008 Jan 12
Toritsuka Y, Shino K, Horibe S, Mitsuoka T, Hamada M, Nakata K, Nakamura N, Yoshikawa H (2004) Second-look arthoscopy of anterior cruciate ligament grafts with multistranded hamstring tendons. Arthroscopy 20:287–293
Toritsuka Y, Amano H, Yamada Y, Hamada M, Mitsuoka T, Horibe S, Shino K (2007) Bi-socket ACL reconstruction using hamstring tendons: high versus low femoral socket placement. Knee Surg Sports Traumatol Arthrosc 15:835–846 Epub 2007 Mar 16
Yagi M, Wrong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M (2007) Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 454:100–107
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Acknowledgments
No author or related institution has received any financial benefit from research in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Toritsuka, Y., Amano, H., Kuwano, M. et al. Outcome of double-bundle ACL reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc 17, 456–463 (2009). https://doi.org/10.1007/s00167-008-0707-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0707-7