Abstract
Purpose
Since the development of the anatomic double-bundle anterior cruciate ligament (ACL) reconstruction, many studies have focused on excursion and/or tension of each graft. However, no studies to date have adequately investigated thickness of the graft in anatomic double-bundle ACL reconstruction. To obtain basic knowledge from which an ideal graft thickness can be inferred, thicknesses of the anteromedial bundle (AMB) and posterolateral bundle (PLB) was measured in the normal ACL.
Methods
The right knees of 50 cadavers donated for anatomy instruction were studied. Each ACL was separated into the AMB and PLB, and circumferences at the mid-substance and cross-sectional area at the femoral and tibial footprints were measured in each.
Results
Cross-sectional areas of the AMB and PLB were 36 ± 10 and 32.1 ± 10.2 mm2 at the femoral footprint, and 60.9 ± 21.8 and 52.2 ± 17.3 mm2 at the tibial footprint, respectively. Circumferences at the mid-substance were 14.3 ± 3.3 mm for the ALB and 10.8 ± 3.1 mm for the PLB. A positive correlation was seen between AMB and PLB at each of the three sites.
Conclusion
The AMB is thicker than the PLB, showing a constant correlation in the normal ACL. This suggests that the anteromedial graft must be thicker than the posterolateral graft at least in actual operations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The normal anterior cruciate ligament (ACL) is composed mainly of two bundles [9, 22]: the anteromedial bundle (AMB) and the posterolateral bundle (PLB). Several studies have shown that the PLB contributes to rotational stability near the extension position of the knee and that both bundles contribute to anterior stability [4, 10, 14, 22, 23, 34]. The anatomic double-bundle ACL reconstruction has been developed to precisely and independently reconstruct the AMB and PLB [6, 18, 32], and to date has been reported to yield comparatively excellent results [1, 2, 12, 16, 17, 27, 30, 31]. However, some extremely complicated problems are revisited by having to divide the ACL into two functionally different bundles [21, 24]. If the anteromedial graft (AMG) and posterolateral graft (PLG) become functionally independent of that grafts are placed at an anatomic position, excursion of grafts does not exhibit isometry [29]. In addition, either the AMG or the PLG might be the main recipient of external force according to the knee position. These issues may restrict range of motion or lead to graft rupture [21]. To avoid such problems, many recent studies [7, 8, 13, 19, 33] have examined initial tension and flexion angle at the time of graft fixation, and knowledge is slowly being accumulated. However, extremely few reports have studied the thickness of the graft. That is, if division into two bundles is performed at an inappropriate ratio even with sufficient total thickness of grafts, the thickness of either the AMG or the PLG will be insufficient. The risk of failure will thus increase for one of the grafts. A constant standard in the ratio of AMG to PLG thicknesses thus seems necessary.
The purpose of this study was to obtain basic knowledge of the relationship between thicknesses of the AMB and PLB in the normal ACL. Hypothesis of this study was that the AMB is thicker than the PLB, with a constant correlation.
Materials and methods
The donated cadavers for anatomy practice to Kurume University School of Medicine were used in this study. And therefore, the research protocol of the present study was reviewed and approved by the university ethical committee.
Among 55 formalin-fixed cadavers, one with ACL degeneration due to osteoarthritis, one with ACL calcification, and three in which the ACL could not be separated into the AMB and PLB were excluded. The remaining 50 cadavers (32 men, 18 women) were selected as the study materials, examining the right knee in each case. ACLs were almost normal in all 50 knees and were easily separated into the AMB and PLB. Mean age at the time of death was 79 years (median, 80 years; range, 48–103 years).
Measurement of the ligament
The knee was flexed at 70°–90°, and the muscles, articular capsules, and patellar tendon around the knee were removed using a scalpel. The medial femoral condyle was then resected using an oscillating saw while protecting the ACL with the elevatorium, allowing the whole of the ACL to be observed. The PCL was separated on the tibial side and resected together with the medial femoral condyle. The synovial membrane on the ACL surface, the entirety of which could be observed, was removed with care, and the ACL was separated carefully at the mid-substance of the ligament into the AMB and PLB.
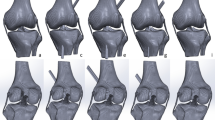
The knee was flexed precisely at 90 degrees using the goniometer and was fixed by 2 Kirshner wires. Superficial fibers at anterior part of the AMB and PLB were carefully traced between the femoral and the tibial insertion, and then, the midpoint of fibers was marked using a marker pen. No. 2 Ethibond suture (Johnson & Johnson, New Brunswick, NJ) was placed around the AMB and PLB at the midpoint of the ligament that was previously marked, and tightened by applying a tension of 0.5 N using a tensionometer (Acufex Microsurgical, Mansfield, MA) (Fig. 1). In this state, the suture was cut from the tip of the tensionometer, and the length of the suture was measured by a unit of 1/10 mm. This measurement was repeated three times, and the mean value was regarded as the circumference.
The AMB and PLB were then separated from each other at the mid-substance. Each separated bundle of fibers was carefully traced up to the point of attachment to the femur and cut from the bone surface with care. In this state, only the functional fibers that continued from the mid-substance were traced, and the mixture fibers except it excluded as much as possible. The remaining footprint was marked using a marker pen. The tibial side was marked in a similar way. Footprints of the AMB and PLB on the femur and tibia were recorded together with a scale using a digital camera (Pentax, Tokyo, Japan). The images were then input into a computer, and cross-sectional areas (CSAs) of the AMB and PLB at the femoral and tibial footprints were measured using image analysis software “NIH Image J” by a unit of 1/10 mm2. This value was measured three times, and the mean of those three values was regarded as the CSA.
Statistical analysis
All measurements were made by only one (M.K) of authors. Because of this, the inter-observer reliability of the measurement could not be calculated. However, intra-observer reliability for each of the three measurements was sufficiently high: R = 0.98, R 2 = 0.95, P < 0.0001 at the femoral footprint; R = 0.86, R 2 = 0.74, P < 0.0001 at the mid-substance; and R = 0.99, R 2 = 0.97, P < 0.0001 at the tibial footprint.
The correlation between measured data for the AMB and PLB at the three sites was analyzed using Pearson’s correlation coefficient. A regression line was then obtained using the measured data for the PLB as an independent variable and those for the AMB as a dependent variable. A confidence level of 95% (P < 0.05) was chosen for statistical significance. Data are presented as mean value ±SD.
All statistical processing was conducted using JMP version 5.0 software (SAS Institute, Cary, NC).
Results
At the femoral footprint, mean (±standard deviation (SD)) CSA was 36.0 ± 10.0 mm2 for the AMB and 32.1 ± 10.2 mm2 for the PLB. Mean CSA ratio (AMB/PLB) was 1.1. At this site, a low positive correlation (r = 0.31, R 2 = 0.10, P = 0.0276) with CSA was observed between the AMB and the PLB at the 3% level (Fig. 2a). At the mid-substance, mean circumference was 14.3 ± 3.3 mm for the AMB and 10.8 ± 3.1 mm for the PLB; the circumference ratio (AMB/PLB) was 1.3. At this site, a high positive correlation (r = 0.76, R 2 = 0.57, P < 0.0001) with circumference was observed between the AMB and the PLB at the 0.01% level (Fig. 2b). At the tibial footprint, mean CSA was 60.9 ± 21.8 mm2 for the AMB and 52.2 ± 17.3 mm2 for the PLB; mean CSA ratio (AMB/PLB) was 1.2. At this site, a positive correlation (r = 0.59, R 2 = 0.35, P < 0.0001) with CSA was observed between the AMB and the PLB at the 0.01% level (Fig. 2c). The linear regression formula using CSA or circumference of the PLB as an independent variable, X, and those of the AMB as a dependent variable, Y, was Y = 0.31X + 26.15 at the femoral footprint, Y = 0.82X + 5.50 at the mid-substance, and Y = 0.74X + 22.09 at the tibial footprint.
Discussion
The present study obtained an important finding, although thickness of the AMB and PLB was only measured in the normal ACL at three sites (femoral footprint, mid-substance, and tibial footprint). This finding was that the AMB is thicker than the PLB with a constant correlation in the normal ACL. The AMG must thus be thicker than the PLG at least when the harvested tendon was divided into two grafts, and marked imbalances in the division of grafts must be avoided.
The implanted graft undergoes remodeling and changes into new ligamentous tissue [3], but the mechanical strength will never exceed that of the normal ligament [5]. The graft thus becomes enlarged and thickened to reinforce overall material strength. To obtain a final structural strength equal to that of the normal ACL, the graft must be as thick as possible because the remodeling process [20] cannot be controlled. However, obtaining an appropriate thickness of graft is not always easy. If the graft is divided in an inappropriate ratio, the thickness of either the AMG or the PLG will be insufficient even if the total thickness of grafts appears adequate. Although the appropriate ratio for thicknesses of the AMG and PLG should logically reflect the situation in the normal ACL, basic data on this issue have been lacking to date.
Many previous studies [11, 15, 25, 26, 28] have addressed the shape and/or CSA of the AMB and PLB at the femoral and tibial footprints. Harner et al. [10] measured CSA of the AMB and PLB using the knees of 10 fresh frozen cadavers. They reported that mean CSAs of the AMB and PLB at the femoral footprint were 47 ± 13 and 49 ± 13 mm2, respectively, compared with 56 ± 21 and 53 ± 21 mm2 at the tibial footprint, respectively. Mean cross-sectional ratio (AMB/PLB) was 1.0 on the femoral side and 1.1 on the tibial side. Takahashi et al. [25], using 32 donated cadavers, reported that mean CSAs of the AMB and PLB on the femoral side were 66.9 ± 2.3 and 66.4 ± 2.3 mm2, respectively, compared with 67.0 ± 18.4 and 52.4 ± 17.6 mm2 on the tibial side. Mean CSA ratio (AMB/PLB) was 1.0 on the femoral side and 1.3 on the tibial side. Cross-sectional ratios of AMB and PLB in the present study were almost the same as those in the above two reports [11, 25]. The method for measurement of the footprint in this study thus appears suitable. However, absolute values for CSA differ considerably among investigations. This may be due to the extreme difficulty in identifying the true border of the attached part of the ligament. At the footprint of the ligament to the bone, the fibers spread toward the bottom, and many surrounding fibrous tissues other than the functional fibers properly become mixed in. The area of the femoral and tibial footprint is thus more than 3.5 times larger than at the mid-substance [11, 35]. Separating the functional fibers from other fibrous tissues is difficult. The absolute value of the CSA will thus differ according to whether the AMB and PLB have been separated, and the area that is regarded as the boundary of the attached part. However, with regard to mean CSA ratio (AMB/PLB), i.e., the ratio of values for the AMB and PLB determined by the same investigator, the results of the three reports, including this study, appear to approximate each other.
On the other hand, no studies have measured CSA of the AMB and PLB at the mid-substance of the ligament. As far as we can tell, data for the femoral footprint obtained by Mochizuki et al. [15] may reflect thickness of the mid-substance of the ligament for the reasons described below. Using 10 donated cadavers, they carefully removed various fibers that were mixed from the surrounding or fibers of the periligamentous membrane and identified a femoral footprint composed only of functional fibers continuous from the mid-substance of the ligament. As a result, the cross-sectional ratio was considered to approximate that of the mid-substance where only functional fibers are aggregated in a compact manner. They reported that mean long and short diameters at the femoral footprints of the AMB and PLB were 9.2 ± 0.7 × 4.7 ± 0.6 mm and 6.0 ± 0.8 × 4.7 ± 0.6 mm, respectively; the mean circumference ratio (AMB/PLB) was 1.3. In the present study, circumference ratios of both the AMB and the PLB at the mid-substance were completely the same as those at the femoral footprint reported by Mochizuki et al. [15] although absolute values of both AMB and PLB were approximately one-third. The circumference ratio of AMB and PLB (AMB/PLB) can thus be interpreted to approximate 1.3 at all levels when only true functional fibers are traced. This means that the AMB is thicker than the PLB when only functional fibers are traced.
Based on present measurements, a trial calculation of the ideal thickness of both the AMG and the PLG was made using a linear regression formula for the femoral footprint, mid-substance, and tibial footprint. In an actual operation, the CSA of the minimum size through which a graft created using a cylindrical sizing tube with an increment of 0.5 mm in diameter can pass is regarded as the CSA of the graft, by assuming the cross-sectional shape to be a circle. On this basis, the diameter of the ideal AMG derived from the linear regression formula is shown in Table 1, when the diameter of the PLG created during actual surgery is set in 0.5-mm increments. Thus, in our opinion, the most important indicator seems to be the reference value at the mid-substance of the ligament, since the positive correlations observed at both the femoral and the tibial footprints were not particularly strong and many outliers were seen. Accordingly, the diameter of the AMG should ideally exceed that of the PLG by more than 0.9–0.4 mm, if the diameter of the PLG usually used in clinical ranges from 4.5 to 7.0 mm. Other surgeons may trust the data of the femoral footprint or the tibial footprint, but it is desirable for AMG to be thicker than PLG in this situation.
This study had several limitations. First, formalin-fixed cadavers were used. Due to the dehydrating effects of formalin fixation, the measured results may be less than actual conditions, particularly at the mid-substance. However, this condition should apply equally to the AMB and PLB, and thus would not influence the relationship between the AMB and the PLB. Second, the age of donor cadavers was much higher than that of patients who actually undergo ACL reconstruction. However, the cadavers did not belong to a patient group that usually has knee problems requiring total knee arthroplasty or arthroscopy. No individuals showed moderate or more severe degenerative changes, and the ACLs were considered to be almost normal. The present results are thus considered to be sufficiently accurate. Furthermore, some factors that may influence the thickness of the ACL were not sufficiently considered. Width and shape of the intercondylar notch were not measured. Height and weight of the formalin-fixed cadavers could not be measured accurately, and these data had not been recorded during the lifetimes of the donors. Gender and lengths of the femur and tibia were considered, but did not influence the results (data not shown). However, evidence that these factors did, in fact, influence the thickness of the ACL was insufficient. At least for ordinary clinical settings, results of this study can be considered sufficiently reliable.
As clinical relevance, the result of this study shows one opinion on a clinical problem how two grafts prepared from the harvested tendon had better be assigned to AMG and PLG each. Namely, a thicker graft should be used for AMG, and a little thin graft should be used for PLG, but it had better be kept the difference in the diameter within less than about 1 mm, in the anatomic double-bundle ACL reconstruction. This thing may support a traditional way that many surgeons practice by own experience.
Conclusion
The AMB is thicker than the PLB, showing a constant correlation in the normal ACL. This suggests that the AMG must be thicker than the PLG at least when the harvested tendon was divided into two grafts in actual operations. Furthermore, marked imbalances in graft division must be avoided.
References
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38:25–34
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single- and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 454:108–113
Amiel D, Kleiner JB, Akeson WH (1986) The natural history of the anterior cruciate ligament autograft of patellar tendon origin. Am J Sports Med 14:449–462
Amis AA, Dawkins GPC (1991) Functional anatomy of the anterior cruciate ligament: fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br 73:260–267
Butler DL, Grood ES, Noyes FR, Olmstead ML, Hohn RB, Arnoczky SP, Siegel MG (1989) Mechanical properties of primate vascularized vs. nonvascularized patellar tendon grafts; changes over time. J Orthop Res 7:68–79
Christel P, Sahasrabudhe A, Basdekis G (2008) Anatomic double-bundle anterior cruciate ligament reconstruction with anatomic aimers. Arthroscopy 24:1146–1151
Cuomo P, Rama KRBS, Bull AMJ, Amis AA (2007) The effects of different tensioning strategies on knee laxity and graft tension after double-bundl anterior cruciate ligament reconstruction. Am J Sports Med 35:2083–2090
Farrow LD, Parker RD (2010) The relationship of lateral anatomic structures to exiting guide pins during femoral tunnel preparation utilizing an accessory medial portal. Knee Surg Sports Traumatol Arthrosc 18:747–753
Ferretti M, Levicoff EA, Macpherson TA, Moreland MS, Cohen M, Fu FH (2007) The fetal anterior cruciate ligament: an anatomic and histologic study. Arthroscopy 23:278–283
Gabriel MT, Wong EIS, Woo SLY, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22:85–89
Harner CD, Baek GH, Vogrin TM, Carlin GJ, Kashiwaguchi S, Woo SL-Y (1999) Quantitative analysis of human cruciate ligament insertions. Arthroscopy 15:741–749
Kondo E, Yasuda K (2007) Second-look arthroscopic evaluations of anatomic double-bundle anterior cruciate ligament reconstruction: relation with postoperative knee stability. Arthroscopy 23:1198–1209
Mae T, Shino K, Matsumoto N, Hamada M, Yoneda M, Nakata K (2007) Anatomical two-bundle versus Rosenberg’s isometric bi-socket ACL reconstruction: a biomechanical comparison in laxity match pretension. Knee Surg Sports Traumatol Arthrosc 15:328–334
Mae T, Shino K, Matsumoto N, Nakata K, Nakamura N, Iwahashi T (2006) Force sharing between two grafts in the anatomical two-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 14:505–509
Mochizuki T, Muneta T, Nagase T, Shirasawa S, Akita K, Sekiya I (2006) Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:356–361
Muneta T, Koga H, Morito T, Yagishita K, Sekiya I (2006) A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy 22:252–258
Muneta T, Koga H, Mochizuki T, Ju Y-J, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15:618–624
Murray PJ, Alexander JW, Gold JE, Icenogle KD, Noble PC, Lowe WR (2010) Anatomic double-bundle anterior cruciate ligament reconstruction: kinematics and knee flexion angle–graft tension relation. Arthroscopy 26:202–213
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66:344–352
Otsubo H, Shino K, Nakamura N, Nakata K, Nakagawa S, Koyanagi M (2007) Arthroscopic evaluation of ACL grafts reconstructed with the anatomical two-bundle technique using hamstring tendon autograft. Knee Surg Sports Traumatol Arthrosc 15:720–728
Petersen W, Zantop T (2007) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Sahasrabudhe A, Christel P, Anne F, Appleby D, Basdekis G (2010) Postoperative evaluation of tibial footprint and tunnels characteristics after anatomic double-bundle anterior cruciate ligament reconstruction with anatomic aimers. Knee Surg Sports Traumatol Arthrosc 18:1599–1606
Seon JK, Gadikota HR, Wu J-L, Sutton K, Gill TJ, Li G (2010) Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med 38:1359–1367
Takahashi M, Doi M, Abe M, Suzuki D, Nagano A (2006) Anatomical study of the femoral and tibial insertions of the anteromedial and posterolateral bundle of human anterior cruciate ligament. Am J Sports Med 34:787–792
Tállay A, Lim MH, Bartlett J (2008) Anatomical study of the human anterior cruciate ligament stump’s tibial insertion footprint. Knee Surg Sports Traumatol Arthrosc 16:741–746
Toritsuka Y, Amano H, Kuwano M, Iwai T, Mae T, Ohzono K, Shino K (2009) Outcome of double-bundle ACL reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc 17:456–463
Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S (2008) Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci 13:122–129
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SLY (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yasuda K, Tanabe Y, Kondo E, Kitamura N, Tohyama H (2010) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 26:S21–S34
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Yoo YS, Jeong WS, Shetty NS, Ingham SJM, Smolinski P, Fu FH (2010) Changes in ACL length at different knee flexion angles: an in vivo biomechanical study. Knee Surg Sports Traumatol Arthrosc 18:292–297
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Zantop T, Petersen W, Sekiya JK, Musahl V, Fu FH (2006) Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc 14:982–992
Acknowledgments
The authors special thank Dr. Takashi Inoue (Department of Orthopaedic Surgery, Takagi Hospital), Dr. Hidetaka Murakami (Department of Orthopaedic Sports Medicine, Murakami Hospital), and Dr. Megumi Noyama (Department of Orthopaedic Surgery, Kurume University School of Medicine) for their kindly assistance and helpful discussion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katouda, M., Soejima, T., Kanazawa, T. et al. Relationship between thickness of the anteromedial bundle and thickness of the posterolateral bundle in the normal ACL. Knee Surg Sports Traumatol Arthrosc 19, 1293–1298 (2011). https://doi.org/10.1007/s00167-011-1417-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1417-0