Abstract
Anatomic reconstruction of the anterior cruciate ligament through an accessory medial portal has become increasingly popular. The purpose of this study is to describe the relationship of guide pin exit points to the lateral anatomic structures when preparing the anterior cruciate ligament femoral tunnel through an accessory medial portal. We utilized seven fresh frozen cadaveric knees. Utilizing an anteromedial approach, a guide wire was placed into the center of each bundle’s footprint. Each guide wire was advanced through the lateral femoral cortex. The guide pins were passed at 90, 110, and 130° of knee flexion. The distances from each guide pin to the closest relevant structures on the lateral side of the knee were measured. At 90° the posterolateral bundle guide pin was closest to the lateral condyle articular cartilage (mean 5.4 ± 2.2 mm) and gastrocnemius tendon (mean 5.7 ± 2.1 mm). At 110° the posterolateral bundle pin was closest to the gastrocnemius tendon (mean 4.5 ± 3.4 mm). At 130° the posterolateral bundle pin was closest to the gastrocnemius tendon (mean 7.2 ± 5.5 mm) and lateral collateral ligament (mean 6.8 ± 2.1 mm). At 90° the anteromedial bundle guide pin was closest to the articular cartilage (mean 2.0 ± 2.0 mm). At 110° the anteromedial bundle pin was closest to the articular cartilage (mean 7.4 ± 3.5 mm) and gastrocnemius tendon (mean 12.3 ± 3.1 mm). At 130° the AM bundle pin was closest to the gastrocnemius tendon (mean 8.2 ± 3.2 mm) and LCL (mean 15.1 ± 2.9 mm). Neither guide pin (anteromedial or posterolateral bundle) put the peroneal nerve at risk at any knee flexion angle. At low knee flexion angles the anteromedial and posterolateral bundle guide pins closely approximated multiple lateral structures when using an accessory medial arthroscopic portal. Utilizing higher flexion angles increases the margin of error when preparing both femoral tunnels. During preparation of the anterior cruciate ligament femoral tunnel through an accessory anteromedial portal the tunnels should be drilled in at least 110° of knee flexion in order to move guide pin exit points away from important lateral knee structures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament has long been known to have two, distinct functional bundles. However, traditional anterior cruciate ligament reconstruction has attempted to reconstruct the more important anteromedial bundle by placing the femoral tunnel “high” in the intercondylar notch at the 1 o’clock or 11 o’clock positions in left and right knees, respectively. Recently there has been much interest in anatomic double-bundle reconstruction of the anterior cruciate ligament. While clinical evidence is lacking to support the routine use of double-bundle anterior cruciate ligament reconstruction in all patients [10, 24, 26, 36], recently published anatomic studies have given surgeons a better understanding of the three dimensional topography of the anterior cruciate ligament femoral attachment [6, 8, 9, 20, 25, 32, 33, 40]. This knowledge is important in both single and double-bundle reconstruction as it suggests a more lateral starting point on the lateral wall of the intercondylar notch brings the femoral tunnel closer to the true footprint of the native anterior cruciate ligament [10, 13, 34].
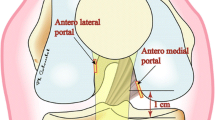
During endoscopic reconstruction of the anterior cruciate ligament, the femoral tunnel has traditionally been prepared using a trans-tibial technique. While this technique allows for easy preparation of the anterior cruciate ligament femoral tunnel, it can also result in vertical, non-anatomic femoral tunnel placement [1, 13, 16, 34]. Due to this difficulty with anatomic femoral tunnel placement using the trans-tibial technique, some authors prefer to drill the femoral tunnel through an accessory medial arthroscopic portal [3, 27, 37]. One of the downsides of femoral tunnel preparation through an accessory anteromedial arthroscopic portal is the shorter tunnel lengths that are obtained compared to the trans-tibial technique [14, 28]. We have also noticed anecdotally that with more anatomic placement of the femoral tunnel through an accessory medial arthroscopic portal, the guide pin has migrated to a more lateral exit point at the distal thigh (Fig. 1). To our knowledge, there are no published studies describing the lateral anatomic structures at risk during drilling of the anterior cruciate ligament anteromedial and posterolateral bundle femoral tunnels using an accessory medial arthroscopic portal.
Anatomic femoral tunnel placement during single-bundle reconstruction at 90° of flexion. a Lateral knee radiograph demonstrating fixation device (arrowhead) at the posterolateral aspect of the lateral femoral condyle. b Axial magnetic resonance image demonstrating subchondral location of femoral tunnel (arrow). c Axial magnetic resonance image demonstrating fixation device (double arrow) adjacent to lateral head of gastrocnemius tendon (forked arrow)
The purpose of this study is to describe the relationship of guide pin exit points to the lateral anatomic structures when preparing the anterior cruciate ligament femoral tunnel through an accessory medial portal. We hypothesize that the articular cartilage at the posterior border of the lateral femoral condyle and the lateral gastrocnemius tendon are both at risk of guide pin penetration when preparing the anterior cruciate ligament femoral tunnel through an accessory medial arthroscopic portal, especially at lower knee flexion angles.
Materials and methods
We utilized seven fresh frozen human knees for this study. Each specimen was transected at mid-femur and mid-tibia. The femur and tibia of each knee was placed into aluminum cylinders and potted using Woods Metal. This fixation was backed up with two orthogonal, 3.5 mm transfixion pins. The femoral pot was placed into a clamp and the tibial pot was secured in a semi-circular metal frame in order to maintain the appropriate flexion angle during guide pin insertion. Utilizing a medial parapatellar arthrotomy we carefully removed the anterior cruciate ligament, preserving the osseous anatomy of the femoral footprint to aid with guide pin placement. We identified the anteromedial and posterolateral bundle footprints on the lateral wall of the intercondylar notch. The knee was carefully positioned at 90° of flexion as measured with a manual goniometer. Lines parallel to the femoral and tibial shafts were utilized as landmarks to determine the flexion angle. In order to standardize pin placement, the guide pin was passed into the intercondylar notch just lateral to the medial femoral condyle and just above the anterior horn of the medial meniscus. A 2.7 mm guide pin was placed into the center of the posterolateral bundle footprint and advanced through the lateral cortex. Another guide pin was placed into the center of the anteromedial bundle footprint and advanced through the lateral femoral cortex. Guide pin placement was repeated at 110 and 130° of knee flexion. After each pin was placed, the drill was placed on the opposite end of the pin and used to withdraw the guide pin a few millimeters beneath the cortex of the lateral wall of the intercondylar notch. This allowed for subsequent pin placement using identical starting points in the center of the anteromedial and posterolateral bundle footprints.
After all six guide pins were placed into the knee, we carefully exposed the lateral anatomic structures of the knee. Using a digital caliper, the distance from each guide pin to relevant nearby anatomic structures was measured. Each measurement was repeated three times.
Results
The average age of the seven knee specimens were 61 years. There was one female knee and six male knees. Results for the knee measurements are summarized in Table 1. The relevant structures for the 90° posterolateral bundle guide pin were the articular cartilage at the posterior aspect of the lateral femoral condyle and the tendon of the lateral head of the gastrocnemius muscle. For the 90° anteromedial bundle guide pin, the relevant structures were the same. For the 110° posterolateral bundle guide pin, the relevant structures were the femoral attachment of the gastrocnemius muscle and the lateral collateral ligament. For the 110° anteromedial bundle guide pin the articular cartilage and gastrocnemius tendon were closest in proximity. For the 130° posterolateral bundle guide pin the gastrocnemius femoral attachment, lateral collateral ligament femoral attachment, and popliteus femoral attachment were most relevant. For the 130° anteromedial bundle guide pin the gastrocnemius femoral attachment and lateral collateral ligament femoral attachment were closest in proximity.
At 90° of knee flexion the posterolateral bundle guide pin was on average 5.4 ± 2.2 and 5.7 ± 2.1 mm from the articular cartilage and lateral head of gastrocnemius tendon, respectively. In no specimens did the guide pin violate the articular cartilage or the gastrocnemius tendon. The anteromedial bundle guide pin was on average 2.0 ± 2.0 and 14.5 ± 1.7 mm from the articular cartilage margin and gastrocnemius tendon, respectively, at this flexion angle. In two specimens the anteromedial bundle guide pin penetrated the articular cartilage at the posterior margin of the lateral femoral condyle (Fig. 2c). No anteromedial bundle guide pins penetrated the gastrocnemius tendon.
Distal femur after placement of anteromedial and posterolateral bundle guide pins. a Iliotibial band intact. b Lateral anatomic structures dissected. c Posterolateral view of distal femur with articular cartilage border indicated (dotted line). LCL lateral collateral ligament, POP popliteus tendon, GAS lateral head of gastrocnemius tendon. PL1, PL2, and PL3 indicates posterolateral bundle pins placed at 130, 110, and 90°, respectively. AM1, AM2, and AM3 indicate anteromedial bundle guide pins placed at 130, 110, and 90°, respectively
At 110° the posterolateral bundle guide pin was on average 4.5 ± 3.4, 9.9 ± 2.7, and 18.3 ± 3.0 mm from the origin of the lateral head of gastrocnemius tendon, lateral collateral ligament, and popliteus tendons, respectively. In one specimen the guide pin pierced the origin of the gastrocnemius tendon. The anteromedial bundle guide pin was on average 7.4 ± 3.5 and 12.3 ± 3.1 mm from the articular cartilage and gastrocnemius tendon, respectively. No structures were violated with this guide pin.
At 130° the posterolateral bundle guide pin was on average 7.2 ± 5.5, 6.8 ± 2.1, and 14.0 ± 4.6 mm from the gastrocnemius origin, lateral collateral ligament attachment, and popliteus femoral attachment, respectively. In one specimen, the guide pin did violate the gastrocnemius origin. The anteromedial bundle guide pin was on average 8.2 ± 3.2 and 15.1 ± 2.9 mm from the gastrocnemius origin and lateral collateral ligament femoral attachment, respectively. No lateral structures were violated with this anteromedial bundle guide pin.
Discussion
The principle findings of this study demonstrate that guide pins exit near multiple anatomic structures during preparation of both the anterior cruciate ligament anteromedial and posterolateral bundle femoral tunnels utilizing an accessory medial portal. Guide pins are situated particularly close to these important structures when drilling either tunnel at lower flexion angles.
Injuries to the anterior cruciate ligament are extremely common. Over 100,000 anterior cruciate ligament reconstructions are performed in the United States each year. Traditional anterior cruciate ligament reconstruction has reconstructed the anterior cruciate ligament anteromedial bundle. Recently there has been increased interest in anatomic reconstruction of the anterior cruciate ligament. It has been long known that the anterior cruciate ligament is comprised of two functional bundles [11, 25, 29]. Over 30 years ago Girgis et al. [11] demonstrated the differential tension in the separate portions of the anterior cruciate ligament during knee flexion and extension. These authors found that the entire anterior cruciate ligament is taught in knee extension and only the anteromedial portion was taught with knee flexion [11]. Norwood and Cross [29] later described the importance of the anteromedial bundle in resistance of anterior tibial translation and the posterolateral bundle in rotatory stability of the knee. Various biomechanical studies have also characterized the different roles of the two functional bundles with respect to knee kinematics [4, 23, 38, 39]. Based in part on this biomechanical data, some authors have recently recommended anatomic reconstruction of both the anterior cruciate ligament anteromedial and posterolateral bundles.
Due to the recent surge in interest in anatomic reconstruction of the anterior cruciate ligament many studies have been published describing the anatomy of the anterior cruciate ligament functional bundles as well as the topographical anatomy of its femoral attachment along the lateral wall of the intercondylar notch [6, 8, 9, 20, 25, 32, 33]. The radiographic anatomy of the femoral attachment site has also been well described [5, 7]. A better understanding of the three dimensional anatomy of the anterior cruciate ligament femoral attachment has led to more lateral positioning on the lateral wall of the intercondylar notch. Furthermore, multiple authors have demonstrated the vertical, non-anatomic tunnel placement less effectively restores the rotational stability of the knee [19, 21]. Loh et al. [21] demonstrated biomechanically that grafts placed more laterally at the “10 o’clock” position more effectively resisted rotatory loads when compared to grafts placed at the “11 o’clock” position. Clinical observations by Lee et al. [19] found that vertical tunnel positioning resulted in a residual pivot shift on physical examination. These studies further illustrate the importance of more lateral femoral tunnel placement.
Several authors have described in detail the lateral anatomy of the distal femur as it pertains to lateral ligament injury and reconstruction [17, 18]. The lateral collateral ligament, peroneal nerve, popliteus tendon, biceps femoris tendon, and the tendon of the lateral head of the gastrocnemius are the major structures on the lateral aspect of the knee. The femoral attachment of the lateral collateral ligament lays an average of 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle [17, 18]. The lateral gastrocnemius tendon attaches to the femur approximately 13.8 mm posterior to the lateral collateral ligament femoral attachment [17, 18]. The popliteus tendon femoral attachment is in the anterior fifth of the popliteal sulcus, an average of 18.5 mm from the center of the lateral collateral ligament femoral attachment [17, 18]. The biceps femoris tendon lies posterior to the femoral condyle and inserts on the posterior aspect of the fibular head [17, 18]. Finally, the peroneal nerve lies on the posterior border of the biceps femoris.
Multiple authors have recently demonstrated that anatomic drilling of the ACL femoral tunnel is best through a medial arthroscopic portal [2, 10, 14, 15, 22, 30, 35]. Golish et al. [14] evaluated femoral tunnel starting point and length in response to various positioning of the tibial tunnel. These authors found that with more medial positioning of the anterior cruciate ligament tibial tunnel, more anatomic positioning of the femoral tunnel could be achieved [14]. The resultant increased lateral femoral tunnel positioning resulted in shorter femoral tunnel length overall [14]. With preparation of the femoral tunnel through a medial arthroscopic portal the femoral tunnel achieved anatomic positioning, but tunnel lengths averaged only 23 mm [14]. Basdekis et al. [2] evaluated femoral tunnel orientation with respect to knee flexion angle during single bundle reconstruction through a standard anteromedial arthroscopic portal. These authors recommended drilling at 110° of knee flexion [2]. These authors found that drilling at 90° of knee flexion could result in posterior wall blow-out [2]. At 130° of knee flexion, the authors found the increased acuity of the femoral tunnel with respect to the lateral wall of the intercondylar notch would not be acceptable [2]. Other authors have recommended the use of a far medial working portal for femoral tunnel guide pin placement, an accessory medial portal [3, 10, 27, 37]. Fu et al. [10] demonstrated that the anatomic site of the anteromedial bundle could only be reached 3% of the time when utilizing a trans-tibial technique through the anteromedial bundle tibial tunnel. With preparation through an accessory medial portal the anteromedial bundle footprint could be accessed 96% of the time [10].
Despite our knowledge of the anatomy of the anterior cruciate ligament’s two functional bundles and the topographical and radiographic anatomy of the intercondylar notch, not much is known about the lateral anatomic structures at risk during drilling of the anterior cruciate ligament femoral tunnel through a low, accessory medial portal. Neven et al. [28] recently evaluated that lateral structures were at risk during drilling of the posterolateral bundle femoral tunnel through a low anteromedial portal. These authors found that no lateral structures were at risk when drilling the posterolateral femoral tunnel in 120° of knee flexion [28]. These findings were contrary to what we have seen anecdotally utilizing an accessory medial portal (Fig. 1). Our accessory medial portal is situated more medial than the low anteromedial portal described by Neven et al. [28]. We hypothesized that a more medial accessory medial portal would cause the guide pin to exit at an even more lateral position on the distal femur, potentially placing the lateral structures there at risk. Furthermore, these authors did not evaluate which structures would be a risk with placement and preparation of the anteromedial bundle femoral tunnel.
At 90° of flexion, both the anteromedial bundle and posterolateral bundle guide pins were situated extremely close to the posterior articular cartilage border of the lateral femoral condyle. Larger diameter tunnels drilled in this position would potentially violate the articular surface in this area. Furthermore the subchondral location of this tunnel (Fig. 1) may have deleterious consequences with respect to subchondral collapse of the femoral condyle. Increasing knee flexion moves both guide pins to a more anterior position on the distal femur. The increased anterior positioning moves each pin farther away from the articular cartilage border. With increasing knee flexion (110 and 130°), the anteromedial bundle guide pin lies far from all major anatomic structures on the lateral aspect of the knee. The posterolateral bundle guide pin lies close to the origin of the lateral head of the gastrocnemius tendon at 110° of flexion. At 130° of hyper-flexion, the posterolateral bundle guide pin lies closest to lateral collateral ligament femoral attachment. No other lateral structures were in jeopardy. The surgeon should be aware of the proximity of the posterolateral bundle guide pin to the gastrocnemius origin and lateral collateral ligament femoral attachment at 110 and 130°, respectively. Considering these close anatomic relationships, violation of the lateral femoral cortex during drilling of the posterolateral bundle femoral tunnel should be avoided as injury to the gastrocnemius and lateral collateral ligament femoral attachments may occur.
This study has a few weaknesses. The first weakness is the use of an arthrotomy for pin placement rather than an arthroscopic portal. Multiple authors have also utilized this technique for anterior cruciate ligament anatomic studies [12, 31]. We felt this was the best way to standardize pin placement. Rather than utilizing a potentially displaceable soft tissue portal for pin placement, we elected to use bony landmarks (medial femoral condyle and tibial plateau) to truly standardize pin placement. This is our technique for portal placement intraoperatively. The second weakness is the small sample size. Even with a larger sampling of cadaveric knees, we still expect that guide pins will exit at the lateral cortex of the distal femur, in the vicinity of several important lateral structures.
Conclusion
At low knee flexion angles multiple lateral structures are at risk during preparation of both the anteromedial and posterolateral bundle femoral tunnels when using an accessory medial arthroscopic portal. Utilizing higher flexion angles increases the margin of error when preparing both femoral tunnels, particularly if the lateral cortex is violated with the reamer. During preparation of the anterior cruciate ligament femoral tunnel through an accessory anteromedial portal the tunnels should be drilled in at least 110° of knee flexion in order to decrease the risk of injury to important lateral knee structures if blow-out of the lateral cortex should occur.
References
Arnold MP, Koolos J, Kampen AV (2001) Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 9:194–199
Basdekis G, Abisafi C, Christel P (2008) Influence of knee flexion angle on femoral tunnel characteristics when drilled through the anteromedial portal during anterior cruciate ligament reconstruction. Arthroscopy 24:459–464
Chhabra A, Starman JS, Ferretti M, Vidal AF, Zantop T, Fu FH (2006) Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. J Bone Joint Surg Am 88:2–10
Edwards TB, Guanche CA, Petrie SG, Thomas KA (1999) In vitro comparison of elongation of the anterior cruciate ligament and single- and dual-tunnel anterior cruciate ligament reconstructions. Orthopedics 22:577–584
Farrow LD, Chen MR, Cooperman DR, Goodfellow DB, Robbin MS (2008) Radiographic classification of the femoral intercondylar notch posterolateral rim. Arthroscopy 24:1109–1114
Farrow LD, Chen MR, Cooperman DR, Victoroff BN, Goodfellow DB (2007) Morphology of the femoral intercondylar notch. J Bone Joint Surg Am 89:2150–2155
Farrow LD, Gillespie RS, Victoroff BN, Cooperman DR (2008) Radiographic location of the lateral intercondylar ridge. Am J Sports Med 36:2002–2006
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23:1218–1225
Fu FH, Jordan SS (2007) The lateral intercondylar ridge—a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg Am 89:2103–2104
Fu FH, Shen W, Starman JS, Okeke N, Irrgang JJ (2008) Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med 36:1263–1274
Girgis FG, Marshall JL, Monajem A (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res 106:216–231
Giron F, Buzzi R, Aglietti P (1999) Femoral tunnel position in anterior cruciate ligament reconstruction using three techniques. A cadaver study. Arthroscopy 15:750–756
Giron F, Cuomo P, Edwards A, Bull AM, Amis AA, Aglietti P (2007) Double-bundle “anatomic” anterior cruciate ligament reconstruction: a cadaveric study of tunnel positioning with a transtibial technique. Arthroscopy 23:7–13
Golish SR, Baumfield JA, Schoderbek RJ, Miller MD (2007) The effect of femoral tunnel starting position on tunnel length in anterior cruciate ligament reconstruction: a cadaveric study. Arthroscopy 23:1187–1192
Harner CD, Honkamp NJ, Ranawat AS (2008) Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy 24:113–115
Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE (2008) Reconstruction technique affects femoral tunnel placement in anterior cruciate ligament reconstruction. Clin Orthop Relat Res 466:1467–1474
LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32:1405–1414
LaPrade RF, Ly TV, Wentorf FA, Engebretsen L (2003) The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med 31:854–860
Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H, Kim CH (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23:771–778
Liu R, Farrow LD, Messerschmitt P, Cooperman DR, Gilmore A, Goodfellow DB (2008) Anatomical study of the pediatric intercondylar notch. J Pediatr Orthop 28:177–183
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between the 11 o’clock and 10 o’clock femoral tunnel placement. Arthroscopy 19:297–304
Lubowitz JH (2009) Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy 25:95–101
Mae T, Shino K, Miyama T, Shinjo H, Ochi T, Yoshikawa H, Fujie H (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy 17:708–716
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421
Mochizuki T, Muneta T, Nagase T, Shirasawa S, Akita KI, Sekiya I (2006) Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:356–361
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Nakagawa T, Takeda H, Nakajima K, Nakayama S, Fukai A, Kachi Y, Kawano H, Miura T, Nakamura K (2008) Intraoperative 3-dimensional imaging-based navigation assisted anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:1161–1167
Neven E, D’Hooghe P, Bellemans J (2008) Double-bundle anterior cruciate ligament reconstruction: a cadaveric study on the posterolateral tunnel position and safety of the lateral structures. Arthroscopy 24:436–440
Norwood LA, Cross MJ (1977) The intercondylar shelf and the anterior cruciate ligament. Am J Sports Med 5:171–176
O’Donnell JB, Scerpella TA (1995) Endoscopic anterior cruciate ligament reconstruction: modified technique and radiographic review. Arthroscopy 11:577–584
Petersen W, Tretow H, Weimann A, Herbort M, Fu FH, Raschke M, Zantop T (2007) Biomechanical evaluation of two techniques for double-bundle anterior cruciate ligament reconstruction. One tibial tunnel versus two tibial tunnels. Am J Sports Med 35:228–234
Petersen W, Zantop T (2006) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Purnell ML, Larson AI, Clancy W (2008) Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med 28:2083–2090
Rue JH, Ghodadra N, Bach BR (2008) Femoral tunnel placement in single-bundle anterior cruciate ligament reconstruction: a cadaveric study relating transtibial lateralized femoral tunnel position to the anteromedial and posterolateral bundle femoral origins of the anterior cruciate ligament. Am J Sports Med 36:73–79
Scranton PE, Pinczewski L, Auld KM, Khalfayan EE (1996) Outpatient endoscopic quadruple hamstring anterior cruciate ligament reconstruction. Oper Tech Orthop 6:177–180
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Sohn DH, Garrett WE (2009) Transitioning to anatomic anterior cruciate ligament graft placement. J Knee Surg 22:155–160
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Zantop T, Petersen W, Sekiya JK, Musahl V, Fu FH (2006) Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc 14:982–992
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farrow, L.D., Parker, R.D. The relationship of lateral anatomic structures to exiting guide pins during femoral tunnel preparation utilizing an accessory medial portal. Knee Surg Sports Traumatol Arthrosc 18, 747–753 (2010). https://doi.org/10.1007/s00167-009-0902-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0902-1