Abstract
It is not well known how much tension should be applied to ACL graft at the time of graft fixation. As a step to determine the optimal initial tension, it is indispensable to know the graft tension to restore normal anterior–posterior (A–P) laxity (laxity match pretension, LMP). The objective was to determine the LMP in ACL reconstruction for the anatomical two-bundle technique and for the Rosenberg’s isometric bi-socket one, and to compare these two techniques in LMP. Twenty-four patients with unilateral chronic ACL insufficiency were divided into the following two groups. The anatomical two-bundle technique was performed on 12 patients via two femoral tunnels at 9 and 10 o’clock or 2 and 3 o’clock on the posterior margin of the notch and two tibial tunnels (Group A), while the Rosenberg’s isometric bi-socket reconstruction was performed on the remaining 12 patients through two femoral tunnels at 10 and 11 o’clock or 1 and 2 o’clock and one wider tibial tunnel (Group B). After two doubled semitendinosus grafts were fixed with two EndoButton-CL®s on the femur, they were temporarily fixed to the tension-adjustable force gauge on the tibia, respectively. The total tension applied to grafts was set at 10, 20, 30, 40, or 50 N at 20° of knee flexion, and the A–P laxity was measured by applying A–P drawer load of 134 N at 20° of flexion. By comparing the measured laxity with that for the opposite healthy knee, the tension to restore the normal A–P laxity (LMP) was estimated. The mean LMP of 7.3 N in Group A was significantly smaller than that of 25.8 N in Group B. The anatomical two-bundle technique makes it possible to more effectively restore A–P stability with lower initial tension than the isometric Rosenberg’s bi-socket reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ACL reconstruction is one of the most frequently performed operations in the current orthopedic practice. To restore normal knee kinematics, the anatomical graft placement has recently been advocated. We did start performing the modified Rosenberg’s isometric bi-socket technique in 1995, using autogenous hamstring tendons and creating two femoral sockets at 1 and 2 o’clock or 10 and 11 o’clock in the posterior margin of the notch around the superior margin of ACL femoral footprint [12, 13]. However, Toritsuka et al. [16] reported that the graft-PCL impingement leading to loosening of the graft was observed in some cases via isometric bi-socket technique, as the grafts reconstructed with this technique were considered to be different from the normal ACL. We have then established the technique “the anatomical two-bundle ACL reconstruction” in 2001, in which two tunnels in the femur and the tibia are separately created in the central area of the footprints of ACL [14]. However, there are still some unsolved problems such as an initial tension.
About the initial tension at the time of graft fixation, Fleming et al. [5] reported that there was corresponding decrease in anterior–posterior (A–P) laxity with an increment of initial tension, while there were few reports about the adequate initial tension to the graft in ACL reconstruction. Yasuda et al. [18] divided ACL-reconstructed patients into three different initial graft tension groups (20, 40, and 80 N) and observed for 2 or more years. They suggested that relatively high initial tension (up to 80 N) reduced the postoperative anterior laxity of the knee joint after ACL reconstruction in single-socket technique. Thus, it is the important theme to decide the initial tension at the graft fixation in ACL reconstruction. However, the initial tension in ACL reconstruction was applied clinically by manual maximum pull at most institutes, and no quantitative data on the tension have been available. Recently, Double Spike Plate (DSP)® (Meira Co. Ltd., Nagoya, Japan) to fix a graft at predetermined initial tension in a clinical setting has become available [15]. However, the ideal initial tension is still unknown, while the initial tension applied to a graft is considered one of the key factors for success in ACL reconstruction [3–5, 10]. As a step to determine the ideal tension, it is indispensable to estimate the tension to restore the normal (A–P) laxity (laxity match pretension, LMP). There are some previous reports about the LMP, while the data in all these reports were obtained from the reconstruction via a single femoral socket/tunnel technique in cadaveric knees [2, 8, 17]. Therefore, the purposes of this study were to determine the LMP in ACL reconstruction using quadrupled hamstring tendons via the isometric bi-socket technique or the anatomical two-bundle one in the operating theatre, and to compare these two ACL reconstruction techniques in LMP.
Materials and methods
Twenty-four patients with unilateral chronic ACL injury, who had consented to be involved in this study, were included. Their age ranged from 16 to 39 years, with a mean of 26.9 years. There were 15 males and 9 females. The interval from injury to ACL reconstruction was 87.3 ± 44.5 days. Intraoperatively, their ACLs were found completely torn. Thirteen cases also had tear to the medial meniscus, and nine had tear to the lateral meniscus. In those with medical meniscal tear, nine knees underwent meniscal repair, three did menisectomy, and one did rasping without repair. In the cases with lateral meniscal tear, four knees underwent meniscal repair, two did menisectomy, and three did rasping. There was neither other ligament injury nor severer articular cartilage damage than Grade II; fissuring or fibrillation less than one-half the thickness of the articular cartilage. These cases were randomly divided into the following two groups and had ACL reconstruction with either of the two different techniques under arthroscopy (Table 1). The one surgeon (TM) performed 20 ACL reconstructions and assisted all the other surgeries.
Anatomical two-bundle ACL reconstruction (Group A) (12 cases: eight males and four females)
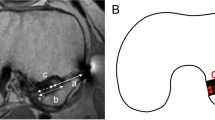
Using an antero-lateral entry femoral aimer (Smith & Nephew Inc. Endoscopy, Andover, MA, USA), a 2.4 mm guide wire was inserted from outside of the lateral cortex of the femur to the supero-posterior portion of the posterolateral bundle (PLB) footprint (5 mm anterior to the posterior margin at 9 or 3 o’clock of the notch). Then a 5.0–6.0 mm tunnel was created for the posterolateral graft (PLG) by over-drilling. Similarly, another 2.4 mm guide wire was inserted from the lateral femoral cortex to the supero-posterior portion of the anteromedial bundle (AMB) footprint (5 mm anterior to the posterior margin at 10 or 2 o’clock of the notch). Then a 5.0–6.0 mm tunnel was created for the anteromedial graft (AMG) by over-drilling. For the tibia, two guide wires were inserted in parallel from the medial tibial cortex to the center of AMB and PLB footprints with a drill guide system (Smith & Nephew Inc. Endoscopy), and then two 5.0–6.0 mm tunnels were created by over-drilling (Fig. 1a–c).
Position of femoral tunnels in the anatomical two-bundle technique. Two femoral tunnels were created at 9 and 10 o’clock or 2 and 3 o’clock on the posterior margin of the lateral femoral condyle. a A diagram of femoral tunnels. b Femoral tunnels viewed arthroscopically through antero medial portal. c X-ray for lateral view
Rosenberg’s bi-socket technique (Group B) (12 cases: seven males and five females)
Using the tibial drill guide system, a 2.4 mm guide wire was inserted from the tibial cortex medial to the tibial tubercle to the center of the ACL footprint. Then a single tibial tunnel of 8.0–9.0 mm was created by over-drilling. Next, through the tibial tunnel, a 2.4 mm guide wire was inserted at the superior margin of the femoral ACL footprint on the lateral wall of the intercondylar notch (5 mm anterior to the posterior margin at 11 or 1 o’clock of the notch). Then a 5.5–6.0 mm socket was created for the AMG with 25 mm in depth by over-drilling followed by over-drilling to the anterolateral femoral cortex with a 4.5 mm drill. Similarly the femoral socket/tunnel for the PLB with a diameter of 4.5–5.5 mm was created at the ACL footprint in the direction of 10 or 2 o’clock (Fig. 2a, b).
Graft preparation and fixation
In both techniques, previously harvested semitendinosus tendon was transected in half and then folded to make a pair of doubled grafts. First, EndoButton-CL® (Smith & Nephew Inc. Endoscopy) of appropriate length based on the femoral tunnel length was placed to the loop end of the graft, and two no. 3 polyester threads were whip-stitched to the free end of each doubled graft. Each graft was introduced through the tibial tunnels to the femoral tunnels and fixed on the lateral femoral cortex by turning EndoButton®s. In the anatomical two-bundle ACL reconstruction, though the straight 5.0–6.0 mm femoral tunnels were created in outside-in fashion in spite of recommended channel of 4.5 mm for Endo-Button® fixation, the grafts were safely fixed on the lateral side of femoral cortex with Endo-Button®s. Then, the graft sutures of the two grafts were separately tied to two tension-adjustable force gauges fixed on the tibial cortex around the exit of the tunnel.
Measurement of LMP
First, a total of 10 N of initial tension, 5 N to each graft, was applied using the force gauge on the tibial cortex at 20° of knee flexion after load relaxation for 5 min (Fig. 3). Then the A–P displacement of the tibia was measured with Knee Laxity Tester® (Stryker, USA) when an A–P load of 134 N was applied at the same knee position. Similarly, the total tension of 20, 30, 40, or 50 N to the graft was applied as the pretension at 20° of knee flexion for each trial in the same manner. Then A–P displacement measurement was repeated. The A–P displacement of the uninjured opposite knee was also measured. All measurements were completed by the same examiners for all tests to reduce variability. The initial tension and A–P displacement were plotted on a graph. The LMP for each patient was estimated from the A–P displacement of the uninjured opposite tibia, based upon the assumption that the initial tension and A–P displacement are inversely proportional. Actually the average of the correlation coefficient between the initial tension and A–P displacement was − 0.956 ± 0.04 (Fig. 4).
For the statistical analysis, Mann–Whitney’s U test was used, and P values equal to or less than 0.05 were considered statistically significant.
Results
In Group A, the mean A–P displacement was 12.3, 10.2, 8.8, 8.0, and 6.0 mm when the initial tension was set at 10, 20, 30, 40, and 50 N, respectively, while that on the opposite uninjured knee was 12.5 mm. In Group B, the mean A–P displacement was 14.7, 13.8, 12.8, 11.5, and 10.2 mm at each initial tension, respectively, while that on the opposite uninjured knee was 13.2 mm (Fig. 5a, b).
The estimated LMP values for each patient were between 2.2 and 14 N in Group A, while those varied from 6.2 to 52.3 N in Group B (Fig. 6). The mean estimated LMP of 7.3 ± 4.2 N in Group A was significantly lower than that of 25.8 ± 11.2 N in Group B.
Discussion
The optimal initial tension applied to the graft in the ACL reconstruction is still unclear. Considering load relaxation to the graft following its fixation and its remodeling process, the tension greater than LMP should be applied. However, excessive tension may make the joint stiffness abnormal, hinder flexion–extension, promote graft failure, or lead to degeneration of the articular cartilage [1, 10, 11, 19]. Yoshiya et al. [19] compared microangiography and histology at 3 months after anterior cruciate ligament reconstruction in dogs with a tension of 1 N to those with a tension of 39 N, and reported that the grafts under excessive tension of 39 N underwent focal degeneration and that the collagen fibers within them were replaced by mucoid extra-cellular matrix. In microangiography, they also reported that improved vascularity was found when the initial tension was 1 N rather than 39 N. On the other hand, insufficient initial tension to the graft would lead to loose knees. Therefore, the LMP could be assumed to serve as the reference point at the time of deciding the optimal initial tension, and its investigation is unquestionably important.
There are several previously reported studies on LMP. Burks and Leland [2] reported the LMP to be 37 N in the single-socket technique using doubled hamstring tendons, and Woo et al. [17] reported that of 45 N in the single-socket technique using quadrupled hamstring tendons. In the results obtained from this study, the mean LMP was 25 N in the isometric bi-socket technique and 7.8 N in the anatomical two-bundle technique, respectively. The latter was especially close to the in situ force of the normal ACL at 20° of flexion reported by Markolf et al. [7]. The LMP obtained in this study were smaller than those in previous studies done on cadavers, although the conditions of the experiments were different. This may suggest that these two techniques used in this study are biomechanically superior to those in the previous reports, because smaller amount of LMP was required to restore the normal laxity.
Then, comparing the two-bundle techniques in LMP value, the LMP in the anatomical two-bundle ACL reconstruction was significantly lower than that in the isometric bi-socket technique. Thus, the former technique is considered more effective in restoring stability of the knee. The possible explanations are as follows: (1) location of the femoral sockets/tunnels; (2) number of the tibial tunnels; (3) the distance between the fixation points.
For the location of the femoral sockets/tunnels, our tunnels were created at 9 and 10 o’clock or 2 and 3 o’clock on the posterior margin of the notch or in the central area of the ACL footprint in order to mimic fiber orientation of the natural ACL in knee extension, while the sockets were created at 10 and 11 o’clock or 1 and 2 o’clock in the isometric bi-socket technique. There are some previously reported studies on the location of the femoral sockets. Loh et al. [6] reported when the 10 and 11 o’clock locations of the femoral sockets were compared in single-socket ACL reconstruction using bone-patellar tendon-bone graft, the socket at 10 o’clock was superior in terms of rotation, but there was no difference in anterior stability. Markolf et al. [9] also reconstructed using the similar technique and compared the location of the femoral sockets at 10, 11, and 12 o’clock, and reported no difference among the three groups in the displacement when 100 N of force was applied anteroposteriorly or in LMP. However, these reports were based on reconstructions achieved by the single-socket technique, which was quite different from the two-bundle techniques used in this study. Furthermore, there were no investigations on the lower femoral tunnel locations such as 3 or 9 o’clock. It could be assumed from our results that the graft in the lower femoral tunnel had somewhat affect on the anterior stability.
As for the number of the tibial tunnels, two tunnels are made at the ACL footprint in the anatomical two-bundle technique, while there is only one tibial tunnel in the isometric bi-socket one. At the time of anterior drawer force applied to the tibia in the bi-socket technique, the posteriorly positioned bundle first is pushed by the posterior wall of the tunnel, and then the anteriorly positioned bundle indirectly carries the load via the posteriorly positioned bundle. On the other hand, in the anatomical two-bundle ACL reconstruction, both bundles have tunnel walls posteriorly and can directly carry the load via the bony wall. Thus, the anatomical two-bundle technique could more efficiently perform to control the anterior stability than the bi-socket one.
Finally, for the distance between the fixation points, the femoral tunnels in the anatomical two-bundle technique were created from outside of the lateral cortex or the femur using an antero-lateral entry femoral aimer, while those in the bi-socket technique were made through the tibial tunnel. Thus, because of the different technique in creation of the femoral tunnels and the difference in the direction of the femoral tunnels, the length of the femoral tunnels was shorter in the anatomical two-bundle technique than in the bi-socket technique. And as the location of the femoral tunnels was lower in the anatomical two-bundle technique than in the bi-socket technique, the length of the grafts in the joint and consequently the distance between the fixations were also shortened in the anatomical two-bundle technique. Therefore, as the stress relaxation of the graft–suture complex was reduced and the force transmission to grafts became more efficiently against the anterior drawer force, graft force to restore normal laxity was needed to be smaller in this technique.
For these reasons mentioned above, we may conclude that the anatomical two-bundle ACL reconstruction is more effective in achieving stability of the knee equivalent to the uninjured knee with lower LMP. Since this study was performed during surgery under anesthesia using the opposite knee as the control, the accuracy of the measurements may be inferior to the previous studies using cadaveric knees. However, this is the first study to obtain LMP in vivo, and these data may be more clinically useful since they included the muscles and soft tissues around the knees. The data obtained in this study would contribute to improvement of the surgical outcome.
Conclusion
The mean graft tension to restore normal A–P laxity (LMP) was 7.3 N in the anatomical two-bundle technique and 25.8 N in the isometric bi-socket one. The “anatomical” two-bundle ACL reconstruction technique makes it possible to stabilize the knee with lower initial tension.
References
Arms SW, Pope MH, Johnson RJ (1990) Analysis of ACL failure strength and initial strains in the canine model. Trans Orthop Res Soc 15:524
Burks RT, Leland R (1988) Determination of graft tension before fixation in anterior cruciate ligament reconstruction. Arthroscopy 4:260–266
Bylski-Austrow DI, Grood ES, Hefzy MS, Holden JP, Butler DL (1990) Anterior cruciate ligament replacements: a mechanical study of femoral attachment location, flexion angle at tensioning, and initial tension. J Orthop Res 8:522–531
Eagar P, Hull ML, Howell SM (2004) How the fixation method stiffness and initial tension affect anterior load-displacement of the knee and tension in anterior cruciate ligament grafts: a study in cadaveric knees using a double-loop hamstrings graft. J Orthop Res 22:613–624
Fleming B, Beynnon B, Howe J, McLeod W, Pope M (1991) Effect of tension and placement of a prosthetic anterior cruciate ligament on the anteroposterior laxity of the knee. J Orthop Res 10:177–186
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: Comparison between 11 o’clock and 10 o’clock femoral tunnel placement. Arthroscopy 19:297–304
Markolf KL, Gorek JF, Kabo M, Shapiro MS (1990) Direct measurement of resultant forces in the anterior cruciate ligament. J Bone Joint Surg Am 72:557–567
Markolf KL, Burchfield DM, Shapiro MM, Davis BR, Finerman G, Slauterbeck JL (1996) Biomechanical consequences of replacement of the anterior cruciate ligament with a patellar ligament allograft. Part 1: insertion of the graft and anterior–posterior testing. J Bone Joint Surg Am 78:1720–1727
Markolf KL, Hame S, Hunter DM, Oakes DA, Zoric B, Gause P, Finerman GA (2002) Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 20:1016–1024
Melby A III, Noble JS, Askew MJ, Boom AA, Hurst FW (1991) The effects of graft tensioning on the laxity and kinematics of the anterior cruciate ligament reconstructed knee. Arthroscopy 7:257–266
O’Donoghue DH, Rockwood CCA Jr, Frank GR, Jack SC, Kenyon R (1966) Repair of the anterior cruciate ligament in dogs. J Bone Joint Surg 48-A:503–519
Rosenberg TD, Graf B (1994) Techniques for ACL reconstruction with Multi-Trac drill guide. Acufex Microsurgical Inc., Mansfield
Rosenberg TD, Brown GC, Deffner KT (1997) Anterior cruciate ligament reconstruction with a quadrupled semitendinosus autograft. Sports Med Arthrosc Rev 5:51–58
Shino K, Horibe S, Hamada M, Nakamura N, Nakata K, Mae T, Toritsuka Y (2002) Allograft anterior cruciate ligament reconstruction. Tech Knee Surg 1:78–85
Shino K, Mae T, Maeda A, Miyama T, Shinjo H, Kawakami H (2002) Graft fixation with predetermined tension using a new device, the double spike plate. Arthroscopy 18:908–911
Toritsuka Y, Shino K, Horibe S, Mitsuoka T, Hamada M, Nakata K, Nakamura N, Yoshikawa H (2004) Second-look arthroscopy of anterior cruciate ligament grafts with multistranded hamstring tendons. Arthroscopy 20:287–293
Woo SL, Fox RJ, Sakane M, Livesay GA, Rudy TW, Runco TJ, Li G, Allen CR, Fu FH (1997) Force and force distribution in the anterior cruciate ligament and its clinical implications. First place winner of the inaugural GOTS-Beiersdorf Research Award competition for Sports Medicine. Sportorthopadic-Sporttaumatologie 13:37–48
Yasuda K, Tsujino J, Tanabe Y, Kaneda K (1997) Effects of initial graft tension on clinical outcome after anterior cruciate ligament reconstruction. Autogenous doubled hamstring tendons connected in series with polyester tapes. Am J Sports Med 25:99–106
Yoshiya S, Andrish JT, Manley MT, Bauer TW (1987) Graft tension in anterior cruciate ligament reconstruction. An in vivo study in dogs. Am J Sports Med 15:464–470
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mae, T., Shino, K., Matsumoto, N. et al. Anatomical two-bundle versus Rosenberg’s isometric bi-socket ACL reconstruction: a biomechanical comparison in laxity match pretension. Knee Surg Sports Traumatol Arthrosc 15, 328–334 (2007). https://doi.org/10.1007/s00167-006-0172-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0172-0