Abstract
The main therapeutic agent for gastroesophageal reflux disease (GERD) is a proton pump inhibitor (PPI). Plasma levels and the acid inhibitory effect of PPIs depend on the activity of cytochrome P450 (CYP) 2C19, which is polymorphic. Genotypes of CYP2C19 are classified into three groups: rapid metabolizers (RMs: *1/*1), intermediate metabolizers (IMs: *1/*X), and poor metabolizers (PMs: *X/*X), where *1 and X represent the wild type and the mutant allele, respectively. RMs include ultra-rapid metabolizers, who possess the CYP2C19*17 allele. The pharmacokinetics and pharmacodynamics of PPIs differ among different CYP2C19 genotype groups. Plasma PPI levels and intragastric pH values during PPI treatment are lowest in the RM group, intermediate in the IM group, and highest in the PM group. These CYP2C19-genotype-dependent differences in the pharmacokinetics and pharmacodynamics of PPIs influence the healing and recurrence of GERD during PPI treatment, suggesting the need for CYP2C19 genotype-based tailored therapy for GERD. CYP2C19 pharmacogenetics should be taken into consideration for the personalization of PPI-based therapy. However, the clinical usefulness of CYP2C19 genotype testing in GERD therapy should be verified in clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Introduction
Gastroesophageal reflux disease (GERD) is a common disorder estimated to affect approximately 35–40% of the adult population in the Western world.[1] GERD now represents a major indication for proton pump inhibitors (PPIs). However, there seem to be some patients who do not respond to the usual daily dose of a PPI (e.g. omeprazole 20 mg or lansoprazole 30 mg).[2,3] Therefore, it is of clinical importance to develop an optimal therapeutic strategy for GERD patients who are refractory to a PPI at the standard dose.
PPIs are substituted benzimidazoles and are mainly metabolized by the cytochrome P450 (CYP) system in the liver. The principal enzyme involved in the metabolism of PPIs is CYP2C19, though CYP3A4 is also involved in PPI metabolism.[4–8] There are interindividual differences in the activity of CYP2C19, and the pharmacokinetics and pharmacodynamics of PPIs are influenced by CYP2C19 genetic polymorphism.
Herein, we describe and discuss the influence of CYP2C19 genetic polymorphism on the pharmacokinetics and pharmacodynamics of PPIs and on clinical outcomes of PPI-based therapies for GERD. We also discuss the prospects for CYP2C19 genotype-based personalized treatment of GERD.
2. Effects of CYP2C19 Polymorphism on the Pharmacokinetics and Pharmacodynamics of Proton Pump Inhibitors (PPIs)
2.1 Genetic Differences in the PPI-Metabolizing Enzyme CYP2C19
CYP2C19 is involved in the first step of metabolism of all PPIs (figure 1).[9,10] Because the metabolites of PPIs (such as 5-hydroxyomeprazole and omeprazole sulfone) have no acid-inhibitory effect, the therapeutic effect depends on plasma levels of the PPIs, which are determined by the activity of CYP2C19. There are genotypic differences that affect the activity of CYP2C19. Various genetic mutations involved in CYP2C19 polymorphism have been discovered in ethnically different populations.[11] However, interindividual differences in the activity of CYP2C19 can be explained by the combination of two point mutations, CYP2C19 *2 of exon 5 and CYP2C19 *3 of exon 4, in most cases.[12–14] The phenotypes resulting from polymorphism of this enzyme are generally classified into three genotype groups: rapid metabolizers (RMs: *1/*1), intermediate metabolizers (IMs: *1/*X), and poor metabolizers (PMs: *X/*X), where *1 represents the wild-type allele and *X represents the mutated allele. The nomenclature of genotype groups of CYP2C19 varies in the literature; for example, CYP2C19 genotype groups are classified into extensive metabolizers (EMs), IMs, and PMs in some papers.[15–17] However, in many important papers on CYP2C19,[18–38] the classification of EMs has included both *1/*1 homozygotes and *1/*X heterozygotes (= IMs), therefore, usage of the term ‘EM’ as the genotype of *1/*1 may be confusing. Accordingly, to avoid confusion for readers, the term ‘RMs’, rather than ‘EMs’, is used to denote homozygotes of CYP2C19 *1/*1 in this paper.
CYP2C19 *2 is a single base-pair mutation from guanine to adenine in exon 5 of CYP2C19, which creates a truncated nonfunctional protein. This defect accounts for approximately 75–83% of the PM allele in both Japanese and Caucasian subjects.[14] CYP2C19 *3 is a mutation from guanine to adenine at position 636 of exon 4 of CYP2C19, which creates a premature stop codon.[12] The frequencies of RMs, IMs, and PMs of this enzyme differ among different ethnic groups, with the incidence of PMs being higher in Asians than in Caucasians and Africans.[13,39–41] The CYP2C19 *3 allele is absent in Caucasians; in this ethnic group, the PM phenotype is mainly attributed to the CYP2C19 *2 allele alone. Representative frequencies of phenotypes and alleles in different ethnic groups are summarized in table I.
CYP2C19 *17 has been found to be associated with the ultra-rapid metabolizer (UM) phenotype of CYP2C19 (*17/*17 homozygotes).[45] There are ethnic difference in the frequency of this allele.[42,43,46] The allele frequency of CYP2C19 *17 is around 18% in Swedes and Ethiopians, but is only 4.4% in Chinese and 1.3% in Japanese populations (table I).[44,45]
2.2 Effect of CYP2C19 Polymorphism on the Pharmacokinetics of PPIs
When omeprazole 20 mg, lansoprazole 30 mg, or rabeprazole 20 mg are given, plasma concentrations of the three PPIs differ among the three different CYP2C19 genotype groups (RMs, IMs, and PMs) [figure 2a].[47] Plasma omeprazole levels in the PM group are sustained for a long time after dosing. The mean value for the area under the plasma concentration-time curve of omeprazole in the PM group is about 13 times as high as that in the RM group (table II). Similar CYP2C19 genotype-dependent differences in plasma PPI levels are observed with other PPIs such as lansopazole, rabeprazole, and esomeprazole (figure 2a and 2b, and table II).[22,47–50] Although there are some differences in individual PPIs, the plasma levels of all PPIs are generally influenced by CYP2C19 genotypic differences.
Influence of CYP2C19 polymorphism on the pharmacokinetics of omeprazole, lansoprazole, and rabeprazole. Plasma concentrations of the three proton pump inhibitors were highest in the poor metabolizer group, intermediate in the intermediate metabolizer group, and lowest in the rapid metabolizer group. (Adapted from Shirai et al.[48] and Furuta et al.,[49] with permission.)
There have been conflicting data on the influence of CYP2C19*17 on the pharmacokinetics of PPIs.[51–55] The CYP2C19 *17 allele was first reported to be associated with ultra-rapid metabolism of a PPI in a Swedish group.[45,51] However, more recent reports from different institutions have indicated that CYP2C19 *17-associated differences in pharmacokinetics of PPIs are not significant.[52,53] A meta-analysis[56] of the impact of CYP2C19 *17 on the clinical outcomes of PPIs has indicated that the clinical impact of CYP2C19 *17/*17 is almost the same as that of CYP2C19 *1/*1, although CYP2C19 *17 is associated with an increased risk of bleeding in patients treated with clopidogrel.[42,57] Therefore, in contrast to data relating to clopidogrel, recent data have indicated that assignment of CYP2C19 *17 homozygotes as UMs, rather than RMs or EMs, is inadequate in the clinical setting of PPIs. Further accumulation of data is needed on the influence of the CYP2C19 *17 allele on clinical outcomes of acid-related disorders treated with PPIs.
2.3 Effect of CYP2C19 Polymorphism on Gastric Acid Inhibition with PPIs
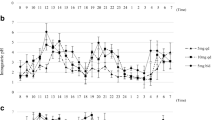
Because plasma levels of PPIs differ among different CYP2C19 genotype groups, the intragastric pH profiles also differ when a PPI (e.g. omeprazole 20 mg, lansoprazole 30 mg, or rabeprazole 20 mg) is administered (figure 3). The mean 24-hour intragastric pH is lowest in the RM group, intermediate in the IM group, and highest in the PM group.[47] The acid inhibition achieved by omeprazole, lansoprazole, or rabeprazole in the RM group is likely to become insufficient under the so-called standardized dosing scheme (table III).[47,59]
(–c) Profiles of intragastric pH values as a function of CYP2C19 genotype status on day 7 for once-daily dosing of () omeprazole 20 mg, (b) lansoprazole 30 mg, and (c) rabeprazole 20 mg. Because intragastric pH is influenced by food, the timings of meals are indicated on the graphs. (d) Influence of CYP2C19 polymorphism on the mean 24-hour intragastric pH achieved by the different proton pump inhibitors. There were CYP2C19-phenotype-dependent differences in the mean 24-hour intragastric pH achieved by omeprazole and lansoprazole, but not rabeprazole. (Adapted from Shirai et al.[48] and Furuta et al.,[49] with permission.)
Several studies have analyzed whether the CYP2C19 genotype influences the acid inhibition achieved by PPIs. For omeprazole, reports have shown that the acid inhibition achieved by once-daily dosing of 10 mg, 20 mg, or 40 mg was influenced by the CYP2C19 genotype.[38,47,48,60–66] The acid inhibition achieved by once-daily dosing of esomeprazole 20 mg or 40 mg was also influenced by the CYP2C19 genotype,[22,61,67,68] although dosing of 10 mg 4 times daily or 20 mg twice daily was not.[22] The acid inhibitory effect of lansoprazole 15 mg or 30 mg once daily was shown to depend on the CYP2C19 genotype,[49,58,60,69,70] as was once-daily rabeprazole (10 mg and 20 mg) in most[26,60,65,67,68,71–76] but not all reports.[29,48,70] Interestingly, rabeprazole 10 mg twice daily was shown not to be influenced by the CYP2C19 genotype status.[73] Thus, although the acid inhibition achieved by PPIs administered once daily appears to be influenced by the CYP2C19 genotype, divided or frequent dosing seems to minimize the influence of CYP2C19 genotypic differences.
2.4 Other Polymorphisms Associated with the Pharmacokinetics and Pharmacodynamics of PPIs
Because PPIs are absorbed from the small intestine, genetic polymorphism of the transporter of PPIs affects the pharmacokinetics and pharmacodynamics of these drugs. P-glycoprotein, an enzyme coded by the ATP-binding cassette, sub-family B (MDR/TAP), member 1 gene (ABCB1; previously known as multidrug resistance transporter gene 1 [MDR1]) is associated with absorption of PPIs from the small intestine, and is polymorphic. Kodaira et al.[77] studied the influence of the ABCB1 3435C/T polymorphism on the pharmacokinetics and pharmacodynamics of lansoprazole in Japanese subjects and found that the plasma levels of lansoprazole were higher in subjects with the ABCB1 3435 TT genotype than in those with the CT or CC genotypes. However, there was no significant difference in the acid inhibition achieved by lansoprazole among different ABCB1 3435C/T genotype groups. They concluded that the influence of ABCB1 polymorphism on the pharmacokinetics and pharmacodynamics of a PPI was smaller than that of CYP2C19 polymorphism and could be disregarded in the clinical setting.
CYP3A4 is also associated with the metabolism of PPIs.[78] However, genotypes associated with CYP3A4 activity have not been fully elucidated.
3. Effect of CYP2C19 Polymorphism on Gastroesophageal Reflux Disease (GERD) Treatment by PPIs
Because GERD healing rates depend on the levels of acid inhibition,[79] and because acid inhibition achieved by a PPI dosed once daily differs among different CYP2C19 genotypes, as noted above, the rates of healing of GERD by a PPI dosed once daily should theoretically be influenced by the CYP2C19 genotype status.
The influence of CYP2C19 genotypes on the rates of healing of GERD (erosive reflux esophagitis [RE] and non-erosive reflux disease [NERD]) has been evaluated in several studies. The clinical effect of some PPIs on RE were reported to depend on CYP2C19 genotypes when a PPI was dosed once daily (table IV).[80–82,85–87] For example, when lansoprazole 30 mg was administered for 8 weeks to GERD patients with mucosal breaks (grades A–D in the Los Angeles Classification),[88] the rate of healing of mucosal breaks was lowest in the RM group and highest in the PM group, with intermediate healing rates observed in the IM group. The rate of healing of mucosal breaks in patients with grade C or D GERD who carried a CYP2C19 RM genotype was dramatically low (1 of 6 patients [16.7%]; 95% CI 0.4, 64.1).[82] Similarly, Kawamura et al.[81] reported that the rate of healing of mucosal breaks in RM patients was the lowest among the three different CYP2C19 genotype groups when they were treated with lansoprazole 30 mg once daily. This study indicated that acid inhibition achieved by a daily dose of lansoprazole 30 mg in the PM genotype group is clinically sufficient for GERD treatment, but that in IMs and RMs this dose might be insufficient in some cases.
On the other hand, the influence of CYP2C19 polymorphisms on the rates of healing of GERD by rabeprazole and esomeprazole seems to differ from that observed with lansoprazole or omeprazole. Schwab et al.[83] reported that esomeprazole-induced healing of GERD was unrelated to the CYP2C19 genotype. Ariizumi et al.[84] reported that the therapeutic effects of rabeprazole 10 mg/day on RE were sufficient and were not influenced by CYP2C19 polymorphism (table IV). The involvement of CYP2C19 in the metabolism of rabeprazole and esomeprazole is relatively minor in comparison with its influence on the metabolism of omeprazole and lansoprazole, which might contribute to the lack of influence of CYP2C19 polymorphism on the GERD cure rates observed with rabeprazole or esomeprazole. Because the acid inhibitory potency of rabeprazole is higher than those of omeprazole and lansoprazole,[89] the plasma levels of rabeprazole achieved by RMs might be sufficient to inhibit acid secretion to the levels needed for GERD treatment.
Recurrence of RE during maintenance therapy with a PPI depends on CYP2C19 genotypes. The symptomatic recurrence rate in RE patients treated with lansoprazole 15 mg was lowest in RMs, and that in PMs was the highest of the three groups.[86] Kawamura et al.[85] reported that CYP2C19 genotypes influenced the remission of RE during maintenance therapy with lansoprazole. Saitoh et al.[87] reported that CYP2C19 genotypes affected the rate of recurrence of GERD symptoms during PPI maintenance therapy. Together, these studies suggest that initial and maintenance PPI therapy for RE is influenced by CYP2C19 genotypes.
However, the effect of CYP2C19 genotypes does not seem potent in patients with NERD. Kinoshita et al.[90] and Uemura et al.[91] independently studied the influence of CYP2C19 genotypes on the treatment of NERD by a PPI and concluded that the CYP2C19 genotype was not associated with therapeutic outcomes. However, Furuta et al.[92] reported that a step-up of the PPI dose (e.g. from rabeprazole 10 mg once daily to rabeprazole 10 mg twice daily and to 20 mg twice daily) was effective for patients who were refractory to the PPI at the standard dose, suggesting that insufficient acid inhibition is one of the reasons for therapeutic failure of a PPI in patients with NERD. Further studies are needed to verify the influences of CYP2C19 genotypes on the efficacy of a PPI for NERD.
In summary, CYP2C19 genotype status is considered to be one of the predictable determinants of the results of PPI-based therapy for RE. Therefore, an individualized therapeutic strategy based on the individual CYP2C19 genotype status is expected to increase the healing rates achieved by initial therapy with a PPI for GERD.
4. Strategies for Sufficient Acid Inhibition in Rapid Metabolizers of CYP2C19
As discussed above, one of the reasons for failure of PPI therapy for GERD is insufficient acid inhibition achieved by the PPI in patients with RM genotypes of CYP2C19. Overcoming the insufficient acid inhibition achieved by a PPI in RMs should result in an increase in GERD cure rates. For this purpose, several approaches have been tested. The acid inhibitory effect of histamine H2 receptor antagonists (H2RAs), such as famotidine, is not affected by the CYP2C19 genotype status and was shown to be superior to that of lansoprazole for controlling nocturnal intragastric pH in RM patients.[58] Sugimoto et al.[75] also administered an H2RA to RMs and reported that the addition of famotidine could achieve sufficient acid inhibition in such patients. Furuta et al.[93] reported that concomitant use of famotidine and lansoprazole yielded sufficient acid inhibition in CYP2C19 RMs. Adding an evening dose of an H2RA to a morning dose of a PPI appears to be effective for control of nocturnal acid breakthrough in individuals who are resistant to standard PPI treatment.[94–96] Therefore, addition of an H2RA is a useful strategy to overcome the insufficient acid inhibition achieved by a PPI in RMs.
Another approach to this problem is to increase the dosing schedule for a PPI. As noted above, frequent divided dosing of a PPI can minimize the influence of CYP2C19 genotypes. When lansoprazole 30 mg is administered four times daily in order to sustain plasma lansoprazole levels all day long (figure 4a), complete acid inhibition can be achieved even in RMs (figure 4b).[49] Interestingly, the peak plasma concentration (Cmax) of lansoprazole in RMs receiving this dosage was not increased in comparison with that achieved by once-daily dosing of 30 mg (figure 4a) and was not as high as that observed in PMs, although sufficient acid inhibition was achieved in RMs. Sugimoto et al.[76] reported that four-times-daily dosing of rabeprazole 10 mg achieved higher acid inhibition than that achieved by once-daily dosing of rabeprazole 40 mg. Similarly, Lou[22] reported that acid inhibition achieved by esomeprazole 20 mg twice daily or 10 mg four times daily did not differ among CYP2C19 genotype groups, although that achieved with esomeprazole 40 mg once daily did differ. Therefore, for CYP2C19 RMs, the optimal dosing scheme for a PPI is twice daily to four times daily. This strategy should be used when a patient is refractory to a PPI dosed once daily.
(a) Mean (± standard error) plasma concentration-time curves and (b) mean (± standard error) intragastric pH values versus time for lansoprazole after the final dosing of lansoprazole 30 mg once daily and lansoprazole 30 mg 4 times daily for 8 days in 5 patients with CYP2C19 rapid metabolizer genotypes. With 4-times-daily dosing of lansoprazole 30 mg, plasma levels of lansoprazole are sustained during each of the dosing intervals, thus complete acid inhibition (i.e. an intragastric pH of approximately 7.0) can be achieved. * Indicates dosing of lansoprazole 30 mg 4 times daily. (Reproduced from Furuta et al.,[49] with permission.)
5. Is Individualized Therapy for GERD Based on Genetic Testing Useful?
Unfortunately, there have been no studies of pharmacogenomics-guided therapies for GERD. As discussed above, the efficacy of PPIs depends on CYP2C19 genotypes; therefore, CYP2C19 genotype-guided adjustment of the dosing of a PPI is preferable. If the CYP2C19 genotype can be determined before the study, an optimal dosing scheme for a PPI can be developed in each patient, which is expected to increase the rate of cure of GERD during initial therapy. The recommended initial dosing schedules are as follows: four-times-daily dosing of a PPI at the standard dose for RMs, twice-daily dosing of a PPI at the standard dose for IMs, and once-daily dosing of a PPI at the standard dose for PMs. Thereafter, the dose of the PPI can be decreased (or increased) on the basis of the response of each patient to the PPI therapy (step-down or step-up) [figure 5]. This strategy is expected to increase the initial rates of response of GERD to PPI therapy.
6. Interaction of PPIs with Other Drugs
Patients taking a PPI sometimes take other medicines, some of which interact with the PPI. Therefore, the prescribing clinician must know about drug-drug interactions between PPIs and other drugs.
PPI-induced changes in gastric pH values sometimes influence the absorption of other drugs. Inhibition of gastric acid secretion increases the absorption of acid-labile drugs such as digoxin and sulfonyl urea, and weak acids such as diazepam, aspirin, and the diuretic furosemide. On the other hand, inhibition of acid secretion decreases the absorption of weak acids such as ketoconazole, itraconazole, dipyridamole, tetracycline, cephalosporin antibiotics, gefitinib, and erlotinib.[9,97,98] To avoid this interaction in the case of ketoconazole, it is recommended that the PPI is taken with cola, because the acidity of cola (∼pH 2.5) lessens the inhibition of ketoconazole absorption by the PPI.[99]
PPIs sometimes interact with CYP substrates. Stedman and Barclay[100] summarized the drug-drug interaction of different PPIs via CYPs and reported that there was some variation in their potential for drug interactions due to differences in enzyme inhibition. Kodaira et al.[101] reported the effect of different PPIs on CYP activity assessed by the [13C]-aminopyrine breath test in relation to CYP2C19 polymorphisms. They reported that different PPIs inhibited CYP activity to different extents. However, a higher PPI dose (e.g. omeprazole 80 mg) seemed to further inhibit CYP2C19 metabolic activity in RMs but increased it in PMs, indicating that a higher dose of a PPI induces other enzymes, such as CYP1A2.
The interaction between PPIs and clopidogrel has been focused on. In 2008, the consensus and guidelines of the American College of Cardiology Foundation (ACCF), American College of Gastroenterology (ACG), and American Heart Association (AHA) on antiplatelet therapy were published,[102–104] and they recommended that patients with a risk of peptic ulcer and/or those who were treated with two or more antiplatelet agents be treated with a PPI. However, clopidogrel is metabolically activated by CYP2C19 – the plasma level of the active metabolite of clopidogrel depends on the activity of CYP2C19. As a matter of fact, the inhibitory effect of clopidogrel on platelet aggregation depends on CYP2C19 genotypes[105] and is also associated with clinical events.[106] Moreover, concomitant use of clopidogrel and a PPI induces a drug-drug interaction via CYP2C19, resulting in decreased activation of clopidogrel. Juurlink et al.[107] reported that concomitant therapy with a PPI was associated with an increased risk of reinfarction. Ho et al.[108] reported that concomitant use of clopidogrel and a PPI was associated with an increased risk of adverse outcomes compared with use of clopidogrel without a PPI, and they suggested that use of a PPI might be associated with attenuation of the benefits of clopidogrel. These reports suggest that there are benefits (i.e. gastric protection) and risks (i.e. attenuation of clopidogrel efficacy) with concomitant use of a PPI in patients undergoing antiplatelet therapy including clopidogrel. This is the therapeutic dilemma of prophylactic use of PPI in antiplatelet therapy.
Furuta et al.[109] studied the effects of omeprazole, lansoprazole, and rabeprazole on the antiplatelet functions of clopidogrel in relation to CYP2C19 genotype status and found that the three PPIs attenuated the antiplatelet functions of clopidogrel to different degrees and that the levels of attenuation of clopidogrel by PPIs depended on CYP2C19 genotype status. They found that separate dosing of clopidogrel and omeprazole could not avoid this interaction (figure 6a). Although the efficacy of clopidogrel was decreased by a PPI in CYP2C19 RMs, the levels of antiplatelet function of clopidogrel after attenuation by a PPI in this group were generally not problematic (i.e. they were rarely decreased to the levels of a ‘low responder’ [inhibition of platelet aggregation <30%]) [figure 6b]. On the other hand, in patients with an IM genotype of CYP2C19, a conversion from responder to low-responder status occurs easily. Patients with CYP2C19 PM genotypes were low responders irrespective of PPI use. Therefore, the influence of a PPI on the activity of clopidogrel also depends on CYP2C19 genotypes.
Effects of morning or evening dosing of omeprazole on the efficacy of clopidogrel () in all patients and (b) in different CYP2C19 genotype groups. The decreased efficacy of clopidogrel caused by concomitant dosing of omeprazole was not restored by separate dosing of omeprazole overall (), but when the patients were analyzed separately according to CYP2C19 genotype (b), it was restored in CYP2C19 rapid metabolizers by separate dosing of omeprazole. In carriers of CYP2C19 *2 or *3 or both (intermediate and poor metabolizers), omeprazole appeared to decrease the efficacy of clopidogrel, which did not seem to be restored by separate dosing of omeprazole. (Reproduced from Furuta et al.,[109] with permission.)
Although prospective studies have indicated that the influence of PPIs on the clinical effect of clopidogrel is not problematic,[110,111] all pharmacokinetic studies have indicated the presence of a drug-drug interaction between PPIs and clopidogrel. Patients receiving dual antiplatelet therapy who are at risk of gastrointestinal bleeding should be treated with a PPI. However, clinicians must take this interaction into consideration for careful follow-up of patients.
7. Conclusion
The clinical effects of PPIs depend on the CYP2C19 genotypes of patients, as discussed in this review. Therefore, adjustments of the dose and dosing schedule for a PPI according to the CYP2C19 genotype should be useful for optimal PPI treatment in patients with GERD. The pharmacogenomics-based strategy requires genotyping tests in advance and therefore seems more costly, but we expect that such a cost could be offset by several benefits obtained from the higher cure rates achieved by the initial pharmacogenomics-based treatment.
References
Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis 1976; 21 (11): 953–6.
Bardhan KD. The role of proton pump inhibitors in the treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 1995; 9 Suppl. 1: 15–25.
Klinkenberg-Knol EC, Festen HP, Jansen JB, et al. Long-term treatment with omeprazole for refractory reflux esophagitis: efficacy and safety. Ann Intern Med 1994; 121 (3): 161–7.
Andersson T, Regardh CG, Dahl-Puustinen ML, et al. Slow omeprazole metabolizers are also poor S-mephenytoin hydroxylators. Ther Drug Monit 1990; 12 (4): 415–6.
Andersson T, Regardh CG, Lou YC, et al. Polymorphic hydroxylation of S-mephenytoin and omeprazole metabolism in Caucasian and Chinese subjects. Pharmacogenetics 1992; 2 (1): 25–31.
Sohn DR, Kobayashi K, Chiba K, et al. Disposition kinetics and metabolism of omeprazole in extensive and poor metabolizers of S-mephenytoin 4′-hydroxylation recruited from an Oriental population. J Pharmacol Exp Ther 1992; 262 (3): 1195–202.
Pearce RE, Rodrigues AD, Goldstein JA, et al. Identification of the human P450 enzymes involved in lansoprazole metabolism. J Pharmacol Exp Ther 1996; 277 (2): 805–16.
Yamazaki H, Inoue K, Shaw PM, et al. Different contributions of cytochrome P450 2C19 and 3A4 in the oxidation of omeprazole by human liver microsomes: effects of contents of these two forms in individual human samples. J Pharmacol Exp Ther 1997; 283 (2): 434–42.
Humphries TJ, Merritt GJ. Review article: drug interactions with agents used to treat acid-related diseases. Aliment Pharmacol Ther 1999; 13 Suppl. 3: 18–26.
Furuta T, Shirai N, Sugimoto M, et al. Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies. Drug Metab Pharmacokinet 2005; 20 (3): 153–67.
The Human Cytochrome P450 (CYP) Allele Nomenclature Committee. CYP2C19 allele nomenclature [online]. Available from URL: http://www.cypalleles.ki.se/cyp2c19.htm [Accessed 2012 Jul 17].
DeMorais SM, Wilkinson GR, Blaisdell J, et al. Identification of a new genetic defect responsible for the polymorphism of (S)-mephenytoin metabolism in Japanese. Mol Pharmacol 1994; 46 (4): 594–8.
deMorais SM, Goldstein JA, Xie HG, et al. Genetic analysis of the S-mephenytoin polymorphism in a Chinese population. Clin Pharmacol Ther 1995; 58 (4): 404–11.
deMorais SM, Wilkinson GR, Blaisdell J, et al. The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem 1994; 269 (22): 15419–22.
Thacker DL, Modak A, Nguyen PD, et al. Stereoselective pharmacokinetics of stable isotope (+/−)-[(13)C]-pantoprazole: implications for a rapid screening phenotype test of CYP2C19 activity. Chirality. Epub 2011 Sep 20.
Tazaki J, Jinnai T, Tada T, et al. Prediction of clopidogrel low responders by a rapid CYP2C19 activity test. J Atheroscler Thromb 2012; 19 (2): 186–93.
Kirchheiner J, Muller G, Meineke I, et al. Effects of polymorphisms in CYP2D6, CYP2C9, and CYP2C19 on trimipramine pharmacokinetics. J Clin Psychopharmacol 2003; 23 (5): 459–66.
Chang M, Dahl ML, Tybring G, et al. Use of omeprazole as a probe drug for CYP2C19 phenotype in Swedish Caucasians: comparison with S-mephenytoin hydroxylation phenotype and CYP2C19 genotype. Pharmacogenetics 1995; 5 (6): 358–63.
Furuta T, Shirai N, Takashima M, et al. Effects of genotypic differences in CYP2C19 status on cure rates for Helicobacter pylori infection by dual therapy with rabeprazole plus amoxicillin. Pharmacogenetics 2001; 11 (4): 341–8.
Furuta T, Shirai N, Sugimoto M, et al. Pharmacogenomics of proton pump inhibitors. Pharmacogenomics 2004; 5 (2): 181–202.
Gawronska-Szklarz B, Wrzesniewska J, Starzynska T, et al. Effect of CYP2C19 and MDR1 polymorphisms on cure rate in patients with acid-related disorders with Helicobacter pylori infection. Eur J Clin Pharmacol 2005; 61 (5–6): 375–9.
Lou HY, Chang CC, Sheu MT, et al. Optimal dose regimens of esomeprazole for gastric acid suppression with minimal influence of the CYP2C19 polymorphism. Eur J Clin Pharmacol 2009; 65 (1): 55–64.
Miura M, Tada H, Yasui-Furukori N, et al. Effect of clarithromycin on the enantioselective disposition of lansoprazole in relation to CYP2C19 genotypes. Chirality 2005; 17 (6): 338–44.
Padol S, Yuan Y, Thabane M, et al. The effect of CYP2C19 polymorphisms on H. pylori eradication rate in dual and triple first-line PPI therapies: a meta-analysis. Am J Gastroenterol 2006; 101 (7): 1467–75.
Sapone A, Vaira D, Trespidi S, et al. The clinical role of cytochrome p450 genotypes in Helicobacter pylori management. Am J Gastroenterol 2003; 98 (5): 1010–5.
Sheng YC, Wang K, He YC, et al. Effect of CYP2C19 genotypes on the pharmacokinetic/pharmacodynamic relationship of rabeprazole after a single oral dose in healthy Chinese volunteers. Eur J Clin Pharmacol 2010; 66 (11): 1165–9.
Suzuki T, Matsuo K, Sawaki A, et al. Influence of smoking and CYP2C19 genotypes on H. pylori eradication success. Epidemiol Infect 2007; 135 (1): 171–6.
Wang H, Nie YQ, Dai SJ, et al. The effect of proton pump inhibitor on intragastric acidity and it relation to S-mephenytoin hydroxylase genetic polymorphism. Zhonghua Nei Ke Za Zhi 2003; 42 (11): 777–80.
Yamano HO, Matsushita HO, Yanagiwara S. Plasma concentration of rabeprazole after 8-week administration in gastroesophageal reflux disease patients and intragastric pH elevation. J Gastroenterol Hepatol 2008; 23 (4): 534–40.
Zhao F, Wang J, Yang Y, et al. Effect of CYP2C19 genetic polymorphisms on the efficacy of proton pump inhibitor-based triple therapy for Helicobacter pylori eradication: a meta-analysis. Helicobacter 2008; 13 (6): 532–41.
Inomata S, Nagashima A, Itagaki F, et al. CYP2C19 genotype affects diazepam pharmacokinetics and emergence from general anesthesia. Clin Pharmacol Ther 2005; 78 (6): 647–55.
Furuta T, Kodaira C, Nishino M, et al. [13C]-pantoprazole breath test to predict CYP2C19 phenotype and efficacy of a proton pump inhibitor, lansoprazole. Aliment Pharmacol Ther 2009; 30 (3): 294–300.
Kodaira C, Uchida S, Yamade M, et al. Influence of different proton pump inhibitors on activity of cytochrome P450 assessed by [(13)C]-aminopyrine breath test. J Clin Pharmacol 2012; 52 (3): 432–9.
Hu YM, Xu JM, Mei Q, et al. Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotype in healthy Chinese subjects. Acta Pharmacol Sin 2005; 26 (3): 384–8.
Klotz U. Clinical impact of CYP2C19 polymorphism on the action of proton pump inhibitors: a review of a special problem. Int J Clin Pharmacol Ther 2006; 44 (7): 297–302.
Miura M, Tada H, Yasui-Furukori N, et al. Pharmacokinetic differences between the enantiomers of lansoprazole and its metabolite, 5-hydroxylansoprazole, in relation to CYP2C19 genotypes. Eur J Clin Pharmacol 2004; 60 (9): 623–8.
Qiao HL, Hu YR, Tian X, et al. Pharmacokinetics of three proton pump inhibitors in Chinese subjects in relation to the CYP2C19 genotype. Eur J Clin Pharmacol 2006; 62 (2): 107–12.
Wang Y, Zhang H, Meng L, et al. Influence of CYP2C19 on the relationship between pharmacokinetics and intragastric pH of omeprazole administered by successive intravenous infusions in Chinese healthy volunteers. Eur J Clin Pharmacol 2010; 66 (6): 563–9.
Xie HG, Kim RB, Stein CM, et al. Genetic polymorphism of (S)-mephenytoin 4′-hydroxylation in populations of African descent. Br J Clin Pharmacol 1999; 48 (3): 402–8.
Kubota T, Chiba K, Ishizaki T. Genotyping of S-mephenytoin 4′-hydroxylation in an extended Japanese population. Clin Pharmacol Ther 1996; 60 (6): 661–6.
Xie HG, Stein CM, Kim RB, et al. Allelic, genotypic and phenotypic distributions of S-mephenytoin 4′-hydroxylase (CYP2C19) in healthy Caucasian populations of European descent throughout the world. Pharmacogenetics 1999; 9 (5): 539–49.
Strom CM, Goos D, Crossley B, et al. Testing for variants in CYP2C19: population frequencies and testing experience in a clinical laboratory. Genet Med 2012; 14 (1): 95–100.
Rudberg I, Mohebi B, Hermann M, et al. Impact of the ultrarapid CYP2C19*17 allele on serum concentration of escitalopram in psychiatric patients. Clin Pharmacol Ther 2008; 83 (2): 322–7.
Sugimoto K, Uno T, Yamazaki H, et al. Limited frequency of the CYP2C19*17 allele and its minor role in a Japanese population. Br J Clin Pharmacol 2008; 65 (3): 437–9.
Sim SC, Risinger C, Dahl ML, et al. A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther 2006; 79 (1): 103–13.
Anichavezhi D, Chakradhara Rao US, Shewade DG, et al. Distribution of CYP2C19*17 allele and genotypes in an Indian population. J Clin Pharm Ther 2012; 37 (3): 313–8.
Furuta T, Ohashi K, Kosuge K, et al. CYP2C19 genotype status and effect of omeprazole on intragastric pH in humans. Clin Pharmacol Ther 1999; 65 (5): 552–61.
Shirai N, Furuta T, Moriyama Y, et al. Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther 2001; 15 (12): 1929–37.
Furuta T, Shirai N, Xiao F, et al. Effect of high-dose lansoprazole on intra-gastic pH in subjects who are homozygous extensive metabolizers of cytochrome P4502C19. Clin Pharmacol Ther 2001; 70 (5): 484–92.
AstraZeneca. Nexium capsule: interview form 2011 (in Japanese). Osaka: AstraZeneca, 2011.
Baldwin RM, Ohlsson S, Pedersen RS, et al. Increased omeprazole metabolism in carriers of the CYP2C19*17 allele; a pharmacokinetic study in healthy volunteers. Br J Clin Pharmacol 2008; 65 (5): 767–74.
Ohlsson Rosenborg S, Mwinyi J, Andersson M, et al. Kinetics of omeprazole and escitalopram in relation to the CYP2C19*17 allele in healthy subjects. Eur J Clin Pharmacol 2008; 64 (12): 1175–9.
Kearns GL, Leeder JS, Gaedigk A. Impact of the CYP2C19*17 allele on the pharmacokinetics of omeprazole and pantoprazole in children: evidence for a differential effect. Drug Metab Dispos 2010; 38 (6): 894–7.
Gumus E, Karaca O, Babaoglu MO, et al. Evaluation of lansoprazole as a probe for assessing cytochrome P450 2C19 activity and genotype-phenotype correlation in childhood. Eur J Clin Pharmacol 2012; 68 (5): 629–36.
Kurzawski M, Gawronska-Szklarz B, Wrzesniewska J, et al. Effect of CYP2C19*17 gene variant on Helicobacter pylori eradication in peptic ulcer patients. Eur J Clin Pharmacol 2006; 62 (10): 877–80.
Li-Wan-Po A, Girard T, Farndon P, et al. Pharmacogenetics of CYP2C19: functional and clinical implications of a new variant CYP2C19*17. Br J Clin Pharmacol 2010; 69 (3): 222–30.
Sibbing D, Gebhard D, Koch W, et al. Isolated and interactive impact of common CYP2C19 genetic variants on the antiplatelet effect of chronic clopidogrel therapy. J Thromb Haemost 2010; 8 (8): 1685–93.
Shirai N, Furuta T, Xiao F, et al. Comparison of lansoprazole and famotidine for gastric acid inhibition during the daytime and night-time in different CYP2C19 genotype groups. Aliment Pharmacol Ther 2002; 16 (4): 837–46.
Saitoh T, Watanabe Y, Kubo Y, et al. Effect of H2 blockers on the circadian rhythm of intragastric acidity. Biomed Pharmacother 2002; 56 Suppl. 2: 349s–352s.
Shimatani T, Moriwaki M, Xu J, et al. Acid-suppressive effects of rabeprazole: comparing 10 mg and 20 mg twice daily in Japanese Helicobacter pylori-negative and -positive CYP2C19 extensive metabolisers. Dig Liver Dis 2006; 38 (11): 802–8.
Miehlke S, Lobe S, Madisch A, et al. Intragastric acidity during administration of generic omeprazole or esomeprazole — a randomised, two-way crossover study including CYP2C19 genotyping. Aliment Pharmacol Ther 2011; 33 (4): 471–6.
Hu XP, Xu JM, Hu YM, et al. Effects of CYP2C19 genetic polymorphism on the pharmacokinetics and pharmacodynamics of omeprazole in Chinese people. J Clin Pharm Ther 2007; 32 (5): 517–24.
Sagar M, Bertilsson L, Stridsberg M, et al. Omeprazole and CYP2C19 polymorphism: effects of long-term treatment on gastrin, pepsinogen I, and chromogranin A in patients with acid related disorders. Aliment Pharmacol Ther 2000; 14 (11): 1495–502.
Kita T, Tanigawara Y, Aoyama N, et al. CYP2C19 genotype related effect of omeprazole on intragastric pH and antimicrobial stability. Pharm Res 2001; 18 (5): 615–21.
Inamori M, Togawa JI, Takahashi H, et al. Comparison of the effect on intragastric pH of a single dose of omeprazole or rabeprazole: which is suitable for on-demand therapy? J Gastroenterol Hepatol 2003; 18 (9): 1034–8.
Sugimoto M, Furuta T, Shirai N, et al. Initial 48-hour acid inhibition by intravenous infusion of omeprazole, famotidine, or both in relation to cytochrome P450 2C19 genotype status. Clin Pharmacol Ther 2006; 80 (5): 539–48.
Li ZS, Zhan XB, Xu GM, et al. Effect of esomeprazole and rabeprazole on intragastric pH in healthy Chinese: an open, randomized crossover trial. J Gastroenterol Hepatol 2007; 22 (6): 815–20.
Hunfeld NG, Touw DJ, Mathot RA, et al. A comparison of the acid-inhibitory effects of esomeprazole and rabeprazole in relation to pharmacokinetics and CYP2C19 polymorphism. Aliment Pharmacol Ther 2012; 35 (7): 810–8.
Furuta T, Shirai N, Kodaira M, et al. Pharmacogenomics-based tailored versus standard therapeutic regimen for eradication of H. pylori. Clin Pharmacol Ther 2007; 81 (4): 521–8.
Adachi K, Katsube T, Kawamura A, et al. CYP2C19 genotype status and intragastric pH during dosing with lansoprazole or rabeprazole. Aliment Pharmacol Ther 2000; 14 (10): 1259–66.
Nishino M, Sugimoto M, Kodaira C, et al. Relationship between low-dose aspirin-induced gastric mucosal injury and intragastric pH in healthy volunteers. Dig Dis Sci 2010; 55 (6): 1627–36.
Horai Y, Kimura M, Furuie H, et al. Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther 2001; 15 (6): 793–803.
Shimatani T, Inoue M, Kuroiwa T, et al. Rabeprazole 10mg twice daily is superior to 20 mg once daily for night-time gastric acid suppression. Aliment Pharmacol Ther 2004; 19 (1): 113–22.
Hayato S, Hasegawa S, Hojo S, et al. Dose-response relationships of rabeprazole 5, 10, 20, and 40mg once daily on suppression of gastric acid secretion through the night in healthy Japanese individuals with different CYP2C19 genotypes. Eur J Clin Pharmacol 2012 May; 68 (5): 579–88.
Sugimoto M, Furuta T, Shirai N, et al. Comparison of an increased dosage regimen of rabeprazole versus a concomitant dosage regimen of famotidine with rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotypes. Clin Pharmacol Ther 2005; 77 (4): 302–11.
Sugimoto M, Furuta T, Shirai N, et al. Different dosage regimens of rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotype status. Clin Pharmacol Ther 2004; 76 (4): 290–301.
Kodaira C, Sugimoto M, Nishino M, et al. Effect of MDR1 C3435T polymorphism on lansoprazole in healthy Japanese subjects. Eur J Clin Pharmacol 2009 Jun; 65 (6): 593–600.
Ishizaki T, Horai Y. Review article: cytochrome P450 and the metabolism of proton pump inhibitors — emphasis on rabeprazole. Aliment Pharmacol Ther 1999; 13 Suppl. 3: 27–36.
Bell NJ, Burget D, Howden CW, et al. Appropriate acid suppression for the management of gastro-oesophageal reflux disease. Digestion 1992; 51 Suppl. 1: 59–67.
Zendehdel N, Biramijamal F, Hossein-Nezhad A, et al. Role of cytochrome P450 2C19 genetic polymorphisms in the therapeutic efficacy of omeprazole in Iranian patients with erosive reflux esophagitis. Arch Iran Med 2010; 13 (5): 406–12.
Kawamura M, Ohara S, Koike T, et al. The effects of lansoprazole on erosive reflux oesophagitis are influenced by CYP2C19 polymorphism. Aliment Pharmacol Ther 2003; 17 (7): 965–73.
Furuta T, Shirai N, Watanabe F, et al. Effect of cytochrome P4502C19 genotypic differences on cure rates for gastroesophageal reflux disease by lansoprazole. Clin Pharmacol Ther 2002; 72 (4): 453–60.
Schwab M, Klotz U, Hofmann U, et al. Esomeprazole-induced healing of gastroesophageal reflux disease is unrelated to the genotype of CYP2C19: evidence from clinical and pharmacokinetic data. Clin Pharmacol Ther 2005; 78 (6): 627–34.
Ariizumi K, Ohara S, Koike T, et al. Therapeutic effects of 10mg/day rabeprazole administration on reflux esophagitis was not influenced by the CYP2C19 polymorphism. J Gastroenterol Hepatol 2006; 21 (9): 1428–34.
Kawamura M, Ohara S, Koike T, et al. Cytochrome P450 2C19 polymorphism influences the preventive effect of lansoprazole on the recurrence of erosive reflux esophagitis. J Gastroenterol Hepatol 2007; 22 (2): 222–6.
Furuta T, Sugimoto M, Kodaira C, et al. CYP2C19 genotype is associated with symptomatic recurrence of GERD during maintenance therapy with low-dose lansoprazole. Eur J Clin Pharmacol 2009 Jul; 65 (7): 693–8.
Saitoh T, Otsuka H, Kawasaki T, et al. Influences of CYP2C19 polymorphism on recurrence of reflux esophagitis during proton pump inhibitor maintenance therapy. Hepatogastroenterology 2009; 56 (91–92): 703–6.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999; 45: 172–80.
Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors — comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65 (1): 19–31.
Kinoshita Y, Ashida K, Hongo M. Randomised clinical trial: a multicentre, double-blind, placebo-controlled study on the efficacy and safety of rabeprazole 5 mg or 10 mg once daily in patients with non-erosive reflux disease. Aliment Pharmacol Ther 2011; 33 (2): 213–24.
Uemura N, Inokuchi H, Serizawa H, et al. Efficacy and safety of omeprazole in Japanese patients with nonerosive reflux disease. J Gastroenterol 2008; 43 (9): 670–8.
Furuta T, Shimatani T, Sugimoto M, et al. Investigation of pretreatment prediction of proton pump inhibitor (PPI)-resistant patients with gastroesophageal reflux disease and the dose escalation challenge of PPIs — TORNADO study: a multicenter prospective study by the Acid-Related Symptom Research Group in Japan. J Gastroenterol 2011; 46 (11): 1273–83.
Furuta T, Shirai N, Sugimoto M, et al. Effect of concomitant dosing of famotidine with lansoprazole on gastric acid secretion in relation to CYP2C19 genotype status. Aliment Pharmacol Ther 2005; 22 (1): 67–74.
Xue S, Katz PO, Banerjee P, et al. Bedtime H2 blockers improve nocturnal gastric acid control in GERD patients on proton pump inhibitors. Aliment Pharmacol Ther 2001; 15 (9): 1351–6.
Peghini PL, Katz PO, Castell DO. Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology 1998; 115 (6): 1335–9.
Kinoshita Y, Adachi K, Fujishiro H. Therapeutic approaches to reflux disease, focusing on acid secretion. J Gastroenterol 2003; 38 Suppl. 15: 13–9.
Reynolds JC. The clinical importance of drug interactions with antiulcer therapy. J Clin Gastroenterol 1990; 12 Suppl. 2: S54–63.
Jaruratanasirikul S, Sriwiriyajan S. Effect of omeprazole on the pharmacokinetics of itraconazole. Eur J Clin Pharmacol 1998; 54 (2): 159–61.
Chin TW, Loeb M, Fong IW. Effects of an acidic beverage (Coca-Cola) on absorption of ketoconazole. Antimicrob Agents Chemother 1995; 39 (8): 1671–5.
Stedman CA, Barclay ML. Review article: comparison of the pharmacokinetics, acid suppression and efficacy of proton pump inhibitors. Aliment Pharmacol Ther 2000; 14 (8): 963–78.
Kodaira C, Uchida S, Yamade M, et al. Influence of different proton pump inhibitors on activity of cytochrome P450 assessed by [13C]-aminopyrine breath test. J Clin Pharmacol 2012 Mar; 52 (3): 432–9.
Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2008; 52 (18): 1502–17.
Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. Am J Gastroenterol 2008; 103 (11): 2890–907.
Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation 2008; 118 (18): 1894–909.
Umemura K, Furuta T, Kondo K. The common gene variants of CYP2C19 affect pharmacokinetics and pharmacodynamics in an active metabolite of clopidogrel in healthy subjects. J Thromb Haemost 2008; 6 (8): 1439–41.
Collet JP, Hulot JS, Pena A, et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet 2009; 373 (9660): 309–17.
Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ 2009; 180 (7): 713–8.
Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA 2009; 301 (9): 937–44.
Furuta T, Iwaki T, Umemura K. Influences of different proton pump inhibitors on the anti-platelet function of clopidogrel in relation to CYP2C19 genotypes. Br J Clin Pharmacol 2010; 70 (3): 383–92.
O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet 2009; 374 (9694): 989–97.
Bhatt DL, Cryer BL, Contant CF, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med 2010; 363 (20): 1909–17.
Acknowledgments
The Center for Clinical Research at Hamamatsu University School of Medicine has received grants from Takeda Pharmaceutical Co., Ltd., AstraZeneca KK, and Eisai Co., Ltd., and Drs. Furuta and Sugimoto have received lecture fees from those companies. The authors have no other conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Furuta, T., Sugimoto, M. & Shirai, N. Individualized Therapy for Gastroesophageal Reflux Disease. Mol Diagn Ther 16, 223–234 (2012). https://doi.org/10.1007/BF03262211
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03262211