Abstract
Background and aims
The effect of multidrug resistance transporter gene 1 (MDR1) on the bioavailability and kinetics of several substrates has not yet been fully elucidated. We evaluated the influence of MDR1 C3435T polymorphism on the pharmacokinetics and pharmacodynamics of lansoprazole in Japanese subjects.
Methods
Fifteen healthy volunteers with the rapid extensive metabolizer genotype of CYP2C19 were classified into three MDR1 C3435T genotype groups: C/C (n = 5), C/T (n = 5), and T/T (n = 5). Lansoprazole 30 mg was administered orally for 15 days. The intragastric pH and plasma lansoprazole levels were determined on days 1 and 15.
Results
On day 1, the mean Cmax of lansoprazole in the T/T group was significantly higher than that in the C/C or C/T groups (T/T 1,248, C/C 618, C/T 607 ng/ml; P = 0.038). On day 15, similar MDR1 genotype-dependent differences were observed in the Cmax of lansoprazole, although smaller than the differences observed on day 1. In contrast, the intragastric pH attained after lansoprazole administration did not differ among MDR1 genotype groups on either day 1 or day 15.
Conclusion
Although the sample size was small, our study demonstrated that the MDR1 C3435T polymorphism influenced the pharmacokinetics, but not the pharmacodynamics (i.e., intragastric pH), of lansoprazole in rapid metabolizers of CYP2C19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proton-pump inhibitors (PPIs) such as lansoprazole, omeprazole, rabeprazole, esomeprazole, and pantoprazole are in current clinical use as potent gastric-acid inhibitors. PPIs inhibit gastric-acid secretion by interaction with H+/K+-ATPase in gastric parietal cells [1, 2]. The major indication for PPIs is acid-related diseases, such as peptic ulcer, gastroesophageal reflux disease (GERD), and Zollinger-Ellison syndrome [3–7]. PPIs are also used to eradicate Helicobacter pylori (H. pylori) infection in combination with antimicrobial agents such as clarithromycin (CAM), metronidazole (MNZ), and amoxicillin (AMPC) [8–10].
PPIs are mainly metabolized in the liver by cytochrome P450 isoenzyme 2C19 (CYP2C19), an enzyme whose activity varies due to genetic differences. The genotypes of CYP2C19 are classified into three groups: rapid metabolizer (RM = *1/*1), intermediate metabolizer (IM = *1/*X), and poor metabolizer (PM = *X/*X, where *X = *2 or *3) [11]. The pharmacokinetics and pharmacodynamics of PPIs differ by CYP2C19 genotype [12, 13]: during PPI treatment, plasma PPI and intragastric pH levels are lowest in the RM group and highest in the PM group. These genotype-dependent differences in pharmacokinetics and pharmacodynamics of PPIs are reflected in the cure rates for H. pylori infection following a PPI-based treatment regimen [11, 14]. Factors other than CYP2C19 polymorphism that affect the cure rates of H. pylori infection include bacterial susceptibility to clarithromycin [15], smoking, and compliance, among others. However, interindividual differences in clinical outcomes are still observed even in individuals who exhibit similarities with regard to these factors, suggesting that other factors influence the pharmacokinetics and pharmacodynamics of PPIs.
MDR1 codes the P-glycoprotein (P-gp), a component of adenosine triphosphate (ATP)-binding-cassette (ABC) transporters [16]. P-gp functions as the energy-dependent exporter of substances from cells and prevents accumulation of potentially toxic and also carcinogenetic substances and metabolites in cells. P-gp expression represents one of the most important mechanisms for the failure of chemotherapeutic treatment of cancer [17]. P-gp is expressed on the surface of not only cancer cells but also normal cells such as hepatocytes, enterocytes, and endothelial cells of brain blood vessels. Genetic differences affect the expression of MDR1 [18]. A synonymous single nucleotide polymorphism (SNP) in exon 26 (C3435T) has sometimes been reported to be associated with altered P-gp activity [18]. Plasma levels of digoxin, a representative substrate of MDR1, have been found to differ among MDR1 C3435T genotype groups [19].
Lansoprazole is a substrate of P-gp [20], but the impact of MDR1 C3435T polymorphism on the pharmacokinetics and pharmacodynamics of lansoprazole has not been fully elucidated. Recent clinical studies have revealed that lansoprazole-based therapies for H. pylori infection are affected by MDR1 C3435T polymorphism [21, 22]). However, several reports have indicated that P-gp activity is also affected by the G2677A/T (Ala893Thr or Ala893Ser) and/or C1236T (synonymous) polymorphism [23, 24]. Interestingly, MDR1 C3435T is in linkage disequilibrium with other polymorphisms such as G2677A/T and C1236T. Meta-analysis has suggested that these haplotypes, rather than the single polymorphism, may be more predictive of P-gp activity [25]. Here, we investigated whether MDR1 C3435T polymorphism as well as haplotypes affected the pharmacokinetics and pharmacodynamics of lansoprazole in healthy Japanese subjects with the rapid metabolizer genotype of CYP2C19.
Methods
Eighty healthy Japanese subjects were invited to be genotyped for CYP2C19 and MDR1 C3435T and serologically tested for H. pylori infection as described below. Of these, 15 with the RM genotype of CYP2C19 (*1/*1) and different MDR1 C3435T genotypes were enrolled into this study. All participants were seronegative for H. pylori infection and had different MDR1 C3435T genotypes (MDR1 3435C/C = 5, C/T = 5, T/T = 5), with no history of peptic ulcer, hepatic disorders, cardiovascular disorders, renal diseases, or other serious conditions. Participants had consumed no alcohol or taken any drugs for at least 1 month prior to this study.
Participants were given a single daily oral dose of 30 mg lansoprazole (Takepron, Takeda Pharmaceutical, Osaka, Japan) at 0800 for 15 days. Intragastric pH was monitored 24 h/day, and blood samples were collected at 0, 0.5, 1, 2, 3, 5, 7, 10, and 24 h after drug administration on days 1 and 15. Meals with the same contents were served at 0800, 1230, and 1800 on days 1 and 15, with caloric counts measuring 300, 600, and 800 kcal, respectively. All subjects gave written informed consent, and the study protocol was approved by the Ethics Committee of Hamamatsu University School of Medicine.
Genotyping of CYP2C19 and MDR1
CYP2C19 genotyping was performed by PCR-RFLP using DNA extracted from whole blood [26]. Those subjects homozygous for the 1* allele (*1/*1) were defined as RMs of CYP2C19.
MDR1 C3435T polymorphisms were identified by PCR-RFLP as reported previously [27] and classified as C/C, C/T, or T/T polymorphism. MDR1 C1236T and G2677A/T genotypes were similarly determined in all subjects and classified as C/C, C/T, or T/T for C1236T, and as G/G, G/T, G/A, A/T, or T/T for G2677A/T [28].
Diagnosis of H. pylori infection
H. pylori infection was assessed by serological testing. Anti-H. pylori antibody titer was measured by enzyme immunoassay (E plate; Eiken Chemical, Tokyo, Japan) with an assay value <10 U/mL considered negative and >10 U/mL considered positive for infection [29].
Analysis of lansoprazole in plasma
Plasma concentrations of lansoprazole were determined by liquid chromatography (HPLC)/mass spectrometry (LC/MS). Briefly, plasma samples (0.2 mL) containing 10 ng of isobutyl p-hydroxybenzoate as an internal standard were diluted with 0.7 mL of water and applied to an OASIS HLB extraction cartridge (Waters, Milford, MA, USA). The cartridge was then washed with 5% methanol in water (1.0 mL) and eluted with ethanol (1.0 mL). The elution was evaporated under a stream of nitrogen gas at 40°C, and the residue was reconstituted in 200 μL of mobile phase (acetonitrile/10 mM ammonium acetate, 44:56, v/v). A 30-μL aliquot was injected into the HPLC apparatus and analyzed using an analytical column (Symmetry C18, 5 mm, 2.1 × 150 mm; Waters) with the mobile phase delivered at a flow rate of 0.3 mL/min at 40°C. The mass spectrometer was operated in positive ionization mode with selected ion recording acquisition at 370 m/z for lansoprazole. The limit of quantification was 0.1 ng/mL, and the intra-assay coefficient of variation was <10.4%.
Statistical analysis
Numerical values are given as mean ± SD. The pharmacokinetic parameters for lansoprazole were estimated by noncompartmental analysis. Maximum plasma concentration (Cmax) and the time at maximum plasma concentration (Tmax) were estimated directly from observed plasma concentration-time data. The area under the concentration vs. time curve (AUC) was calculated by the trapezoidal rule for the observed values. Genotype frequencies of MDR1 C1236T, C3435T, and G2677A/T genotypes were compared using the χ2-test. Statistically significant differences in pharmacokinetic and pharmacodynamics parameters among the three different MDR1 C3435T genotype groups were assessed by one-way ANOVA followed by the Scheffe’s multiple comparison test. Presence or absence of changes in pharmacological parameters between day 1 and 15 was assessed by paired t-test. All P-values were two-sided, and values were considered statistically significant at P < 0.05.
Results
Examination of the demographic data of subjects found that mean age and sex did not differ significantly among the three MDR1 genotype groups (Table 1). We observed a possible linkage disequilibrium between MDR1 C3435T and G2677A/T polymorphisms. The incidence of the 2677 G/G genotype was markedly high in the 3435 C/C group, that of 2677 G/T was markedly high in the 3435 C/T group, and that of 2677 T/T was markedly high in the 3435 T/T group (Table 1). A similar but not statistically significant tendency was observed between C3435T polymorphism and C1236T polymorphism.
Figure 1 shows the mean plasma concentration-time curves of lansoprazole as a function of MDR1 C3435T polymorphism on day 1 and day 15. Concentrations differed among the three different MDR1 C3435T genotypes following a 30-mg single-dose administration of lansoprazole. Plasma lansoprazole levels in the T/T group appeared higher than those in the C/T and C/C groups on day 1 (Fig. 1a). This MDR1 C3435T genotype-dependent difference in levels was still apparent on day 15, but appeared smaller than on day 1 (compare Fig. 1b with a).
Plasma lansoprazole level as a function of MDR1 C3435T genotype status on day 1 (a) and day 15 (b). A 30-mg dose of lansoprazole was given in a single daily oral administration for 15 days. Blood samples were collected on days 1 and 15 at the indicated time points. The peak of the plasma lansoprazole concentration on day 1 was higher in the T/T group (circles) than in the other groups (triangles C/T and squares C/C) (a)
Pharmacokinetic parameters of lansoprazole are summarized in Table 2. On day 1, the mean Cmax in the T/T group was significantly higher than that in the C/C and C/T groups (T/T 1,248 vs. C/C 618 and C/T 607 ng/ml; P = 0.043, 0.042) (Table 2). Mean AUC0–24 h on day 1 was highest in the T/T group (3,653 h·ng/ml), although the difference between groups was not statistically significant (C/C 2,506, C/T 2,375 h·ng/ml) (Table 2). Further, mean Tmax on day 1 was shortest in the T/T group.
However, these MDR1 C3435T genotype-dependent differences in pharmacokinetics parameters observed on day 1 seemed to lessen by day 15. The mean Cmax of lansoprazole increased from day 1 to 15 in the C/C and C/T groups, and the increase in the C/T group was statistically significant (P = 0.014) (Fig. 2). However, this increase was not observed in the T/T group, resulting in a smaller difference in Cmax on day 15 among the three groups (mean Cmax at day 15: C/C 1,021, C/T 1,332, and T/T 1,459 ng/ml). Although mean Cmax of the T/T group on day 15 still appeared highest of the three, the difference was not statistically significant.
Changes in Cmax of lansoprazole from day 1 to day 15 as a function of MDR1 C3435T genotype status. There was a statistically significant difference in the mean Cmax of lansoprazole among the three different genotype groups on day 1. From day 1 to day 15, the means of Cmax in the C/C (squares) and C/T (triangles) groups increased, and the increase in the C/T group in particular was statistically significant (P = 0.014), while the increase in the T/T group (circles) was small. This resulted in a smaller apparent difference in the means of Cmax among the three genotype groups on day 15 then on day 1
Similarly, the mean AUC0–24 h of the MDR1 3435 C/C, C/T, and T/T groups on day 15 were 2,901, 3,897, and 4,654 h·ng/ml, respectively, with no statistically significant differences among them. Further, Tmax for all three groups on day 15 appeared nearly identical (Table 2).
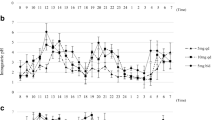
Figures 3b and c show intragastric pH profiles of the different MDR1 genotype groups over 24 h on days 1 and 15, respectively. Control profiles of intragastric pH are shown in Fig. 3a, and intragastric pH parameters are summarized in Table 3. The mean 24-h intragastric pH on day 1 was 3.1 in the C/C group, 3.5 in the C/T group, and 3.8 in the T/T group, with no statistically significant differences in the mean 24-h intragastric pH among the three genotypes (P = 0.566). Similarly, there were no statistically significant differences among MDR1 genotype group for the intragastric pH profile on day 15, nor was there a statistically significant difference in the percentage time for intragastric pH < 4 among the groups on both days 1 and 15 (Table 3).
The 24-h intragastric pH profiles as a function of MDR1 C3435T genotype status. a Control intragastric pH profiles. b and c Intragastric pH levels with daily dosing of lansoprazole 30 mg on days 1 and 15, respectively. The intragastric pH profiles of the three MDR1 C3435T genotype groups (squares C/C, triangles C/T, and circles T/T) appeared nearly identical, irrespective of dosing schedule
Influence of MDR1 G2677A/T/C3435T haplotype
To further analyze the influence of MDR1 haplotype, we compared the pharmacokinetics and pharmacodynamics of lansoprazole in the groups with the MDR1 2677G/G and 3435C/C (GC/GC) type and the MDR1 2677T/T and 3435T/T (TT/TT) type. The Cmax and AUC0–24 h of lansoprazole appeared higher, but not significantly so, in the TT/TT group in comparison with measurements in the GC/GC group on both day 1 and day 15. However, this haplotype demonstrated no influence on the mean 24-h intragastric pH attained by lansoprazole (Table 4).
Discussion
Here, we found that the pharmacokinetics of lansoprazole were influenced by the MDR1 C3435T polymorphism in a group of Japanese subjects. However, the acid inhibition attained with daily administration of 30 mg of lansoprazole was not affected by this polymorphism. Further, these findings demonstrate for the first time that the influence of the MDR1 C3435T genotypic difference on the pharmacokinetics of lansoprazole decreases following repeated dosing. We therefore assume that the MDR1 C3435T polymorphism is of limited importance in the usual therapeutic dosing schedule for lansoprazole.
The multidrug-resistant transporter encoded by MDR1 is a member of the ATP-binding cassette superfamily of membrane transporters [27] and has the potential to expel unnecessary or toxic exogenous substances or metabolites from cells. More than 40 SNPs have been discovered in MDR1. In 2000, Hoffmeyer et al. [19] first demonstrated that an SNP in exon 26 of the MDR1 gene (C3435T) was associated with lower intestinal MDR1 levels and higher plasma levels of orally dosed digoxin. Thus, the MDR1 3435T/T genotype is thought to be associated with higher plasma levels of MDR1 substrates. However, the effects of MDR1 polymorphism on the pharmacokinetics and pharmacodynamics of other substrates have not been fully verified.
Recent in vitro data have indicated that lansoprazole is a P-glycoprotein substrate [20], but whether the pharmacokinetics and pharmacodynamics of lansoprazole are affected by the MDR1 C3435T polymorphism in humans has not been clearly established. Our results here showed that plasma levels in the T/T group were the highest of the three MDR1 genotype groups, a finding expected based on the Hoffmeyer report [19]. Interestingly, this between-group difference decreased after repeated dosing of lansoprazole, and the kinetic dispositions of lansoprazole in the C/C and C/T groups became closer to those of the T/T group with increasing Cmax. This observation indicates that lansoprazole inhibits the activity of MDR1 gradually in the C/C and C/T groups. Further studies are required to verify this finding.
Contrarily, our present study further demonstrated that the MDR1 C3435T polymorphism did not affect the gastric-acid inhibition attained by lansoprazole on either day 1 or day 15. Although we are unable to explain why MDR1 genotype was associated with plasma concentration but not intragastric pH, particularly on day 1, we suspect the following: First, because all subjects in the present study had the RM genotype of CYP2C19, lansoprazole metabolism in the liver may have been so fast that the influence of MDR1 genotypic differences on the pharmacokinetics of lansoprazole could not be reflected in the pharmacodynamics. Second, although Cmax was highest in the T/T group, there was no significant difference in AUC values among the three MDR1 genotype groups, indicating that plasma lansoprazole levels in the T/T group did not remain high long enough to affect the intragastric pH. This finding could be explained by our previous report, which indicated that the acid-inhibitory effect of PPI depended on the time spent above the threshold concentration, not on the Cmax [30].
Several reports have cited findings contrary to those of Hoffmeyer. Nakamura et al. [31] suggested that the expression of serum digoxin of MDR1 mRNA in the duodenum of individuals homozygous for 3435T (T/T) was higher than in individuals with the C/C or C/T genotypes in Japanese subjects. Another meta-analysis review has indicated that MDR1 C3435T polymorphism does not affect the pharmacokinetics of digoxin or the expression of MDR1 mRNA [25]. The single SNP in exon 26 (C3435T) is a synonymous SNP, so it does not change the encoded amino acid sequence. However, MDR1 C3435T has been reported to be in linkage disequilibrium with other common functional nonsynonymous polymorphisms such as MDR1 exon 21 (G2677A/T, Ala893Thr, or Ala893Ser) [32]. In the present study, the C3435T polymorphism was linked with G2677T and C1236T (a synonymous SNP in exon 12) polymorphisms [27]. In fact, MDR1 C1236T, G2677T, and C3435T polymorphisms have been reported to be part of a common haplotype [33].
Recent studies have demonstrated that the activity of MDR1 is related to not only C3435T but also C1236T and G2677A/T polymorphisms, and that haplotypic analysis of these SNPs is important for the precise evaluation of MDR1 activity. Park et al. reported that the clinical effects of fentanyl were significantly dependent on both MDR1 C1236T and C3435T polymorphisms [34]. Kim et al. reported that the haplotypic analysis of SNPs at positions 2677 and 3435 was well associated with the pharmacokinetics of amlodipine [35]. In the present study, analysis of the effect of G2677A/T and C3435T haplotype showed that haplotype analysis could not clarify the gene-dose effect on lansoprazole. We therefore believe that analysis of single SNP of C3435T is sufficient to estimate MDR1 activity. Ultimately, the function of MDR1 C3435T polymorphism remains controversial and is confounded by several genetic as well as ethnic and geographic factors.
Miura et al. [36] reported that the Cmax and AUC0–24 h of lansoprazole were significantly increased in Japanese patients with the MDR1 3435C allele. However, these authors admitted that the effect of this polymorphism in clinical practice seemed negligible, on the basis that these polymorphisms were not associated with gastroesophageal complications in gastroesophageal reflux disease (GERD) patients treated with lansoprazole. We found that plasma lansoprazole levels, as for Cmax, were highest in the T/T group of the three MDR1 genotype groups, a finding that was opposite to that seen by Miura et al. However, our results also demonstrated that MDR1 C3435T polymorphism did not affect the acid inhibition attained by lansoprazole at the standard dose, although a difference in the plasma lansoprazole levels was seen among the three genotype groups on day 1. Moreover, we observed that the MDR1 genotype-dependent difference in plasma lansoprazole levels decreased and lost statistical significance following repeated dosing, as on day 15. We therefore consider that the effect of MDR1 C3435T on the pharmacodynamics of lansoprazole may be small in clinical practice because administration of PPIs in GERD patients usually occurs over an extended period of time.
Several limitations of our study warrant mention. First, we did not evaluate the effect of MDR1 in subjects with the IM and PM genotypes of CYP2C19. Since the plasma concentration of lansoprazole depended on the CYP2C19 genotype status, it would be better to perform the same study in IMs and PMs of CYP2C19. However, the frequency of PMs in Japan is only 19–23% [26], therefore it was difficult to enroll a sufficient number of PM subjects with different MDR1 genotypes. Second, our study population was a small pool of healthy volunteers, not patients. These results should therefore be considered preliminary.
In conclusion, our study demonstrates that pharmacokinetics of lansoprazole depends on MDR1 C3435T polymorphism in Japanese subjects, but its pharmacodynamics does not. Interestingly, the impact of MDR1 C3435T polymorphism on the pharmacokinetics of lansoprazole becomes smaller after repeated doses. These preliminary findings suggest that the MDR1 polymorphism is of limited relevance in therapeutic regimens involving lansoprazole. To verify the relevance of MDR1 polymorphism in patients treated with lansoprazole, future studies in clinical practices should include CYP2C19 IMs and PMs as well as RMs.
Abbreviations
- CYP2C19:
-
Cytochrome P450 2C9
- Helicobacter pylori :
-
H. pylori
- IM:
-
Intermediate metabolizer
- MDR1:
-
Multidrug resistance transporter gene 1
- PPI:
-
Proton-pump inhibitor
- PM:
-
Poor metabolizer
- RM:
-
Rapid metabolizer
References
Nagaya H, Satoh H, Maki Y (1990) Possible mechanism for the inhibition of acid formation by the proton pump inhibitor AG-1749 in isolated canine parietal cells. J Pharmacol Exp Ther 252(3):1289–1295
Nagaya H, Inatomi N, Nohara A et al (1991) Effects of the enantiomers of lansoprazole (AG-1749) on (H++K+)-ATPase activity in canine gastric microsomes and acid formation in isolated canine parietal cells. Biochem Pharmacol 42(10):1875–1878
Blum RA (1996) Lansoprazole and omeprazole in the treatment of acid peptic disorders. Am J Health Syst Pharm 53(12):1401–1415
Lockhart SP (1994) Clinical review of lansoprazole. Br J Clin Pract Suppl 75:48–55 discussion 56–57
Langtry HD, Wilde MI (1997) Lansoprazole. An update of its pharmacological properties and clinical efficacy in the management of acid-related disorders. Drugs 54(3):473–500
Inatomi N, Nagaya H, Takami K et al (1991) Effects of a proton pump inhibitor, AG-1749 (lansoprazole), on reflux esophagitis and experimental ulcers in rats. Jpn J Pharmacol 55(4):437–451
Carswell CI, Goa KL (2001) Rabeprazole: an update of its use in acid-related disorders. Drugs 61(15):2327–2356
Unge P (1996) Review of Helicobacter pylori eradication regimens. Scand J Gastroenterol Suppl 215:74–81
Asaka M, Sugiyama T, Kato M et al (2001) A multicenter, double-blind study on triple therapy with lansoprazole, amoxicillin and clarithromycin for eradication of Helicobacter pylori in Japanese peptic ulcer patients. Helicobacter 6(3):254–261
Furuta T, Futami H, Arai H et al (1995) Effects of lansoprazole with or without amoxicillin on ulcer healing: relation to eradication of Helicobacter pylori. J Clin Gastroenterol 20(Suppl 2):S107–111
Furuta T, Shirai N, Sugimoto M et al (2004) Pharmacogenomics of proton pump inhibitors. Pharmacogenomics 5(2):181–202
Miura M, Tada H, Yasui-Furukori N et al (2004) Pharmacokinetic differences between the enantiomers of lansoprazole and its metabolite, 5-hydroxylansoprazole, in relation to CYP2C19 genotypes. Eur J Clin Pharmacol 60(9):623–628
Furuta T, Ohashi K, Kosuge K et al (1999) CYP2C19 genotype status and effect of omeprazole on intragastric pH in humans. Clin Pharmacol Ther 65(5):552–561
Furuta T, Ohashi K, Kamata T et al (1998) Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann Intern Med 129(12):1027–1030
Murakami K, Sato R, Okimoto T et al (2002) Eradication rates of clarithromycin-resistant Helicobacter pylori using either rabeprazole or lansoprazole plus amoxicillin and clarithromycin. Aliment Pharmacol Ther 16(11):1933–1938
Kullak-Ublick GA, Becker MB (2003) Regulation of drug and bile salt transporters in liver and intestine. Drug Metab Rev 35(4):305–317
Ambudkar SV, Dey S, Hrycyna CA, Ramachandra M et al (1999) Biochemical, cellular, and pharmacological aspects of the multidrug transporter. Annu Rev Pharmacol Toxicol 39:361–398
Hitzl M, Drescher S, van der Kuip H et al (2001) The C3435T mutation in the human MDR1 gene is associated with altered efflux of the P-glycoprotein substrate rhodamine 123 from CD56+natural killer cells. Pharmacogenetics 11(4):293–298
Hoffmeyer S, Burk O, von Richter O et al (2000) Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci USA 97(7):3473–3478
Pauli-Magnus C, Rekersbrink S, Klotz U, Fromm MF (2001) Interaction of omeprazole, lansoprazole and pantoprazole with P-glycoprotein. Naunyn Schmiedebergs Arch Pharmacol 364(6):551–557
Gawronska-Szklarz B, Wrzesniewska J, Starzynska T et al (2005) Effect of CYP2C19 and MDR1 polymorphisms on cure rate in patients with acid-related disorders with Helicobacter pylori infection. Eur J Clin Pharmacol 61(5–6):375–379
Furuta T, Sugimoto M, Shirai N et al (2007) Effect of MDR1 C3435T polymorphism on cure rates of Helicobacter pylori infection by triple therapy with lansoprazole, amoxicillin and clarithromycin in relation to CYP 2C19 genotypes and 23S rRNA genotypes of H. pylori. Aliment Pharmacol Ther 26(5):693–703
Kim RB, Leake BF, Choo EF et al (2001) Identification of functionally variant MDR1 alleles among European Americans and African Americans. Clin Pharmacol Ther 70(2):189–199
Wasilewska A, Zalewski G, Chyczewski L et al (2007) MDR-1 gene polymorphisms and clinical course of steroid-responsive nephrotic syndrome in children. Pediatr Nephrol 22(1):44–51
Chowbay B, Li H, David M, Cheung YB et al (2005) Meta-analysis of the influence of MDR1 C3435T polymorphism on digoxin pharmacokinetics and MDR1 gene expression. Br J Clin Pharmacol 60(2):159–171
Kubota T, Chiba K, Ishizaki T (1996) Genotyping of S-mephenytoin 4′-hydroxylation in an extended Japanese population. Clin Pharmacol Ther 60(6):661–666
Cascorbi I, Gerloff T, Johne A et al (2001) Frequency of single nucleotide polymorphisms in the P-glycoprotein drug transporter MDR1 gene in white subjects. Clin Pharmacol Ther 69(3):169–174
Komoto C, Nakamura T, Sakaeda T et al (2006) MDR1 haplotype frequencies in Japanese and Caucasian, and in Japanese patients with colorectal cancer and esophageal cancer. Drug Metab Pharmacokinet 21(2):126–132
Kawai T, Kawakami K, Kudo T, Ogiahara S et al (2002) A new serum antibody test kit (E plate) for evaluation of Helicobacter pylori eradication. Intern Med 41(10):780–783
Sugimoto M, Furuta T, Shirai N et al (2004) Different dosage regimens of rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotype status. Clin Pharmacol Ther 76(4):290–301
Nakamura T, Sakaeda T, Horinouchi M et al (2002) Effect of the mutation (C3435T) at exon 26 of the MDR1 gene on expression level of MDR1 messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clin Pharmacol Ther 71(4):297–303
Horinouchi M, Sakaeda T, Nakamura T et al (2002) Significant genetic linkage of MDR1 polymorphisms at positions 3435 and 2677: functional relevance to pharmacokinetics of digoxin. Pharm Res 19(10):1581–1585
Tang K, Ngoi SM, Gwee PC et al (2002) Distinct haplotype profiles and strong linkage disequilibrium at the MDR1 multidrug transporter gene locus in three ethnic Asian populations. Pharmacogenetics 12(6):437–450
Park HJ, Shinn HK, Ryu SH et al (2007) Genetic polymorphisms in the ABCB1 gene and the effects of fentanyl in Koreans. Clin Pharmacol Ther 81(4):539–546
Kim KA, Park PW, Park JY (2007) Effect of ABCB1 (MDR1) haplotypes derived from G2677T/C3435T on the pharmacokinetics of amlodipine in healthy subjects. Br J Clin Pharmacol 63(1):53–58
Miura M, Satoh S, Tada H et al (2006) Influence of ABCB1 C3435T polymorphism on the pharmacokinetics of lansoprazole and gastroesophageal symptoms in Japanese renal transplant recipients classified as CYP2C19 extensive metabolizers and treated with tacrolimus. Int J Clin Pharmacol Ther 44(12):605–613
Acknowledgements
This work was supported by a grant-in-aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (20590718). We thank Ms. Kageyama for her help in measuring plasma concentrations of lansoprazole.
Conflict of interest
No authors had any conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kodaira, C., Sugimoto, M., Nishino, M. et al. Effect of MDR1 C3435T polymorphism on lansoprazole in healthy Japanese subjects. Eur J Clin Pharmacol 65, 593–600 (2009). https://doi.org/10.1007/s00228-009-0625-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0625-8