Abstract
Background and Aims
Gastric acid plays an important role in the pathogenesis of gastric mucosal lesions. We investigated whether aspirin-induced gastric mucosal injury might have any association with the intragastric pH.
Materials and Methods
Fifteen healthy, Helicobacter pylori-negative volunteers randomly underwent the four different 7-day regimens: (1) aspirin 100 mg, (2) rabeprazole 10 mg, (3) aspirin 100 mg + rabeprazole 10 mg, and (4) aspirin 100 mg + rabeprazole 40 mg. Gastric mucosal injury based on the modified Lanza score (MLS), 24-h intragastric pH, and histopathology of gastric mucosa were evaluated prior to the start and on day 7 of each regimen.
Results
The median MLSs were 0 in the baseline and the rabeprazole 10 mg regimen. The median MLS in the aspirin regimen was 3, while those in both aspirin + rabeprazole 10 mg and aspirin + rabeprazole 40 mg regimens were 0. Rabeprazole significantly prevented the gastric mucosal injury by aspirin (P = 0.001 for rabeprazole 10 mg and P = 0.005 for rabeprazole 40 mg). The MLSs were negatively correlated with the 24-h intragastric pH (P = −0.711, < 0.001), whereas aspirin had no effect on the intragastric pH. Aspirin expanded the mean diameter of the microvessels of the gastric mucosa, which, in turn, was negatively correlated with the intragastric pH.
Conclusions
Aspirin might induce gastric mucosal injury by affecting the mucosal microvessels in an acid-dependent manner. Sustained maintenance of the intragastric pH at an elevated value is necessary to prevent gastric mucosal damage induced by aspirin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies have revealed that the main causes of development of peptic ulcer diseases are Helicobacter pylori (H. pylori) infection and non-steroidal anti-inflammatory drugs (NSAID) [1]. The prevalence of H. pylori infection is now decreasing, with an expected decrease in the incidence of H. pylori-related peptic ulcer. On the other hand, the use of low-dose aspirin for primary and secondary prophylaxis against cardiovascular and cerebrovascular diseases is increasing [2], and the incidence of NSAID-related peptic ulcer, particularly that related to the use of low-dose aspirin, appears now to be increasing [3].
Aspirin inhibits cyclooxygenase-1 (COX-1) activity and, thereby, platelet aggregation, which contributes to the prevention of cardiovascular events [4]. However, inhibition of COX-1 activity decreases the prostaglandin E2 (PGE2) synthesis in the gastric mucosa and affects the gastric mucosal defense mechanisms, resulting in increased susceptibility of the gastric mucosa to damage [5]. Because both prostaglandins and leukotrienes are produced from arachidonic acid, COX-1 inhibition also results in a spill-over effect on leukotrienes, including leukotriene B4, which are known as extremely potent vasoconstrictors and inducers of inflammation, and may be responsible for some of the aspirin-induced gastric mucosal damage. Moreover, at an acidic pH, aspirin enters the gastric mucosal cells by non-ionic diffusion and induces cellular damage directly, leading to disruption of the gastric barrier and subsequent back-diffusion of hydrogen ions into the mucosa, resulting in local mucosal injury. Through the above-mentioned pathways, aspirin often induces gastroduodenal lesions [6]. In fact, Yeomans et al. [7] reported that 10.7% of 187 patients under treatment with low-dose aspirin (i.e., 75–325 mg/day) had peptic ulcer and that 63.1% of these subjects had gastric erosive lesions. Derry et al. [8] reported that long-term therapy with aspirin was associated with a significant increase in the incidence of gastrointestinal hemorrhage and that neither reduction in the dose of aspirin nor the use of enteric-coated aspirin could reduce incidence of gastrointestinal hemorrhage. These reports suggest that low-dose aspirin readily causes gastric mucosal injury. Therefore, development of an appropriate strategy for the prevention of gastric mucosal injury induced by low-dose aspirin is clinically important.
Proton-pump inhibitors (PPIs) are now widely used for the prevention and control of aspirin-induced gastric mucosal injury. Pilotto et al. [9] reported that PPI treatment was associated with a reduced risk of development of peptic ulcer lesions in NSAID/aspirin users, and concluded that co-treatment with a PPI is advisable in patients treated with an NSAID and/or aspirin. Serrano et al. [10] reported that antisecretory agents, such as PPIs and histamine H2 receptor antagonists (H2RAs), reduce the risk of upper gastrointestinal bleeding [RR: 0.22 (0.07–0.75)]. However, it remains unclear how much acid inhibition is needed for the prevention of aspirin-induced gastric mucosal injury.
PPIs are mainly metabolized by CYP2C19, and genetic differences in the activity of this enzyme have been recognized. Subjects are classified into three groups based on the genotype of CYP2C19: rapid metabolizers (RMs), intermediate metabolizers (IMs), and poor metabolizers (PMs) [11]. In PMs of CYP2C19, plasma levels of PPIs such as omeprazole and lansoprazole are markedly increased, and the pharmacodynamic effect of PPIs (i.e., acid inhibition) is enhanced in comparison with that in IMs or RMs of CYP2C19. As a matter of fact, the cure rate of H. pylori infection by PPI-based therapy depends on the CYP2C19 genotype status, and the rates in the PMs have been shown to be the highest [12]. On the other hand, rabeprazole (rabeprazole) is reduced mainly via a non-enzymatic pathway to thioether-rabeprazole [13, 14], and the acid-inhibitory effect of rabeprazole has been considered to be less influenced by the CYP2C19 genotype as compared with that of the other PPIs [15, 16], although several studies have contrarily suggested that the plasma levels of rabeprazole and the gastric acid-inhibitory effect of rabeprazole are also quite dependent on the CYP2C19 status [17, 18].
Therefore, we investigated the relationship between the severity of aspirin-induced gastric mucosal injury and the intragastric pH. We also examined whether the preventive effect of rabeprazole against aspirin-induced gastric mucosal injury depended on the CYP2C19 genotype status.
Materials and Methods
Subjects and CYP2C19 Genotyping
Blood samples were obtained from 59 healthy Japanese volunteers after obtaining written informed consent from each of them. Deoxyribonucleic acid (DNA) was extracted from each subject’s leukocytes using a commercially available kit (Iso-Quick; ORCA Research, Bothell, WA, USA). Genotyping for identifying the CYP2C19 wild-type gene (1*) and the 2 mutated alleles, CYP2C19*2 in exon 5 and CYP2C19*3 in exon 4, was performed by a polymerase chain reaction-restriction fragment length polymorphism method using allele-specific primers. Based on the CYP2C19 genotype, the subjects were classified into three groups: RMs (*1/*1), IMs (*1/*2 or *1/*3), and PMs (*2/*2, *2/*3, or *3/*3). The presence of H. pylori infection was screened by a serological test (HM-CAP kit; Enteric Products, Stony Brook, NY, USA).
A total of 15 H. pylori-negative healthy volunteers (5 RMs, 5 IMs, and 5 PMs) were enrolled in this study after obtaining their informed consent. Serum pepsinogen (PG) I and PG II levels were measured by radioimmunoassay (Abbott Japan, Tokyo, Japan), and the PG I–PG II ratio was calculated for serologic evaluation of the presence/absence of atrophic gastritis in all the 15 subjects enrolled in the study. None of them consumed alcohol or smoked for at least 2 weeks prior to the study period and they also abstained during the study period. None of the subjects had taken any drugs for at least 2 weeks prior to the study period, nor took any drugs during the study period.
Study Protocol
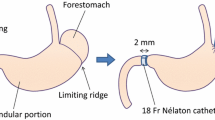
This was an open-label single-arm protocol study. Firstly, all subjects underwent endoscopy and 24-h intragastric pH monitoring to obtain baseline data and to confirm that none of the subjects had any severe gastroduodenal disorders or abnormal gastric acid secretion before initiation of any of following four regimens. Secondly the subjects were administered the following all four regimens for 7 days and were allocated following order: aspirin 100 mg od (Bayaspirin 100 mg; Bayer, Osaka, Japan; aspirin regimen), rabeprazole 10 mg od (Pariet; Eisai, Tokyo, Japan; rabeprazole 10 mg regimen), aspirin 100 mg od plus rabeprazole 10 mg od (aspirin + rabeprazole 10 mg regimen), and aspirin 100 mg od plus rabeprazole 10 mg qid (aspirin + rabeprazole 40 mg regimen). On day 7 of each regimen, endoscopy and 24-h intragastric pH monitoring were repeated, as described later. A washout period of at least 2 weeks was set between the two treatments.
All subjects were provided with two low-fat meals on day 7 (lunch at 1200 hours, dinner at 1800 hours). Mineral water was allowed as needed, but no other beverages were permitted. The study protocol was approved in advance by the Ethics Committee of Hamamatsu University School of Medicine.
Endoscopy and Collection of Gastric Mucosal Samples for Histopathology
Endoscopy was performed after the subject had fasted overnight, with an Olympus GIF-XQ 240 flexible gastroscope (Olympus Corporation, Tokyo, Japan) introduced using the xylocaine throat spray. During the endoscopy, more than 40 pictures were taken by an expert endoscopist who was blinded to any other information about the subject. Endoscopic images were also recorded on video. The grade of gastric mucosal injury was graded independently, based on the modified Lanza score (MLS) system (Grade 0 = no erosion/hemorrhage, Grade 1 = 1–2 lesions of erosion and/or hemorrhage are localized in one area of the stomach, Grade 2 = 3–5 lesions of erosion and/or hemorrhage are localized in one area of the stomach, Grade 3 = 6–9 lesions of erosion and/or hemorrhage are localized in one area of the stomach or no more than 10 lesions appear in two areas in the stomach, Grade 4 = erosion and/or hemorrhage appear in three areas in the stomach or no less than 10 lesions in the whole stomach, and Grade 5 = gastric ulcer) [19, 20], by two other expert endoscopists who were also blinded to any information about the subjects. When the two endoscopists differed on the score assigned, they arrived at a consensus by reviewing the video images.
Biopsy specimens were taken from the gastric mucosa free of macroscopic gastric mucosal injury from three points: the major curvature of the gastric antrum, minor curvature of the lower part of the gastric corpus, and major curvature of the upper part of the gastric corpus. The gastric biopsy specimens were stained with hematoxylin-eosin (H&E). The severities of gastritis and inflammation were assessed according to the updated Sydney system [21]. The mean score from the three points was used as the gastritis score in each subject. The diameters of the subepithelial microvessels were determined by measurement of the minor axis of each vessel, because the length of the vascular longer axis, but not that of the minor axis, depends on the angle of the section. The mean diameter of 30 randomly selected subepithelial microvessels from three points was calculated. A single pathologist (H.S.) who was unaware of any clinical information about the patients examined all the biopsy specimens.
Twenty-Four-Hour Intragastric pH Monitoring
Twenty-four-hour intragastric pH monitoring was performed in each trial phase. At 30 min after the endoscopy, an antimony pH catheter (Medtroinc, Minneapolis, MN, USA) was inserted transnasally under local anesthesia and placed 5 cm distal to the gastric cardia. The intragastric pH data were recorded with a Digitrapper MK III (Medtronic Functional Diagnostics, Skovlunde, Denmark).
Symptom Index
Symptoms such as heartburn, abdominal pain, indigestion, diarrhea, and constipation were assessed using the GSRS questionnaire [22], with minor modification. Each of the above symptoms was graded on a scale of 1–7.
Statistical Analysis
The intragastric pH values, the percent time period for which the intragastric pH remained at <4.0, the MLS values, the symptom scores and the histological values were expressed as the median (and range). The median intragastric pH values over 24 h were obtained from the raw pH values. Statistically significant differences in the median MLS and median intragastric pH values among different regimens (i.e., control, rabeprazole 10 mg, aspirin, aspirin + rabeprazole 10 mg, and aspirin + rabeprazole 40 mg) were determined by Friedman’s test followed by Wilcoxon’s signed-rank test. Statistically significant differences in the values of MLS and intragastric pH among the different CYP2C19 genotype groups were determined by the Mann–Whitney U test when a significant difference was observed by the Kruskal-Wallis test. Statistically significant associations between the MLS and intragastric pH during the treatments including low-dose aspirin were assessed by calculating Spearman’s correlation coefficients.
All the statistical analyses were performed with the StatView software (SAS Institute, Cary, NC, USA). All P values were two-sided, and P < 0.05 was considered as indicating statistical significance.
Results
In all the 15 subjects enrolled in the study, the study was completed according to protocol between November 2006 and November 2007 at the university hospital. There were no significant differences in the demographic or clinical characteristics (e.g., age, sex, and PG I/PG II) at baseline among the different CYP2C19 genotype groups (Table 1). None of the subjects experienced any adverse events associated with aspirin, such as gastrointestinal hemorrhage or major abdominal symptoms.
Aspirin-Induced Gastric Mucosal Injury and Preventive Effect of Rabeprazole
The changes in the MLS in each subject associated with the different treatments are shown in Fig. 1. The median (range) MLS in the baseline was 0 (0–1). Significant increase of the median MLS (3, 0–5) was observed in the aspirin regimen in comparison with that in the control. Next, the median MLS in the Rabeprazole 10 mg regime decreased to 0 (0–3). However, the aspirin-induced gastric mucosal damage was attenuated in the aspirin + rabeprazole 10 mg regimen; the median MLS in this regimen was 0 (0–2), as in the baseline and rabeprazole 10 mg regimen. Although the median MLS was similarly 0 in the aspirin + rabeprazole 40 mg regimen, the maximum MLS also decreased in this group from 2 to 1.
Gastric mucosal injury with different regimens; baseline, aspirin, rabeprazole (RPZ) 10 mg, aspirin + RPZ 10 mg, and aspirin + RPZ 40 mg. Gastric mucosal injury was given as modified Lanza score (MLS). Treatment with RPZ 10 mg did not change the MLS in comparison with the baseline. The 7-day treatment with aspirin significantly increased the median MLS in comparison with those of baseline and RPZ 10 mg (P < 0.005, 0.005). However, the concomitant treatment with RPZ 10 mg inhibited the aspirin-induced increase of MLS. The concomitant treatment with aspirin and RPZ 40 mg decreased the maximum of the MLS from 2 to 1, although the median MLS with this regimen did not change
Twenty-Four-Hour Intragastric pH With the Different Regimens
The median 24-h intragastric pH and the percent time period over which the intragastric pH remained at <4 for each treatment are summarized in Fig. 2. The median 24-h intragastric pH was increased in the groups treated with rabeprazole as compared with that in the baseline. The median 24-h intragastric pH in the rabeprazole 40 mg regimen was significantly higher than that in the rabeprazole 10 mg regimen (P < 0.001). There were no significant differences in the median 24-h intragastric pH between baseline and aspirin regimen, rabeprazole regimen and aspirin + rabeprazole 10 mg regimen (Fig. 2a).
Median 24-h intragastric pH (a) and percent time for intragastric pH < 4 (b) with different regimens. a Median 24-h intragastric pH was increased by the regimens including RPZ (i.e., RPZ 10 mg, RPZ 10 mg with aspirin, RPZ 40 mg with aspirin) in comparison with that of baseline. The median 24-h intragastric pH attained by RPZ 40 mg was significantly higher than that by RPZ 10 mg (P < 0.001). However, aspirin alone did not change the median 24-h intragastric pH. b The median percent time for intragastric pH < 4 was significantly decreased by the regimens including RPZ in comparison with that of baseline. The median percent time for intragastric pH < 4 attained by RPZ 40 mg was significantly shorter than that by RPZ 10 mg (P < 0.001). However, aspirin alone did not change the median percent time for intragastric pH < 4
The median percent time period over which the intragastric pH remained at <4 was significantly decreased in the patients receiving rabeprazole as compared with that in the baseline. This parameter was significantly shorter in the rabeprazole 40 mg regimen as compared with that in the rabeprazole 10 mg regimen (P < 0.001). There were no significant differences in the median percent time period over which the intragastric pH remained at <4 between baseline and aspirin regimen, rabeprazole regimen and aspirin + rabeprazole 10 mg regimen (Fig. 2b).
We determined the effect of aspirin on the gastric acid secretion in the subjects treated with or without rabeprazole and observed that aspirin had no influence on the intragastric pH or on the percent time period over which the intragastric pH remained at <4 (Fig. 2a, b).
Correlation Between the Severity of Mucosal Injury and the Intragastric Acidity
The correlations between the MLS following treatment with aspirin and the mean 24-h intragastric pH or percentage time period over which the intragastric pH remained at <4 are shown in Fig. 3. The 24-h intragastric pH and the percent time period over which the intragastric pH remained at <4 were each significantly related to the MLS, with correlation coefficients of −0.711 and 0.730, respectively (P < 0.001 for both; Fig. 3a, b). There was a statistically significant difference in the MLS between subjects with an intragastric pH value of <4 and those with the value of ≥4; the MLS was 0 in 20 of 29 subjects with a 24-h intragastric pH of ≥4, while it was 0 in only 2 of the 16 subjects with a 24-h intragastric pH of <4.0 (P < 0.001; Fig. 4).
Correlation between aspirin-induced gastric mucosal injury and intragastric acidity. a Correlation between 24-h intragastric pH and MLS and b correlation between the percent time for intragastric pH < 4 and MLS after 7-day treatment with different regimens including aspirin. The 24-h intragastric pH level and the percent time for intragastric pH < 4 are each significantly correlated to MLS with −0.711 and 0.730 of correlation coefficients, respectively (P < 0.001)
The frequencies of MLSs by aspirin stratified by median 24-h intragastric pH ≥ 4 (n = 29) or < 4 (n = 16). There was a statistically significant difference between incidences of MLS in the subjects with intragastric pH ≥ 4 and those <4. The MLS of 0 was found in 20 of 29 subjects with intragastric pH ≥ 4, while only 2 of 16 subjects with pH < 4.0 had MLS of 0 (P < 0.0001)
Histopathological Changes Induced by Aspirin With/Without Rabeprazole in Relation to the Intragastric pH and Mucosal Injury
Although aspirin induced endoscopic gastric mucosal injury, the median of the activity scores was 0 in all the subjects treated with aspirin in this study. Similarly, the scores for inflammation remained uninfluenced by treatment with aspirin in the study groups (data not shown).
Treatment with aspirin for 7 days significantly increased the median diameter of the subepithelial microvessels (18.0 μm, 13.0–22.3) as compared with that in the baseline regimen (11.3 μm, 8.7–16.0). In the concomitantly treated aspirin + rabeprazole 10 mg regimen, significant decrease of the diameter (14.0 μm, 9.7–21.7) as compared with that in the aspirin-alone regimen was observed. The median diameter of the microvessels in the aspirin + rabeprazole 40 mg regimen (11.3 μm, 8.7–19.3) was almost the same as that in the baseline regimen (Fig. 5).
Changes in the length of a minor axis of gastric subepithelial microvessels with different regimens. The length of minor axis of microvessel in aspirin regimen was significantly wide compared with those of baseline and RPZ 10 mg regimen. In the concomitant of RPZ and aspirin regimen, those decreased according to RPZ doses
Histopathological findings with different regimens in a representative case are shown in Fig. 6. Subepithelial microvessels were dilated with aspirin in comparison with control and treatment with rabeprazole alone (cf. Fig. 6b with a and c). When aspirin was administered with rabeprazole 10 or 40 mg, such dilation was suppressed (Fig. 6d, e).
The correlations among the intragastric acidity, the histological parameters and the MLSs are shown in Fig. 7. The intragastric pH was significantly correlated with the mean diameter of the subepithelial microvessels (Fig. 7a), but not with the scores for the activity of gastritis (Fig. 7b, c). The mean diameter of the subepithelial microvessels was significantly correlated with the MLS (Fig. 7d), but the scores for gastritis activity and inflammation were not (Fig. 7e, f).
The correlations of intragastric acidity with histological parameters: small vessel diameter (a), activity of gastritis (monocyte infiltration) (b) and inflammation (poly-nuclear cell infiltration) (c) and those of histological parameters, such as vessel diameter (d), activity of gastritis (e) and inflammation (f) with MLSs. The intragastric acidity was significantly correlated with subepithelial microvessel diameter, and higher 24-h pH value decrease diameter of subepithelial microvessel (a). However, there was no significant correlation with intragastric pH value and inflammatory cell infiltration (b,c). The MLS score was significantly correlated with subepithelial microvessel diameter, and according to increasing MLS score, the diameter of subepithelial microvessel gradually increased (d). However, there was no significant correlation with MLS score and inflammatory cell infiltration (e,f)
Symptoms by Aspirin With/Without Rabeprazole
The median scores of all the gastrointestinal symptoms remained one throughout the study periods. No statistical significant differences in the symptom scores were observed among the different treatments (details of data not shown).
Effect of the CYP2C19 Genotype Status on the Intragastric pH and MLS
The median 24-h intragastric pH, the percent time period over which the intragastric pH remained at <4 and the median MLS associated with the different treatments as a function of the CYP2C19 genotype status are summarized in Table 2. The median 24-h intragastric pH in the aspirin + rabeprazole 40 mg regimen differed significantly among the different CYP2C19 genotype groups (IMs vs PMs, P = 0.028), while in the rabeprazole 10 mg and aspirin + rabeprazole 10 mg regimens, there was a tendency towards an increase in the intragastric pH in the PMs as compared with that in the other two genotype groups, although the differences were not statistically significant. Similarly, there were statistically significant differences in the percent time period over which the gastric pH remained at <4 attained in the aspirin + rabeprazole 40 mg regimen among the three different CYP2C19 genotype groups (IMs vs PMs, P = 0.008). However, no significant differences in the MLS associated with any of the treatments were observed among the different CYP2C19 genotype groups.
Discussion
In this study, we observed that short-term treatment with low-dose aspirin induced gastric mucosal injury, which was prevented by rabeprazole, one of the representative PPIs, and that the severity of the gastric mucosal injury induced by aspirin was closely related to the intragastric pH. When the intragastric pH was controlled at higher than 4 in a sustained manner, the aspirin-induced mucosal injury could be effectively prevented. Therefore, we believe that to prevent aspirin-induced gastric mucosal injury, the 24-h intragastric pH should be maintained at higher than 4 by concomitant treatment with a PPI.
The role of gastric acid in the pathogenesis of NSAID-induced gastric mucosal injury was intensively studied by Funatsu et al. [23]. They studied the gastric mucosal microcirculation in rats treated with diclofenac in the absence and presence of acid. They found that the gastric mucosal microcirculation was significantly decreased by diclofenac in the presence of acid. Elliott et al. [24] reported that indomethacin induced gastric mucosal injury in an intragastric pH-dependent manner. Kitchingman et al. [25] reported that the higher intragastric pH levels associated with the administration of ranitidine attenuated aspirin-induced gastric mucosal injury. These reports indicate that gastric acid plays an important role in the pathogenesis of gastric mucosal injury induced by NSAIDs, including aspirin. In fact, sufficient gastric acid inhibition by a high dose of an H2RA or PPI is reported to be a useful strategy for the prevention of NSAID/aspirin-related gastric lesions. However, no studies have demonstrated how much gastric acid inhibition is needed for the prevention of gastric mucosal injury by low-dose aspirin. In the present study, aspirin-induced gastric mucosal injury was rarely observed in subjects in whom the intragastric pH was controlled at higher than 4. Therefore, we propose that the intragastric pH should be sufficiently suppressed for the prevention of gastric mucosal injury during aspirin dosing (i.e., intragastric pH >4).
Whether NSAIDs including low-dose aspirin might affect gastric acid secretion has not yet been fully elucidated. Savarino et al. [26] reported an increase of the gastric acidity after NSAID treatment for a month in female patients with rheumatoid arthritis of recent onset, whereas Janssen et al. [27] reported that indomethacin did not influence the intragastric pH in rheumatoid arthritis patients, irrespective of the presence/absence of a history of peptic ulcer disease. In the present study, low-dose aspirin did not influence gastric acidity. Therefore, we think that, at the dose used in the present study, aspirin induces gastric mucosal injury, but does not affect gastric acid secretion.
There are several reports on the effects of aspirin on the histopathology of the gastric mucosa, some of which indicate that aspirin induces inflammation in gastric mucosa [28, 29]. In the present study, we examined the effects of low-dose aspirin on the histopathology of the gastric mucosa in humans based on the updated Sydney system and found that aspirin did not induce inflammatory cell infiltration of the gastric mucosa. Whether aspirin induces inflammation of the gastric mucosa in humans, therefore, remains to be verified in a future study.
In the present study, we found that the median diameter of the gastric mucosal subepithelial microvessels was increased following treatment with low-dose aspirin. Yao et al. [30] previously reported that the gastric mucosal subepithelial microvessels were expanded by aspirin, which we confirmed in this study. Interestingly, we observed that this increase in the microvessel diameter was inversely correlated with the intragastric pH, indicating that aspirin influences the microvessels of the gastric mucosa in an acid-dependent manner. Kitahora et al. [31] reported that aspirin alone had no effect on the superficial gastric mucosal microcirculation in the rat, but that application of hydrochloric acid induced the formation of numerous white thrombi in the arterioles and venules, which resulted in disruption of the blood flow. Although we could not detect the formation of white thrombi in the microvessels by usual optical microscopy, we assume that stasis of the microcirculation by thrombi induced to form in an acid-dependent manner by aspirin might be reflected by the increase in the microvessel diameter. However, further studies will be needed to precisely clarify the effects of aspirin on the gastric mucosal microcirculation in humans.
As compared with other PPIs, the metabolism of rabeprazole has been reported to be influenced to a lesser degree by genotypic differences in CYP2C19. However, several reports have demonstrated that the metabolism and plasma levels of rabeprazole and its acid-inhibitory effects depend on the CYP2C19 genotype status [16]. In the present study, we observed CYP2C19 genotype-dependent differences in the intragastric pH during treatment with 40 mg rabeprazole, whereas the preventive effect of rabeprazole against low-dose aspirin-induced gastric mucosal injury did not depend on the CYP2C19 genotype status. We think that the acid-inhibitory effect of rabeprazole in RMs of CYP2C19 is sufficient for the prevention of low-dose aspirin-induced gastric mucosal injury. In fact, the mean intragastric pH obtained by treatment with 10 mg rabeprazole daily was 5.3 in the present study. Shimatani et al. [32] also reported that the mean 24-h intragastric pH obtained with rabeprazole treatment at 10 mg daily was 4.0 in RMs of CYP2C19.
Finally, we have to interpret our study results within the scope of the limitations of this study, as follows: firstly, the study period might have been too short; and secondly, our study subjects were young, healthy, and H. pylori-negative individuals, different from the usual recipients of low-dose aspirin treatment. Therefore, our study should be considered as preliminary, and further studies with the enrollment of older subjects treated with low-dose aspirin for longer periods of time are needed.
In conclusion, the present study demonstrated that low-dose aspirin induces gastric mucosal injury in an acid-dependent manner. We confirmed that sufficient acid inhibition (i.e., 24-h intragastric pH > 4) is important for the prevention of gastric injury induced by low-dose aspirin. Daily treatment with 10 mg rabeprazole could prevent aspirin-induced gastric mucosal injury, irrespective of the CYP2C19 genotype status.
Abbreviations
- COX:
-
Cyclooxygenase
- CYP2C19:
-
Cytochrome P450 2C19
- H. pylori :
-
Helicobacter pylori
- IM:
-
Intermediate metabolizer
- MLS:
-
Modified Lanza score
- NSAID:
-
Non-steroidal anti-inflammatory drug
- PG:
-
Prostaglandin
- PM:
-
Poor metabolizer
- RM:
-
Rapid metabolizer
References
Nishikawa K, Sugiyama T, Kato M, et al. Non-Helicobacter pylori and non-NSAID peptic ulcer disease in the Japanese population. Eur J Gastroenterol Hepatol. 2000;12(6):635–640.
Awtry EH, Loscalzo J. Aspirin. Circulation. 2000;101(10):1206–1218.
Taha AS, Angerson WJ, Knill-Jones RP, Blatchford O. Upper gastrointestinal haemorrhage associated with low-dose aspirin and anti-thrombotic drugs - a 6-year analysis and comparison with non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2005;22(4):285–289.
Collaborative overview of randomised trials of antiplatelet therapy–I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. Bmj. 1994;308(6921):81-106.
Schoen RT, Vender RJ. Mechanisms of nonsteroidal anti-inflammatory drug-induced gastric damage. Am J Med. 1989;86(4):449–458.
Halter F. Mechanism of gastrointestinal toxicity of NSAIDs. Scand J Rheumatol Suppl. 1988;73:16–21.
Yeomans ND, Lanas AI, Talley NJ, et al. Prevalence and incidence of gastroduodenal ulcers during treatment with vascular protective doses of aspirin. Aliment Pharmacol Ther. 2005;22(9):795–801.
Derry S, Loke YK. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta-analysis. BMJ. 2000;321(7270):1183–1187.
Pilotto A, Franceschi M, Leandro G, et al. Proton-pump inhibitors reduce the risk of uncomplicated peptic ulcer in elderly either acute or chronic users of aspirin/non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2004;20(10):1091–1097.
Serrano P, Lanas A, Arroyo MT, Ferreira IJ. Risk of upper gastrointestinal bleeding in patients taking low-dose aspirin for the prevention of cardiovascular diseases. Aliment Pharmacol Ther. 2002;16(11):1945–1953.
Furuta T, Shirai N, Sugimoto M, Ohashi K, Ishizaki T. Pharmacogenomics of proton pump inhibitors. Pharmacogenomics. 2004;5(2):181–202.
Furuta T, Shirai N, Takashima M, et al. Effect of genotypic differences in CYP2C19 on cure rates for Helicobacter pylori infection by triple therapy with a proton pump inhibitor, amoxicillin, and clarithromycin. Clin Pharmacol Ther. 2001;69(3):158–168.
Ishizaki T, Horai Y. Review article: cytochrome P450 and the metabolism of proton pump inhibitors—emphasis on rabeprazole. Aliment Pharmacol Ther. 1999;13(Suppl 3):27–36.
Yasuda S, Horai Y, Tomono Y, et al. Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′-hydroxylation status. Clin Pharmacol Ther. 1995;58(2):143–154.
Adachi K, Katsube T, Kawamura A, et al. CYP2C19 genotype status and intragastric pH during dosing with lansoprazole or rabeprazole. Aliment Pharmacol Ther. 2000;14(10):1259–1266.
Shirai N, Furuta T, Moriyama Y, et al. Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther. 2001;15(12):1929–1937.
Ieiri I, Kishimoto Y, Okochi H, et al. Comparison of the kinetic disposition of and serum gastrin change by lansoprazole versus rabeprazole during an 8-day dosing scheme in relation to CYP2C19 polymorphism. Eur J Clin Pharmacol. 2001;57(6–7):485–492.
Horai Y, Kimura M, Furuie H, et al. Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther. 2001;15(6):793–803.
Lanza FL, Royer GL Jr, Nelson RS, Chen TT, Seckman CE, Rack MF. A comparative endoscopic evaluation of the damaging effects of nonsteroidal anti-inflammatory agents on the gastric and duodenal mucosa. Am J Gastroenterol. 1981;75(1):17–21.
Naito Y, Yoshikawa T, Iinuma S, et al. Rebamipide protects against indomethacin-induced gastric mucosal injury in healthy volunteers in a double-blind, placebo-controlled study. Dig Dis Sci. 1998;43(9 Suppl):83S–89S.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification, grading of gastritis. The updated Sydney System. International workshop on the histopathology of gastritis Houston, 1994. Am J Surg Pathol. 1996;20(10):1161–1181.
Svedlund J, Sjodin I, Dotevall G. GSRS—a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33(2):129–134.
Funatsu T, Chono K, Hirata T, Keto Y, Kimoto A, Sasamata M. Mucosal acid causes gastric mucosal microcirculatory disturbance in nonsteroidal anti-inflammatory drug-treated rats. Eur J Pharmacol. 2007;554(1):53–59.
Elliott SL, Ferris RJ, Giraud AS, Cook GA, Skeljo MV, Yeomans ND. Indomethacin damage to rat gastric mucosa is markedly dependent on luminal pH. Clin Exp Pharmacol Physiol. 1996;23(5):432–434.
Kitchingman GK, Prichard PJ, Daneshmend TK, Walt RP, Hawkey CJ. Enhanced gastric mucosal bleeding with doses of aspirin used for prophylaxis and its reduction by ranitidine. Br J Clin Pharmacol. 1989;28(5):581–585.
Savarino V, Mela GS, Zentilin P, et al. Effect of one-month treatment with nonsteroidal antiinflammatory drugs (NSAIDs) on gastric pH of rheumatoid arthritis patients. Dig Dis Sci. 1998;43(3):459–463.
Janssen M, Baak LC, Jansen JB, Dijkmans BA, Vandenbroucke JP, Lamers CB. Effects of indomethacin on intragastric pH and meal-stimulated serum gastrin secretion in rheumatoid arthritis patients. Aliment Pharmacol Ther. 1993;7(4):393–400.
Odashima M, Otaka M, Jin M, et al. Attenuation of gastric mucosal inflammation induced by aspirin through activation of A2A adenosine receptor in rats. World J Gastroenterol. 2006;12(4):568–573.
Wallace JL, Zamuner SR, McKnight W, et al. Aspirin, but not NO-releasing aspirin (NCX-4016), interacts with selective COX-2 inhibitors to aggravate gastric damage and inflammation. Am J Physiol Gastrointest Liver Physiol. 2004;286(1):G76–G81.
Yao T, Kato M, Asaka M. Pathology of gastric mucosal injury induced by low-dose aspirin. Gi Forefr. 2007;3(1):32–36. Japanese.
Kitahora T, Guth PH. Effect of aspirin plus hydrochloric acid on the gastric mucosal microcirculation. Gastroenterology. 1987;93(4):810–817.
Shimatani T, Inoue M, Kuroiwa T, et al. Acid-suppressive efficacy of a reduced dosage of rabeprazole: comparison of 10 mg twice daily rabeprazole with 20 mg twice daily rabeprazole, 30 mg twice daily lansoprazole, and 20 mg twice daily omeprazole by 24-hr intragastric pH-metry. Dig Dis Sci. 2005;50(7):1202–1206.
Acknowledgments
This study was supported by a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (20590718) and (20014007) and grants from Ministry of Health, Labour and Welfare (19-19). The abstract of the study was presented at the Annual Meeting of the American Gastroenterological Association held in San Diego, CA, USA, in May 2008. We greatly appreciate the help of our endoscopy room staff, Ms. Chieko Matsumoto, Ms Kinuko Maruyama, Ms Satoko Takebayashi, Ms Keiko Kikuchi and Ms Hitomi Tanaka.
Conflict of Interest Statement
None of the authors have any conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Study highlights: we demonstrate for the first time that low dose aspirin induces gastric mucosal injury in the intragastric acidity-dependent manner in humans. We also show that aspirin induces dilatation of gastric subepithelial microvessels, which also depends on intragastric acidity. These endoscopic and histopathological changes can be prevented by concomitant treatment with rabeprazole, a proton-pump inhibitor.
Rights and permissions
About this article
Cite this article
Nishino, M., Sugimoto, M., Kodaira, C. et al. Relationship Between Low-Dose Aspirin-Induced Gastric Mucosal Injury and Intragastric pH in Healthy Volunteers. Dig Dis Sci 55, 1627–1636 (2010). https://doi.org/10.1007/s10620-009-0920-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0920-3