Abstract
In contemporary dentistry, resin-based materials are extensively used for the fabrication of direct and indirect restorations. As the materials available on the market feature increasingly complex chemical compositions and include a variety of ingredients with distinct physical and chemical properties, bioadhesion and biofilm formation on the surface of these materials are difficult to predict. These considerations are particularly relevant for modern resin-based materials that have been tailored with the intention to modulate the formation of biofilms on their surface. The aim of the current summary is to outline the contemporary scientific knowledge regarding the role of complex resin-based materials for bioadhesion and biofilm formation on their surface.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Over the years, resin-based materials have steadily gained more attention in dentistry, and the materials are still booming. Resin-based materials can be used for the fabrication of both direct and indirect dental restorations, which indicates that the mechanical requirements as well as the physical and chemical properties of these materials must be tailored in dependence on their range of application. Regarding their interaction of resin-based materials with microorganisms and biofilms, the role of these materials has continuously changed. While in the past resin-based materials have regularly been associated with high levels of plaque on their surface, the picture is now less clear and the situation even more complex. Bioadhesion as well as biofilm formation on the surface of dental materials is influenced by numerous effects; moreover, the results of both clinical and laboratory studies on this topic are heavily dependent on the experimental conditions applied. Nevertheless, previous investigations have identified that surface roughness, surface free energy, chemical composition, and surface topography [1, 2] have a significant effect on bioadhesion and biofilm formation on the surface of these materials. A detailed discussion on this topic can be found in Chap. 5. In situ studies are regarded as the gold standard in investigations dealing with bioadhesion and biofilm formation [3] as they allow biofilm formation under physiological conditions in situ, including the whole spectrum of microorganisms in the oral cavity. However, analysis of bioadhesion and biofilm formation in laboratory trials features the advantages of standardization and high-throughput screening. Moreover, laboratory approaches allow an estimation of bioadhesion and biofilm formation on the surface of experimental materials, which is probably why most investigations were performed under strict laboratory experimental conditions.
To date, numerous different resin-based materials differing in composition and properties are available on the market. The materials can be used either for the fabrication of direct restorations (such as resin-based composites) or for the fabrication of indirect restorations (such as removable dentures), which are usually fabricated in the dental laboratory. Regarding their impact on bioadhesion and biofilm formation in the oral cavity, these materials feature different conditions. Due to the extension of removable denture prostheses, resin-based materials for the fabrication of dentures are in close and extensive contact to gingival tissues. In contrast to resin-based materials designed for the replacement of tooth tissues, they do not have to withstand chewing forces, which coincides with a completely different chemical composition. Thus, with regard to bioadhesion, it is necessary to consider these materials from different point of views.
6.2 Resin-Based Materials for Direct Restorations
6.2.1 Introduction
Contemporary resin-based materials for the fabrication of direct dental restorations are most frequently resin-based composites (RBCs), which include materials that feature a resin matrix supplemented with a sophisticated filler fraction to minimize shrinkage and maximize wear resistance. From a clinical point of view, resin-based composites are distinguished by their consistency, ranging from flowable to condensable materials. However, for estimating the impact of these materials on bioadhesion and biofilm formation, this classification is of little value, and special attention has to be drawn on the chemical composition of these materials. In most current commercial RBC formulations, the resin matrix contains Bis-GMA (bisphenol-A-glycidyl methacrylate), which requires blending with other dimethacrylates such as urethane dimethacrylate (UDMA), triethylene glycol dimethacrylate (TEGDMA), or hydroxyethylmethacrylate (HEMA) due to its high viscosity and its unsuitability to incorporate large filler volume fractions [4]. In order to improve the internal structure of the resin-based composite and to chemically bond the hydrophobic resin matrix to the hydrophilic filler fraction, coupling agents such as silanes are employed. Most of the contemporary resin-based composite materials for direct restorations are photopolymerizable materials including photo initiators, for instance camphorquinone; some formulations have included PPD (acetyl benzoyl/1-phenyl-1,2-propanedione), Lucirin® TPO (monoacetylposphine oxide/2,4,6-trimethylbenzoyldiphenylphosphine oxide), or Irgacure® 819 (bisacylphosphine oxide/phenylbis(2,4,6-trimethylbenzoyl)phosphine oxide) [5]. The filler fraction in modern RBC formulations is complex, and usually comprises nanoscaled filler particles or, in so-called nanohybrid materials, both nano- and microscaled filler particles.
Apart from these classical RBCs, glass ionomer cements can be supplemented with a polymeric ingredient; these materials are usually defined as resin-modified glass ionomer cements (RMGIC). However, these materials are only infrequently used and, in most cases, applied in temporary restorations; thus, the focus of the current outline is set on RBCs.
6.2.2 The Role of RBC Filler Fraction on Bioadhesion and Biofilm Formation
The filler fraction accounts for the surface roughness and topography of RBCs. The relevance of surface roughness for bioadhesion and biofilm formation has extensively been discussed in the last decades. For titanium implant surfaces, Bollen and co-workers have introduced a threshold at 0.2 μm, suggesting that lower values for surface roughness than this threshold do not have an impact on biofilm formation [6]. Similar observations have been published by the Rimondini group, who introduced a threshold at Ra of 0.088 μm and Rz of 1.027 μm [7]. While it is difficult to simply transfer this threshold to other materials with a more complex composition, the conventional wisdom still is that RBCs foster biofilm formation on their surface in comparison to other tooth-colored dental materials such as ceramics or glass ionomer cements [8]. However, these results appear to be particularly true for early RBC formulations, which included large filler particles and featured only insufficient chemical bonding between resin matrix and filler fraction. These materials were difficult to polish, and as a result from hydrolytic effects and wear, the disintegration of fillers from the RBC surfaces continuously produced surfaces with high surface roughness. As microorganisms preferentially adhere to surface imperfections that provide shelter from shear stresses, this phenomenon fosters the adhesion of microorganisms. However, coinciding with a continuous improvement of the mechanical properties of RBCs, materials with very tiny filler particles have been developed and the problem of insufficient bonding between filler particles and resin matrix has largely been overcome.
Figure 6.1 illustrates the history development of filler fraction in resin-based composites. Different shapes and particle size distributions of fillers of modern resin-based composite materials were determined by scanning electron microscopy and displayed in Figure 6.2. Early investigations showed an accumulation of pellicle on filler particles and the crevice between filler and matrix. This circumstance can lead to deterioration, loss of fillers, or degradation of the filler-matrix bonding [9]. Modern RBC formulations may feature volume fractions of up to 89% filler particles [10], and recent clinical studies highlighted that the surface roughness of modern materials is far lower than the previously introduced thresholds [11]. Figure 6.3 displays the surface of a modern RBC as analyzed by atomic force microscopy. As a result, it is unlikely that further modifications will produce RBCs with relevantly diminished surface roughness. However, apart from pure surface roughness some laboratory studies have underlined that biofilm formation can be significantly impacted by the surface topography of filler-supplemented resin-based materials. Data from various groups have demonstrated that different polishing regimes can significantly impact biofilm formation on the surface of a single material, although the differences in surface roughness between these interfaces were negligible [10,11,13]. These results respond to the knowledge that has been gathered in other biological systems and underline that effective modification of the surface topography of dental materials may produce surfaces with antifouling properties [1]. For instance, the topography of shark skin is less susceptible for bioadhesion and serves as an inspiration for several micropatterned surfaces developed for the use in other fields of medicine as well as marine environments [13,14,16]. Surface structuring leads to increased water contact angles and therewith hydrophobicity. Furthermore, micro-structured surface patterns trap air, which decreases the available contact area between the substratum surface and microorganisms. Also, quorum sensing between microorganisms seems to be reduced due to topographical barriers. Frenzel and co-workers developed an approach to produce different composite surface structures to reduce bioadhesion on dental restorations. One conceivable future implementation of the advantages of biomaterials’ surfaces is engineering matrix strips which microstructure the composite during the placement of the restoration [1]. This procedure might allow the production of direct restorations with optimized surfaces that are less susceptible to biofilm formation.
The development of the state of the art of dental composite formulations based on filler particle modifications, based on Ferracane [5], p. 32
6.2.3 The Role of RBC Surface Properties on Bioadhesion and Biofilm Formation
Apart from surface roughness, surface free energy is regarded as one of the major factors that impact biofilm formation on the surface of dental materials. While the underlying thermodynamical principles are complex, a simple rule of thumb is that surfaces with low surface free energy attract less plaque than surfaces with high surface free energy. This relation has been proven for a variety of simple polymeric materials such as polytetrafluorethylene (PFTE) or polyethylene (PE) in several in situ experiments [2]; however, the relation between surface free energy and biofilm formation is more complex and less clear for complex materials such as RBCs. RBCs consist of chemically distinct ingredients with different surface free energies, which finally results in a complex surface that includes areas with both low (matrix) and high (fillers) surface free energy (cf. Fig. 6.1). Thus, relations between surface free energy and microbial adhesion and subsequent biofilm formation are hard to establish, which might serve as an explanation why conflicting results have been reported regarding the role of the surface free energy of a RBC on biofilm formation [17, 18]. In some laboratory studies, biofilm formation was lower on the surface of a RBC material with a distinct hydrophobic resin matrix based on siloranes than on the surface of conventionally applied methacrylate-based materials [19, 20]. However, in situ studies did not support the results of the laboratory investigations [21], which underlines that the results from laboratory approaches cannot be simply transferred into clinical settings. As the proportion of the resin matrix on the surface of a RBC is low due to the abundancy of the filler fraction, it is likely that differences in surface free energy resulting from a variation of the resin matrix may only affect bioadhesion and biofilm formation under controlled and very strict experimental conditions. Judging from the current evidence, it appears that surface free energy cannot serve as a reliable predictor of bioadhesion and biofilm formation on the surface of complex RBCs. Overall, the importance of RBC surface properties on bioadhesion seems to decrease with increasing biofilm formation time and growing biofilm layer [22].
6.2.4 The Role of the RBC Resin Matrix on Bioadhesion and Biofilm Formation
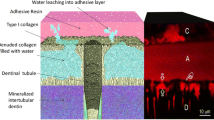
In comparison to filler fraction, only little effort has so far been made to identify and elucidate the interaction of the resin matrix with bioadhesion. While it is clear from the history of the filler fraction in RBCs that the proportion of the resin matrix in the surface of RBCs has gradually diminished, some researchers have highlighted that the resin matrix has a relevant impact on biofilm formation on the surface of RBCs [11]. Brambilla and co-workers have shown that Streptococcus mutans biofilm formation decreases with increasing curing time, which has been attributed to a decreased concentration of unpolymerized monomers [23]. Previous studies have also highlighted that the colonization of specimens fabricated from different experimental resins with Streptococcus mutans is different despite similar surface properties [24], which underlines the existence of an effect of the resin matrix on bioadhesion. However, the exact mechanisms which are responsible for these results are not yet clear. It is well known that polymerization of resin-based materials is never complete, and modern mixtures feature a degree of conversion ranging around 60–70%. Leakage of unpolymerized resin monomers as well as biodegradation of the resin matrix by oral microorganisms might have an impact on oral microorganisms [11]. In the past, it has been suggested that monomers such as UDMA, EGDMA, DEGDMA, and TEGDMA may promote growth and proliferation of cariogenic microorganisms [25, 26]; however, recent publications could not corroborate this hypothesis [27].
6.2.5 Modifications of RBCs with Antimicrobial Agents
Several approaches to equip RBCs with antimicrobial properties have been described, including the incorporation of agents like silver ions [28, 29], zinc oxide nanoparticles [30], quaternary ammonium derivatives [31], chlorhexidine acetate [32], and many others. Antimicrobial agents delay, reduce, or avoid biofilm formation through direct contact or leaching. However, these agents may lead to impaired mechanical properties and decreased degrees of conversion. Also, the antibacterial effects are often temporary [33], featuring a burst effect followed by a rapid decrease. Early studies indicated an antimicrobial effect on Streptococcus mutans by quaternary ammonium polyethylenimine nanoparticles for at least 1 month [31] and silver-supplemented materials for 6 months [34]. At the same time, little or no release of silver or quaternary ammonium was observed. Moreover, Yoshida and co-workers reported that supplementing RBCs with different silver agents produced materials with very distinct mechanical properties [34], which underlines that it is not indifferent to the antimicrobial agent used. With regard to this aspect, it has been reported that quaternary ammonium polyethylenimine nanoparticles do not compromise the mechanical properties of a supplemented RBC [31]. Other studies suggest even higher mechanical strength (diametral tensile strength, fracture toughness) in RBCs supplemented with titanium and silver-tin-copper filler particles [35]. More information on this can be found in Chaps. 8, 9, and 10.
6.2.6 The Role of Degradation of RBCs by Microorganisms: A Circulus Vitiosus?
However, although no simple relations between the composition and availability of resin monomers and bioadhesion have yet been identified, it is undoubted that oral microorganisms interact with the matrix constituents of RBCs. It has been highlighted that the presence of biofilms on the surface of RBCs leads to deterioration of the RBC surface [35,36,38]. This phenomenon is due to biodegradation of the resin matrix, an effect that has frequently been addressed in dental materials science and is caused by esterases from cariogenic bacteria [39]. As acids may also provoke degradation of RBCs [40], it is likely that acids produced by cariogenic microorganisms can also affect the surface of RBCs. Recent literature indicates that deterioration of RBC surfaces by microorganisms is dependent on the bacterial strain as well as the composition of the resin matrix. Bis-GMA-free formulations did not show changes in surface roughness after exposition to cariogenic streptococci, while Bis-GMA-containing RBC formulations were significantly affected [41]. Results from in situ studies indicate that RBCs with urethane dimethacrylate matrix are less vulnerable against deterioration than RBCs with mixed matrices (UDMA, Bis-GMA, and DDMA). Moreover, an accumulation of pellicle was observed on filler particles and between filler and the matrix [9]. Simple monospecies biofilms including cariogenic microorganisms such as Streptococcus mutans seem to have a more distinct effect on the surface than multispecies biofilms [41]. While recent studies identified only slight increases in surface roughness in a nanometer range after exposition to the various biofilms [41], early studies showed that the surface of RBCs is relevantly affected [37, 39]. Thus, it is not yet clear as to how far biodeterioration of RBCs by microorganisms produces an impaired RBC surface that substantially fosters subsequent bioadhesion. While current scientific evidence is still scarce, it might be recommended to regularly polish RBC restorations in order to minimize a potential negative effect of a roughened surface.
6.3 Resin-Based Materials for Indirect Restorations
6.3.1 Introduction
Resin-based materials for indirect dental restorations include materials for the fabrication of removable dentures as well as polymer-based materials for the CAD/CAM fabrication of indirect restorations such as inlays, partial crowns, crowns, and fixed-partial dentures.
Resin-based materials have been used for decades for the fabrication of removable dental prostheses. For these applications, poly(methyl methacrylate) (PMMA) is still regarded as the material of choice, although some other materials have been introduced as well. Alternative denture materials can be divided into methacrylate-containing and methacrylate-free materials (cf. Table 6.1/Fig. 6.4). The latter group features the advantages of little elution of monomers and high biocompatibility. Thus, they are particularly suitable in patients with allergies. At the same time, these materials are difficult to repair and to reline since they are chemically inert [42]. Some of the materials are very flexible and can be used in patients with microstomia (e.g., polyamide).
Further innovations in this field include machinable PMMA-based materials for CAD/CAM fabrication of denture bases. Moreover, innovative materials from the family of poly(aryl ether ketone) (PAEK) such as poly(ether ether ketone) (PEEK) or poly(ether ketone ketone) (PEKK) have been introduced in the last years. In contrast to PMMA-based dentures, these polymers feature the advantages of CAD/CAM fabrication, improved mechanical properties [43], low allergenic potential [44], as well as low weight [45]. In case of PEEK or PEKK, even complex tooth- or implant-supported denture prostheses can be fabricated from the polymeric material without a supporting alloy framework (cf. Fig. 6.5) [45, 46]. PEEK and PEKK differ in their ratio of ketone and ether groups. As PEKK contains more ketone groups it is slightly stiffer than PEEK. Its mechanical, optical, and chemical properties are similar to PEEK [47]. Since PEEK was introduced earlier into the dental market than PEKK and is available for different fabrication techniques (e.g., heat pressing, CAD/CAM) it is more popular than PEKK. Therefore, studies on PEKK are still scarce. While PEKK is supplemented with a filler fraction of about 10 wt% titanium dioxide filler particles, PEEK is available both without and with a filler fraction of up to 30 wt% titanium dioxide filler particles. These fillers enhance the mechanical properties of PAEK but do also account for their grayish appearance. Generally, PAEK materials feature higher stability, rigidity, and resistance to hydrolysis compared to other resin-based materials like PMMA [48, 49]. Depending on the proportion of crystalline and amorphous contributions to the PAEK formulation, its chemical and optical properties differ: While a higher percentage of crystalline parts promotes resistance to acids, alkalis, and organic solvents, a higher proportion of the amorphous phase coincides with enhanced translucency [50]. In order to combine good chemical and aesthetic properties, PAEK restorations with a higher percentage of crystalline parts can be veneered or lined using resin-based materials [46, 51]. Crystalline PEKK, which shows higher flexural and tensile strength, is preferably used for the fabrication of crowns and fixed dental prosthesis, while amorphous PEKK can be applied for the fabrication of removable prosthesis [52]. Stawarczyk and co-workers identified increased fracture loads for milled PEEK restorations compared to those which had been pressed from granular. Materials which were pressed from industrially fabricated pellets and milled PEEK restorations showed spontaneous and brittle fractures in the pontic areas without deformation, whereas pressed materials from granular rather deformed than fractured [53]. Overall, PEEK restorations withstand high breaking loads (1300 N), which are far higher than average masticatory forces (400 N) and three times higher than fracture loads of other machinable resin-based materials like PMMA [54, 55].
6.3.2 Biofilms and Resin-Based Materials for the Fabrication of Removable Dentures
Although biofilm-associated diseases such as caries or periodontitis are almost irrelevant in edentulous patients, biofilm formation on the surface of dentures is a relevant issue. Manual skills decrease with age; as a result, dentures are frequently not cleaned adequately. In hospitalized patients, the time available for oral care by the nursing staff is limited, too, which regularly results in poorly cleaned denture prostheses (cf. Fig. 6.7). As removable dentures cover large areas of the edentulous gum tissues, these circumstances make them an ideal and extensive reservoir for biofilms, which are a relevant risk factor for local and systemic implications. Denture-related stomatitis constitutes a common local biofilm-associated disease in denture wearers with a prevalence of 15% to over 70% [56]. Candida albicans plays a major role in the pathogenesis of denture-related stomatitis [57]. This fungus has three morphological forms: blastospores, hyphae, and pseudohyphae. The morphological transformation of C. albicans from blastospores to hyphae coincides with a maturing process of the biofilm and induces an increased pathogenicity and virulence [56,57,59]. This transformation seems to be regulated by secreted proteases and their activity [60]. Aspartate proteinases are among the most frequently discussed virulence factors of C. albicans, as they contribute decisively to the degradation of host proteins and promote the invasion of the fungus into the oral mucous membranes as well as the development of Candida-associated prosthetic stomatitis [61]. C. albicans cells organized in biofilms secrete higher levels of aspartate proteases than planktonic cells [62]. Moreover, the activity of the proteinases correlates with the severity of denture stomatitis [60]. Since the risk of tissue invasion of C. albicans increases with the presence of fungal hyphae in mature biofilms, regular oral and denture hygiene is essential [59, 63]. Besides oral hygiene, surface properties as well as surface topography of dental materials shall be optimized in order to minimize fungal and microbial adherence. The substratum surface properties may promote a genetic response which leads to the transformation from blastospores to hyphae [63,64,66]. Apart from that, high polar contribution to surface free energy increases the proliferation of C. albicans, e.g., on urethane dimethacrylate (UDMA)-based denture base materials and soft denture liners (siloxane based) [67]. C. albicans hyphae seem to adhere preferentially to hydrophobic rather than hydrophilic surfaces [64, 68]. Moreover, porosities in the denture base foster microbial and fungal adherence by increasing the available surface [69]. An increased number of hyphae was observed in biofilms on siloxane-based soft denture liners compared to PMMA- and UDMA-based denture base materials [59]. Fungal proliferation promotes the deterioration of the surface of denture liners, which may coincide with further irritations of the mucosa [66]. Therefore, long-term use of soft denture liners cannot be recommended. Moreover, denture age and continuous denture wearing are important factors in the development of denture-related stomatitis [57]. Figure 6.6 illustrates differences in surface appearance between new and aged denture bases.
For the relining of denture prostheses, materials based on acrylate or silicone (soft denture liner) can be used. The physical properties of relining materials seem to affect biofilm formation significantly [59, 70]: For instance, C. albicans preferentially adheres to hydrophobic rather than hydrophilic surfaces [64]. Hence, hydrophilic coatings of denture surfaces might decrease the attachment of hydrophobic fungal cells like those of C. albicans [68]. Further investigations showed that C. albicans adherence on polyamides is higher than on PMMA [71]. Materials with smooth surfaces as well as low surface free energy feature less fungal-microbial adherence than materials with rough surfaces and high surface free energy [22]. Surface properties seem to influence especially the early fungal-microbial colonization on dental materials; with maturation of the biofilms, the differences in biofilm formation between various materials gradually diminish [22].
Apart from biofilm-induced diseases such as denture-related stomatitis biofilms on removable denture prostheses may also have other systemic consequences. As respiratory pathogenic microorganisms have been identified in denture plaque [72, 73], denture wearing has been associated with the occurrence of pneumonias in elderly patients [74, 75]. Pneumonia is a common infection in elderly people and constitutes the most frequent cause of mortality from nosocomial infection in elderly patients with a mortality rate up to 25% [76, 77]. Aspiration of oropharyngeal bacteria into the lungs due to dysphagia and nocturnal denture wearing as well as weakened host defense mechanisms may lead to respiratory infections [78, 79]. Especially for hospitalized patients it is often difficult to maintain a sufficient oral care due to impaired cleaning abilities or limited help provided by the nursing staff (cf. Fig. 6.7) [74]. Moreover, elderly patients have difficulties in accessing professional dental care and consequently appear at the dental office when having denture problems or pain [74, 79]. Thus, regular oral care is required [72, 77, 80], which includes the mechanical removal of denture plaque. Figure 6.7 displays a removable denture prosthesis with extensive accumulation of biofilms. Several studies showed that oral hygiene may have a positive effect on morbidity and mortality from pneumonia: One of ten deaths due to pneumonia in nursing homes may be prevented by improving oral hygiene [77]. Another approach would be the development of materials which feature as little bioadhesion as possible. However, with regard to respiratory microorganisms no scientific data are currently available regarding an impact of the substratum material.
6.3.3 Biofilms on Resin-Based Materials for Fixed Dental Restorations
Scientific data on the formation of biofilms on these materials is limited, as most of the materials have only recently been introduced into the dental market. Nevertheless, it might be possible that resin-based materials polymerized in an industrial setting feature reduced biofilm formation in comparison to their counterparts which are polymerized under clinical conditions. It is conceivable that milled restorations and restorations made by heat pressing from industrially fabricated pellets might show lower biofilm formation due to higher homogeneity as they also feature better mechanical properties compared to those of non-industrially fabricated materials [53]. A recent study contrasted several restorative materials for CAD/CAM fabrication regarding biofilm formation. Interestingly, the acrylate-based material featured significantly lower biofilm formation in comparison to the polymer-infiltrated ceramic as well as zirconia [81]. The authors assumed that materials with a higher ratio of organic constituents (polymer) feature less biofilm formation than materials with a higher ratio of inorganic constituents (ceramic). This conclusion is surprising as several researchers have reported conflicting results [81,82,84]. However, some studies also confirmed lower biofilm adhesion on composite than, e.g., on ceramic surfaces [85]. Certainly, these findings depend on the used type of ceramic or polymer, its finishing, the used bacteria species, and, finally, the study design. Hence, these results may not be easily transferred into clinical considerations, underlining the relevance of well-designed and adequate in vivo studies.
References
Frenzel N, Maenz S, Sanz Beltrán V, Völpel A, Heyder M, Sigusch BW, et al. Template assisted surface microstructuring of flowable dental composites and its effect on microbial adhesion properties. Dent Mater. 2016;32(3):476–87. https://doi.org/10.1016/j.dental.2015.12.016.
Teughels W, van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006;17(Suppl 2):68–81. https://doi.org/10.1111/j.1600-0501.2006.01353.x.
Hannig C, Hannig M. The oral cavity—a key system to understand substratum-dependent bioadhesion on solid surfaces in man. Clin Oral Investig. 2009;13(2):123–39. https://doi.org/10.1007/s00784-008-0243-3.
Hahnel S, Dowling AH, El-Safty S, Fleming GJP. The influence of monomeric resin and filler characteristics on the performance of experimental resin-based composites (RBCs) derived from a commercial formulation. Dent Mater. 2012;28(4):416–23. https://doi.org/10.1016/j.dental.2011.11.016.
Ferracane JL. Resin composite—state of the art. Dent Mater. 2011;27(1):29–38. https://doi.org/10.1016/j.dental.2010.10.020.
Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997;13(4):258–69.
Rimondini L, Farè S, Brambilla E, Felloni A, Consonni C, Brossa F, Carrassi A. The effect of surface roughness on early in vivo plaque colonization on titanium. J Periodontol. 1997;68(6):556–62. https://doi.org/10.1902/jop.1997.68.6.556.
Svanberg M, Mjör IA, Orstavik D. Mutans streptococci in plaque from margins of amalgam, composite, and glass-ionomer restorations. J Dent Res. 1990;69(3):861–4. https://doi.org/10.1177/00220345900690030601.
Gröger G, Rosentritt M, Behr M, Schröder J, Handel G. Dental resin materials in vivo—TEM results after one year: a pilot study. J Mater Sci Mater Med. 2006;17(9):825–8. https://doi.org/10.1007/s10856-006-9841-2.
Wang R, Habib E, Zhu XX. Evaluation of the filler packing structures in dental resin composites: From theory to practice. Dent Mater. 2018;34(7):1014–23. https://doi.org/10.1016/j.dental.2018.03.022.
Ionescu A, Wutscher E, Brambilla E, Schneider-Feyrer S, Giessibl FJ, Hahnel S. Influence of surface properties of resin-based composites on in vitro Streptococcus mutans biofilm development. Eur J Oral Sci. 2012;120(5):458–65. https://doi.org/10.1111/j.1600-0722.2012.00983.x.
Hahnel S, Wastl DS, Schneider-Feyrer S, Giessibl FJ, Brambilla E, Cazzaniga G, Ionescu A. Streptococcus mutans biofilm formation and release of fluoride from experimental resin-based composites depending on surface treatment and S-PRG filler particle fraction. J Adhes Dent. 2014;16(4):313–21. https://doi.org/10.3290/j.jad.a31800.
Park JW, Song CW, Jung JH, Ahn SJ, Ferracane JL. The effects of surface roughness of composite resin on biofilm formation of Streptococcus mutans in the presence of saliva. Oper Dent. 2012;37(5):532–9. https://doi.org/10.2341/11-371-L.
Mann EE, Manna D, Mettetal MR, May RM, Dannemiller EM, Chung KK, et al. Surface micropattern limits bacterial contamination. Antimicrob Resist Infect Control. 2014;3:28. https://doi.org/10.1186/2047-2994-3-28.
Reddy ST, Chung KK, McDaniel CJ, Darouiche RO, Landman J, Brennan AB. Micropatterned surfaces for reducing the risk of catheter-associated urinary tract infection: an in vitro study on the effect of sharklet micropatterned surfaces to inhibit bacterial colonization and migration of uropathogenic Escherichia coli. J Endourol. 2011;25(9):1547–52. https://doi.org/10.1089/end.2010.0611.
Schumacher JF, Long CJ, Callow ME, Finlay JA, Callow JA, Brennan AB. Engineered nanoforce gradients for inhibition of settlement (attachment) of swimming algal spores. Langmuir. 2008;24(9):4931–7. https://doi.org/10.1021/la703421v.
Hahnel S, Ionescu AC, Cazzaniga G, Ottobelli M, Brambilla E. Biofilm formation and release of fluoride from dental restorative materials in relation to their surface properties. J Dent. 2017;60:14–24.
Ionescu AC, Hahnel S, Cazzaniga G, Ottobelli M, Braga RR, Rodrigues MC, Brambilla E. Streptococcus mutans adherence and biofilm formation on experimental composites containing dicalcium phosphate dihydrate nanoparticles. J Mater Sci Mater Med. 2017;28(7):108.
Brambilla E, Ionescu A, Cazzaniga G, Ottobelli M. Influence of light-curing parameters on biofilm development and flexural strength of a silorane-based composite. Oper Dent. 2016;41(2):219–27. https://doi.org/10.2341/14-279-L.
Buergers R, Schneider-Brachert W, Hahnel S, Rosentritt M, Handel G. Streptococcal adhesion to novel low-shrink silorane-based restorative. Dent Mater. 2009;25(2):269–75. https://doi.org/10.1016/j.dental.2008.07.011.
Claro-Pereira D, Sampaio-Maia B, Ferreira C, Rodrigues A, Melo LF, Vasconcelos MR. In situ evaluation of a new silorane-based composite resin’s bioadhesion properties. Dent Mater. 2011;27(12):1238–45. https://doi.org/10.1016/j.dental.2011.08.401.
Hahnel S, Wieser A, Lang R, Rosentritt M. Biofilm formation on the surface of modern implant abutment materials. Clin Oral Implants Res. 2015;26(11):1297–301. https://doi.org/10.1111/clr.12454.
Brambilla E, Gagliani M, Ionescu A, Fadini L, García-Godoy F. The influence of light-curing time on the bacterial colonization of resin composite surfaces. Dent Mater. 2009;25(9):1067–72. https://doi.org/10.1016/j.dental.2009.02.012.
Hahnel S, Rosentritt M, Buergers R, Handel G. Surface properties and in vitro Streptococcus mutans adhesion to dental resin polymers. J Mater Sci Mater Med. 2008;19(7):2619–27. https://doi.org/10.1007/s10856-007-3352-7.
Hansel C, Leyhausen G, Mai UE, Geurtsen W. Effects of various resin composite (co)monomers and extracts on two caries-associated micro-organisms in vitro. J Dent Res. 1998;77(1):60–7. https://doi.org/10.1177/00220345980770010601.
Kawai K, Torii M, Tuschitani Y. Effect of resin components on the growth of Streptococcus mutans. J Osaka Univ Dent Sch. 1988;28:161–70.
Nedeljkovic I, Yoshihara K, de Munck J, Teughels W, van Meerbeek B, van Landuyt KL. No evidence for the growth-stimulating effect of monomers on cariogenic Streptococci. Clin Oral Investig. 2017;21(5):1861–9. https://doi.org/10.1007/s00784-016-1972-3.
Buergers R, Eidt A, Frankenberger R, Rosentritt M, Schweikl H, Handel G, Hahnel S. The anti-adherence activity and bactericidal effect of microparticulate silver additives in composite resin materials. Arch Oral Biol. 2009;54(6):595–601. https://doi.org/10.1016/j.archoralbio.2009.03.004.
Yamamoto K, Ohashi S, Aono M, Kokubo T, Yamada I, Yamauchi J. Antibacterial activity of silver ions implanted in SiO2 filler on oral streptococci. Dent Mater. 1996;12(4):227–9. https://doi.org/10.1016/S0109-5641(96)80027-3.
Tavassoli Hojati S, Alaghemand H, Hamze F, Ahmadian Babaki F, Rajab-Nia R, Rezvani MB, et al. Antibacterial, physical and mechanical properties of flowable resin composites containing zinc oxide nanoparticles. Dent Mater. 2013;29(5):495–505. https://doi.org/10.1016/j.dental.2013.03.011.
Beyth N, Yudovin-Farber I, Bahir R, Domb AJ, Weiss EI. Antibacterial activity of dental composites containing quaternary ammonium polyethylenimine nanoparticles against Streptococcus mutans. Biomaterials. 2006;27(21):3995–4002. https://doi.org/10.1016/j.biomaterials.2006.03.003.
Leung D, Spratt DA, Pratten J, Gulabivala K, Mordan NJ, Young AM. Chlorhexidine-releasing methacrylate dental composite materials. Biomaterials. 2005;26(34):7145–53. https://doi.org/10.1016/j.biomaterials.2005.05.014.
Jandt KD, Sigusch BW. Future perspectives of resin-based dental materials. Dent Mater. 2009;25(8):1001–6. https://doi.org/10.1016/j.dental.2009.02.009.
Yoshida K, Tanagawa M, Atsuta M. Characterization and inhibitory effect of antibacterial dental resin composites incorporating silver-supported materials. J Biomed Mater Res. 1999;47(4):516–22.
Jandt KD, Al-Jasser AMO, Al-Ateeq K, Vowles RW, Allen GC. Mechanical properties and radiopacity of experimental glass-silica-metal hybrid composites. Dent Mater. 2002;18(6):429–35.
Beyth N, Bahir R, Matalon S, Domb AJ, Weiss EI. Streptococcus mutans biofilm changes surface-topography of resin composites. Dent Mater. 2008;24(6):732–6. https://doi.org/10.1016/j.dental.2007.08.003.
Fúcio SBP, Carvalho FG, Sobrinho LC, Sinhoreti MAC, Puppin-Rontani RM. The influence of 30-day-old Streptococcus mutans biofilm on the surface of esthetic restorative materials—an in vitro study. J Dent. 2008;36(10):833–9. https://doi.org/10.1016/j.jdent.2008.06.002.
Padovani GC, Fúcio SBP, Ambrosano GMB, Sinhoreti MAC, Puppin-Rontani RM. In situ surface biodegradation of restorative materials. Oper Dent. 2014;39(4):349–60. https://doi.org/10.2341/13-089-C.
Bourbia M, Ma D, Cvitkovitch DG, Santerre JP, Finer Y. Cariogenic bacteria degrade dental resin composites and adhesives. J Dent Res. 2013;92(11):989–94. https://doi.org/10.1177/0022034513504436.
Borges MAP, Matos IC, Mendes LC, Gomes AS, Miranda MS. Degradation of polymeric restorative materials subjected to a high caries challenge. Dent Mater. 2011;27(3):244–52. https://doi.org/10.1016/j.dental.2010.10.009.
Nedeljkovic I, de Munck J, Ungureanu A-A, Slomka V, Bartic C, Vananroye A, et al. Biofilm-induced changes to the composite surface. J Dent. 2017;63:36–43. https://doi.org/10.1016/j.jdent.2017.05.015.
Fueki K, Ohkubo C, Yatabe M, Arakawa I, Arita M, Ino S, et al. Clinical application of removable partial dentures using thermoplastic resin. Part II: material properties and clinical features of non-metal clasp dentures. J Prosthodont Res. 2014;58(2):71–84.
Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodont Res. 2016;60(1):12–9. https://doi.org/10.1016/j.jpor.2015.10.001.
Zoidis P, Papathanasiou I, Polyzois G. The use of a modified poly-ether-ether-ketone (PEEK) as an alternative framework material for removable dental prostheses. A clinical report. J Prosthodont. 2016;25(7):580–4. https://doi.org/10.1111/jopr.12325.
Hahnel S, Scherl C, Rosentritt M. Interim rehabilitation of occlusal vertical dimension using a double-crown-retained removable dental prosthesis with polyetheretherketone framework. J Prosthet Dent. 2018;119(3):315–8. https://doi.org/10.1016/j.prosdent.2017.02.017.
Stawarczyk B, Thrun H, Eichberger M, Roos M, Edelhoff D, Schweiger J, Schmidlin PR. Effect of different surface pretreatments and adhesives on the load-bearing capacity of veneered 3-unit PEEK FDPs. J Prosthet Dent. 2015;114(5):666–73. https://doi.org/10.1016/j.prosdent.2015.06.006.
Silla M, Eichenberger M, Stawarczyk B. Polyetherketonketon (PEKK) als Restaurationswerkstoff in der modernen Zahnmedizin: eine Literaturübersicht. Quintessenz Zahntech. 2016;42(2):176–90.
Kurtz SM, Devine JN. Biomaterials. 2007;28(32):4845–69. https://doi.org/10.1016/j.biomaterials.2007.07.013.
Tetelman ED, Babbush CA. A new transitional abutment for immediate aesthetics and function. Implant Dent. 2008;17(1):51–8. https://doi.org/10.1097/ID.0b013e318167648c.
Rosentritt M, Ilie N, Lohbauer U, editors. Werkstoffkunde in der Zahnmedizin. Moderne Materialien und Technologien. Stuttgart: Georg Thieme Verlag; 2018.
Rosentritt M, Preis V, Behr M, Sereno N, Kolbeck C. Shear bond strength between veneering coposite and PEEK after different surface modifications. Clin Oral Investig. 2015;19(3):739–44. https://doi.org/10.1007/s00784-014-1294-2.
Fuhrmann G, Steiner M, Freitag-Wolf S, Kern M. Resin bonding to three types of polyaryletherketones (PAEKs)-durability and influence of surface conditioning. Dent Mater. 2014;30(3):357–63. https://doi.org/10.1016/j.dental.2013.12.008.
Stawarczyk B, Eichberger M, Uhrenbacher J, Wimmer T, Edelhoff D, Schmidlin PR. Three-unit reinforced polyetheretherketone composite FDPs: influence of fabrication method on load-bearing capacity and failure types. Dent Mater J. 2015;34(1):7–12. https://doi.org/10.4012/dmj.2013-345.
Helkimo E, Carlsson GE, Helkimo M. Bite force and state of dentition. Acta Odontol Scand. 1977;35(6):297–303.
Stawarczyk B, Ender A, Trottmann A, Özcan M, Fischer J, Hämmerle CHF. Load-bearing capacity of CAD/CAM milled polymeric three-unit fixed dental prostheses: effect of aging regimens. Clin Oral Investig. 2012;16(6):1669–77. https://doi.org/10.1007/s00784-011-0670-4.
Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J. Prosthodont. 2011;20(4):251–60.
Bilhan H, Sulun T, Erkose G, Kurt H, Erturan Z, Kutay O, Bilgin T. The role of Candida albicans hyphae and Lactobacillus in denture-related stomatitis. Clin Oral Investig. 2009;13(4):363–8. https://doi.org/10.1007/s00784-008-0240-6.
Leberer E, Ziegelbauer K, Schmidt A, Harcus D, Dignard D, Ash J, et al. Virulence and hyphal formation of Candida albicans require the Ste20p-like protein kinase CaCla4p. Curr Biol. 1997;7(8):539–46. https://doi.org/10.1016/S0960-9822(06)00252-1.
Susewind S, Lang R, Hahnel S. Biofilm formation and Candida albicans morphology on the surface of denture base materials. Mycoses. 2015;58(12):719–27. https://doi.org/10.1111/myc.12420.
Ramage G, Coco B, Sherry L, Bagg J, Lappin DF. In vitro Candida albicans biofilm induced proteinase activity and SAP8 expression correlates with in vivo denture stomatitis severity. Mycopathologia. 2012;174(1):11–9. https://doi.org/10.1007/s11046-012-9522-2.
Hube B, Albrecht A, Bader O, Beinhauer S, Felk A, Fradin C, et al. Pathogenitätsfaktoren bei Pilzinfektionen. Bundesgesundheitsbl—Gesundheitsforsch—Gesundheitsschutz. 2002;45:159–65.
Mendes A, Mores AU, Carvalho AP, Rosa RT, Samaranayake LP, Rosa EAR. Candida albicans biofilms produce more secreted aspartyl protease than the planktonic cells. Biol Pharm Bull. 2007;30(9):1813–5. https://doi.org/10.1248/bpb.30.1813.
Gow NAR, van de Veerdonk FL, Brown AJP, Netea MG. Candida albicans morphogenesis and host defence: discriminating invasion from colonization. Nat Rev Microbiol. 2011;10(2):112–22. https://doi.org/10.1038/nrmicro2711.
ten Cate JM, Klis FM, Pereira-Cenci T, Crielaard W, de Groot PWJ. Molecular and cellular mechanisms that lead to Candida biofilm formation. J Dent Res. 2009;88(2):105–15. https://doi.org/10.1177/0022034508329273.
Douglas LJ. Candida biofilms and their role in infection. Trends Microbiol. 2003;11(1):30–6. https://doi.org/10.1016/S0966-842X(02)00002-1.
Pereira-Cenci T, Deng DM, Kraneveld EA, Manders EMM, Del Bel Cury AA, ten Cate JM, Crielaard W. The effect of Streptococcus mutans and Candida glabrata on Candida albicans biofilms formed on different surfaces. Arch Oral Biol. 2008;53(8):755–64. https://doi.org/10.1016/j.archoralbio.2008.02.015.
Koch C, Bürgers R, Hahnel S. Candida albicans adherence and proliferation on the surface of denture base materials. Gerodontology. 2013;30(4):309–13. https://doi.org/10.1111/ger.12056.
Yoshijima Y, Murakami K, Kayama S, Liu D, Hirota K, Ichikawa T, Miyake Y. Effect of substrate surface hydrophobicity on the adherence of yeast and hyphal Candida. Mycoses. 2010;53(3):221–6. https://doi.org/10.1111/j.1439-0507.2009.01694.x.
Gomes AS, Sampaio-Maia B, Vasconcelos M, Fonesca PA, Figueiral H. In situ evaluation of the microbial adhesion on a hard acrylic resin and a soft liner used in removable prostheses. Int J Prosthodont. 2015;28(1):65–71. https://doi.org/10.11607/ijp.4080.
Tari BF, Nalbant D, Al Dogruman F, Kustimur S. Surface roughness and adherence of Candida albicans on soft lining materials as influenced by accelerated aging. J Contemp Dent Pract. 2007;8(5):18–25.
Freitas-Fernandes FS, Cavalcanti YW, Ricomini Filho AP, Silva WJ, Del Bel Cury AA, Bertolini MM. Effect of daily use of an enzymatic denture cleanser on Candida albicans biofilms formed on polyamide and poly(methyl methacrylate) resins: an in vitro study. J Prosthet Dent. 2014;112(6):1349–55. https://doi.org/10.1016/j.prosdent.2014.07.004.
O’Donnell LE, Smith K, Williams C, Nile CJ, Lappin DF, Bradshaw D, et al. Dentures are a reservoir for respiratory pathogens. J Prosthodont. 2016;25(2):99–104. https://doi.org/10.1111/jopr.12342.
Urushibara Y, Ohshima T, Sato M, Hayashi Y, Hayakawa T, Maeda N, Ohkubo C. An analysis of the biofilms adhered to framework alloys using in vitro denture plaque models. Dent Mater J. 2014;33(3):402–14.
El-Solh AA. Association between pneumonia and oral care in nursing home residents. Lung. 2011;189(3):173–80. https://doi.org/10.1007/s00408-011-9297-0.
Iinuma T, Arai Y, Abe Y, Takayama M, Fukumoto M, Fukui Y, et al. Denture wearing during sleep doubles the risk of pneumonia in the very elderly. J Dent Res. 2015;94(3 Suppl):28S–36S. https://doi.org/10.1177/0022034514552493.
Niederman MS. Nosocomial pneumonia in the elderly patient. Chronic care facility and hospital considerations. Clin Chest Med. 1993;14(3):479–90.
Sjögren P, Nilsson E, Forsell M, Johansson O, Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56(11):2124–30. https://doi.org/10.1111/j.1532-5415.2008.01926.x.
Mojon P. Oral health and respiratory infection. J Can Dent Assoc. 2002;68(6):340–5.
Scannapieco FA, Papandonatos GD, Dunford RG. Associations between oral conditions and respiratory disease in a national sample survey population. Ann Periodontol. 1998;3(1):251–6. https://doi.org/10.1902/annals.1998.3.1.251.
Tada A, Miura H. Prevention of aspiration pneumonia (AP) with oral care. Arch Gerontol Geriatr. 2012;55(1):16–21. https://doi.org/10.1016/j.archger.2011.06.029.
Astasov-Frauenhoffer M, Glauser S, Fischer J, Schmidli F, Waltimo T, Rohr N. Biofilm formation on restorative materials and resin composite cements. Dent. Mater. 2018; https://doi.org/10.1016/j.dental.2018.08.300.
Aykent F, Yondem I, Ozyesil AG, Gunal SK, Avunduk MC, Ozkan S. Effect of different finishing techniques for restorative materials on surface roughness and bacterial adhesion. J Prosthet Dent. 2010;103(4):221–7. https://doi.org/10.1016/S0022-3913(10)60034-0.
Eick S, Glockmann E, Brandl B, Pfister W. Adherence of Streptococcus mutans to various restorative materials in a continuous flow system. J Oral Rehabil. 2004;31(3):278–85. https://doi.org/10.1046/j.0305-182X.2003.01233.x.
Tanner J, Robinson C, Söderling E, Vallittu P. Early plaque formation on fibre-reinforced composites in vivo. Clin Oral Investig. 2005;9(3):154–60.
Hauser-Gersprach I, Kulik EM, Weiger R, Decker E-M, von Ohle C, Meyer J. Adhesion of Streptococcus sanguinis to dental implant and restorative materials in vitro. Dent Mater J. 2007;26(3):361–6. https://doi.org/10.4012/dmj.26.361.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Günther, E., Fuchs, F., Hahnel, S. (2021). Complex Polymeric Materials and Their Interaction with Microorganisms. In: Ionescu, A.C., Hahnel, S. (eds) Oral Biofilms and Modern Dental Materials . Springer, Cham. https://doi.org/10.1007/978-3-030-67388-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-67388-8_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67387-1
Online ISBN: 978-3-030-67388-8
eBook Packages: MedicineMedicine (R0)