Abstract
Objective
This study tested the fracture load of milled and conventionally fabricated polymeric and glass-ceramic three-unit fixed dental prostheses (FDPs) after aging.
Materials and methods
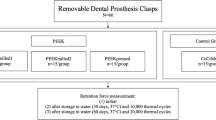
FDPs were fabricated (N = 1,050) from four computer-aided design and computer-aided manufacturing (CAD/CAM) resins: (1) AT (artBlock Temp); (2) TC (Telio CAD); (3) ZP (ZENO PMMA); (4) CT (CAD-Temp); two conventionally fabricated resins, (5) IES (integral esthetic press), (6) CMK (CronMix K), and a glass-ceramic (control) (7) PG (IMAGINE PressX). Specimens of each group were tested immediately after fabrication (n = 15 per material). Seventy-five FDPs per material type were stored in artificial saliva (37°C) and 15 of them were randomly selected after aging (1, 7, 28, 90, and 180 days) for fracture load measurement. The remaining specimens (n = 60 per material) were subjected to chewing simulation (×120.000–1.200.000, 49 N, 5°C/50°C). The data were analyzed using two-way and one-way ANOVA followed by Scheffé test.
Results
The interactions between FDP materials and aging time in both storage media showed a significant impact on the results (p < 0.001). Among saliva storage groups, TC and ZP showed the highest, and PG the lowest fracture load (p < 0.05). AT and CT were not affected from chewing simulation. TC, ZP, and AT presented the highest in ascending order (p < 0.05), PG and CMK showed the lowest fracture load after chewing simulation (p < 0.001).
Conclusions
Aging did not influence the fracture load of FDPs made of CAD/CAM resins. FDPs made of glass–ceramic showed significantly lower fracture load than those of all resin FDPs. Clinical relevance: Considering fracture load measurements, CAD/CAM resins tested could be alternative materials to glass–ceramic for FDP construction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tooth-colored temporary fixed dental prostheses (FDPs) can be constructed and milled from polymeric resin blocks using computer-aided design/computer-aided manufacturing (CAD/CAM) technology [1] either at labside or chairside. Chairside fabricated reconstructions can be cemented at the same session, thus reducing the treatment time, and eliminating the need for making temporary prostheses.
Polymeric blanks for CAD/CAM technology are industrially polymerized under standardized parameters at high temperature and pressure. Hence, microstructure and mechanical properties of the resin blocks exhibit constant quality. This allows for the production of reconstructions with higher flexural strengths compared to conventionally fabricated ones [1, 2]. In general, temporaries are made of chemically cured resins either in powder/liquid (PMMA) or paste form (resin composite). While for direct temporary FDPs, usually, chemically polymerized composites are used; for indirect ones, PMMA-based resins are preferred that are polymerized under pressure in a polymerization device. The polymerization parameters are fundamental for the mechanical properties [3]. However, compared to CAD/CAM milled FDPs, the quality of manually processed ones may be highly affected by the operator.
Glass–ceramic materials for fixed reconstructions require certain thickness to have adequate fracture resistance, whereas resin materials are more fracture-resistant even in thin reconstructions [4, 5]. The wear characteristics of resin-based materials offer some advantages over glass–ceramics as they yield to less wear in the antagonist enamel [6, 7]. Therefore, due to their mechanical properties and brittleness, conventional glass–ceramics are not indicated for multiple unit FDPs, but for single crowns [8]. Therefore, recently introduced polymeric CAD/CAM resins are considered as alternative materials to glass–ceramics. However, limited information is available on their long-term mechanical durability [1, 2].
The aim of this study was to investigate the effect of saliva storage and chewing simulation on the fracture load of conventionally and CAD/CAM fabricated polymeric three-unit FDPs. The first hypothesis tested was whether the CAD/CAM resin FDPs show similar fracture load after aging simulations compared to conventionally fabricated ones. The second hypothesis tested was whether the fracture load of CAD/CAM resin FDPs is higher than glass–ceramic three-unit FDPs.
Materials and methods
This study tested the fracture load of three-unit FDPs fabricated from four different CAD/CAM materials, two manually processed resins and one glass–ceramic (Table 1).
One hundred fifteen identically shaped three-unit FDPs were fabricated from each material. The connectors had a cross-section of 7.36 mm2, an occlusogingival height of 3.2 mm, and a buccolingual width of 2.3 mm [9]. The occlusal surfaces were kept flat. For the production of the specimens, a steel model with two abutments simulating an FDP between a second premolar and a second molar was used. Abutments of this model were cylindrical (diameter, 7 mm premolar; 8 mm molar) with a 1-mm circular shoulder and 6° taper [9]. They were made of steel to minimize their residual deformation during the loading test and are surrounded by a 0.5-mm layer of plastic cover that allowed for simulation of the periodontium [10, 11]. The holder of the test setup was made of an aluminum alloy having cylindrical holes of 7.8 and 8.8 mm diameter and a distance of 16.5 mm between centers of the holes.
The CAD/CAM resins (N = 600, n = 150 per material) and 150 wax blanks (ZENO TEC Wax Disc, Wieland Dental, Pforzheim, Germany) for the press ceramic FDPs were milled using a master STL-file of a three-unit FDP. The Cerec inLab system (Sirona, Bensheim, Germany) was used for AT, TC, and CT, while the ZENO Tec System (ZENO 4030 M1, Wieland Dental) was employed for ZP and the wax templates.
Subsequently, for the glass–ceramic specimens, the wax templates were invested (Wilavest Universal, Wieland Dental) according to the manufacturer’s instructions. After evaporating the wax in a standard oven (EWL Type 5636, KaVo, EWL, Leutkirch, Germany), the PG specimens were pressed in a special oven (EP 600, Ivoclar Vivadent, Schaan, Liechtenstein). The investment material was removed after cooling in an air abrasion unit (CEMAT NT4, Wassermann, Hamburg, Germany) using 50-μm alumina particles (Renfert, Hilzingen, Germany) at 2 bar pressure. Finally, glaze paste was applied on the crowns and fired in a ceramic oven (Astromat D4, DEKEMA, Freilassing, Germany).
For the conventionally fabricated FDPs, one silicone key with a standard shape and size was used. The manually polymerized resins were filled in the silicone key and polymerized according to the respective manufacturer’s instructions (Table 1). The surface of direct temporary FDPs (CMK) was ground with a fine polish brush (Soft PD H DT2, Pluradent, Offenbach, Germany). In order to simulate the clinical environment, the indirect temporary FDPs (IEP) were relined with a PMMA resin (TAB 2000, Lot.No: 61565, Kerr, Bioggio, Switzerland) and polymerized according to the manufacturer’s instruction (Table 1). Thereafter, the final indirect temporary FDPs were finished and polished.
The fabricated FDPs of each material (n = 150) were then randomly divided into three groups; FDPs for direct measurements (n = 15), for saliva storage (n = 75), and for chewing simulation (n = 60).
Saliva storage
The FDPs were stored in artificial saliva (Fusayama/Meyer: KCl 0.4 g/l, NaCl 0.4 g/l, CaCl2, 2H2O 0.906 g/l, NaH2PO4, 2H2O 0.690 g/l, Na2S, 9H2O 0.005 g/l, and urea 1 g/l; pH = 4.7) at 37°C in an incubator (ED 240; Binder; Tuttlingen, Germany). Fifteen specimens were randomly selected after 1, 7, 28, 90, and 180 days for fracture load measurements.
Chewing simulation
Chewing simulation (custom made: University of Zurich) with thermal cycling (5°C/50°C; transfer time, 10 s; dwell time, 120 s) was performed for 120,000, 240,000, 640,000, and 1,200,000 masticatory cycles [12]. The FDPs were loaded under 49 N at a frequency of 1.67 Hz. For simulating a typical clinical situation, mesiobuccal cusp from nearly identical maxillary human molars, fixed in amalgam (Dispersalloy; Dentsply; Konstanz, Germany), acted as antagonists. The tips of the cusps were rounded to a spherical shape. The horizontal distance between FDP and the enamel antagonist was 3 mm. After chewing simulation, the specimens were subjected to fracture load testing.
Fracture load measurement
The fracture load test was performed in a universal testing machine (Zwick/Roell Z010, Zwick, Ulm, Germany). The FDPs were placed on the abutments without using cement and loaded with a flat-ended rod (diameter 5 mm) at the center of the pontic from the occlusal–gingival direction until fracture occurred (crosshead speed 1 mm/min) (Fig. 1). In order to avoid force peaks, a piece of 0.3-mm teflon foil (Angst + Pfister, Zurich, Switzerland) was placed between the pontic and the loading jig.
Statistical analysis
The fracture load data were analyzed using a statistical software program (SPSS version 19, SPSS Inc., Chicago, IL, USA). Initially, the descriptive statistics were computed. Two-way and one-way ANOVA followed by Scheffé post-hoc test were used for the analysis of fracture load data for saliva-stored and chewing-simulated FDPs. The fracture load of specimens that fractured during the chewing simulation before actual testing was considered as 0 N. In all tests, p-values smaller than 5% were considered as statistically significant.
Results
Saliva storage
The two-way interaction (FDP materials versus aging) was significant (p < 0.001). Also, the interactions between FDP materials and aging time showed significant impact on the results (p < 0.001). Therefore, the fixed effects FDP materials and aging cannot be compared directly as the higher order interactions were found to be significant. Consequently, several different analyses were provided and splitted at levels of FDP materials and aging factors depending on the hypothesis of interest (Table 2). The results of the descriptive statistics (mean, SD, 95% CI) with one-way ANOVA results for the fracture load of each tested group are presented in Table 3.
The control group, PG, and three of the CAD/CAM fabricated FDPs—TC, ZP, and CT—were not significantly affected by saliva storage up to 180 days (Fig. 2). The CAD/CAM resin AT presented significantly higher fracture load after 1-day storage compared to 180 days of storage (p < 0.001). In contrast, the indirect temporary FDPs made of IEP (p < 0.001) and direct temporaries made of CMK (p < 0.001) were significantly affected by saliva storage. Fracture load of IEP decreased significantly after 180 days compared to initial values or after 1-day saliva storage. The mean fracture load of CMK increased up to 7 days of storage (p < 0.001), but after this time point, the results decreased. After 7 days, the values were significantly higher compared to 90 days of storage (p < 0.05).
The CAD/CAM resin FDPs AT, TC, and ZP showed the highest fracture load, followed by indirect temporary resin IEC. From the CAD/CAM resin FDPs, CT presented significantly lower values compared to the remaining CAD/CAM resins and conventional resin, IEP (p < 0.05). The lowest values were observed for the control group at all time points. The direct resin, CMK, showed initially similar values to the glass–ceramic tested, but after 1 day up to 180 days of storage, CMK showed higher values than the glass–ceramic.
Chewing simulation
The two-way interaction (FDP materials versus aging) was significant (p < 0.001). Also, the interactions between FDP materials and aging time showed a significant impact on the results (p < 0.001). Therefore, the fixed effects FDP materials and aging cannot be compared directly as the higher order interactions were found to be significant. Consequently, several difference analyses were provided and splitted at levels of FDP materials and aging factors depending on the hypothesis of interest (Table 4). The results of the descriptive statistics (mean, SD, 95% CI) with 1-way ANOVA results for the fracture load of each tested group are presented in Table 5.
Only two FDP materials, namely CAD/CAM resins AT (p = 0.717) and CT (p = 0.255), were not affected from chewing simulation (Fig. 3). Among the CAD/CAM resins a significant decrease was observed after 1,200,000 masticatory cycles for ZP (p < 0.001) (one FDP was fractured) and after 120,000 cycles for TC (p < 0.001).
The conventional resin IEC (p < 0.001) and the control group (p < 0.001) showed decreased fracture load with the increase in the number of masticatory cycles. The fracture load of CMK increased after 120,000 cycles and then decreased with the increase in masticatory cycles, and after 640,000 cycles, all specimens were fractured during the chewing simulation. In the group IEP, 1, 2, 6, and 12 specimens were fractured after 120,000, 240,000, 640,000, 1,200,000 cycles, respectively. In CMK group, 4, 15, and 15 specimens were fractured after 240,000, 640,000, and 1,200,000 cycles, respectively. The control group showed 2 fractured FDPs after 240,000, 8 fractured FDPs after 640,000, and 15 fractured FDPs after 1,200,000 cycles (Table 6).
All tested FDPs fractured typically between the abutment and the pontic at the connector area.
Discussion
In general, the results of this study showed that storage in saliva and chewing simulation did not influence industrially polymerized CAD/CAM resins, except ZP, compared to indirect or direct temporary FDPs tested. Therefore, the first hypothesis of this study is rejected. By industrially polymerizing CAD/CAM resins under optimal conditions, the mechanical strength is increased and the risk for porosities within the restorations is reduced [13]. In contrast, the mechanical properties of conventionally fabricated resin FDPs are dependent on the operator, mixing proportions of the resin components, polymerization device, and duration of the polymerization, among others.
In this study, glass–ceramic was used as control group. Glass–ceramic is the most commonly used material for CAD/CAM single crowns and inlays or onlays. The glass–ceramic FDPs presented the lowest values compared to all tested CAD/CAM resins. Consequently, the second hypothesis is accepted.
After 1-day saliva storage at 37°C, the direct temporary resin tested in this study (CMK) showed an increase in fracture load values, probably due to post-polymerization of the monomer. In another study, similar results were obtained initially and 1 day after storage [14]. In this study, after 1-day storage in saliva and chewing simulator, the fracture load increased for CMK. Burtscher [15] reported that radicals may be active over a period of 7 days, leading to a significant post-polymerization. The results of this study with CMK support this statement when the results up to 7 days are considered. This can, however, be stated only for saliva storage. With CMK in the chewing simulator, the results showed some post-polymerization possibility between initial and 1 day.
The specimens were subjected to chewing simulation, where the stress for all specimens was standardized and reproducible. The use of a loading machine with additional artificial aging by thermocycling is a well-proven and established method to simulate the clinical situation [16, 17]. It is claimed that the chewing simulation of 1,200,000 cycles corresponds to 5 years in vivo [18]. However, this assumption has not yet been systematically verified with different materials and is only based on the extrapolation of 4-year clinical wear data on amalgam fillings and 6-month data of composite inlays [18]. Thus, the correlation was only used for the measurements of abrasion stability. In summary, more longitudinal clinical aging data are still needed. At the time, only trends and indications as to the true extent of aging can be obtained.
The setup with the steel model used could have a negative impact on the fracture load results. It has been previously reported, that the mean fracture loads of FDPs decrease on rigidly mounted abutments compared to non-rigidly mounted ones [19, 20]. The authors reported that the elastic modulus of the abutment had an influence on the fracture load of FDPs [19, 20]. Another study showed that increasing the elastic modulus of the abutments results in increased fracture load [21]. Non-rigidly mounted abutments with an elastic modulus similar to that of natural teeth behave similarly to the clinical situation [2, 22]. In addition, in this study, the FDPs were not cemented on the abutment. Possible effect of cement use should be further investigated since lack of cement might have created inferior bending forces and less damping effect.
The FDP design had flat occlusal surfaces, not representing the real clinical situation. The lack of veneering materials and occlusal morphology are limitations of this study. Therefore, this study serves for only ranking the materials. Further studies should test these aspects as well. In the present study, the connector area of the FDPs was 7.36 mm2. The manufacturer of artBlock Temp recommends 9 mm2 and of CAD-Temp 12 mm2; those are higher section area than employed here. Clinically, such a large surface area may jeopardize the periodontal tissues. Therefore, in this study, FDPs had a smaller connector surface area. An increased connector surface area may surely increase the results [23].
Constant clinical occlusal forces of 12 to 90 N and occasional maximum forces up to 909 N in posterior areas can be assumed depending on the type of measurement, gender, restoration type, diet, and other parameters [24]. Therefore, failures of the tested FDPs were observed below 500 N. Thus, the fracture load tested in this study may not withstand the clinical applications without restrictions.
Fasbinder et al. [25] studied the clinical performance of CAD/CAM fabricated composite inlays and observed that the resin-based composite inlays had a significantly better color match at 3 years than did the glass–ceramic inlays. Resin-based composite CAD/CAM inlays performed as good as glass–ceramic CAD/CAM inlays after 3 years of clinical service. Lehmann et al. [26] observed clinical failures and complications such as wear facet, plaque accumulation in single resin composite crowns after 5 years. They concluded that composite crowns might be recommended for long-term temporary use. However, the complication rate and the increased plaque accumulation may restrict the indication for permanent restorations. Vanoorbeek et al. [27] in a clinical study up to 3 years of function observed that resin composite single-tooth restorations had inferior success rates compared to all-ceramic ones. Due to the inferior esthetics and wear resistance of resin composite crowns, all-ceramic crowns remain the preferred treatment material for CAD/CAM-generated metal-free single restorations. Future developments with PMMA- or composite-based FDPs should concentrate on improvement of wear stability of such materials that could still be considered inferior to glass–ceramics.
Based on the findings after chewing simulation, CAD/CAM resins have obvious advantages over conventionally fabricated ones. However, clinical studies are needed to support the use of CAD/CAM resins in long-term restorations.
Conclusions
Within the limitations of this study, the following conclusions can be drawn:
-
1.
The tested CAD/CAM resin FDPs, with the exception of ZP, were not influenced by storage in saliva and chewing simulation compared to conventionally fabricated ones.
-
2.
CAD/CAM resins—AT, TC, and ZP—presented higher fracture load compared to CAD/CAM resin CT.
-
3.
Glass–ceramic three-unit FDPs showed lower mean fracture load compared to the tested manually and CAD/CAM fabricated resin FDPs.
References
Alt V, Hannig M, Wostmann B, Balkenhol M (2011) Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater 27:339–347
Goncu Basaran E, Ayna E, Vallittu PK, Lassila LV (2011) Load-bearing capacity of handmade and computer-aided design–computer-aided manufacturing-fabricated three-unit fixed dental prostheses of particulate filler composite. Acta Odontol Scand 69:144–150
Banerjee R, Banerjee S, Prabhudesai PS, Bhide SV (2010) Influence of the processing technique on the flexural fatigue strength of denture base resins: an in vitro investigation. Indian J Dent Res 21:391–395
Rocca GT, Bonnafous F, Rizcalla N, Krejci I (2010) A technique to improve the esthetic aspects of CAD/CAM composite resin restorations. J Prosthet Dent 104:273–275
Lin CL, Chang YH, Liu PR (2008) Multi-factorial analysis of a cusp-replacing adhesive premolar restoration: a finite element study. J Dent 36:194–203
Krämer N, Kunzelmann KH, Taschner M, Mehl A, Garcia-Godoy F, Frankenberger R (2006) Antagonist enamel wears more than ceramic inlays. J Dent Res 85:1097–1100
Giordano R (2006) Materials for chairside CAD/CAM-prodeced restorations. J Am Dent Assoc 137:14S–21S
Chaysuwan D, Sirinukunwattana K, Kanchanatawewat K, Heness G, Yamashita K (2011) Machinable glass-ceramics forming as a restorative dental material. Dent Mater J 30:358–367
Luthy H, Filser F, Loeffel O, Schumacher M, Gauckler LJ, Hammerle CH (2005) Strength and reliability of four-unit all-ceramic posterior bridges. Dent Mater 21:930–937
Rosentritt M, Behr M, Scharnagl P, Handel G, Kolbeck C (2011) Influence of resilient support of abutment teeth on fracture resistance of all-ceramic fixed partial dentures: an in vitro study. Int J Prosthodont 24:465–468
Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, Naumann M (2011) In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand 69:316–318
Rechenberg DK, Göhring TN, Attin T (2010) Influence of different curing approaches on marginal adaptation of ceramic inlays. J Adhes Dent 12:189–196
Poticny DJ, Klim J (2010) CAD/CAM in-office technology: innovations after 25 years for predictable, esthetic outcomes. J Am Dent Assoc 141:5S–9S
Balkenhol M, Kohler H, Orbach K, Wostmann B (2009) Fracture toughness of cross-linked and non-cross-linked temporary crown and fixed partial denture materials. Dent Mater 25:917–928
Burtscher P (1993) Stability of radicals in cured composite materials. Dent Mater 9:218–221
Manhart J, Schmidt M, Chen HY, Kunzelmann KH, Hickel R (2001) Marginal quality of tooth-colored restorations in class II cavities after artificial aging. Oper Dent 26:357–366
Rosentritt M, Siavikis G, Behr M, Kolbeck C, Handel G (2008) Approach for valuating the significance of laboratory simulation. J Dent 36:1048–1053
Rosentritt M, Behr M, van der Zel J, Feilzer AJ (2009) Approach for valuating the influence of laboratory simulation. Dent Mater 25:348–352
Fischer H, Weber M, Eck M, Erdrich A, Marx R (2004) Finite element and experimental analyses of polymer-based dental bridges reinforced by ceramic bars. J Biomech 37:289–294
Mahmood DJ, Linderoth EH, Vult von Steyern P (2011) The influence of support properties and complexity on fracture strength and fracture mode of all-ceramic fixed dental protheses. Acta Odontol Scand 69:229–237
Scherrer SS, de Rijk WG (1993) The fracture resistance of all-ceramic crowns on supporting structures with different elastic moduli. Int J Prosthodont 6:462–467
Keulemans F, Lassila LV, Garoushi S, Vallittu PK, Kleverlaan CJ, Feilzer AJ (2009) The influence of framework design on the load-bearing capacity of laboratory-made inlay-retained fibre-reinforced composite fixed dental prostheses. J Biomech 42:844–849
Pfeiffer P, Grube L (2006) Effect of pontic height on the fracture strength of reinforced interim fixed partial dentures. Dent Mater 22:1093–1097
Waltimo A, Kononen M (1995) Maximal force and its association with signs and symptoms of craniomandibular disorders in young Finnish non-patients. Acta Ordontol Scand 53:254–258
Fasbinder DJ, Dennison JB, Heys DR, Lampe K (2005) The clinical performance of CAD/CAM-generated composite inlays. J Am Dent Assoc 136:1714–1723
Lehmann F, Spiegl K, Eickemeyer G, Rammelsberg P (2009) Adhesively luted, metal-free composite crowns after five years. J Adhes Dent 11:493–498
Vanoorbeek S, Vandamme K, Lijnen I, Naert I (2010) Computer-aided designed/computer-assisted manufactured composite resin versus ceramic single-tooth restorations: a 3-year clinical study. Int J Prosthodont 23:223–230
Acknowledgments
We are grateful to Merz Dental, Vita Zahnfabrik, Ivoclar Vivadent, and Wieland Dental for the financial and material support.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stawarczyk, B., Ender, A., Trottmann, A. et al. Load-bearing capacity of CAD/CAM milled polymeric three-unit fixed dental prostheses: Effect of aging regimens. Clin Oral Invest 16, 1669–1677 (2012). https://doi.org/10.1007/s00784-011-0670-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0670-4