Abstract
In the present study, two different fibre-reinforced composites (FRCs) (glass and polyethylene FRC), dental ceramic and restorative composite were compared with respect to early plaque formation in vivo. Disc-shaped specimens were randomly distributed among the upper first and second molars of 14 healthy adult volunteers. Plaque samples were collected 24 h after the attachment of the specimens. Mutans streptococci (MS), non-mutans streptococci and total facultative bacteria were cultured. The plaque recovered from polyethylene FRC harboured significantly more MS than the plaque of ceramic, restorative composite and glass FRC. For the counts of non-mutans streptococci and total facultative bacteria, polyethylene FRC showed the highest counts, and ceramic showed a trend towards lower counts. The amount of plaque accumulation showed an association to the earlier reported surface roughness values of the studied materials. It was concluded that in the oral environment, polyethylene FRC promotes plaque accumulation and adhesion of MS more than glass FRC, restorative composite and dental ceramic. Glass FRC resembles restorative composite with respect to plaque accumulation and the adherence of MS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fibre-reinforced composites (FRCs) are materials with good cosmetic and mechanical properties. As dental materials, they are currently used in fixed partial dentures, periodontal splints and as reinforcements of removable dentures. The most commonly used fibre types in clinical dentistry are glass and ultra high molecular weight (UHMW) polyethylene fibres. Fibres differ among other things with respect to their surface properties. Polyethylene has low surface-free energy, whereas glass is a high surface energy material. The fibres of an FRC are preferably covered with the matrix polymer or with restorative or veneering particulate filler composite. However, in marginal areas of crowns and removable dentures or during polishing, the fibres may be exposed to the oral cavity and come into contact with oral microbes.
The formation of dental plaque is the primary step in the development of caries and periodontal disease. All non-shedding surfaces in the oral cavity, biological or artificial, are available as substrates for the development and growth of dental plaque. Subsequent to the formation of an acquired salivary pellicle, the first colonisers of these surfaces are streptococci, commonly Streptococcus sanguinis [15]. After 24 h the plaque constitutes mainly of streptococci and gram-positive rods, like actinomyces [15, 16, 21]. The predominant streptococcal species in a 1-day-old dental plaque are S. sanguinis, Streptococcus mitis and Streptococcus oralis, sometimes also referred to as members of the group non-mutans streptococci. The caries-associated mutans streptococci (MS) can also be found in the early plaque. Their proportion of the total streptococci is, however, low, 2% at most [16]. MS are a virulent group of bacteria, including the following species: Streptococcus mutans, Streptococcus sobrinus, Streptococcus rattus, Streptococcus cricetus, Streptococcus macacae and Streptococcus downei [23]. MS adhere to components of the salivary pellicle via adhesins and produce extracellular polysaccharides in the presence of sucrose [1]. Their predominant receptor proteins in the pellicle are the high molecular weight glycoproteins, agglutinins [5, 10]. Parotid saliva, the main source of agglutinins in the oral cavity, is found to promote the adherence of S. mutans more than whole or submaxillary saliva [6].
In our previous studies concerning bacterial adhesion to FRCs, we found differences in the in vitro binding of S. mutans to different FRCs and were able to correlate it to the surface roughness of these materials [20]. Polyethylene FRC was found to have a rougher surface and binds more S. mutans than other studied FRCs, namely, glass, aramid and carbon/graphite FRCs. We also found that a parotid saliva pellicle promoted S. mutans adhesion in vitro to dental ceramic and glass fibres [20]. The pellicles formed on these materials were found to contain high amounts of high molecular weight (HMW) agglutinins. Based on these findings, it is interesting to speculate whether individuals with a parotid saliva that promotes the adherence of S. mutans in vitro would harbour more MS in the plaque of these materials also in vivo.
In the oral environment, adhesion and colonisation take place under competition of several microbial species, and the composition of the acquired pellicle differs from experimental pellicles.
The aim of this study was thus to compare early plaque formation in vivo on two different FRC materials and conventional restorative materials.
Materials and methods
Materials
The materials used in this study are listed in Table 1. Two different FRCs, a restorative particulate filler composite (Z250; 3M Dental Products, St. Paul, MN, USA) and a high-leucite ceramic material used for ceramic fillings and crowns (Finesse All-Ceramic; Dentsply, York, PA, USA), were studied. Disc-shaped test specimens with a diameter of 4 mm and a height of 1.5 mm were fabricated out of each material. Fabrication of test specimens has been described earlier [20]. The top surface of the specimens was wet-ground and polished using a silicon carbide paper (grit 2400). Scanning electron micrographs of the surface of the FRC specimens were taken to ensure the proper wetting and homogenous distribution of reinforcing fibres (JEOL, JSM 5500, UK) (Fig. 1).
Scanning electron micrographs of glass (a) and polyethylene (b). FRC specimen surfaces showing the perpendicular orientation of fibres to the surface. Reinforcing fibres are evenly distributed in the composite and well wetted by the matrix polymer. No voids between fibres and matrix polymer are present. Original magnification ×500
The average surface roughness (Ra) of the studied materials was measured in the previous study [20]. The average roughness values (μm) of the polished test specimens were: ceramic 0.05, restorative composite 0.05, glass FRC 0.07 and polyethylene FRC 0.51. The surface of polyethylene FRC was found to be significantly rougher than the other studied materials.
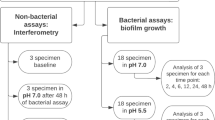
Plaque formation and collection
Plaque formation in vivo on four different materials was studied in 14 healthy adult volunteers (3 males, 11 females, mean age 31.7 years, range 21–52 years). The test specimens were attached to the buccal surfaces of the upper molars of the subjects (Fig. 2). Materials were randomly distributed among the upper first and second molars, and the subjects were unaware of the distribution. The subjects were advised not to brush their upper teeth and not to use xylitol-containing products or anti-microbial mouth rinses during the plaque accumulation period. Detergent-free toothpaste was used during the plaque accumulation period. None of the participants used anti-microbial drugs during the study.
The upper molars and premolars were professionally cleaned with pumice to remove plaque and pellicle. An area of the size of the specimen was etched with 37% orthophosphoric acid for 30 s, rinsed and dried thoroughly. Adhesive resin was applied and light-cured for 10 s. A small amount of flowable composite was applied, specimen was placed on top of the composite, and composite was cured with light for 20 s. Sharp edges were rounded using rotating polishing instruments and water cooling. After the test specimens were attached, subjects chewed sucrose-containing chewing gum for 1 min to promote the adhesion of MS. A sample of stimulated saliva was collected for the assessment of salivary counts of MS. One hundred microlitres of the saliva was inoculated into 900 μl of tryptic soy broth (TSB) and stored as frozen.
Plaque samples were collected 24 h after the attachment of the test specimens. The surface of the test specimens was gently rinsed with saline, and plaque was collected by rubbing the surface of each specimen with three applicator sticks (Quick-Stick, Dentonova AB, Huddinge, Sweden) containing approximately 4 μl of NaCl solution. Care was taken not to touch the outer unpolished surfaces of the specimens with the sticks. The tips of the sticks were cut off and collected into a tube containing 900 μl of TSB. A plaque sample from the buccal enamel surface of the upper second premolar was collected similarly. This sample, collected from roughly the same surface area as were the specimens, represented the enamel plaque. Due to possible differences in the plaque collection area, no quantitative comparisons were made between enamel plaque and plaque formed on test specimens. The samples were stored in −70°C before cultivation. After plaque collection the specimens were removed, and the excess composite was finished off using hand instruments and rotating polishing instruments. Finally, fluoride varnish was applied on the polished enamel surfaces. The same person (J.T.) performed all plaque collections.
Microbiological analyses
A laboratory assistant and an experienced microbiologist performed the microbiological analyses. Both were blinded as to the sample coding. The transport tubes of the plaque samples and saliva samples were thawed and vortexed thoroughly. To detach the micro-organisms from the collection tips, the samples were ultrasonically treated for 10 s. Ten-microlitre aliquots of serial tenfold dilutions of the plaque samples were plated on agar plates. MS were cultured on Mitis salivarius agar containing bacitracin (MSB) [12]. The plates were incubated for 2 days in 7% CO2 atmosphere at 37°C. MS were identified on the basis of colony morphology and counted using a stereomicroscope. The identification of S. mutans and S. sobrinus was performed as described earlier [8, 19]. Non-mutans streptococci were cultured for 2 days in air on Mitis salivarius agar at 37°C. All streptococcal-like colonies were counted as non-mutans streptococci. Total facultatives were cultured for 3 days anaerobically on blood agar at 37°C. All colonies were counted.
Statistical analyses
Statistical analyses to compare the materials were performed with non-parametric tests due to the small sample size. At first stage the data were subjected to a Friedman test. When statistical differences among materials were detected, subsequent comparisons were done using Wilcoxon signed-rank test. With this test all studied materials were compared to restorative composite, and the studied FRCs were compared with each other. Statistical analyses were performed with SPSS for Windows (Rel. 10.0.5, 1999; SPSS Inc., Chicago, IL, USA).
Results
Mutans streptococci were detected in the saliva samples of all subjects. Five subjects showed low salivary MS counts (<104 colony-forming units (CFU)/ml), six showed moderate (104–105 CFU/ml) and three showed high counts (>105 CFU/ml), respectively. Two of the subjects with low salivary MS counts showed no adherence of MS to the studied materials. All subjects with MS adherence to the studied materials had MS adherence on the enamel plaque as well. S. sobrinus was detected from the samples of only one subject. The counts were combined with S. mutans counts. The mean logarithmic CFU count (±SD) was 1.0±1.34 for ceramic, 1.4±1.28 for restorative composite, 1.7±1.25 for glass FRC and 2.4±1.19 for polyethylene FRC. The distribution of subjects according to MS counts on the studied materials is illustrated in Fig. 3. Ceramic samples showed most often no growth of MS, whereas MS were found from all polyethylene samples, and half of the samples revealed more than 10 CFUs after cultivation (Fig. 3). For the counts of MS, the Friedman test revealed a statistically significant difference between the materials (p=0.010). The plaque samples of polyethylene FRC showed significantly more MS than the samples of restorative composite (p=0.006) and glass FRC (p=0.050). Restorative composite, ceramic and glass FRC did not differ with respect to MS counts.
The results of the microbiological examinations of non-mutans streptococci and total facultative bacteria found from the samples of the studied materials are shown in Figs. 4 and 5. For the counts of non-mutans streptococci, significant differences were found between the materials (p=0.002). Polyethylene FRC showed the highest counts, and ceramic showed the lowest. In the pairwise comparisons, polyethylene FRC differed significantly from restorative composite (p=0.006) and glass FRC (p=0.007). Examinations of the counts of total facultative bacteria also revealed differences between the materials (p=0.012). Polyethylene again showed the highest counts and differed significantly from glass FRC (p=0.008). Glass FRC, ceramic and restorative composite showed similar adhesion of both non-mutans streptococci and facultative bacteria, and no statistically significant differences between these materials could be found.
Discussion
In the present study, four dental materials were compared with respect to plaque formation in vivo. Significant differences were found between the materials in all the microbiological examinations performed.
Buccal surfaces of upper molars were selected for the attachment site of the specimens, as the caries-associated MS are known to colonise preferentially the buccal posterior parts of the dentition. Due to occlusal conditions, the specimens are better protected from detaching forces in the upper jaw. The influence of parotid saliva on the pellicle composition is also strongest in the upper posterior region [2]. Several methods to study in vivo plaque formation have been reported [13, 14, 18]. Recently, Wood et al. used an in situ plaque-generating device to study plaque architecture by means of confocal scanning laser microscopy [24]. The present study, however, focused on the plaque microbial composition and adhesion of MS, and the plaque formation and collection method used provides adequate information for these investigations. Our main interest was to compare plaque formation on different restorative materials. Thus, the plaque that formed on the natural enamel surfaces of premolars was used as a qualitative control.
The number of subjects (14) in the present study is relatively low. On the other hand, all subjects carried all four materials simultaneously on their teeth, and the surface area of the specimens was carefully adjusted to be equal in all materials. Blinding was used in the microbiological examinations but not in the attachment of the specimens and the collection of plaque samples. The same experienced dental professional performed all plaque samplings. The studied materials differ in their colour and surface appearance, and blinding as to the material was thus not possible during plaque sampling. However, the relatively small intra-individual differences, as indicated by the standard deviations, support the reliability of the results despite the lack of blinding.
The counts of non-mutans streptococci and total facultative bacteria resembled each other for all studied materials, with facultatives showing a trend of slightly higher counts. In the 24-h plaque samples, the number of facultatives most likely reflects the number of streptococci. Nyvad and Kilian found that a 1-day-old early plaque on enamel and root surfaces was composed mainly of streptococci (77%), with S. mitis and S. sanguinis as the predominant species [15]. Gram-positive rods, commonly Actinomyces, were found to be the second most common species, constituting approximately 10% of the plaque bacteria. Streptococci have previously been found as the predominant species in a 24-h plaque on restorative materials as well [18]. Similarly, in the present study, all materials seem to harbour an early plaque that consists mainly of streptococci.
The amount of plaque accumulation based on the counts of non-mutans streptococci and total facultative bacteria showed an association to the earlier reported surface roughness values of the studied materials [20]. Polyethylene FRC, as the roughest material, promoted plaque accumulation significantly more than the other smoother materials. Ceramic, having the smoothest surface, showed a trend towards less plaque accumulation, although the difference was significant only in comparison with polyethylene FRC. Glass FRC and restorative composite showed very similar plaque accumulation properties. These materials resemble each other also in their surface physico-chemical properties. They are both composite materials composed of inorganic filler particles in an organic polymer matrix. In the case of glass FRC, glass fibres are the inorganic fillers. Polymer matrices of both composites are commonly based on dimethacrylate monomer systems. Their surface roughness values after polishing are also very similar and significantly lower than the roughness of polyethylene FRC [20]. These findings are supported by several authors stating that rough surfaces promote bacterial adhesion [4, 17, 18].
The physico-chemical characteristics of a surface, such as material surface-free energy, have been shown to affect bacterial adhesion in vitro [4] and in vivo [22]. High-energy surfaces have been shown to attract more micro-organisms than low surface-free energy materials. In the present study, polyethylene, the lower surface-energy material, was found to harbour more micro-organisms than the higher energy materials. This was accounted for the higher surface roughness of polyethylene FRC. Our results seem to be in line with Quirynen and Bollen [17] stating that in the oral environment, surface roughness seems to be a governing factor over the influence of surface-free energy determining the amount of plaque accumulation on dental materials. Moreover, the materials studied, despite the ceramic, appeared as composites in the present study.
The surface of polyethylene FRC also harboured more MS than other materials studied. Glass FRC and restorative composite resembled each other in the colonisation of MS as well. The least growth of MS was observed in the plaque recovered from the ceramic samples. Seven of the 12 subjects with MS in their plaque had no growth of MS on the ceramic samples, whereas all 12 subjects showed colonisation of MS on polyethylene (Fig. 3). These in vivo findings are in accordance with our earlier in vitro results of S. mutans adherence. Polyethylene FRC was found to promote the initial adherence of S. mutans ATCC 25175. In addition to the higher surface roughness, we found its pellicle protein composition favourable to S. mutans adhesion [20].
In the previous study, we also found that the pellicles recovered from ceramic and E-glass, which contained high amounts of agglutinin, promoted the adhesion of S. mutans [20]. Our present in vivo findings are not, however, consistent with these in vitro observations. Carlen et al. demonstrated a correlation between individual in vitro saliva-mediated binding and the in vivo prevalence of S. mutans [7]. They, however, investigated an older plaque (4d). Multiplication of initially attached species will most likely lead to higher counts of MS during plaque growth, and correlations are thus more easily revealed. The high proportion of samples with no growth of MS in the present study also makes analyses difficult. Furthermore, the strain used by Carlen et al. in the in vitro adherence experiments (S. mutans Ingbritt) binds preferentially to HMW agglutinins [3], whereas the adhesion of S. mutans ATCC 25175 is mediated by other salivary proteins as well [20]. Other components of saliva may also compete with agglutinin for binding sites and influence the incorporation of agglutinin into the pellicle in vivo [9, 11]. Along with the influence of the secretions of other salivary glands, the competition between different microbial species is a factor missing from the in vitro conditions of earlier studies.
Nyvad and Kilian have shown that the numbers of MS in the early plaque are associated with individual caries activity [16]. The significantly greater number of MS in the early plaque on polyethylene FRC may result in the development of a more cariogenic plaque as the microbial mass increases through cell division during the first days.
To conclude, the present study showed that in the oral environment, polyethylene FRC promotes plaque accumulation and the adhesion of MS more than glass FRC, restorative composite and dental ceramic do. Glass FRC resembles restorative composite with respect to plaque accumulation and the adherence of MS.
References
Banas J, Russell R, Ferretti J (1990) Sequence analysis of the gene for the glucan-binding protein Streptococcus mutans Ingbritt. Infect Immun 58:667–673
Carlén A, Borjesson A, Nikdel K, Olsson J (1998) Composition of pellicles formed in vivo on tooth surfaces in different parts of the dentition, and in vitro on hydroxyapatite. Caries Res 36:447–455
Carlén A, Bratt P, Stenudd C, Olsson J, Strömberg N (1998) Agglutinin and acidic proline-rich protein receptor patterns may modulate bacterial adherence and colonization on tooth surfaces. J Dent Res 77:81–90
Carlén A, Nikdel K, Wennerberg A, Holmberg K, Olsson J (2001) Surface characteristics and in vitro biofilm formation on glass ionomer and composite resin. Biomaterials 22:481–487
Carlén A, Olsson J (1995) Monoclonal antibodies against a high-molecular-weight agglutinin block adherence to experimental pellicles on hydroxyapatite and aggregation of Streptococcus mutans. J Dent Res 74:1040–1047
Carlen A, Olsson J, Borjesson AC (1996) Saliva-mediated binding in vitro and prevalence in vivo of Streptococcus mutans. Arch Oral Biol 41:35–39
Carlén A, Olsson J, Ramberg P (1996) Saliva mediated adherence, aggregation and prevalence in dental plaque of Stretococcus mutans, Streptococcus sanguis and Actinomyces spp, in young and elderly humans. Arch Oral Biol 41:1133–1140
Fujiwara T, Sasada E, Mima N, Ooshima T (1991) Caries prevalence and salivary mutans streptococci in 0–2-year old children in Japan. Community Dent Oral Epidemiol 19:151–154
Gahnberg L, Olsson J, Krasse B, Carlén A (1982) Interference of salivary immunoglobulin A antibodies and other salivary fractions with adherence of Streptococcus mutans to hydroxyapatite. Infect Immun 37:401–406
Gibbons R, Hay D (1988) Human salivary acidic proline-rich proteins and statherin promote the attachment of Actinomyces viscosus LY7 to apatitic surfaces. Infect Immun 56:439–445
Gibbons R, Hay D (1989) Adsorbed salivary acidic proline-rich proteins contribute to the adhesion of Streptococcus mutans JBP to apatitic surfaces. J Dent Res 68:1303–1307
Gold O, Jordan H, van Houte J (1973) A selective medium for Streptococcus mutans. Arch Oral Biol 18:1357–1364
Leonhardt A, Olsson J, Dahlen G (1995) Bacterial colonization on titanium, hydroxyapatite, and amalgam surfaces in vivo. J Dent Res 74:1607–1612
Nyvad B, Fejerskov O (1987) Transmission electron microscopy of early microbial colonization of human enamel and root surfaces in vivo. Scand J Dent Res 95:297–307
Nyvad B, Kilian M (1987) Microbiology of the early colonization of human enamel and root surfaces in vivo. Scand J Dent Res 95:369–380
Nyvad B, Kilian M (1990) Comparison of the initial streptococcal microflora on dental enamel in caries-active and in caries-inactive individuals. Caries Res 24:267–272
Quirynen M, Bollen CML (1995) The influence of surface roughness and surface-free energy on supra- and subgingival plaque formation in man. A review of the literature. J Clin Periodontol 22:1–14
Siegrist BE, Brecx MC, Gusberti FA, Joss A, Lang NP (1991) In vivo early human dental plaque formation on different supporting substances. A scanning electron microscopic and bacteriological study. Clin Oral Implants Res 2:38–46
Söderling E, Isokangas P, Pienihäkkinen K, Tenovuo J (2000) Influence of maternal xylitol consumption on acquisition of mutans streptococci by infants. J Dent Res 79:882–887
Tanner J, Carlén A, Söderling E, Vallittu P (2003) Adsorption of parotid saliva proteins and adhesion of Streptococcus mutans ATCC 25175 to dental fiber-reinforced composites. J Biomed Mater Res 66B:391–398
Theilade E, Theilade J, Mikkelsen L (1982) Microbiological studies on early dento-gingival plaque on teeth and Mylar strips in humans. J Periodontal Res 17:12–25
Weerkamp A, Quirynen M, Marechal M, Van der Mei H, van Steenberghe D, Busscher H (1989) The role of surface free energy in the early in vivo formation of dental plaque on human enamel and polymeric substrata. Microb Ecol Health Dis 2:11–18
Whiley RA, Beighton D (1998) Current classification of the oral streptococci. Oral Microbiol Immunol 13:195–216
Wood SR, Kirkham J, Marsh PD, Shore RC, Nattress B, Robinson C (2000) Architecture of intact natural human plaque biofilms studied by confocal laser scanning microscopy. J Dent Res 79:21–27
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanner, J., Robinson, C., Söderling, E. et al. Early plaque formation on fibre-reinforced composites in vivo. Clin Oral Invest 9, 154–160 (2005). https://doi.org/10.1007/s00784-005-0317-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-005-0317-4