Abstract
Many diagnoses may also have an associated form of the occult spinal dysraphisms. Many of these are uncommonly related, but some (e.g., anorectal atresia) are frequently seen in conjunction with an underlying spinal malformation. Each of these diagnoses should be investigated fully in order to minimize long-term consequences of an untreated or unrecognized tethered spinal cord.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Occult spinal dysraphism (OSD) denotes a group of anomalies resulting from errors during embryogenesis with midline mesenchymal, neural, and ectodermal elements failing to form properly. OSD was initially classified by von Recklinghausen when he studied spina bifida caused by improper fusion of embryonic tissues. Over the last century, its definition has widened to encompass split cord malformation (SCM), meningocele manqué, neurenteric cysts, dermal sinus tract (DST), lipomyelomeningocele (LMMC), fatty filum terminale, and tethered cord syndrome (TCS). Most of these disorders share their symptomology and clinical features. Most cause progressive neurological deficits, impairment, urological abnormalities, and orthopedic degradation to some degree, while some have no clinical symptoms [1].
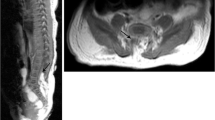
The exact incidence of OSD is unknown, but with the dawn of technologically advanced imagining techniques such as computed tomography (CT) and magnetic resonance imaging (MRI), OSD lesions are becoming more and more readily identifiable and recognized incidentally.
Tethered Cord Syndrome
Tethered cord syndrome (TCS), filum terminale syndrome, or cord-traction syndrome denotes a gamut of congenital anomalies resulting in an uncharacteristically low-lying position of the conus medullaris [2]. The resultant sequelae are neurological sensory and motor deficiencies. TCS was first described by Fuchs in 1910 [3]. He described urinary incontinence in patients with myelomeningocele when they flexed the spine and hypothesized that the incontinence was a result of abnormal spinal cord tension. Lichtenstein [1] added to Fuchs’s hypothesis by describing patients with incomplete fusion and malformations, such as congenital abnormalities of the spinal cord and vertebral column, and linked spinal cord dysfunction and tethering lesions [1]. In 1953, Garceau invented the term “filum terminale syndrome.” He observed three patients with progressive spinal deformity and neurological symptoms and deduced that this was due to a thickened filum terminale [4]. Not until 1976 was the term “tethered spinal cord” used by Dr. Hoffman and his colleagues. They described 31 patients who had elongated spinal cords with symptoms that improved after sectioning of the filum terminale [5].
Knowledge of the relevant anatomy and embryology is necessary to understand TCS fully. As described in a recent review by Lew and Kothbauer [6], the neural tube forms during neurulation at days 18–28 of gestation. The ectoderm that will eventually form the neural tube begins to close around days 22–23 and extends cephalad and caudad with the posterior neuropore closing by day 25–27. After neurulation is complete, the distal neural tube undergoes canalization and then neuralization. Undifferentiated cells from the primitive streak lead to formation of the caudal cell mass. This mass leads to the formation of vacuoles that fuse and develop into the distal neural tube. The caudal cell mass will in turn become the conus medullaris, filum terminale, and the cauda equina. By days 43–48, the ventriculus terminalis forms at the end of the neural tube near the coccyx, leading to the future location of the conus medullaris.
TCS has been studied extensively over the last decade, mostly in animal models. In a study of felines, Yamada et al. demonstrated that by adding weights to the filum terminale , simulating a tethered cord, they could identify the neurological effects of TCS. With tethering being greatest on the more caudal end of the spinal cord and the rostral end being more robust owing to the buffering ability of the dentate ligaments, blood flow and oxidative metabolism were significantly impaired. Using this model, the reversibility and the degree of injury were based on the duration and magnitude of the tethering. It was demonstrated that prolonged immobility of the spinal cord and nerve roots causes longitudinal stretching of the spinal cord, leading to blood supply compromise [7]. Koçak et al. conducted a study involving guinea pigs, using cyanoacrylate to fix the filum terminale [8]. They found that a simulated tethered cord caused ischemic injury and decreased conduction in motor and sensory nerve fibers. In previous studies, it was thought that the abnormal and inelastic filum can interfere with the embryological ascent of the conus medullaris relative to the vertebrae. This leads to a low-lying conus medullaris (below L1/L2), the characteristic trait of TCS. More recent studies have shown that over a 12-year period of tracking of 73 patients, 13 patients whose cord ended at or above the L1-L2 space still displayed symptoms of TCS [9].
In one case series by Khoshhal et al., 35 patients over 7 years were reviewed. The dysraphisms most frequently associated with TCS were lipomeningomyelocele (LMMC) , found in 12 of the 35 patients (34.3%), myelomeningocele in 8 (22.8%), dermal sinus tract in 5 (14.3%), split cord malformation in 4 (11.4%), meningocele in 3 (8.6%), and a thick filum terminale in 3 (8.6%) [10].
OSD with isolated imperforate anus can be as high as 15% in TCS and patients with associated VACTERL as high as 60% [11]. Two of the primary and most prevalent associations with TCS are caudal agenesis and anorectal atresia syndromes. These include the OEIS cluster, imperforate anus, cloacal exstrophy, omphalocele, and spinal anomalies; VACTERL (vertebral anomalies, anal atresia, cardiac anomalies, tracheoesophageal fistula, renal and limb anomalies); and the triad of Currarino, anorectal malformation or congenital anorectal stenosis, sacrococcygeal osseous defect, and presacral mass. VACTERL is commonly associated with TCS and has been found in up to 78% of patients with a tethered cord [12]. TCS was associated with Currarino syndrome in up to 26.7% of patients [13, 14]. In another case report, ultrasonography revealed a sacrococcygeal teratoma associated with a tethered spinal cord during the 23rd week of pregnancy [15].
Miller-Dieker syndrome has been associated with TCS. TCS was secondary to a thickened filum terminale and/or a dermal sinus tract in two case studies [16, 17]. There has also been an association between Chiari type I malformations and TCS, one study showing that TCS was present with Chiari type I malformations in 14% of the patient population studied and 63% with low-lying cerebellar tonsils [18]. In another study of 170 patients with TCS, 10 (6%) had a Chiari type I malformation [19].
Fatty Filum Terminale
Fatty filum terminale is also known as lipoma of the filum terminale, thick filum terminale, or filar lipoma. The filum terminale is a fibrous band comprising two portions: the filum terminale internum, which connects the conus medullaris to the dural sac, and the filum terminale externum, which connects the dural sac to the coccyx [20]. A common cause of TCS, fatty filum terminale develops when the filum, which is normally a viscoelastic band that allows the conus medullaris to move slightly during spinal extension and flexion, is infiltrated with adipose tissue and becomes thickened. When there is excessive stress and traction caudally on the conus medullaris, the end result is a tethered cord [21]. Understanding the embryology of this condition, and other forms of TCS, is vital for understanding how such lesions occur: errors during secondary neurulation, when the distal spine caudal to S2 and the filum terminale form [22]. Errors during canalization or regression of the caudal cell mass between days 28 and 48 are believed to contribute to the formation of a low-lying conus, terminal lipomas, and fatty filum terminale [6]. McLendon et al. demonstrated that adipose tissue is a common finding in patients with TCS and can often be detected by computed tomography scans [21]. They suggest that adipose in the filum is not diagnostic for tethering of the spinal cord, but if the adipose is picked up by CT scans then the clinician should ask “is there tethering?” They also note that adipose tissue can be found in the filum terminale in about 19% of the asymptomatic adult population, while only 6% were detectable by CT. Tight filum terminale or fatty filum is said to constitute as many as 25% of all lesions causing TCS [22]. Interestingly, this common cause of TCS has been associated with pain and with urinary dysfunction. Urological and neurological symptoms are a function of the magnitude and duration of traction placed on the spinal cord. Traction that has been sustained for a long time could potentially result in more severe and irreversible neurological dysfunction.
Finn et al. recently recommended that for symptomatic conus lipomas and filum lipomas, the treatment should be surgical intervention. If the patients are asymptomatic with a fatty filum, then close observation will suffice [23]. Most people consider surgical intervention appropriate for symptomatic patients with TCS and low-lying conus [24].
One study of 293 patients with TCS revealed that 190 (64.8%) had fatty filum terminale [25]. In another study of 33 patients with split cord malformations, 26 (78.8%) had a fatty filum terminale [26]. Approximately 67% of patients with syringomyelia have an associated fatty or tight filum terminale [27].
Neurocutaneous melanosis (NCM) , where large congenital melanocytic nevi are associated with melanocytic deposits in the leptomeninges, has been identified in five cases over a 12-year period, all five patients having one or more spinal abnormalities. Three (60%) had a low-lying conus medullaris , of whom two had a fatty filum terminale causing a tethered cord [28].
Split Cord Malformation
Another major group considered part of the TCS spectrum is split cord malformation (SCM), diastematomyelia or diplomyelia (two hemicords). Diastematomyelia is a closed neural tube defect in which the spinal cord is longitudinally split by a fibrous band or a bone spicule. Split cord syndrome can refer to either diastematomyelia or diplomyelia. The nomenclature has been revised recently to eliminate some of the confusion in the literature. Diastematomyelia is a split cord in which the two halves are separated by a bone spicule and contained within separate dural sleeves; in diplomyelia the two hemicords lie within a common dural sac, more commonly with two complete sets of nerve roots, divided by a fibrous band [29]. In this section, we will use SCM and diastematomyelia interchangeably.
Diastematomyelia , found in a quarter of OSD patients, is thought to develop before primary neurulation or more specifically during gastrulation. Pang suggested that it arises during development when adhesions occur between the endoderm and the ectoderm, leading to the formation of a mesenchymal tract splitting the spinal cord [30]. The spinal cord is tethered at the level of the bisecting bony spur/dorsal band and/or by a fatty filum terminale. Clinical examination of these patients reveals cutaneous stigmata such as tufts of lumbosacral hair. About 85% of patients diagnosed with confirmed diastematomyelia demonstrated bony abnormalities, and 50% presented with scoliosis.
In previous studies [30], the symptoms of SCM were described as similar to those in TCS. Pang found that the adult SCM population he studied had severe pains in the legs and perineum with additional sensorimotor findings. Children presented slightly differently, with gait abnormalities but with less pain and progressive spinal and foot deformities. Proctor and Scott (2001) found that while some patients with SCM presented with obvious urological symptoms, formal testing revealed occult urological abnormalities in as many as 75% [29]. Pérez et al. presented comparable results and recommendations. They studied 27 patients with SCM, 14 of whom had urological complaints, most commonly urge incontinence [31]. They suggest that all patients with confirmed SCM should undergo formal urological testing.
A characteristic of SCM is its unique tandem prevalence with other nervous system lesions, specifically fatty filum terminale, lipomyelomeningocele, myelomeningocele, and Chiari malformations. A recent study of 113 patients showed that 56 had one spinal cord lesion and 76 had two or more. One hundred and thirteen patients (100%) had a tight filum terminale, 26 (23.0%) a myelomeningocele, 23 (20.4%) a myelomeningocele manqué, 19 (16.8%) a meningocele, 12 (10.6%) an intradural lipoma, 8 (7.1%) a dermal sinus tract, 7 (6.2%) a hemimyelomeningocele, 6 (5.3%) an epidermoid, 5 (4.4%) a dermoid, 5 (4.4%) a lipomyelomeningocele, 5 (4.4%) an intrasacral meningocele, 4 (3.5%) a second SCM at a different vertebral level, and 1 (0.88%) a teratoma [32]. Another more recent study showed that 33 patients with diastematomyelia had a 78.8% likelihood of tandem thick filum terminale, 9.1% had dermal sinus tracts, and 6.1% a lipomyelomeningocele [26]. One source cites up to 38% of patients with SCM having simultaneous syringomyelia [27]. More recently, other studies have confirmed that upward of 50–85% of patients with SCM have a secondary comorbidity. Albright et al. mention that scoliosis in patients with a tethered cord and SCM is as high as 90% [27].
Lipomyelomeningocele
Lipomyelomeningocele (LMMC), or conus lipoma, a lipoma of the conus medullaris, is another key group of OSDs that leads to tethering of the spinal cord (TCS). LMMC results from an error during the first part of spinal cord formation, primary neurulation. Primary neurulation involves folding of the neuroectoderm and formation of the neural tube that becomes the spinal cord. This occurs on postovulatory day (POD) 18. The notochord induces the overlying ectoderm to proliferate as neuroectoderm, forming a groove that progressively elevates until it fuses and forms the neural tube. Superficial ectoderm separates from the neuroectoderm and fuses at the midline during disjunction. The mesoderm forms the posterior bony and soft tissue elements. Premature disjunction occurs when migration of the mesodermal elements that eventually form fatty tissue leads to a defect covered with skin or a closed defect due to ectodermal fusion preceding formation.
In previous studies it was noted that LMMC has a female to male ratio of 2:1 and an incidence rate of 1:400 [22]. Patients classically present with bladder dysfunction, intractable pain, cutaneous stigmata, and progressive neurological motor and sensory decline [33]. LMMCs are the most common type of spinal lipomas [23]. Commonly, investigation begins by noting cutaneous markers such as a subcutaneous lumbosacral mass, found in approximately 90% of patients. LMMC is commonly diagnosed during infancy [23, 34]. Other common stigmata are skin dimples, hemangiomas, hair patches, skin tags, and depigmented regions. While cutaneous signs and neurological deficits are common, up to 48% of patients are completely asymptomatic and normal at presentation. As with other spinal dysraphisms, there is a strong neurological and urological deficit, the urological deficit being the most common initial neurological manifestation, seen in as many as 60% of patients with LMMC [35]. These patients have a progressive and downward deterioration of urological and neurological function. In one study, 62.5% of patients who presented at less than 6 months of age and 29% of those presenting at more than 6 months were asymptomatic [36]. In another study of 34 patients, all children above the age of 5 years were symptomatic, while all those under 4 years old were asymptomatic [37]. A large retrospective review on outcomes of patients with LMMC found that urological and bowel dysfunction did not improve over time. However, motor and sensory symptoms did show signs of recovery as 10 of the 11 patients undergoing surgical retethering went back to their preoperative functional status. Although asymptomatic patients are common, natural progression of the disease leads to neurological and urological deterioration, urinary bladder dysfunction typically occurring in the age range 0–2 years, while motor and sensory symptoms progress later in life, typically in the teenage and young adolescent years [38]. Early diagnosis, surgical intervention, and untethering are crucial for minimizing otherwise catastrophic neurological dysfunction [33].
As in other OSDs, the literature describes some peculiar yet interesting associations of LMMCs. TCS is fundamentally linked to LMMCs as the lipoma anchors the cord to the adjacent dura and soft tissue [39]. In a study of 97 patients, Hoffman et al. found a few common associations and noted that 4% had urological anomalies, 3.1% terminal hydromyelia, 3.1% dermal sinuses, 3.1% SCM, 3.1% dermoid and/or epidermoid cysts, 3.1% diastematomyelia, 1.0% anal stenosis, and 1.0% Down syndrome (trisomy 21) [36]. To compound these findings, Kanev et al. noticed a different set of anomalies in their patient set. Among 80 patients with confirmed LMMC observed over 35 years, 8.75% had scoliosis, 7.5% an amniotic band extremity deformity, 5.0% sacral dysgenesis, 2.5% hydromyelia, and 2.5% stenosis. More recently, Tubbs et al. noticed that Chiari type I malformation had a higher incidence in patients with LMMC than the general population. Among their 54 patients, roughly 13% with a Chiari malformation had a tandem LMMC [40]. Agopian et al. found 14.4% of their spina bifida patients to have LMMC [41, 42]. Currarino syndrome is often associated with LMMC, which is considered one part of the “triad of Currarino.” The triad consists of an anorectal malformation (ARM), a sacral vertebral bony defect, and a presacral mass [14]. In 1 study of 13 patients with Currarino syndrome , 5 (38.4%) had LMMC [13]. To our knowledge, the literature describes two patients with LMMC together with duplication of the spine [43, 44]. The most common neural tube defects are encephalocele and myelomeningocele, and we discovered one case report of a patient who had a LMMC, complete situs inversus, occipital encephalocele, and tetralogy of Fallot. This was the first such case described and invites further research into links or associations between OSD and encephaloceles [45]. Among 11 patients identified with a collection of anomalies and lesions known as PELVIS syndrome (perineal hemangioma, external genitalia malformations, LMMC, vesico-renal abnormalities, imperforate anus, and skin tag), 3 (27.3%) had a LMMC [46]. Sirenomelia or mermaid syndrome was found in one study in which all five patients with cloacal exstrophy had some form of OSD: four had terminal myelocystoceles and one had a LMMC [47]. Another case report identified a sacrococcygeal teratoma associated with a tethered spinal cord during the 23rd week of pregnancy by ultrasonography [15]. One study noted that up to 21% of patients with LMMC had associated syringomyelia [48]. Tubbs et al. found two patients with LMMC associated with Pacinian corpuscles [49].
Neurenteric Cysts of the Spine
First described by Puusepp in 1934, neurenteric (NE) cysts are erratic lesions of the central nervous system that are lined with intestinal epithelium [50]. The World Health Organization describes neurenteric cysts as “lined by mucin-secreting epithelium resembling that of the gastrointestinal tract” [51]. Spinal neurenteric cysts are congenital abnormalities derived from an anomalous connection between the primitive endoderm and ectoderm during the third week of life. The cysts are considered endodermal in origin because of such markers as vertebral anomalies, gut cysts, bowel reduplication, and keratin markers [52]. They have acquired numerous different names in the literature such as neurenteric cyst, enterogenous cyst, enteric cyst, gastrocytoma, dorsal enteric fistula, split notochord syndrome, and teratoid cyst [52]. Neurenteric cysts are not limited to the spinal column but can be found in other areas of the body, specifically the brain, mediastinum, abdominal cavity, and pelvis [53]. These alternative locations are rare, intraspinal neurenteric cysts accounting for 0.3–0.5% of all spinal “tumors” [54]. Neurenteric cysts are not true tumors in the traditional sense in that they do not arise from teratomas, but more closely resemble hamartomas, which are displaced pockets of endodermally derived tissue [49].
Neurenteric cysts can be located anywhere in the spine and present differently. Rauzzino et al. had 13 patients, ages ranging from 5 weeks to 52 years, most presenting early in life, classically during the first two decades, while older patients presented during their fourth decade. Presentation varied, younger patients presenting with the class of cutaneous markers associated with OSD, older ones with neurological dysfunction and pain. Their locations ranged from C2 to L5, with no lesions in the craniocervical junction. The cysts have most commonly been found in relation to the spinal cord, dorsal to the spinal cord as intradural and extramedullary masses and occasionally as an extradural dorsal mass. The second most common location for them is intramedullary, followed by anterolateral and anterior positions. Common locations along the vertebral column are thoracolumbar, upper thoracic, cervical spine, and lower lumbar region, in sequence from most common to least common [52].
Intraspinal neurenteric cysts can be stand-alone but have also been found with tandem congenital anomalies, 50% of presentations being accompanied by vertebral anomalies including vertebral defects, Klippel-Feil syndrome, spondylolisthesis and other congenital defects such as meningomyelocele, syringomyelia, spinal lipoma, diastematomyelia, and intramedullary epidermoid cysts [55, 56]. Other simultaneous anomalies were mentioned in the study by Arai et al.; among their 43 cases with neurenteric cysts, two patients had grossly abnormal vertebral bodies, and two had myelomeningoceles [57]. Years later, Rauzzino and colleagues studied 13 patients and noted that 12 of them (92%) had a vertebral malformation in addition to the neurenteric cysts. Eight (62%) had posterior vertebral column abnormalities in the form of spina bifida, five (39%) had anterior vertebral column abnormalities, two (15%) had Klippel-Feil abnormalities, and two (15%) had scoliosis. They also noted that 69% of their patients had another form of spinal dysraphism, 31% having split cord malformations, 31% intradural lipoma, 23% fatty filum terminale, and 8% each having meningocele, meningocele manqué, and syringomyelia [52].
Compression of the spinal cord by neurenteric cysts and inflammatory reaction to the cysts’ inner contents are the aggravators of most presenting symptoms [58]. Pain is the primary complaint, either radicular (31%) or local (54%), but there are other presentations, albeit rare, such as aseptic and bacterial meningitis, chronic pyrexia, and paraplegia [59, 60]. In some patients, symptoms have been reported to fluctuate, the two main hypotheses suggesting either the cyst itself ruptures or changes in the rates of mucin synthesis and reabsorption by the cyst wall [61, 62]. Classically, neurenteric cysts are insidious and even asymptomatic, so diagnosis is often delayed until the patients have suffered critical motor loss or other significant neuropathies [63].
Imaging modalities include plain spine roentgenograms, computed tomography (CT), and magnetic resonance imaging (MRI), the last named being the quintessential diagnostic modality [64].
Neurenteric cysts can easily be seen on MRI as hypointense on T1-weighted (T1WI) scans and hyperintense to isointense on T2WI scans compared to cerebrospinal fluid (CSF) [65]. The cystic fluid can appear hyperintense to isointense in comparison to CSF on both T1WI and T2WI owing to different protein content in the cyst fluid or to hemorrhage within the cyst itself. Rim enhancement is rarely achieved by contrast medium [65]. There are various surgical approaches, and one may choose one over the other depending on the location and level of the lesion [66,67,68].
Dermal Sinus Tracts of the Spine
Congenital dermal sinuses, a distinctive form of OSD that presents classically with meningitis, neural compression, and TCS, occur in about one in every 1500 births [69]. Dermal sinus tracts are lined with simple squamous epithelium and can penetrate anywhere in the midline from the occiput to the lumbosacral region [70]. The dermal sinus tract can traverse multiple spinal levels before it crosses the dural defect to an attachment on the spinal cord or filum terminale [71]. The etiology is thought to be failure during disjunction, causing adhesion between the neural and cutaneous ectoderm [72]. During embryological development the ectoderm separates into two distinct portions, the neuroectoderm and the cutaneous ectoderm. This process, known as “disjunction,” is thought to be the source of the error responsible for forming dermal sinus tracts, sometimes referred to as “incomplete disjunction.” This abnormal disjunction, or failure to separate fully, takes place around the fourth week of development during primary neurulation. Gupta et al. found a correlation of 11.34% between dermal sinus tracts and other forms of spinal dysraphism [73]. Dermal sinus tracts can be associated with other abnormalities such as myelomeningocele, LMMC, and SCM [30]. Roughly 60% of dermal sinus tracts enter the subarachnoid space with up to 27% attached to the neural elements of the conus medullaris and filum terminale [74]. According Kanev and Park, the tracts can also end blindly within the extradural space in as many as 20% of patients and rarely end subcutaneously or within the paraspinal muscles [71].
Patients present classically with cutaneous stigmata such as a pit or dimple just superior to the intergluteal crease. Some patients also have skin tags, lipomas (subcutaneous), hairy patches or hypertrichosis, and hemangiomas. A rare finding, a pseudotail, a dermal appendage, has been reported recently in the literature associated with OSD, specifically alongside dermal sinus tracts [75]. The most common location for these stigmata is the lower lumbar or lumbosacral region, thoracic and cervical sinuses being significantly rarer [69]. Kanev and Park report an apparent male preponderance and infer that a family history of spinal dysraphism is highly unlikely. They state that all midline skin pits above the intergluteal fold should be assumed to communicate with intraspinal elements. Importantly, midline skin pits below the top of the intergluteal crease are blind to sacrococcygeal dimples, and there are no connections between the surface and intraspinal elements [71]. Dermal sinuses are dangerous because they can foster bacterial overgrowth and cause catastrophic infection, particularly meningitis and abscesses. They occur in approximately 50% of cases, the most common organisms being Staphylococcus aureus and Escherichia coli . Multiple episodes of meningitis and abscess can occur until the sinus tract is repaired [76].
Most patients have intact neurological functions at birth, but as they age and go through their growth spurts, symptoms begin to arise similar to those of other OSDs: pain, abnormal curvature of the spine, orthopedic deformities, gait disturbances, sensory and motor deficits, urological dysfunction, and weakness [77].
Ultrasonography easily identifies the subcutaneous tracts and also lesions associated with the dermal sinus tract, such as intraspinal inclusion tumors. Computed tomography using fine-section slices with sagittal reconstructions after administration of an intrathecal contrast agent is the method of choice for locating the bony landmarks and sinus tract attachment point. However, CT myelography is not recommended if a superficial sinus infection is suspected, as introducing the contrast agent can cause the organisms to spread to the CSF. Recently, CT studies have been replaced by high-resolution MRI, giving the provider a three-dimensional visualization of the tract path and other associated malformations. The sinus tract appears as a low-intensity tract that climbs into the subcutaneous tissue with high intensity on both T1- and T2-weighted images [78]. In contrast to the advantages of modern MRI, a normal MRI does not exclude the diagnosis of a sinus tract. Only about 40% of dermal sinus tracts are detected by preoperative MRI, so if the MRI is normal and the tract is above the gluteal crease, surgical exploration is recommended [79].
Regardless of patient age or neurological pathology, dermal sinuses above the intergluteal crease should be surgically removed at the time of diagnosis to prevent future neurological sequelae and catastrophic infections [71]. Radmanesh et al. suggest that all dermal sinus tracts above the sacrococcygeal region should be explored operatively regardless of imaging [80]. A high index of suspicion is warranted for all dimples above the intergluteal fold regardless of imaging data. Any midline dimples need to be examined carefully when an infant suffers from meningitis caused by unusual organisms. Conservative treatment is contraindicated, and surgery should be carried out prophylactically on patients with advanced neurological deficits, to slow the advance of neurological compromise [81].
In 1 study of 33 patients, 3 (9.1%) with split cord malformations had a dermal sinus tract [26]. Dermal sinus tracts have been discussed in the literature. A case report identified 20 individuals with encephaloceles , a congenital malformation involving protrusion of the meninges and/or brain tissue, one of whom (5%) had a dermal sinus tract [82]. Radmanesh et al. described dermoid cysts as the neoplasms most commonly associated with dermal sinus tracts [83]. One study reported an association of 73% between dermal sinus tracts and dermoid inclusion cysts [80], though another study reported a lower association with a value of up to 50% [80].
Terminal Syringomyelia (Syrinx)
Syringomyelia is a fluid-filled cavity within the spinal cord and was first described by Ollivier d’Angers in 1827. Terminal syringomyelia, i.e., involving the distal third of the cord is a component of occult spinal dysraphism. Like many other OSDs, syringomyelia has been associated with myelomeningocele, LMMC, split cord malformation, Chiari type I/II malformations, and TCS. One review of 143 OSD cases over 20 years revealed that 24 (27%) of the 90 patients imaged with MRI had a terminal syrinx [84, 85]. Iskandar et al. found a 3:2 female to male ratio, the most common presenting symptoms of a terminal syrinx being scoliosis, back pain, bowel and urological dysfunction, and a multitude of neurological deficits.
The pathogenesis of syringohydromyelia is still contested, but many articles refer to the hydrodynamic hypothesis of Gardner and Goodall [86]. This is based on the premise that there are pressure differences between the brain and spinal canal. Gardner and Goodall propose that an obstruction in the fourth ventricle or at the level of the foramen magnum increases hydrostatic pressure and causes a shift of CSF from the brain to the central spinal canal. Other hypotheses propose a pathogenesis of syringomyelia secondary to arachnoiditis, trauma, and neoplasm. They suggest that ischemic changes in the spinal cord due to hypovolemia, arachnoiditis-induced compartmentalization of the spinal canal, epidural venous congestion, and cystic degeneration of a neoplasm could all cause pressure differentials and shift CSF from areas of high to low pressure [85].
Classically, patients present with motor weakness, sensory and sphincter disturbances, and pain. There can be significant trunk weakness in some patients who have tandem scoliosis caused by the syrinx. Scoliosis and motor weakness are insidious in onset. In common with other OSD malformations, urological dysfunction is associated with syringomyelia. In the study by Iskandar et al., at least 16 (59%) of 27 patients with terminal syringohydromyelia had some form of scoliosis, and this is consistent with other studies showing a correlation between scoliosis and syringohydromyelia [87]. In the study by Iskandar et al., every patient had one or more tandem OSD malformations. Foot deformities, hypertrichosis, and capillary hemangiomas have been reported in other studies [88].
As with other OSD malformations, diagnosis is best made via high-resolution MRI with and without gadolinium enhancement. Gadolinium contrast agent allows for easy identification of the syrinx and demonstrates its magnitude and reveals any other OSD defects unknown to the provider [89].
Management can be difficult to navigate for this complex disorder. Anderson et al. followed 20 patients over 10 years without intervening surgically and found that about 35% showed no progression of symptoms, 55% had progressive symptoms, and 10% had showed intermittent progression after the initial presentation [90]. There are three broad categories of surgical treatment ultimately based around the differing hypotheses concerning the pathogenesis of syringomyelia. The first surgical approach is based on the Gardner and Goodall hydrodynamic hypothesis. The second group of operations is based on aspirating the cystic contents of the syrinx and the third category on lumboperitoneal shunting with the aim of lowering the craniospinal pressure gradients [37].
Terminal syringomyelia , like other OSDs, has common associations. The most common forms of OSD associated with syringomyelia are SCM, LMMC, myelomeningocele, and thickened filum terminale [91]. Syringomyelia is found in up to one third of OSD cases investigated by MRI scans [27]. Logue and Edwards studied 75 patients with syringomyelia and found that roughly 50% had scoliosis and a Chiari type I malformation [92], while another more recent study showed that 37 (13.5%) of 275 patients with syringomyelia had scoliosis [87]. Another recent study of 163 patients with syringomyelia showed that 59 (36%) had a low neck or hair line, 8 (4.9%) hydrocephalus, 1 (0.61%) Dandy-Walker syndrome, 54 (33.1%) kyphoscoliosis, 1 (0.61%) brain stem glioma, 4 (2.5%) a spinal cord tumor, and 4 (2.5%) an atlantoaxial dislocation [93]. The most common association with syringomyelia is the Chiari type I malformation, the hindbrain hernia. A study of 68 patients with Chiari type I malformation showed that up to 40% had syringomyelia between levels C4 and C6 [94]. Patients with myelomeningoceles had syringomyelia in up to 45% of cases [48, 95].
Conclusions
Many diagnoses may also have an associated form of the occult spinal dysraphisms. Each of these should be investigated in order to minimize long-term consequences of an untreated or unrecognized tethered spinal cord.
References
Lichtenstein B. Spinal dysraphism. Arch Neurol Psychiatr. 1940;44(4):792.
McCormick P, Kaiser M, Angevine P, Ogden A, Mandigo C, Lo L, Anderson R, Feldstein N. Tethered spinal cord – The Spine Hospital at The Neurological Institute of New York. [online] The Spine Hospital at The Neurological Institute of New York; 2017. Available at: http://columbiaspine.org/condition/tethered-spinal-cord/. Accessed 3 Jul 2017.
Fuchs A. Über Beziehungen der Enuresis nocturna zu Rudimentärformen der Spina bifida occulta (myelodysplasie). Ann Surg. 1910;131:109–16.
Garceau G. The filum terminale syndrome. J Bone Joint Surg. 1953;35(3):711–6.
Hoffman H, Hendrick B, Humphreys R. The tethered spinal cord: its protean manifestations, diagnosis and surgical correction. Childs Brain. 1976;2:145–55.
Lew S, Kothbauer K. Tethered cord syndrome: an updated review. Pediatr Neurosurg. 2007;43(3):236–48.
Yamada S, Zinke D, Sanders D. Pathophysiology of “tethered cord syndrome”. J Neurosurg. 1981;54(4):494–503.
Koçak A, Kılıç A, Nurlu G, Konan A, Kılınç K, Çırak B, Çolak A. A new model for tethered cord syndrome: a biochemical, electrophysiological, and electron microscopic study. Pediatr Neurosurg. 2008;26(3):120–6.
Warder D, Oakes W. Tethered cord syndrome and the conus in a normal position. Neurosurgery. 1993;33(3):374–8.
Khoshhal K, Murshid W, Elgamal E, Salih M. Tethered cord syndrome: a study of 35 patients. J Taibah Univ Med Sci. 2012;7(1):23–8.
Hertzler D, DePowell J, Stevenson C, Mangano F. Tethered cord syndrome: a review of the literature from embryology to adult presentation. Neurosurg Focus. 2010;29(1):E1.
Kuo M, Tsai Y, Hsu W, Chen R, Tu Y, Wang H. Tethered spinal cord and VACTERL association. J Neurosurg Pediatr. 2007;106(3):201–4.
Emans P, Kootstra G, Marcelis C, Beuls E, van Heurn L. The Currarino triad: the variable expression. J Pediatr Surg. 2005;40(8):1238–42.
AbouZeid A, Mohammad S, Abolfotoh M, Radwan A, Ismail M, Hassan T. The Currarino triad: what pediatric surgeons need to know. J Pediatr Surg. 2017;52(8):1260–8.
Sivrikoz T, Has R, Esmer A, Kalelioglu I, Yuksel A, Taskin O. Prenatal diagnosis of tethered spinal cord associated with sacrococcygeal teratoma. J Clin Ultrasound. 2016;44(8):506–9.
Chen S, Peng S, Kuo M, Lee W, Liang J. Miller-Dieker syndrome associated with tight filum terminale. Pediatr Neurol. 2006;34(3):228–30.
Hsieh D, Jennesson M, Thiele E, Caruso P, Masiakos P, Duhaime A. Brain and spinal manifestations of Miller-Dieker syndrome. Neurol Clin Pract. 2013;3(1):82–3.
Milhorat T, Bolognese P, Nishikawa M, Francomano C, McDonnell N, Roonprapunt C, Kula R. Association of Chiari malformation type I and tethered cord syndrome: preliminary results of sectioning filum terminale. Surg Neurol. 2009;72(1):20–35.
Glenn C, Cheema A, Safavi-Abbasi S, Gross N, Martin M, Mapstone T. Spinal cord detethering in children with tethered cord syndrome and Chiari type 1 malformations. J Clin Neurosci. 2015;22(11):1749–52.
De Vloo P, Monea A, Sciot R, van Loon J, Van Calenbergh F. The filum terminale: a cadaver study of anatomy, histology, and elastic properties. World Neurosurg. 2016;90:565–573.e1.
McLendon R, Oakes J, Heinz R, Yeates A, Burger P. Adipose tissue in the filum terminale: a computed tomographic finding that may indicate tethering of the spinal cord. Neurosurgery. 1988;22(5):873–6.
Blount J, Elton S. Spinal lipomas. Neurosurg Focus. 2001;10(1):1–13.
Finn M, Walker M. Spinal lipomas: clinical spectrum, embryology, and treatment. Neurosurg Focus. 2007;23(2):1–12.
Jallo G, Kothbauer K, Pradilla G. Controversies in pediatric neurosurgery. New York: Thieme; 2010.
Thompson E, Strong M, Warren G, Woltjer R, Selden N. Clinical significance of imaging and histological characteristics of filum terminale in tethered cord syndrome. J Neurosurg Pediatr. 2014;13(3):255–9.
Barutcuoglu M, Selcuki M, Selcuki D, Umur S, Mete M, Gurgen S, Umur. Cutting filum terminale is very important in split cord malformation cases to achieve total release. Childs Nerv Syst. 2014;31(3):425–32.
Albright A, Pollack I, Adelson P. Principles and practice of pediatric neurosurgery. 2nd ed. New York: Thieme; 2008. p. 366–93.
Tian A, Foster K, Jakacki R, Reyes-Múgica M, Greene S. Neurocutaneous melanosis is associated with tethered spinal cord. Childs Nerv Syst. 2014;31(1):115–21.
Proctor M, Scott R. Long-term outcome for patients with split cord malformation. Neurosurg Focus. 2001;10(1):1–5.
Pang D. Split cord malformation. Neurosurgery. 1992;31(3):481–500.
Pérez L, Barnes N, MacDiarmid S, Oakes W, Webster G. Urological dysfunction in patients with diastematomyelia. J Urol. 1993;149(6):1503–5.
Erşahin Y. Split cord malformation types I and II: a personal series of 131 patients. Childs Nerv Syst. 2013;29(9):1515–26.
Abu-Bonsrah N, Purvis T, Rory Goodwin C, Petteys R, De la Garza-Ramos R, Sciubba D. Adult cervicothoracic lipomyelomeningocele. J Clin Neurosci. 2016;32:157–9.
Barry A, Patten B, Stewart B. Possible factors in the development of the Arnold-Chiari malformation. J Neurosurg. 1957;14(3):285–301.
Warder D. Tethered cord syndrome and occult spinal dysraphism. Neurosurg Focus. 2001;10(1):1–9.
Hoffman H, Taecholarn C, Hendrick E, Humphreys R. Management of lipomyelomeningoceles. J Neurosurg. 1985;62(1):1–8.
Koyanagi I, Iwasaki Y, Hida K, Abe H, Isu T, Akino M. Surgical treatment of syringomyelia associated with spinal dysraphism. Childs Nerv Syst. 1997;13(4):194–200.
Kanev P, Lemire R, Loeser J, Berger M. Management and long-term follow-up review of children with lipomyelomeningocele, 1952–1987. J Neurosurg. 1990;73(1):48–52.
Barkovich A, Raybaud C. Pediatric neuroimaging. 3rd ed. Philadelphia: Wolters Kluwer; 2000. p. 641.
Tubbs R, Bui C, Rice W, Loukas M, Naftel R, Holcombe M, Oakes W. Critical analysis of the Chiari malformation type I found in children with lipomyelomeningocele. J Neurosurg Pediatr. 2007;106(3):196–200.
Agopian A, Canfield M, Olney R, Lupo P, Ramadhani T, Mitchell L, Shaw G, Moore C. Spina bifida subtypes and sub-phenotypes by maternal race/ethnicity in the National Birth Defects Prevention Study. Am J Med Gen Part A. 2011;158A(1):109–15.
Sarris C, Tomei K, Carmel P, Gandhi C. Lipomyelomeningocele: pathology, treatment, and outcomes. Neurosurg Focus. 2012;33(4):E3.
Yiğit H, Özdemir H, Yurduseven E. Duplication of spine with hemi-lipomyelomeningocele. Eur Spine J. 2013;22(S3):487–90.
Levitt M, Dlugy E, Kravarusic D, Ben-Meir D, Rajz G, Konen O, Freud E, Samuk I. Caudal duplication syndrome: the vital role of a multidisciplinary approach and staged correction. Eur J Pediatr Surg Rep. 2015;04(01):001–5.
Franco A, Jo S, Mehta A, Pandya D, Yang C. A rare triad of giant occipital encephalocele with lipomyelomeningocele, tetralogy of fallot, and situs inversus. J Radiol Case Rep. 2016;10(3):36–46.
Girard C, Bigorre M, Guillot B, Bessis D. PELVIS syndrome. Arch Dermatol. 2006;142(7):884–8.
Cohen A. The mermaid malformation: cloacal exstrophy and occult spinal dysraphism. Neurosurgery. 1991;28(6):834–43.
Piatt J. Syringomyelia complicating myelomeningocele: review of the evidence. J Neurosurg Pediatr. 2004;100(2):101–9.
Tubbs R, Kelly D, Mroczek-Musulman E, Oakes W. Occult spinal 91dysraphism and Pacinian hamartomas. Childs Nerv Syst. 2005;21(4):343–4.
Puusepp M. Variété rare de tératome sous-dural de al region cervicale (intestinome): Quadriplégie, extirpation, guérison complète. Rev Neurol. 1934;2:879–86.
Zülch K. Histological typing of tumours of the central nervous system. Geneva: World Health Organization; 1979.
Rauzzino M, Tubbs R, Alexander E, Grabb P, Oakes W. Spinal neurenteric cysts and their relation to more common aspects of occult spinal dysraphism. Neurosurg Focus. 2001;10(1):1–10.
Alrabeeah A, Gillis D, Giacomantonio M, Lau H. Neurenteric cysts—a spectrum. J Pediatr Surg. 1988;23(8):752–4.
Menezes A, Ryken T. Craniocervical intradural neurenteric cysts. Pediatr Neurosurg. 1995;22(2):88–95.
Mann K, Khosla V, Gulati D, Malik A. Spinal neurenteric cyst. Association with vertebral anomalies, diastematomyelia, dorsal fistula, and lipoma. Surg Neurol. 1984;21(4):358–62.
Santos de Oliveira R, Cinalli G, Roujeau T, Sainte-Rose C, Pierre-Kahn A, Zerah M. Neurenteric cysts in children: 16 consecutive cases and review of the literature. J Neurosurg Pediatr. 2005;103(6):512–23.
Arai Y, Yamauchi Y, Tsuji T, Fukasaku S, Yokota R, Kudo T. Spinal neurenteric cyst. Spine. 1992;17(11):1421–3.
Paleologos S, Thom M, Thomas DG. Spinal neurenteric cysts without associated malformations. Are they the same as those presenting in spinal dysraphism? Br J Neurosurg. 2000;14(3):185–94.
Kumar R, Nayak S. Unusual neuroenteric cysts: diagnosis and management. Pediatr Neurosurg. 2002;37(6):321–30.
Cai C, Shen C, Yang W, Zhang Q, Hu X. Intraspinal neurenteric cysts in children. Can J Neurol Sci. 2008;35(05):609–15.
Lippman C, Arginteanu M, Purohit D, Naidich T, Camins M. Intramedullary neurenteric cysts of the spine. J Neurosurg Spine. 2001;94(2):305–9.
Rao M, Rout D, Misra B, Radhakrishnan V. Craniospinal and spinal enterogenous cysts—report of three cases. Clin Neurol Neurosurg. 1996;98(1):32–6.
Rotondo M, D’Avanzo R, Natale M, Pasqualetto L, Bocchetti A, Agozzino L, Scuotto A. Intramedullary neurenteric cysts of the spine. J Neurosurg Spine. 2005;2(3):372–6.
Menezes A, Traynelis V. Spinal neurenteric cysts in the magnetic resonance imaging era. Neurosurgery. 2006;58(1):97–105.
Preece M, Osborn A, Chin S, Smirniotopoulos J. Intracranial neurenteric cysts: imaging and pathology spectrum. Am J Neuroradiol. 2006;27(6):1211–6. Available at: https://www.ncbi.nlm.nih.gov/pubmed/16775266.
Tuzun Y, Izci Y, Sengul G, Erdogan F, Suma S. Neurenteric cyst of the upper cervical spine: excision via posterior approach. Pediatr Neurosurg. 2005;42(1):54–6.
Devkota U, Lam J, Ng H, Poon W. An anterior intradural neurenteric cyst of the cervical spine. Neurosurgery. 1994;35(6):1150–3.
Garg N, Sampath S, Yasha T, Chandramouli B, Indira Devi B, Kovoor J. Is total excision of spinal neurenteric cysts possible? Br J Neurosurg. 2008;22(2):241–51.
Powell K, Cherry J, Hougen T, Blinderman E, Dunn M. A prospective search for congenital dermal abnormalities of the craniospinal axis. J Pediatr. 1975;87(5):744–50.
Amacher L, Hovind L. Intracranial tumefactions in children. Pediatr Neurosurg. 1979;5(6):518–29.
Kanev P, Park T. Dermoids and dermal sinus tracts of the spine. Neurosurg Clin N Am. 1995;6:359–66. Available at: https://www.ncbi.nlm.nih.gov/pubmed/7620359.
French B. The embryology of spinal dysraphism. Clin Neurosurg. 1983;30:295–340. Available at: https://www.ncbi.nlm.nih.gov/pubmed/6365396.
Gupta D, Shastank R, Mahapatra A. An unusual presentation of lumbosacral dermal sinus with CSF leak and meningitis. Pediatr Neurosurg. 2005;41(2):98–101.
Naidich T, Hardwood-Nash D, McLone D. Radiology of spinal dysraphism. Clin Neurosurg. 1983;30:341–65.
Clark P, Davidson L. Case report: pseudotail with dermal sinus tract and tethered cord. J Ultrasound. 2016;19(3):239–41.
Shah R, Chaljub G, Swischuk L. Lower cervical dermal sinus tract and associated intraspinal abscess causing meningitis in a child. Emerg Radiol. 2003;10(3):160–2.
Mete M, Umur A, Duransoy Y, Barutçuoğlu M, Umur N, Gurgen S, Selçuki M. Congenital dermal sinus tract of the spine. J Child Neurol. 2014;29(10):1277–82.
O’Neill B, Gallegos D, Herron A, Palmer C, Stence N, Hankinson T, Corbett Wilkinson C, Handler M. Use of magnetic resonance imaging to detect occult spinal dysraphism in infants. J Neurosurg Pediatr. 2017;19(2):217–26.
Ackerman L, Menezes A. Spinal congenital dermal sinuses: a 30-year experience. Pediatrics. 2003;112(3):641–7.
Radmanesh F, Nejat F, El Khashab M. Dermal sinus tract of the spine. Childs Nerv Syst. 2009;26(3):349–57.
Singh I, Rohilla S, Kumar P, Sharma S. Spinal dorsal dermal sinus tract: an experience of 21 cases. Surg Neurol Int. 2015;6(18):429.
Ramdurg S, Sukanya M, Maitra J. Pediatric encephaloceles: a series of 20 cases over a period of 3 years. J Pediatr Neurosci. 2015;10(4):317.
Thompson D. Spinal inclusion cysts. Childs Nerv Syst. 2013;29(9):1647–55.
Newton E. Syringomyelia as a manifestation of defective fourth ventricular drainage. Ann R Coll Surg Engl. 1969;44:194–213. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2387612/.
Iskandar B, Oakes J, McLaughlin C, Osumi A, Tien R. Terminal syringohydromyelia and occult spinal dysraphism. J Neurosurg. 1994;81(4):513–9.
Gardner W, Goodall R. The surgical treatment of Arnold-Chiari malformation in adults. J Neurosurg. 1950;7(3):199–206.
Rodriguez A, Kuhn E, Somasundaram A, Couture D. Management of idiopathic pediatric syringohydromyelia. J Neurosurg Pediatr. 2015;16(4):452–7.
Hankinson T, Klimo P, Feldstein N, Anderson R, Brockmeyer D. Chiari malformations, syringohydromyelia and scoliosis. Neurosurg Clin N Am. 2007;18(3):549–68.
Timpone V, Patel S. MRI of a syrinx: is contrast material always necessary? Am J Roentgenol. 2015;204(5):1082–5.
Anderson N, Willoughby E, Wrightson P. The natural history and the influence of surgical treatment in syringomyelia. Acta Neurol Scand. 1985;71:472–9.
Tsitouras V, Sgouros S. Syringomyelia and tethered cord in children. Childs Nerv Syst. 2013;29(9):1625–34.
Logue V, Edwards M. Syringomyelia and its surgical treatment – an analysis of 75 patients. J Neurol Neurosurg Psychiatry. 1981;44(4):273–84.
Goel A, Desai K. Surgery for syringomyelia: an analysis based on 163 surgical cases. Acta Neurochir. 2000;142(3):293–302.
Elster A, Chen M. Chiari I malformations: clinical and radiologic reappraisal. Radiology. 1992;183(2):347–53.
Caird J, Flynn P, McConnell R. Significant clinical and radiological resolution of a spinal cord syrinx following the release of a tethered cord in a patient with an anatomically normal conus medullaris. J Neurosurg Pediatr. 2008;1(5):396–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kassem, M.W., Tubbs, R.S. (2019). Associations of the Occult Spinal Dysraphisms. In: Tubbs, R., Oskouian, R., Blount, J., Oakes, W. (eds) Occult Spinal Dysraphism. Springer, Cham. https://doi.org/10.1007/978-3-030-10994-3_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-10994-3_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-10993-6
Online ISBN: 978-3-030-10994-3
eBook Packages: MedicineMedicine (R0)