Abstract
Background
Pancreatic ductal adenocarcinomas (PDACs) are sometimes diagnosed accompanied by rapidly impaired diabetes (PDAC-RID). Although this type of PDAC may have unusual biological features, these features have not been explained.
Methods
Patients with PDAC who underwent upfront pancreatectomy between 2010 and 2018 were retrospectively reviewed. PDAC-RID was defined as a glycated hemoglobin (HbA1c) value of ≥ 8.0% of newly diagnosed diabetes, and acute exacerbation of previously diagnosed diabetes. Other patients were classified as PDAC with stable glycometabolism (PDAC-SG). Clinicopathological factors, long-term survival rates, and recurrence patterns were evaluated.
Results
Of the 520 enrolled patients, 104 were classified as PDAC-RID and 416 as PDAC-SG. There was no significant difference regarding TNM staging, resectability, or adjuvant chemotherapy rate between the groups. However, 5-years cancer-specific survival (CSS) was significantly higher in the PDAC-RID group than in the PDAC-SG group (45.3% vs. 31.1%; p = 0.02). This survival difference was highlighted in relatively early-stage PDAC (≤ pT2N1) (CSS: 60.8% vs. 43.6%; p = 0.01), but the difference was not significant for advanced-stage PDAC. A multivariate analysis of early-stage PDAC showed that PDAC-SG was an independent risk factor of shorter CSS (hazard ratio 1.76; p = 0.02). The hematogenous metastatic rate in early-stage PDAC was lower in the PDAC-RID group than in the PDAC-SG group (18.3% vs. 35.8%; p = 0.01).
Conclusions
PDAC-RID showed a favorable long-term survival rate after curative resection with low hematogenous metastases, which may be due to its unique biology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pancreatic ductal adenocarcinoma (PDAC) is one of the most highly malignant diseases and the fourth leading cause of cancer-related deaths.1 The majority (80–85%) of patients with PDAC present with locally advanced or distant metastatic disease, and only a minority (15–20%) of patients are eligible for surgical resection.2,3 While the development of multidisciplinary treatment has improved the prognosis of PDAC, stratifying patients with PDAC according to tumor biology is important to select an optimal treatment option.4,5
Diabetes is widely known as a risk factor for developing PDAC. Previous studies have shown that the presence of diabetes corresponds with a two- to eightfold increased risk for PDAC.6,7,8 In contrast, it is also known that the development of PDAC itself brings about impaired glycemic control.8,9 This is caused not only by the destruction of the pancreas parenchyma due to malignant infiltration but also by a paraneoplastic phenomenon involving the release of peculiar molecules from the tumor itself.10,11,12 Thus, PDAC accompanied by rapidly impaired diabetes may have a distinct biology and could be a new biological marker to stratify patients preoperatively.
Hence, this study aimed to evaluate the long-term surgical outcome of PDAC accompanied by rapidly impaired diabetes (PDAC-RID), and to reveal its unique biology.
Methods
Selection of Patients
We performed a retrospective cohort study that was approved by the Institutional Review Board of The Cancer Institute Hospital of Japanese Foundation for Cancer Research (approval number: 2020-GA-1092). The clinical data of 637 patients with histologically proven PDAC who underwent curative-intent pancreatectomy between January 2010 and December 2018 were retrieved from a prospectively maintained database. To minimize the effect of hyperbilirubinemia, carbohydrate antigen (CA) 19-9 levels were re-evaluated before treatment after obtaining stable biliary drainage, i.e., serum total bilirubin concentration < 3.0 mg/dL, although data for the re-evaluation of CA19-9 were missing for 6.7% of patients. Of these patients, those who underwent preoperative chemotherapy were excluded because chemotherapy, including steroid administration, could have altered the glycometabolic state or cancer biology.
Definition of Diabetes
A diagnosis of diabetes was based on an elevated glycated hemoglobin (HbA1c) value ≥ 6.5%, fasting plasma glucose concentrations ≥ 126 mg/dL, random plasma glucose concentrations ≥ 200 mg/dL, and/or whether the patients had already received medication or dietary therapy for diabetes.13 Diabetes history was investigated by a medical chart review, and changes in HbA1c values were examined. In the case of newly diagnosed diabetes, it was confirmed that diabetes had not been indicated from the results of previous medical examinations (meaning that the HbA1c value was < 6.5%). PDAC-RID was defined as (1) an HbA1c value ≥ 8.0% of that with newly diagnosed diabetes at the detection of PDAC; and (2) acute exacerbation of previously diagnosed diabetes, which corresponded to ≥ 2.0% elevation in HbA1c levels from baseline and/or new initiation or addition of an oral antidiabetic or insulin when PDAC was detected. Other patients were defined as having PDAC with stable glycometabolism (PDAC-SG). These included patients with an HbA1c value < 8.0% of that with newly diagnosed diabetes at the detection of PDAC, those who had previously diagnosed and controlled diabetes, or those who did not have diabetes.
Treatment Strategy of the Cancer Institute Hospital
Preoperative assessment of tumor resectability was conducted in multidisciplinary team conferences using dynamic computed tomography (CT) and/or magnetic resonance imaging as routine work-ups. Resectability was then classified into resectable, borderline resectable, and unresectable according to the National Comprehensive Cancer Network guideline.14 Before 2015, upfront surgery was applied for patients with resectable PDAC and those with borderline resectable PDAC. After 2015, we started neoadjuvant gemcitabine/nab-paclitaxel therapy for patients with borderline resectable PDAC.15
Preoperative insulin treatment was performed for patients with poor glycemic control (high HbA1c value and/or fasting plasma glucose concentration). Postoperative glycemic control was performed for all patients. The hyperglycemia was treated to maintain glucose concentrations < 180–200 mg/dL perioperatively.16
All surgical procedures were selected according to the tumor location and extent, as described previously.15,17,18 Pancreaticoduodenectomy was performed for the pancreatic head and body PDAC, and distal pancreatectomy was selected for the pancreatic body or tail PDAC. Total pancreatectomy was performed for multiple PDACs or diffuse-extended-type PDAC. Regional lymph node dissection was performed in each procedure. The dissected region of the nerve plexus around the superior mesenteric artery, common hepatic artery, and celiac artery was determined depending on the extent of the tumor to achieve R0 resection.17,19 Distal pancreatectomy with celiac axis resection was performed for pancreatic body cancer invading the celiac axis.18 Combined resection of the portal vein or superior mesenteric vein was conducted if the tumor was close to the veins.20 After curative surgery, adjuvant gemcitabine or S-1 chemotherapy was administered routinely for 6 months.
Pathological Examination
The pathological diagnosis was determined by experts in pancreatic tumor pathology. Pathological data, including differentiation of the tumor, tumor diameter, microscopic lymphatic invasion, vascular invasion, and neural invasion, were collected. With regard to surgical curability, R0 resection was defined as an histologically negative margin, while R1 resection was defined as a positive margin (0 mm rule). The number of resected lymph nodes and metastases were also evaluated. The Eighth Edition of the Union for International Cancer Control Staging was used for determining the TNM stage.21
Postoperative Follow-Up
The patients were followed up every 3 months with laboratory tests and abdominal CT to investigate locoregional or systemic recurrence. Magnetic resonance imaging or positron emission tomography was performed if CT showed lesions suspected of metastasis.
Endpoints
The postoperative short-term outcome was evaluated by the operative time, intraoperative blood loss, postoperative complications, and postoperative hospital stay. Postoperative complications included postoperative pancreatic fistula and delayed gastric emptying.22,23 Surgical complications were evaluated according to the Clavien–Dindo classification.24
The postoperative long-term outcome was evaluated by cancer-specific survival (CSS) and recurrence-free survival (RFS). CSS was calculated as the time from the day of surgery to cancer-related death, and the time was censored at the date of the last follow-up assessment for patients who were still alive or who died of other causes. RFS was calculated as the time from the day of surgery to the day of identifying recurrence by an imaging examination or to death, and the time was censored at the date of the last follow-up assessment for patients who were alive without any recurrence. The follow-up period was evaluated for censored cases.
A subgroup analysis according to T and N factors was also performed. The patients were classified into the following two subgroups: T2 or lower and N1 or lower (early stage), and T3 or higher and N2 or higher (advanced stage). CSS was compared between PDAC-RID and PDAC-SG in each subgroup. The initial recurrent site was compared between PDAC-RID and PDAC-SG. Recurrent sites were classified into the following six categories: liver, lungs, local, distant lymph node, peritoneal dissemination, and others. The ‘others’ category included the remnant pancreas, adrenal gland, bone, and other less common locations. The frequency of hematogenous metastasis, such as the liver, lungs, adrenal gland, and bone, was also compared.
Statistical Analysis
Continuous variables are expressed as the median and range, while categorical variables are presented as frequencies with percentages. The Mann–Whitney U test or Chi-square test was performed for comparison between groups. The Kaplan–Meier method was used to estimate the survival rate, and the log-rank test was applied to compare the survival curves of two groups. Variables with a p-value <0.05 were applied to the subsequent multivariate Cox regression analysis. Independent variables were determined using the backward stepwise method. A p-value <0.05 was defined as statistically significant. All statistical analyses were conducted using IBM SPSS Statistics 25.0 software (IBM Japan, Ltd, Tokyo, Japan).
Results
Selection of Patients
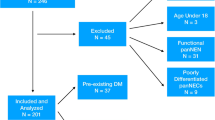
Among the 637 participants, 117 were excluded because of administration of preoperative chemotherapy (Fig. 1). Among all cohorts, no patients received preoperative radiation therapy. The remaining 520 patients were integrated into further analysis. Of these patients, 104 patients were classified into the PDAC-RID group (newly diagnosed diabetes with HbA1c values ≥ 8.0%, n = 40; previously diagnosed diabetes with acute exacerbation, n = 64). Of the newly diagnosed diabetes cases, a diagnosis of diabetes had been ruled out in past medical examinations in most of the patients (HbA1c < 6.5%). The remaining 416 patients were classified into the PDAC-SG group (newly diagnosed diabetes with HbA1c values < 8.0%, n = 29; previously diagnosed diabetes without acute exacerbation, n = 67; and no diabetes, n = 320).
Clinical Background
Preoperative Outcomes
Table 1 shows a comparison of the clinical background between the PDAC-RID and PDAC-SG groups. There was no significant difference in the tumor site, resectability, surgical procedure, or adjuvant chemotherapy induction rate between the groups. The body mass index values of the two groups were comparable. In contrast, the median values of CA19-9 and carcinoembryonic antigen (CEA) were significantly higher in the PDAC-RID group than in the PDAC-SG group (p < 0.01 and p = 0.01, respectively). The median HbA1c value was significantly higher in the PDAC-RID group than in the PDAC-SG group (p < 0.01).
Perioperative Surgical Outcomes
Comparison of perioperative factors in the two groups is shown in Table 1. There was no significant difference in operative time, blood loss, Clavien–Dindo classification (including pancreatic fistula and delayed gastric emptying), or postoperative hospital stay between the PDAC-RID and PDAC-SG groups.
Perioperative Glycemic Control in the Pancreatic Ductal Adenocarcinoma Accompanied by Rapidly Impaired Diabetes (PDAC-RID) Group
In 104 patients in the PDAC-RID group, at the time of detecting PDAC, 49 (47.1%) patients had no medication for hyperglycemia, 50 (48.1%) had been treated by oral hypoglycemic agents, and insulin treatment had already been administered in 5 (4.8%) patients. With regard to preoperative glycemic control, all patients started to take intensive insulin therapy, adding it to the dietary treatment for rapidly impaired glycemic control. A mean of 29.0 (standard deviation [SD] 12.9) units of insulin/day was administered at surgery. At discharge, a mean of 13.2 (SD 8.7) units of insulin/day was administered (p < 0.01 by paired t-test). After discharge, 30 (28.8%) patients terminated any hyperglycemia treatment, 35 (33.7%) converted to oral hypoglycemic agents, and 39 (37.5%) continued insulin therapy. In contrast, among long-standing stable diabetic patients (n = 67), treatment for diabetes remained unchanged in 44 (65.7%) patients, and 14 (20.9%) patients showed worsening of glycemic control and thus intensified the treatment for diabetes. Only 9 (13.4%) patients could downscale treatment. Postoperative metformin treatment was performed in 12 (11.5%) patients.
Pathological Findings
Table 1 also shows the pathological findings in the PDAC-RID and PDAC-SG groups. There was no significant difference in the tumor diameter, differentiation of the tumor, venous invasion, lymphatic invasion, perineural invasion, T factors, N factors, TNM staging, or surgical margin between the two groups.
Long-Term Outcomes
Postoperative long-term survival was evaluated by Kaplan–Meier curves (Fig. 2). With regard to CSS, the median follow-up for censored cases in the PDAC-RID group was 5.10 years, and 5.06 years in the PDAC-SG group. The 5-years CSS rate was 45.3% in the PDAC-RID group and 31.1% in the PDAC-SG group (p = 0.02) (Fig. 2a). The 5-years RFS rate was 35.2% in the PDAC-RID group and 23.8% in the PDAC-SG group (p = 0.04) (Fig. 2b).
Comparison of Kaplan–Meier curves of A CSS and B RFS between patients with PDAC-RID and PDAC-SG. CSS cancer-specific survival, RFS recurrence-free survival, PDAC-RID pancreatic ductal adenocarcinoma accompanied by rapidly impaired diabetes, PDAC-SG pancreatic ductal adenocarcinoma with stable glycometabolism
Subgroup Analyses in Early-Stage (≤ T2N1) and Advanced-Stage (≥T3N2) PDAC
Further analyses were performed to investigate the cause of this favorable prognosis in PDAC-RID. The prognosis between the PDAC-RID and PDAC-SG groups was compared at every T and N stage (electronic supplementary material [ESM] Fig. 1). We found good long-term survival in PDAC-RID in the T1, T2, N0, and N1 subgroups. Therefore, a difference in survival was evident in relatively early-stage PDAC (≤T2N1) but not in advanced-stage PDAC (≥T3N2). In the early-stage subgroup, 60 patients had PDAC-RID, while 218 had PDAC-SG. The 5-years CSS rate for PDAC-RID was 60.8%, which was significantly higher than that for PDAC-SG (43.6%; p = 0.01) [Fig. 3a]. In the advanced-stage subgroup, 44 patients had PDAC-RID, whereas 198 had PDAC-SG. There was no significant difference in the 5-years CSS rate between the two groups (PDAC-RID: 22.0%, and PDAC-SG: 16.8%; p = 0.90) [Fig. 3b].
Subgroup analysis of CSS according to T and N factors. A Kaplan–Meier curves in the T2 or lower and N1 or lower (early stage) subgroup were compared. B Kaplan–Meier curves in the T3 or higher and N2 or higher (advanced stage) subgroup were compared. CSS cancer-specific survival, PDAC-RID pancreatic ductal adenocarcinoma accompanied by rapidly impaired diabetes, PDAC-SG pancreatic ductal adenocarcinoma with stable glycometabolism
Multivariate Cox Regression Analysis
The multivariate Cox regression analysis for CSS in the early-stage subgroup is shown in Table 2. Age ≥70 years (hazard ratio [HR] 1.46; p = 0.04), PDAC-SG (HR 1.76; p = 0.02), a poorly differentiated tumor (HR 1.88; p = 0.01), a positive surgical margin (HR 1.78; p = 0.03), lymph node metastasis (HR 2.28; p < 0.01), and no adjuvant chemotherapy (HR 2.15; p < 0.01) were identified as independent prognostic factors. In contrast, in the advanced-stage subgroup (Table 3), CA19-9 concentrations ≥500 U/mL (HR 1.89, p < 0.01), a poorly differentiated tumor (HR 1.63; p = 0.02), a positive surgical margin (HR 1.55; p = 0.02), lymph node metastasis (HR 2.25; p < 0.01), and no adjuvant chemotherapy (HR 2.53; p < 0.01) were identified as independent prognostic factors.
Recurrence Pattern
The initial recurrent site of the two subgroups in the early and advanced stages is shown in Table 4. During the follow-up, 368 (70.8%) patients had recurrence, of whom 63 (60.6%) patients had PDAC-RID and 305 (73.3%) had PDAC-SG. In the early stage, there was no significant difference in all individual recurrent sites between the PDAC-RID and PDAC-SG groups. However, the hematogenous metastasis rate was significantly lower in the PDAC-RID group than in the PDAC-SG group (p = 0.01). In the advanced stage, the hematogenous metastasis rate appeared to be lower in the PDAC-RID group than in the PDAC-SG group, but this did not reach significance.
Discussion
The intricate and multidirectional relationship between diabetes and PDAC has been known for a long time. This study showed that patients with PDAC-RID had a significantly better long-term survival rate than those with PDAC-SG after upfront curative resection. This interesting finding was particularly noticeable in early-stage cancer (≤T2N1), accompanied by a lower hematogenous metastatic rate in patients with PDAC-RID than in those with PDAC-SG.
One of the features of this study is that we created a new cohort whose rapidly impaired diabetes was associated with the diagnosis of PDAC. The term ‘new-onset diabetes’, which is used for a diagnosis of diabetes within 24 months of detecting PDAC, has often been considered to correspond to this concept.7,8,25,26 However, this classification has several issues. First, patients with long-term diabetes (usually defined as > 2 to 3 years before detecting PDAC) with acute exacerbation should also be included in this concept. Additionally, HbA1c values in patients with PDAC-RID are usually much higher than 6.5%, and thus may only be matched to a subset of the new-onset diabetes cohort. In order to narrow down the cases of rapidly impaired diabetes by PDAC, we limited our criteria to cases of HbA1c ≥ 8.0% among newly diagnosed diabetes cases. This number is the reference value for poor glycemic control worldwide.27 Since the normal value of HbA1c is approximately 5.0–6.0%, the increase in HbA1c value was more than 2.0%. Similarly, of 64 previously diagnosed diabetes patients, changes in HbA1c values in 55 patients were known and were elevated more than 2.0%. Although the HbA1c changes in another 9 patients were unknown, their diabetic treatment was intensified by a local doctor at the time of PDAC diagnosis. This medical history qualified those 9 patients for assignment to PDAC-RID. Additionally, non-diabetic patients and long-standing stable diabetic patients were included in the same category because they were identical in glycometabolism and survival (data not shown). Thus, the new cohort used in this study would be suitable for selecting patients with PDAC whose glycemic control is exacerbated by pancreatic cancer. Additionally, this cohort is easily identified by the serum HbA1c concentration and the patient’s medical history at outpatient care.
The most important finding in this study is that the long-term survival rate after upfront surgery for PDAC-RID was significantly better than for PDAC-SG. Most previous studies showed that diabetes was associated with worse or comparable survival outcomes following the resection of pancreatic cancer.28,29,30,31,32 Although the reason for this discrepant result between studies is unclear, one consideration is that PDAC-RID might have a unique biology among all PDAC patients. In this study, there was no significant difference in well-known prognostic predictors, such as the tumor diameter, lymph node metastasis, anatomical resectability, and induction rate of adjuvant chemotherapy, between PDAC-RID and PDAC-SG. Although CA19-9 concentrations in patients with PDAC-RID were higher than those in patients with PDAC-SG, this tumor marker increases as glycemic control worsens.33 Therefore, CA19-9 concentrations in PDAC with diabetes can be unreliable. CEA concentrations in patients with PDAC-RID were higher than those in patients with PDAC-SG, but the median value in both cohorts was within normal limits. Therefore, this prognostic difference between PDAC-RID and PDAC-SG was apparent, regardless of the tumor conditions. Additionally, the number of cases of pancreatic head and tail cancer between PDAC-RID and PDAC-SG was similar (head, 62 (60.6%) and 262 (63.0%); tail, 11 (10.6%) and 43 (10.3%), respectively), and the rate of a dilated main pancreatic duct (≥ 5 mm) in pancreatic head cancer between these groups was also similar [35 (37.2%) and 131 (34.3%)], which indicated that PDAC-RID was not always due to pancreatic parenchymal dysfunction, and also from the tumor itself.
In this study, a better postoperative prognosis of PDAC-RID was highlighted in the early-stage subgroup, but was less noticeable in the advanced-stage group. This finding suggested that PDAC-RID had a unique cancer biology. Once a tumor has grown to the advanced stage, it acquires a more heterogenous cancer biology, as indicated by an accumulating tumor mutation burden.34,35 Therefore, the prognostic effect of this unique cancer biology may diminish as the tumor progresses. In the early stage, the hematogenous metastasis rate was significantly lower in the PDAC-RID group than in the PDAC-SG group, which might have directly affected the difference in long-term survival rate. Notably, we have reported the optimal pancreatectomy procedure to enhance the local control, which might contribute to the favorable outcome of this unique PDAC.17,20 We subdivided microscopic venous invasion into the following four subclassifications: v0, no evidence of venous invasion; v1, slight venous invasion; v2, moderate venous invasion; and v3, marked venous invasion.36 We found that PDAC-RID tended to have a lower venous invasiveness in the early-stage subgroup (ESM Fig. 2). Therefore, PDAC-RID may be associated with the low frequency of venous invasion. Indeed, these considerations need to be validated in a larger-scale clinical setting. Additionally, molecular biological analyses would clarify the detailed mechanism of the characteristics of PDAC-RID.
The main treatment option for PDAC has changed from surgery only to a combination of surgery and cytotoxic chemotherapies because of recent remarkable developments in medical therapy.5,37 The optimal selection of patients for various treatment options is an important issue. In this study, PDAC-RID in the early stage showed a more favorable long-term survival rate after curative upfront surgery than PDAC-SG. In contrast, previous studies have shown that patients with diabetes are associated with a lower response rate, lower completion rate, and higher rate of death after chemotherapy.38,39,40 Therefore, especially in early-stage PDAC-RID, the indication for neoadjuvant chemotherapy should be carefully considered.
This study has several limitations. First, some patients had incomplete information in their clinical data and diabetes history because of the retrospective design. Therefore, accurate previous HbA1c values cannot be determined for the entire cohort, which might have affected the patient flowchart in this study. Although preoperative biliary interventions were performed for jaundice patients, not all cases of preoperative total bilirubin came within normal range. Thus, the CA19-9 values in jaundice patients might be affected by high total bilirubin values. Second, patients who underwent preoperative chemotherapy were excluded from this study, although this was intentional. Therefore, the association between impaired glycometabolism and the chemotherapeutic effect remains unknown. Third, the mechanism of a better prognosis by upfront resection in patients with PDAC-RID was not able to be fully determined. Fundamental research needs to be performed to discover relevant biomarkers representative of PDAC, which rapidly impairs the glycometabolic state, in the future.
Conclusion
PDAC accompanied by rapidly impaired diabetes shows a favorable postoperative long-term survival rate by upfront curative pancreatectomy, which is especially noticeable in the early stage. This type of pancreatic cancer is easy to discriminate in the clinical setting and may have a unique biology.
REFERENCES
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N England J Med. 2014;371(11):1039–49.
Park W, Chawla A, O’Reilly EM. Pancreatic cancer: a review. JAMA. 2021;326(9):851–62.
Mokdad AA, Minter RM, Zhu H, Augustine MM, Porembka MR, Wang SC, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: a propensity score matched analysis. J Clin Oncol. 2017;35(5):515–22.
Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388(10041):248–57.
Sah RP, Nagpal SJ, Mukhopadhyay D, Chari ST. New insights into pancreatic cancer-induced paraneoplastic diabetes. Nat Rev Gastroenterol Hepatol. 2013;10(7):423–33.
Singhi AD, Koay EJ, Chari ST, Maitra A. Early detection of pancreatic cancer: opportunities and challenges. Gastroenterology. 2019;156(7):2024–40.
Roy A, Sahoo J, Kamalanathan S, Naik D, Mohan P, Kalayarasan R. Diabetes and pancreatic cancer: exploring the two-way traffic. World J Gastroenterol. 2021;27(30):4939–62.
Hart PA, Bellin MD, Andersen DK, Bradley D, Cruz-Monserrate Z, Forsmark CE, et al. Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. Lancet Gastroenterol Hepatol. 2016;1(3):226–37.
Pannala R, Leirness JB, Bamlet WR, Basu A, Petersen GM, Chari ST. Prevalence and clinical profile of pancreatic cancer-associated diabetes mellitus. Gastroenterology. 2008;134(4):981–7.
Aggarwal G, Ramachandran V, Javeed N, Arumugam T, Dutta S, Klee GG, et al. Adrenomedullin is up-regulated in patients with pancreatic cancer and causes insulin resistance in β cells and mice. Gastroenterology. 2012;143(6):1510-7.e1.
Kiritani S, Ono Y, Takamatsu M, Oba A, Sato T, Ito H, et al. Diabetogenic liver metastasis from pancreatic cancer: a case report. Surg Case Rep. 2022;8(1):224.
Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes care. 2022;45 Suppl 1:S17–s38.
Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, et al. Pancreatic adenocarcinoma, Version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Comprehens Cancer Netw. 2017;15(8):1028–61.
Inoue Y, Saiura A, Oba A, Kawakatsu S, Ono Y, Sato T, et al. Optimal extent of superior mesenteric artery dissection during pancreaticoduodenectomy for pancreatic cancer: balancing surgical and oncological safety. J Gastrointestin Surg. 2019;23(7):1373–83.
14. Diabetes Care in the Hospital: Standards of Medical Care in Diabetes-2018. Diabetes care. 2018;41 Suppl 1:S144-s51.
Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, et al. Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. 2015;262(6):1092–101.
Sato T, Inoue Y, Takahashi Y, Mise Y, Ishizawa T, Tanakura K, et al. Distal pancreatectomy with celiac axis resection combined with reconstruction of the left gastric artery. J Gastrointestin Surg. 2017;21(5):910–7.
Inoue Y, Saiura A, Takahashi Y. A novel classification and staged approach for dissection along the celiac and hepatic artery during pancreaticoduodenectomy. World J Surg. 2018;42(9):2963–7.
Oba A, Ito H, Ono Y, Sato T, Mise Y, Inoue Y, et al. Regional pancreatoduodenectomy versus standard pancreatoduodenectomy with portal vein resection for pancreatic ductal adenocarcinoma with portal vein invasion. BJS Open. 2020;4(3):438–48.
Brierley JD, Gospodarowicz MK, Wittekind C. International union against cancer (UICC). TNM classification of malignant tumors. 8th edition. Chichester: Wiley-Blackwell; 2017.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161(3):584–91.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Chari ST, Leibson CL, Rabe KG, Timmons LJ, Ransom J, de Andrade M, et al. Pancreatic cancer-associated diabetes mellitus: prevalence and temporal association with diagnosis of cancer. Gastroenterology. 2008;134(1):95–101.
Yuan C, Babic A, Khalaf N, Nowak JA, Brais LK, Rubinson DA, et al. Diabetes, weight change, and pancreatic cancer risk. JAMA Oncol. 2020;6(10):e202948.
Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese clinical practice guideline for diabetes 2019. J Diab Investig. 2020;11(4):1020–76.
Lv X, Qiao W, Leng Y, Wu L, Zhou Y. Impact of diabetes mellitus on clinical outcomes of pancreatic cancer after surgical resection: a systematic review and meta-analysis. PloS One. 2017;12(2):e0171370.
Chu CK, Mazo AE, Goodman M, Egnatashvili V, Sarmiento JM, Staley CA, et al. Preoperative diabetes mellitus and long-term survival after resection of pancreatic adenocarcinoma. Ann Surg Oncol. 2010;17(2):502–13.
Dandona M, Linehan D, Hawkins W, Strasberg S, Gao F, Wang-Gillam A. Influence of obesity and other risk factors on survival outcomes in patients undergoing pancreaticoduodenectomy for pancreatic cancer. Pancreas. 2011;40(6):931–7.
Balzano G, Dugnani E, Gandolfi A, Scavini M, Pasquale V, Aleotti F, et al. Effect of diabetes on survival after resection of pancreatic adenocarcinoma: a prospective, observational study. PloS One. 2016;11(11):e0166008.
Walter U, Kohlert T, Rahbari NN, Weitz J, Welsch T. Impact of preoperative diabetes on long-term survival after curative resection of pancreatic adenocarcinoma: a systematic review and meta-analysis. Ann Surg Oncol. 2014;21(4):1082–9.
Benhamou PY, Vuillez JP, Halimi S, Meffre G, Bachelot I. Influence of metabolic disturbances of diabetes mellitus on serum CA 19–9 tumor marker. Diabete Metab. 1991;17(1):39–43.
Evan T, Wang VM, Behrens A. The roles of intratumour heterogeneity in the biology and treatment of pancreatic ductal adenocarcinoma. Oncogene. 2022;41(42):4686–95.
Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9(1):34.
Japan Pancreas Society. General Rules for the Study of Pancreatic Cancer, 7th edition revised and enlarged version. Kanehara & Co., Ltd; 2020.
Murphy JE, Wo JY, Ryan DP, Jiang W, Yeap BY, Drapek LC, et al. Total neoadjuvant therapy with FOLFIRINOX followed by individualized chemoradiotherapy for borderline resectable pancreatic adenocarcinoma: a phase 2 clinical trial. JAMA Oncol. 2018;4(7):963–9.
Hank T, Sandini M, Qadan M, Weniger M, Ciprani D, Li A, et al. Diabetes mellitus is associated with unfavorable pathologic features, increased postoperative mortality, and worse long-term survival in resected pancreatic cancer. Pancreatology. 2020;20(1):125–31.
Ma J, Wang J, Ge L, Long B, Zhang J. The impact of diabetes mellitus on clinical outcomes following chemotherapy for the patients with pancreatic cancer: a meta-analysis. Acta Diabetol. 2019;56(10):1103–11.
Rajamanickam ES, Christians KK, Aldakkak M, Krepline AN, Ritch PS, George B, et al. Poor glycemic control is associated with failure to complete neoadjuvant therapy and surgery in patients with localized pancreatic cancer. J Gastrointestin Surg. 2017;21(3):496–505.
Acknowledgment
This research was supported by a Grant-in-Aid for Research from the National Center for Global Health and Medicine (19A2013). The authors thank Ellen Knapp, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
Sho Kiritani, Yoshihiro Ono, Manabu Takamatsu, Sachiyo Yoshio, Mamiko Miyashita, Atsushi Oba, Takafumi Sato, Hiromichi Ito, Yosuke Inoue, Akio Saiura, and Yu Takahashi have no conflicts of interest associated with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2023_14408_MOESM1_ESM.tif
Supplementary fig.1 1 Subgroup analysis of CSS according to T and N factors. (a–c) Kaplan–Meier curves based on the T factor. (d–f) Kaplan–Meier curves based on the N factor. CSS cancer-specific survival, PDAC-RID pancreatic ductal adenocarcinoma accompanied by rapidly impaired diabetes, PDAC-SG pancreatic ductal adenocarcinoma with stable glycometabolism (TIF 87 KB)
10434_2023_14408_MOESM7_ESM.tif
Supplementary fig. 2 Distribution of subdivided venous invasion between PDAC-RID and PDAC-SG. PDAC-RID pancreatic ductal adenocarcinoma accompanied by rapidly impaired diabetes, PDAC-SG pancreatic ductal adenocarcinoma with stable glycometabolism, v0 no evidence of venous invasion, v1 slight venous invasion, v2 moderate venous invasion, v3 marked venous invasion (TIF 91 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kiritani, S., Ono, Y., Takamatsu, M. et al. Unique Biology of Pancreatic Ductal Adenocarcinoma Accompanied by Rapidly Impaired Diabetes: A Favorable Long-Term Survival Following Curative Resection. Ann Surg Oncol 31, 514–524 (2024). https://doi.org/10.1245/s10434-023-14408-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14408-0