Abstract
Aims
A meta-analysis was performed to evaluate the prognostic impact of diabetes on the clinical outcome for patients with pancreatic cancer following the adjuvant chemotherapy.
Methods
To identify all researches and studies relevant to the prognostic impact of diabetes on the clinical outcome for patients with pancreatic cancer following the adjuvant chemotherapy, a comprehensive literature search was performed until January 30, 2018, by searching PubMed, EMBASE, and the Cochrane Library. The relevant data were extracted from included studies by two reviewers independently. HR and its 95% confidence interval (CI) were synthesized using STATA 12.0 software.
Results
All of six studies consisting of 4241 pancreatic cancer patients (1034 patients with DM and 3207 patients without DM) were eligible and included in this meta-analysis. The result of meta-analysis under a fixed model showed that there are significant differences in overall survival (HR 1.16, 95% CI 1.08–1.25, P = 0.000) and T stage (OR 1.30, 95% CI 1.08–2.17, P = 0.005) between PC patients with DM following chemotherapy and PC patients without DM following chemotherapy. There was no significant difference in gender (OR 1.23, 95% CI 1.00–1.50, P = 0.051), tumor locations (OR 1.13, 95% CI 0.81–1.56, P = 0.476), cancer extent (OR 0.85, 95% CI 0.48–1.50, P = 0.569), N stage (OR 1.01, 95% CI 0.58–1.74, P = 0.973), and M stage (OR 0.64, 95% CI 0.21–1.99, P = 0.441) between diabetic PC patients and non-diabetic patients.
Conclusions
Diabetes mellitus patients who undergo chemotherapy for pancreatic cancer present with a reduced survival and lager tumor. Pancreatic cancer patients with DM also have a higher risk of death after chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Pancreatic cancer (PC), ranking fourth leading cause of death among all cancers [1], is predicted to be the second leading cause by 2030. At the time of diagnosis, most patients were diagnosed at an advanced stage with locally advanced unresectable or distant metastasis tumors [2]. Advances in adjuvant chemotherapy have improved survival outcome for patients with PC after radical resection [3]. However, the prognosis for patients with PC is poor. Only 10–20% of patients are eligible for curative surgery and its 5-year survival rate is less than 5%.
Diabetes mellitus (DM) is reported as a risk factor for a number of cancers and associated with development of PC, but its impact on prognosis of patients is still unclear [4, 5]. Recently, many researches and studies have reported that there is a complex relationship between pancreatic cancer and diabetes [6]. Both DM and pancreatic cancer share common risk factors such as insulin resistance, obesity, and genetic factors [7]. DM has been known as both cause and consequences of pancreatic cancer [8]. Use of anti-diabetes medications is also known to be an independent risk factor and one of complications for pancreatic cancer [9]. Compared with normoglycemic patients across all types of cancer, the survival of diabetic individuals with cancer seems to be less (RR 1.4) [10]. However, with the limitation of cohort size and large number of variables, analysis on survival outcomes for pancreatic cancer patients with DM is difficult. In the study from Chu et al. [11], 93 patients (45.4%, 93/209) with preoperative diabetes and pancreatic cancer had a median survival of 15 months, which was less than non-diabetic patients (17 months, HR 1.55).
Thus, the prognostic effect of DM in pancreatic cancer patients following chemotherapy is uncertain. Therefore, we conducted a meta-analysis to evaluate the prognostic impact of diabetes on the clinical outcome for patients with pancreatic cancer following the adjuvant chemotherapy.
Materials and methods
Literature search
To identify all researches and studies relevant to the prognostic impact of diabetes on the clinical outcome for patients with pancreatic cancer following the adjuvant chemotherapy, a comprehensive literature search was performed until January 30, 2018, by searching PubMed, EMBASE, and the Cochrane Library. The search terms were as follows: “Pancreatic Neoplasm” OR “Pancreas Neoplasms” OR “Pancreas Neoplasm” OR “Pancreas Cancers” OR “Pancreas Cancer” OR “Pancreatic Cancer” OR “Pancreatic Cancers” OR “Pancreatic Ductal Carcinomas” OR PC OR PADC, “Diabetes Mellitus” OR “DM” OR “type 2 diabetes” OR “NIDDM” OR “T2DM” OR “IDDM” OR “type 1 diabetes” OR “T1DM” OR “type 3 diabetes” OR “T3DM.” The language in this research was limited to English.
Selection criteria
Eligible studies for this meta-analysis met the following criteria: (1) patients with pancreatic cancer were diagnosed by pathological or histological examination and were treated with chemotherapy; DM disease status was defined as: patients with diabetic history, ongoing treatment with anti-diabetic medication(s) or qualification as DM during the follow-up period; (2) patients with pancreatic cancer were treated with chemotherapy. The regimens of chemotherapy and anti-diabetes medications were not limited; (3) publications reported survival outcomes; (4) sufficient data to estimate the hazard ratio (HR) and its 95% confidence interval (95% CI); (5) publication as a full research article in English.
The exclusion criteria were as follows: (1) case reports, review articles, abstracts, letters, editorials, and meta-analyses; (2) articles without sufficient data to analyze after contacting the authors of the study; (3) duplicate publications.
Data extraction
The relevant data were extracted from included studies by two reviewers independently. If any disagreement appeared, the discussion was necessary for them. Following items were included in data retrieved from each eligible study: (1) basic characteristics of each study, such as authors, year of publication, journal, country, sample size, gender, treatments, duration of follow-up; (2) clinical outcomes: tumor location, cancer extent, T stage, N stage, M stage, and overall survival.
Quality assessment
Two reviewers assessed the quality of retrieved studies by independently reading the full articles according to the Newcastle–Ottawa scale (NOS), which was included: (1) the selection of cohorts (0–4 points); (2) comparability of cohorts (0–2 points); (3) the exposure or outcome of the participant (0–3 points). Finally, the total score of each study represented the overall result of quality assessment. Studies with 7–9 points were regarded as “high quality.”
Data analysis
The primary outcome for this meta-analysis was overall survival for the pancreatic cancer patients with DM following chemotherapy, compared with no-DM patients. The second outcomes were tumor location, cancer extent, TNM stage. Heterogeneity was evaluated with a I2-based Q test: if the P value was higher than 0.1 or I2 was lower than 50%, it demonstrated that all included studies were lacking heterogeneity, and the Mantel–Haenszel method (fixed effect model) was used to merge the studies. Otherwise, the random effect model was adopted. HR and its 95% confidence interval were synthesized using STATA 12.0 software. Subgroup analyses and sensitivity analysis were performed if there is heterogeneity between studies. Potential publication bias was diagnosed and measured by Funnel plots. All P values were two-sided, and statistical significance was accepted as P ≤ 0.05.
Results
Characteristics of included studies
Of 133 articles were screed for eligibility, six studies [12,13,14,15,16,17] consisting of 4241 pancreatic cancer patients (1034 patients with DM and 3207 patients without DM) were eligible and included in this meta-analysis. Detailed information about the flowchart of the study selection process is reported in Fig. 1.
Patients’ characteristics and baseline were presented to indentify patients’ characteristics associated with diabetes (Table 1). All of studies are case–control studies. The median age of included patients was more than 55 years. Pancreatic cancer status was advanced or locally advanced, and few of them accepted the surgery treatment. Gemcitabine-based regimens were used more for chemotherapy of pancreatic cancer in included studies. Type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) patients are both included in this meta-analysis. More DM patients were treated with insulin and metformin. The details of treatment of eligible studies were showed in Table 2. Each of six included trails had a calculated NOS score of 8, suggestive of high methodological quality.
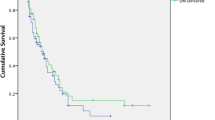
Overall survival for pancreatic cancer patients with DM following chemotherapy
All of included studies reported the HR and its 95% CI for overall survival. Inter-study heterogeneity was not observed by Q test (I2 = 22.0%, P = 0.268). The result of meta-analysis under a fixed model showed that there is a significant difference in overall survival (HR 1.16, 95% CI 1.08–1.25, P = 0.000) between PC patients with DM following chemotherapy and PC patients without DM following chemotherapy (Fig. 2).
Clinical outcomes for pancreatic cancer patients with DM following chemotherapy
Meta-analysis was performed to evaluate whether the DM status effects the clinical outcomes, such as gender, tumor location, cancer extent, and TNM stage.
There was no significant difference in gender (OR 1.23, 95% CI 1.00–1.50, P = 0.051) between diabetic PC patients and non-diabetic patients, which shows no inter-study heterogeneity (I2 = 45.8%, P = 0.117) (Fig. 3).
Four of included studies reported the details of tumor locations (pancreas head, body, and tail), and heterogeneity test showed no statistical difference (I2 = 0.0%, P = 0.611). The result of meta-analysis showed that there is no significant difference between diabetic patients and non-diabetic ones (OR 1.13, 95% CI 0.81–1.56, P = 0.476) (Fig. 4).
Cancer extent is also a risk factor for survival. Pancreatic cancer extents for patients included in this meta-analysis were metastatic pancreatic cancer (MPC) and locally advanced pancreatic cancer (LAPC). The result of meta-analysis showed that there is no significant difference between diabetic and non-diabetic patients (OR 0.85, 95% CI 0.48–1.50, P = 0.569) with significant heterogeneity (I2 = 58.0%, P = 0.067) (Fig. 5).
Compared with non-diabetic patients, significant effect of T stage was seen for PC patients with diabetes mellitus (OR 1.30, 95% CI 1.08-2.17, P = 0.005), but there was no significant difference in T1 stage (OR 0.97, 95% CI 0.28–3.35, P = 0.957), T2 stage (OR 1.21, 95% CI 0.90–1.63, P = 0.201), T3 stage (OR 1.21, 95% CI 0.67–2.17, P = 0.535), and T4 stage (OR 1.44, 95% CI 0.71–2.93, P = 0.309) (Fig. 6). No significant difference was also seen in N stage (OR 1.01, 95% CI 0.58–1.74, P = 0.973) and M stage (OR 0.64, 95% CI 0.21–1.99, P = 0.441).
Discussion
Pancreatic cancer is currently regarded as the fourth most common cause of cancer-related mortality in developed countries. Surgery, chemotherapy, chemoradiotherapy, radiotherapy, and new target therapeutic against growth factor, gene therapy, inhibitors of cell signaling pathway, and immunotherapy are contemporary treatment strategies for patients with pancreatic cancer [18]. However, unfortunately, a large number of patients initially present in advance or metastatic stage. The mainstay of surgical treatments of pancreatic cancer is pancreaticoduodenectomy, distal pancreatectomy, and total pancreatectomy. DM is not only a risk factor but also a complication of pancreatic cancer. Previous studies have suggested that pancreatic cancer also can increase the insulin resistance. New-onset DM was found as a novel marker for patients with pancreatic cancer [19]. BMI more than 30 and medical history of DM were associated with significantly reduced overall survival for pancreatic cancer patients.
American Diabetes Association defined pancreatogenic or pancreatogenous diabetes mellitus as type 3c diabetes, which was caused by the diseases of the exocrine pancreas [20]. Insulin resistance and inadequate pancreatic β-cell function were considered as two major causative factors [21]. Many experimental data have proven various mechanisms of DM as a risk factor for patients with pancreatic cancer. Post-insulin receptor defect was associated with pancreatic cancer, which can impair the synthesis and storage of glycogen [6]. It was also proven that insulin resistance and hyperinsulinemia were caused by higher level of plasma glucagon, the polymorphism of − 23α(A/T), and islet amyloid polypeptide [22]. K-ras codon 12 mutations and HK2 R844K GA/AA genotype have increased the risk of DM for patients with pancreatic cancer [23]. There even exists numerous potential molecular biomarker determining PC-related DM. PC patients usually have a worse survival in the condition of increasing IGF-1(Rs) and 14-amino-acid peptide, which help to predicts poor survival rate and determine the diabetes [24].
The present meta-analysis shows that pancreatic cancer patients with diabetes mellitus have a worse overall survival with a HR of 1.16 compared with non-diabetic patients following chemotherapy. There is a significant effect of T stage for diabetic patients but not for non-diabetic ones. In the result of our meta-analysis, there was no significant difference in gender but with the P value of 0.051, which indicates that male diabetes patients may have a higher risk of pancreatic cancer. According to epidemiological data, the incidence rate of pancreatic cancer among men in 2012 was 4.9 per 100,000 and among women 3.6 per 100,000 [25]. It indicates a trend that the risk of developing pancreatic cancer in male was higher than female.
A recent meta-analysis and systematic review were performed to study the impact of diabetes mellitus on clinical outcomes of pancreatic cancer after surgical resection, the results of which showed that new-onset DM confers a negative impact on survival of pancreatic cancer in patients undergoing surgical resection (RR 1.54, 95% CI 1.24–1.91, P < 0.001) [26]. Interestingly, the association of elevated risk of PC and DM was evaluated by another meta-analysis, the result of which indicated that new-onset T2DM is probably a manifestation of pancreatic cancer, whereas long-term T2D is likely a risk factor for this cancer [27]. Another study involving 16,181 patients showed that patients with DM had worse survival (HR 1.19, 95% CI 1.07–1.32), and tumor stage is an independent risk factor for pancreatic cancer (HR 1.42, 95% CI 1.16–1.73) [28]. Studies also suggested that reduced overall survival for patients with pancreatic cancer was significantly associated with BMI more than 30, advanced disease stage, tumor site (pancreatic body and tail), large tumor size, history of DM, and elevated level of CA199 [29]. DM also was associated with increase mortality of pancreatic cancer patients. Patients with a history of DM before diagnosis of pancreatic cancer have a 1.2 months shorter overall survival and 11 months shorter overall survival after undergoing surgical treatment [30].
The limitations of our meta-analysis should be emphasized as follows: (1) although the heterogeneity was evaluated in our meta-analysis, it is remarkable in the chemotherapy regimens, sample size, and history of previous treatments of the patients; (2) even a comprehensive and systematic literature search was performed, all of studies included in our meta-analysis are case–control studies, which may lead to a high study bias;(3) among the included studies, pancreatic cancer status were advanced or locally advanced, and few of patients accepted the surgery treatment, which could have impacted on our results. We hope that future randomized controlled studies may resolve this problem and provide us with much more high-quality clinical evidence.
In conclusion, diabetes mellitus patients who undergo chemotherapy for pancreatic cancer present with a reduced survival and lager tumor size. Pancreatic cancer patients with DM also have a higher risk of death after chemotherapy. Further studies should focus on the biological mechanisms behind these observations, which may offer new opportunities for diagnosis and therapy about pancreatic cancer and diabetes mellitus.
References
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clinic 67(1):8–29
Hidalgo M, Cascinu S, Kleeff J et al (2015) Addressing the challenges of pancreatic cancer: future directions for improving outcomes. Pancreatology 15(1):8–18
Oettle H, Post S, Neuhaus P et al (2007) Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 297(3):267–277
Everhart J, Wright D (1995) Diabetes mellitus as a risk factor for pancreatic cancer: a meta-analysis. JAMA 273(20):1605–1609
Pannala R, Leirness JB, Bamlet WR et al (2008) Prevalence and clinical profile of pancreatic cancer-associated diabetes mellitus. Gastroenterology 134(4):981–987
Li J, Cao G, Ma Q et al (2012) The bidirectional interation between pancreatic cancer and diabetes. World J Surg Oncol 10(1):171
Hart PA, Chari ST (2013) Diabetes mellitus and pancreatic cancer: why the association matters? Pancreas 42(8):1207–1209
Wang F, Gupta S, Holly EA (2006) Diabetes mellitus and pancreatic cancer in a population-based case–control study in the San Francisco Bay Area, California. Cancer Epidemiol Biomark Prev 14(15):1458–1463
Amin S, Mhango G, Lin J et al (2016) Metformin improves survival in patients with pancreatic ductal adenocarcinoma and pre-existing diabetes: a propensity score analysis. Am J Gastroenterol 111(9):1350–1357
Barone BB, Yeh HC, Snyder CF et al (2008) Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA 300(23):2754–2764
Chu CK, Mazo AE, Goodman M et al (2010) Preoperative diabetes mellitus and long-term survival after resection of pancreatic adenocarcinoma. Ann Surg Oncol 17(2):502–513
Kleeff J, Costello E, Jackson R et al (2016) The impact of diabetes mellitus on survival following resection and adjuvant chemotherapy for pancreatic cancer. Br J Cancer 115(7):887–894
Choi Y, Kim TY, Oh DY et al (2016) The impact of diabetes mellitus and metformin treatment on survival of patients with advanced pancreatic cancer undergoing chemotherapy. Cancer Res Treat 48(1):171
Nakai Y, Isayama H, Sasaki T et al (2013) Clinical outcomes of chemotherapy for diabetic and nondiabetic patients with pancreatic cancer: better prognosis with statin use in diabetic patients. Pancreas 42(2):202–208
He Xiang Y, Yao WY et al (2013) Resolution of new-onset diabetes after radical pancreatic resection; predicts long-term survival in patients with pancreatic ductal cell; adenocarcinoma. Ann Surg Oncol 20(12):3809–3816
Zeiss K, Parhofer KG, Heinemann V et al (2013) Glucose and lipid metabolism in patients with advanced pancreatic cancer receiving palliative chemotherapy. Anticancer Res 33(1):287–292
Currie CJ, Poole CD, Jenkins-Jones S et al (2012) Mortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survival. Diabetes Care 35(2):299–304
Del CM, Rangelova E, Segersvärd R et al (2016) Are there still indications for total pancreatectomy? Updates Surg 68(3):257–263
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 26(suppl 1):S5–S20
Hart PA et al (2016) Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. Lancet Gastroenterol Hepatol 1(3):226–237
Pannala R, Basu A, Petersen GM et al (2009) New-onset diabetes: a potential clue to the early diagnosis of pancreatic cancer. Lancet Oncol 10(1):88–95
Hackeng WM, Hruban RH, Offerhaus GJA et al (2016) Surgical and molecular pathology of pancreatic neoplasms. Diagn Pathol 11(1):47
Dong X, Li Y, Chang P et al (2011) Glucose metabolism gene variants modulate the risk of pancreatic cancer. Cancer Prev Res 4(5):758
Garcea G, Dennison AR, Pattenden CJ et al (2015) Survival following curative resection for pancreatic ductal adenocarcinoma. A systematic review of the literature. JOP 9(2):99–132
Ilic M, Ilic I (2016) Epidemiology of pancreatic cancer. World J Gastroenterol 22(44):9694–9705
Lv X, Qiao W, Leng Y et al (2017) Impact of diabetes mellitus on clinical outcomes of pancreatic cancer after surgical resection: a systematic review and meta-analysis. PLoS ONE 12(2):e0171370
Tan J, You Y, Guo F et al (2017) Association of elevated risk of pancreatic cancer in diabetic patients: a systematic review and meta-analysis. Oncol Lett 13(3):1247–1255
Shen H, Zhan M, Wang W et al (2016) Impact of diabetes mellitus on the survival of pancreatic cancer: a meta-analysis. Oncotarg Ther 9(1):1679–1688
Becker AE, Hernandez YG, Frucht H et al (2014) Pancreatic ductal adenocarcinoma: risk factors, screening, and early detection. World J Gastroenterol 20(32):11182
Li D, Mao Y, Ping C et al (2014) Impacts of new-onset and long-term diabetes on clinical outcome of pancreatic cancer. Am J Cancer Res 5(10):3260–3269
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 81560480), Health Science Research Program of Gansu Province (No. GSWSKY2016-19), and Ph.D. Science Research Foundation of Lanzhou University Second Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there was no any conflict of interests in this article.
Informed consent
None.
Statement of human and animal rights
This study is a meta-analysis of other studies where all procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, J., Wang, J., Ge, L. et al. The impact of diabetes mellitus on clinical outcomes following chemotherapy for the patients with pancreatic cancer: a meta-analysis. Acta Diabetol 56, 1103–1111 (2019). https://doi.org/10.1007/s00592-019-01337-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01337-2