Abstract
Background
Pancreatic diseases have long been associated with impaired glucose control. This study sought to identify the incidence of new insulin-dependent diabetes mellitus (IDDM) after pancreatectomy and the predictive accuracy of hemoglobin A1c (HbA1c) or blood glucose.
Methods
Patients who underwent partial pancreatectomy and had preoperative HbA1c available at two academic institutions were assessed for new IDDM on discharge in relation to complication rates and survival.
Results
Of the 267 patients analyzed, 67% had abnormal HbA1c levels prior to surgery (mean 6.8%, glucose 135 mg/dL). Two hundred eight (77.9%) were not insulin-dependent prior to surgery, and 35 (16.8%) developed new IDDM after resection. On multivariable regression, increasing HbA1c and preoperative glucose were the only significant predictors for new IDDM. Optimal predictive cutoffs (HbA1c of 6.25% and glucose of 121 mg/dL) were determined in a discovery group (n = 143) and confirmed in a validation group (n = 124) with a diagnostic sensitivity of 72.7% and specificity of 84.8%. Patients with new IDDM after resection had higher rates of severe complications (OR 3.39), increased TPN at discharge (OR 4.32), and increased rates of discharge to nursing facilities (OR 2.57) (all P < 0.05). New IDDM was also associated with a decreased cancer-specific survival.
Conclusion
Preoperative HbA1c ≥ 6.25% and blood glucose ≥ 121 mg/dL can accurately identify patients at increased risk of IDDM. These diagnostics may help identify patients in a preoperative setting that may benefit from interventions such as diabetes education or enhanced glucose control preoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rates of pancreatectomy for both malignant and benign pancreatic disease have increased in recent years, with concomitant improvements in morbidity and mortality despite expanded patient selection criteria.3,5,17,25 As the US population ages, there is an increasing incidence of pancreatic cancer, and projections estimate it will be the second leading cause of cancer death by 2030.29 In addition, as the use of cross-sectional imaging increases and the quality of imaging improves, an increasing number of lesions of the pancreas are identified with a percentage requiring resection.13 Currently, the morbidity for pancreaticoduodenectomy remains at 30–50% and quality improvement has focused on perioperative care, with the goal of recognizing and acting upon modifiable risk factors using evidence-based bundles.27,31,32
Glycemic dysfunction is a unique hallmark of pancreatic cancer biology and is bidirectional such that diabetes increases the long-term risk for pancreatic cancer, while pancreatic cancer itself is associated with diabetes.14 Unlike other malignancies, pancreatic cancer puts patients in a diabetogenic state with up to 47% having diabetes mellitus (DM) and 38% having impaired fasting glucose or pre-diabetes.28 This is significantly higher than age-matched controls and may be mechanistically related to parenchymal destruction, β-cell dysfunction, insulin resistance associated with cachexia, or a tumor-mediated paraneoplastic phenomenon.15 This finding holds in premalignant lesions as well; the risk of DM has been shown to be associated with the degree of dysplasia of resected intraductal papillary mucinous neoplasms.20
The incidence of new DM after resection is highest after distal pancreatectomy (up to 36%) due to a loss of the majority of insulin-producing parenchyma.4,9,18 After pancreaticoduodenectomy, the incidence of new-onset diabetes is up to 18%, and half of existing diabetics require increases in DM medication regimens after resection.4,11,23 Acquisition of insulin-dependent diabetes mellitus (IDDM) in the short-term increases perioperative risk such as pancreatic fistula (up to 4.3-fold), but also in the long-term, it is a significant lifestyle-altering change.8,21 DM also plays a role in survival outcomes as multiple studies have found elevated hemoglobin A1c (HbA1c), a measurement of average blood glucose over a 90-day period, to be associated with decreased long-term survival after resection of pancreatic cancer.6,7,12,33
The identification of patients preoperatively who are at risk for developing postoperative IDDM may allow early intervention and the possibility of improving perioperative and long-term outcomes. Prior studies have identified HbA1c thresholds as a risk for post-pancreatectomy diabetes,23 and other studies have identified uncontrolled blood glucose as a predictor for inferior outcomes;33 thus, HbA1c may also be an important predictor of risk. Therefore, the goals of the current investigation were to define factors that may facilitate identification of patients without IDDM patients whom are at risk for developing IDDM postoperatively and quantify adverse outcomes related to new insulin dependence.
Materials and Methods
Data Acquisition and Cohort Selection
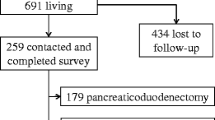
Patients were identified from the Ohio State University (OSU) and Baylor College of Medicine (BCM) who underwent pancreaticoduodenectomy, distal pancreatectomy, and duodenum preserving pancreatic head resection who had a HbA1c measured prior to surgery. Patients who underwent total pancreatectomy were excluded. At OSU, this included patients with operations between November 2011 and October 2017 and at BCM between December 2005 and June 2017. For analysis of our primary outcome — new IDDM at discharge — we split the entire cohort into a discovery group and validation group by including consecutive patients at OSU from November 2011 to January 2017 to the discovery group and the remaining patients from OSU from January to October 2017 as well as the cohort from BCM to the validation group (Supplemental Fig. 1). The study was approved by the institutional review board at both institutions.
Diabetes Definitions
A diabetic history variable was reported based on review of past medical history and preoperative medication list noted in the chart. Patients were also classified by preoperative medication regimen (no medications; oral medications; or insulin). Furthermore, patients were classified based upon preoperative HgA1C (measured within 6-months preoperatively) and blood glucose (measured via serum glucose within 30 days prior to surgery or in the preoperative area using fingerstick point-of-care testing) according to definitions published by the American Diabetic Association (ADA) (pre-diabetes, fasting blood sugar 100–125 mg/dL or HbA1c 5.7–6.5%; diabetes, use of DM meds, fasting blood sugar ≥ 126 mg/dL, or hemoglobin A1c (HbA1c) ≥ 6.5%).1 Glucose was labeled as under control in those patients with a preoperative HbA1c ≤ 7%. Uncontrolled diabetes was defined as a HbA1c ≥ 10%).
The discharge summary from the index hospitalization was used to determine if insulin and/or oral DM medications were continued/prescribed at discharge. If a readmission occurred within 30 days, the subsequent discharge summary was used.
Patients were ultimately classified into 3 groups. Patients were deemed at risk when they did not use insulin preoperatively, irrespective of DM history. If they did not develop insulin dependence after surgery, they were further classified as at-risk-no-change; if they developed insulin dependence after surgery, they were classified as at-risk-new-IDDM. Patients were classified as not at risk when they were already using insulin prior to surgical intervention (known-IDDM). Long-term diabetes outcomes were measured at least 6 months after surgery.
Complication Definitions
Complications were graded I–V based on Clavien-Dindo classification. Severe complications were classified as those grades III and above.10 Postoperative pancreatic fistula and delayed gastric emptying were graded based on published International Study Group of Pancreatic Surgery (ISGPS) definitions.2,34
Statistical Analysis
Diabetic medication use was coded as an ordinal variable with no medications as the lowest, increasing to oral medications and then insulin use with or without oral medications. Death was coded both as death from any cause or death from cancer to determine overall survival (OS) and disease-specific survival (DSS), respectively.
Continuous variables when parametric were analyzed by mean and interquartile range (IQR) using the independent sample t-test with 2-tailed significance. When non-parametric, they were analyzed by median and interquartile range (IQR) using the Kruskal–Wallis test. Binary, ordinal, and categorical variables were compared as proportions using Pearson Chi-square test with 2-tailed significance. Multivariable logistic regression was performed for the primary outcome of interest in the at-risk population only. All variables which met p ≤ 0.05 significance on univariable analysis were included in the multivariable model. Receiver operating characteristic (ROC) curves were created using significant variables on multivariable analysis, as well as the multivariable model, in the discovery patient cohort. Youden’s J statistic (or c-statistic) was calculated as J = sensitivity + specificity – 1 for each point, and the highest value was chosen as the optimal cutoff for each covariate independently. Survival analysis was performed using OS in patients without cancer and using DSS in patients with cancer. A Cox proportional hazard model was created by incorporating all values which were predictive with p ≤ 0.05 significance on univariable analysis. The Kaplan–Meier method was used for plotting proportion surviving over time, and the log-rank statistic was used to compare survival curves. Statistical analysis was performed using SPSS v21 (IBM).
Results
Cohort Characteristics
The current analysis included 267 patients (OSU, 74.2%; BCM, 25.8%) who underwent a partial pancreatectomy and had a recorded preoperative HbA1c available for analysis. The mean age was 62.1 years (IQR 54.0–71.9), the majority were of the white race (84.6%), and approximately half were male (50.9%). A history of diabetes, as defined by the past medical history and preoperative medication list noted in the chart, was present in half of patients (49.8%). There were 43.8% of patients that used oral DM medications or insulin prior to surgery. Amongst all patients, the mean preoperative HbA1c was 6.8% (IQR 5.5–7.7%) with 6% of patients being ≥ 10%. The majority of patients underwent pancreaticoduodenectomy (67.4%), and 62.2% had surgery performed for oncological pathology. Benign pathology represented 37.8% of the cohort, with 21 patients having a diagnosis of chronic pancreatitis (Table 1).
Amongst the 3 groups, the at-risk-no-change group consisted of 173 patients (64.8%), the at-risk-new-IDDM consisted of 35 patients (16.8%), and the known-IDDM group consisted of 59 patients (22.1%) (Table 1). Comparing these 3 groups, those in the at-risk-new-IDDM group had higher mean HbA1c levels than those in the at-risk-no-change group (7.8% compared to 6.0%, p < 0.001) and lower mean HbA1c levels than those in the known-IDDM group (7.8% compared to 8.5%, p < 0.001).
There were no differences in the use of neoadjuvant chemotherapy amongst groups, nor in the specific operations each group underwent (p > 0.05). Laparoscopic/robotic procedures were used more commonly in those patients not using insulin preoperatively (at-risk-no-change, 16.2%; at-risk-new-IDDM, 20.0%; known-IDDM, 3.4%; p = 0.026). The respective representation of the at-risk-new-IDDM groups in the discovery and validation cohorts were not different from each other (16.1% compared to 9.7%, p = 0.122); representation was also not different between OSU and BCM institutions (15.2% compared to 7.2%, p = 0.094).
Factors Associated with New Insulin-Dependent Diabetes After Pancreatectomy
On univariable analysis, several factors were associated with developing new insulin dependence after surgery including elevated levels of preoperative HbA1c (odds ratio (OR) 1.81, p < 0.001), increased levels of glucose (OR 1.03, p < 0.001), and surgery for pancreatic ductal adenocarcinoma (PDAC) compared to benign pathology, (OR 3.60, p = 0.006). Patients who had a HbA1c < 7% were not as likely to develop new insulin dependence after surgery compared to those with a HbA1c above 7% (OR 0.13, p < 0.001). On multivariable modeling, factors that were independently associated with developing new insulin dependence after surgery included increases in HbA1c (OR 1.41, p = 0.007) and increases in glucose levels (OR 1.02, p = 0.004) (Table 2).
A ROC curve analysis was used to determine the discrimination of HbA1c, glucose, and the entire multivariable model for the development of new insulin dependence after surgery in the at-risk cohort. This was performed in the discovery group (n = 103), repeated in the validation group (n = 105) (Fig. 1), and lastly in the entire at-risk cohort (Supplemental Fig. 2). The area under the curve (AUC) analysis shown in the discovery set HbA1c (AUC 0.837, p < 0.001), glucose (0.817, p < 0.001), and the multivariable model (0.888, p < 0.001) all showed good discrimination, though the addition of multiple variables in the model did not add significantly to either HbA1c or glucose alone. From the discovery cohort, the value with the highest sensitivity and specificity in the detection of at-risk patients developing IDDM was found to be at the cutoff of HbA1c ≥ 6.25% and glucose ≥ 121 mg/dL. These values were then applied to the validation group, and the use of both HbA1c and glucose cutoffs showed a diagnostic sensitivity of 72.7% and specificity of 84.8%. Positive predictive value of using both variables together was improved to 36.4%, and negative predictive value stayed at a high level of 96.3%.
ROC curve analysis of discrimination for new IDDM. a In the discovery cohort (n = 103), optimal cutoffs were determined. b In the validation cohort (n = 105), the metrics of the determined cutoffs were evaluated. Abbreviations: area under the curve (AUC), positive predictive value (PPV), negative predictive value (NPV)
Development of Insulin-Dependent Diabetes After Surgery and Postoperative Outcomes
The incidence of postoperative pancreatic fistula did not differ between groups (at-risk-no-change, 19.7%; at-risk-new-IDDM, 17.1%; known-IDDM, 16.9%; p = 0.870) (Supplemental Table 1). Figure 2 displays early postoperative results of the univariable analysis comparing those at-risk-new-IDDM patients to the at-risk-no-change patients. Compared to the at-risk-no-change patients, the at-risk-new-IDDM patients had an increased risk of severe complications (OR 3.39, p = 0.026). This effect was emphasized when looking specifically at Clavien-Dindo class IV complications (OR 7.67, p = 0.016). However, there was no difference in the risk of grade B/C pancreatic fistula between the groups (OR 4.44, p = 0.194). Resource utilization at discharge was increased in the at-risk-new-IDDM patients with increased TPN use (OR 4.32, p = 0.036) and discharge to SNF (OR 2.57, p = 0.030). While severe complications did not lead to increased 30-day mortality, there was an increase in mortality at 1-year (OR 3.37, p = 0.013) in the at-risk-new-IDDM patients.
Long-term diabetes-specific outcomes after pancreatectomy are displayed in Table 3. After 6 months or more of follow-up, 91.2% of patients in the at-risk-new-IDDM group were still requiring insulin. Overall, increases in diabetic medications were seen in 33 patients (12.8%) during the 6 months following surgery. Although the at-risk-no-change group did not require insulin at discharge, there were 9.1% of patients who eventually required insulin for DM management at 6 months. Of the patients who required TPN at discharge (n = 10), all those in the at-risk-new-DM group (n = 4) still required insulin at long-term follow-up. There were limited patients (n = 64) in which a postoperative hemoglobin A1c was available, thus determining glucose control in the at-risk-new-DM cohort was limited.
Long-Term Impact of Diabetes on Survival
On univariable analysis in those with pancreatic cancer, the hazard ratio (HR) was 1.17 (p = 0.033) for each 1% increase in HbA1c. Furthermore, a decreased survival was found in those at-risk patients who developed IDDM after surgery (i.e., the at-risk-new-DM group) compared to the at-risk-no-DM group (HR 2.54, p = 0.020) (Table 4). On multivariable modeling, the only factor independently associated with worse disease-specific survival (DSS) was HbA1c (HR 1.31 per 1% HbA1c increase, p = 0.034). In patients with benign pathology as indication for pancreatectomy, there was a decrease in 3-year OS only in the known-IDDM group (at-risk-no-change, 97%; at-risk-new-DM, 100%; known-IDDM, 71%; p = 0.010) (Supplemental Figure 3).
DSS was then examined amongst the three groups with pancreatic cancer. The median DSS overall was 44.7 months (95% confidence interval 37.8–51.6 months). DSS was decreased in patients in the at-risk-new-DM group compared to the at-risk-no-change group (median DSS, 17.3 months vs. 46.1 months, p = 0.019) (Fig. 3a). As HbA1c was previously found to be independently associated with decreased survival, DSS was next examined in those with a HbA1c ≥ 6.25% compared to those < 6.25%. Patients with a HbA1c ≥ 6.25% were found to have decreased median DSS (23.7 months) compared to patients with HbA1c < 6.25 (median 57.8 months, p = 0.008) (Fig. 3b).
Discussion
The influence of uncontrolled glucose on short- and long-term outcomes after surgery is well-established.6,7,8,12,21,33 Patients undergoing pancreatectomy are at particular risk given that resection removes the β-cells responsible for innate insulin production, evidenced by 16.8% of the study population newly requiring insulin after resection. With the goal of developing reliable measures that can identify patients at risk for developing IDDM preoperatively, HbA1c and blood glucose were identified as independent predictors of postoperative insulin use after pancreatectomy. These findings support recent results of these markers for predicting postoperative diabetes.23,24 The findings also highlight that there are many undiagnosed patients who should be picked up by routine preoperative screening, as 50% of patients were diabetic by history; however, 67% were diabetic or pre-diabetic by established HbA1c or blood glucose criteria before resection. Even those with a preoperative diagnosis of IDDM exhibited poor glucose control evidenced by a HbA1c < 7% in only 40% of these patients, further highlighting the need for necessary screening and intervention.
Patients with new IDDM after surgery were found to have an increased risk of severe complications and discharge to a nursing facility as previously reported.22,26 In addition, outcomes of patients that developed IDDM after surgery had similar outcomes to those with existing IDDM. These data are novel in that they connect a HbA1c screening threshold to the risk of postoperative complications. Furthermore, the findings support the identification of patients at risk for developing IDDM preoperatively in order to not only ascertain their perioperative risk but also potentially to diminish their risks by controlling their glucose perioperatively. This need is emphasized by the finding of those at-risk-new-IDDM patients who had an overall mean HbA1c of 7.8%. Once a patient screens in, interventions such as preoperative teaching and aggressive blood sugar control with insulin may potentially improve complication rates or grade of pancreatic leak. Improvements in glycemic control using insulin preoperatively may also promote adherence to insulin regimens postoperatively. Although clinical decisions should usually not be delayed for glucose management/education, starting early may allow earlier and quicker control as glucose management interventions may need to extend well beyond the postoperative period. Those patients who developed IDDM after resection stayed dependent on insulin in the long-term, evidenced by a majority (91.2%) of those with new-onset IDDM after resection requiring insulin on follow-up 6 months out from surgery.
Hemoglobin A1c and blood glucose were found be good independent predictors (AUC 0.837 and 0.817, respectively) of new IDDM. Cutoff values 6.25% and 121 mg/dL were selected using the discovery group, and application of these values to the validation group showed a 73% sensitivity and 85% specificity. Hemoglobin A1c cutoffs have been examined previously, with one study determining a HbA1c level of 5.7% or greater to be associated with new-onset diabetes after distal pancreatectomy30 and another demonstrating the higher the HbA1C post-pancreatectomy, the greater risk of developing new-onset diabetes.24 These two diagnostics make for excellent screening tools as they are simple, inexpensive, easy to obtain through point-of-care testing in the office. The cutoff values selected are accurate and maximize the sensitivity and specificity. Screening can potentially impact a large volume of patients as 60% meet either cutoff and 34.7% screen positive using both values. The identified screening parameters also resulted in a negative predictive value of 96%, allowing for accurate identification of patients very likely to avoid the need for insulin postoperatively.
It is well-established that a diagnosis of IDDM prior to pancreatectomy lends to a relatively worse long-term prognosis as several studies have previously shown.6,19 The worse survival is hypothesized to be due to larger tumors and may be a marker of more advanced systemic disease which is not managed with resection.19 Furthermore, the resolution of new-onset (within 2 years of diagnosis) IDDM with resection is associated with improved survival.16 Our findings reiterate this finding as those with cancer and HbA1c ≥ 6.25%, while not only being at risk for new insulin dependence, have decreased DSS. Interestingly, it was found that new IDDM after resection was a risk factor for decreased DSS (median 23.7 months vs 57.8 months), similar to those with known IDDM. The decreased survival may be in part due to increased rates of major complications or alternatively further corroborates the link of DM as a sign of aggressive pancreatic cancer biology.
There are limitations which should be acknowledged. First, HbA1c is not a routine part of the workup for pancreatectomy at most institutions, and there may be selection bias in our study population. However, the surgeons at OSU routinely measured HbA1c starting in 2014 and thus are likely representative. The utilization of a discovery and validation group predominately from different institutions to confirm the HbA1c and glucose cutoffs externally validates these findings.7,8,12,21 The duration of preoperative diabetes and the intensity of preoperative medication treatment were not available and thus could not be included in our multivariable model. Furthermore, adherence to diabetic medications and ensuring medication dosing at follow-up was limited. We were not able to differentiate insulin use in relation to the need for TPN on discharge or due to DM. The development of IDDM has clinical and practical implications, as does initiation of new oral antihyperglycemics; a very small minority started oral antihyperglycemics in the postoperative period; however, this subset of patients warrants further investigation. Lastly, the cohort was comprised of two discrete groups (i.e., benign and malignant disease); however, physician care for these patients usually spans both cohorts and inclusivity of each lends to practical conclusions.
Conclusion
HbA1c greater than 6.25% and blood glucose levels greater than 121 mg/dL are simple and accurate screening tools to determine the risk for new insulin dependence after pancreatectomy. Screening should be performed as new IDDM after resection portends increased risk of severe complications and may impact cancer-specific survival outcomes. More aggressive diabetic treatment of patients who screen positive before pancreatectomy may help improve outcomes after resection.
References
2017. Classification and Diagnosis of Diabetes. Diabetes Care. Jan, 40 (Supplement 1), S11–S24. https://doi.org/10.2337/dc17-S005.
Bassi, C. et al. 2017. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 161, 3: 584–591. https://doi.org/10.1016/j.surg.2016.11.014.
Bilimoria, K.Y., Bentrem, D.J., Ko, C.Y., Stewart, A.K., Winchester, D.P. and Talamonti, M.S. 2007. National failure to operate on early stage pancreatic cancer. Annals of Surgery. 246, 2, 173–180. https://doi.org/10.1097/SLA.0b013e3180691579.
Burkhart, R.A. et al. 2015. Incidence and Severity of Pancreatogenic Diabetes After Pancreatic Resection. Journal of Gastrointestinal Surgery. 19, (2015), 217–225. https://doi.org/10.1007/s11605-014-2669-z.
Cameron, J.L. and He, J. 2015. Two thousand consecutive pancreaticoduodenectomies. Journal of the American College of Surgeons. 220, 4, 530–536. https://doi.org/10.1016/j.jamcollsurg.2014.12.031.
Cannon, R.M. et al. 2012. Multi-institutional analysis of pancreatic adenocarcinoma demonstrating the effect of diabetes status on survival after resection. HPB. 14, (2012), 228–235. https://doi.org/10.1111/j.1477-2574.2011.00432.x.
Chagpar, R.B. et al. 2011. Medically Managed Hypercholesterolemia and Insulin-Dependent Diabetes Mellitus Preoperatively Predicts Poor Survival after Surgery for Pancreatic Cancer. Journal of Gastrointestinal Surgery. 15, 4, 551–557. https://doi.org/10.1007/s11605-011-1448-3.
Chu, C.K., Mazo, A.E., Sarmiento, J.M., Staley, C.A., Adsay, N.V., Umpierrez, G.E. and Kooby, D.A. 2010. Impact of Diabetes Mellitus on Perioperative Outcomes after Resection for Pancreatic Adenocarcinoma. Journal of the American College of Surgeons. 210, 4, 463–473. https://doi.org/10.1016/j.jamcollsurg.2009.12.029.
De Bruijn, K.M.J. and Van Eijck, C.H.J. 2015. New-onset Diabetes after Distal Pancreatectomy: A Systematic Review. Annals of Surgery. 261, 5, 854–861. https://doi.org/10.1097/SLA.0000000000000819.
Dindo, D., Demartines, N. and Clavien, P.A. 2004. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 240, 2, 205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Ehehalt, F., Sturm, D., Rösler, M., Distler, M., Weitz, J., Kersting, S., Ludwig, B., Schwanebeck, U., Saeger, H.D., Solimena, M. and Grützmann, R. 2015. Blood glucose homeostasis in the course of partial pancreatectomy - Evidence for surgically reversible diabetes induced by cholestasis. PLoS ONE. 10, 8, e0134140. https://doi.org/10.1371/journal.pone.0134140.
Fan, K.Y. et al. 2014. Baseline hemoglobin-A1c impacts clinical outcomes in patients with pancreatic cancer. JNCCN Journal of the National Comprehensive Cancer Network. 12, 1, 50–57. https://doi.org/10.6004/jnccn.2014.0006.
Gaujoux, S., Brennan, M.F., Gonen, M., D’Angelica, M.I., DeMatteo, R., Fong, Y., Schattner, M., DiMaio, C., Janakos, M., Jarnagin, W.R. and Allen, P.J. 2011. Cystic lesions of the pancreas: Changes in the presentation and management of 1,424 patients at a single institution over a 15-year time period. Journal of the American College of Surgeons. 212, 4, 590–600. https://doi.org/10.1016/j.jamcollsurg.2011.01.016.
Hart, P.A. and Chari, S.T. 2013. Diabetes mellitus and pancreatic cancer: Why the association matters? Pancreas.
Hart, P.A. and Chari, S.T. 2015. Pancreapedia: The Exocrine Pancreas Knowledge Base. Pancreapedia: Exocrine Pancreas Knowledge Base. https://doi.org/10.3998/panc.2015.34.
He, X.Y., Li, J.F., Yao, W.Y. and Yuan, Y.Z. 2013. Resolution of new-onset diabetes after radical pancreatic resection predicts long-term survival in patients with pancreatic ductal cell adenocarcinoma. Annals of Surgical Oncology. 20, 12, 3809–3816. https://doi.org/10.1245/s10434-013-3095-2.
He, J., Ahuja, N., Makary, M.A., Cameron, J.L., Eckhauser, F.E., Choti, M.A., Hruban, R.H., Pawlik, T.M. and Wolfgang, C.L. 2014. 2564 resected periampullary adenocarcinomas at a single institution: Trends over three decades. HPB. 16, 1, 83–90. https://doi.org/10.1111/hpb.12078.
Kang, J.S., Jang, J.Y., Kang, M.J., Kim, E., Jung, W., Chang, J., Shin, Y., Han, Y. and Kim, S.W. 2016. Endocrine Function Impairment after Distal Pancreatectomy: Incidence and Related Factors. World Journal of Surgery. 40, (2016), 440–446. https://doi.org/10.1007/s00268-015-3228-9.
Kleeff, J. et al. 2016. The impact of diabetes mellitus on survival following resection and adjuvant chemotherapy for pancreatic cancer. British Journal of Cancer. 115, 7, 887–894. https://doi.org/10.1038/bjc.2016.277.
Leal, J.N., Kingham, T.P., D’Angelica, M.I., DeMatteo, R.P., Jarnagin, W.R., Kalin, M.F. and Allen, P.J. 2015. Intraductal Papillary Mucinous Neoplasms and the Risk of Diabetes Mellitus in Patients Undergoing Resection Versus Observation. Journal of Gastrointestinal Surgery. 19, (2015), 1974–1981. https://doi.org/10.1007/s11605-015-2885-1.
Lee, W., Yoon, Y.S., Han, H.S., Cho, J.Y., Choi, Y., Jang, J.Y. and Choi, H. 2016. Prognostic relevance of preoperative diabetes mellitus and the degree of hyperglycemia on the outcomes of resected pancreatic ductal adenocarcinoma. Journal of Surgical Oncology. 113, (2016), 203–208. https://doi.org/10.1002/jso.24133.
Malleo, G., Mazzarella, F., Malpaga, A., Marchegiani, G., Salvia, R., Bassi, C. and Butturini, G. 2013. Diabetes mellitus does not impact on clinically relevant pancreatic fistula after partial pancreatic resection for ductal adenocarcinoma. Surgery. 153, 5, 641–650. https://doi.org/10.1016/j.surg.2012.10.015.
Maxwell, D.W., Jajja, M.R., Tariq, M., Mahmooth, Z., Galindo, R.J., Sweeney, J.F. and Sarmiento, J.M. 2019. Development of Diabetes after Pancreaticoduodenectomy : Results of a 10-Year Series Using Prospective Endocrine Evaluation. Journal of the American College of Surgeons. 228, 4, 400–414.
Maxwell, D.W., Jajja, M.R., Galindo, R.J., Nadeem, S.O., Sweeney, J.F., Blair, C.M. and Sarmiento, J.M. 2020. Post-Pancreatectomy Diabetes Index : A Validated Score Predicting Diabetes Development after Major Pancreatectomy. Journal of the American College of Surgeons. 230, 4, 393–404.
Mayo, S.C., Herman, J.M., Cosgrove, D., Bhagat, N., Kamel, I., Geschwind, J.F.H. and Pawlik, T.M. 2013. Emerging approaches in the management of patients with neuroendocrine liver metastasis: Role of liver-directed and systemic therapies. Journal of the American College of Surgeons. 216, 1, 123–134. https://doi.org/10.1016/j.jamcollsurg.2012.08.027.
McAuliffe, J.C. and Christein, J.D. 2013. Type 2 Diabetes Mellitus and Pancreatic Cancer. Surgical Clinics of North America. 93, 3, 619–627. https://doi.org/10.1016/j.suc.2013.02.003.
McMillan, M.T. et al. 2016. Risk-adjusted Outcomes of Clinically Relevant Pancreatic Fistula Following Pancreatoduodenectomy: A Model for Performance Evaluation. Annals of Surgery. 264, 2, 344–352. https://doi.org/10.1097/SLA.0000000000001537.
Pannala, R., Leirness, J.B., Bamlet, W.R., Basu, A., Petersen, G.M. and Chari, S.T. 2008. Prevalence and Clinical Profile of Pancreatic Cancer-Associated Diabetes Mellitus. Gastroenterology. 134, 4, 981–987. https://doi.org/10.1053/j.gastro.2008.01.039.
Rahib, L., Smith, B.D., Aizenberg, R., Rosenzweig, A.B., Fleshman, J.M. and Matrisian, L.M. 2014. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Research. 74, 11, 2913–2921. https://doi.org/10.1158/0008-5472.CAN-14-0155.
Shirakawa, S., Matsumoto, I., Toyama, H., Shinzeki, M., Ajiki, T., Fukumoto, T. and Ku, Y. 2012. Pancreatic Volumetric Assessment as a Predictor of New-Onset Diabetes Following Distal Pancreatectomy. Journal of Gastrointestinal Surgery. 16, 12, 2212–2219. https://doi.org/10.1007/s11605-012-2039-7.
Shubert, C.R., Kendrick, M.L., Habermann, E.B., Glasgow, A.E., Borah, B.J., Moriarty, J.P., Cleary, S.P., Smoot, R.L., Farnell, M.B., Nagorney, D.M., Truty, M.J. and Que, F.G. 2018. Implementation of prospective, surgeon-driven, risk-based pathway for pancreatoduodenectomy results in improved clinical outcomes and first year cost savings of $1 million. Surgery. 163, 3, 495–502. https://doi.org/10.1016/j.surg.2017.10.022.
Vin, Y., Sima, C.S., Getrajdman, G.I., Brown, K.T., Covey, A., Brennan, M.F. and Allen, P.J. 2008. Management and Outcomes of Postpancreatectomy Fistula, Leak, and Abscess: Results of 908 Patients Resected at a Single Institution Between 2000 and 2005. Journal of the American College of Surgeons. 207, 4, 490–498. https://doi.org/10.1016/j.jamcollsurg.2008.05.003.
Walter, U., Kohlert, T., Rahbari, N.N., Weitz, J. and Welsch, T. 2014. Impact of preoperative diabetes on long-term survival after curative resection of pancreatic adenocarcinoma: A systematic review and meta-analysis. Annals of Surgical Oncology. 21, 1082–1089. https://doi.org/10.1245/s10434-013-3415-6.
Wente, M.N., Bassi, C., Dervenis, C., Fingerhut, A., Gouma, D.J., Izbicki, J.R., Neoptolemos, J.P., Padbury, R.T., Sarr, M.G., Traverso, L.W., Yeo, C.J. and Büchler, M.W. 2007. Delayed gastric emptying (DGE) after pancreatic surgery: A suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 142, 5, 761–768. https://doi.org/10.1016/j.surg.2007.05.005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Ellison reports personal fees from McGraw Hill Medical and personal fees from Wolters Kluwer.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
Supplemental Fig. 1 Schematic depicting the discovery and validation groups. Supplemental Fig. 2 ROC curve analysis of discrimination for new IDDM in the entire at-risk cohort (n = 208). Supplemental Fig. 3 Overall survival of patients with benign pathology by diabetes group (n = 102) (PDF 192 kb)
ESM 2
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Wiseman, J.T., Chakedis, J., Beal, E.W. et al. Hemoglobin A1c Is a Predictor of New Insulin Dependence After Partial Pancreatectomy: A Multi-Institutional Analysis. J Gastrointest Surg 25, 3119–3129 (2021). https://doi.org/10.1007/s11605-021-05014-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05014-0