Abstract
Background
Primary hyperparathyroidism (PHPT) affects 2% of Americans over 55 years of age, and is less common in younger patients. Pediatric PHPT patients have higher rates of multigland disease (MGD). We studied young adult patients to determine whether they have similarly elevated rates of MGD and would benefit from routine bilateral neck exploration.
Methods
Retrospective chart review was performed on patients who underwent parathyroidectomy for PHPT (2000–2019). Cohorts were defined by age: Group A (18–40 years) and Group B (> 40 years). Univariate and multivariate logistic regression analyses were performed.
Results
Of 3889 patients with PHPT, 9.1% (n = 352) were included in Group A. On multivariate analysis, multiple endocrine neoplasia (odds ratio [OR] 6.3, 95% confidence interval [CI] 3.1–12.7), male sex (OR 1.3, 95% CI 1.0–1.5), family history of PHPT (OR 2.7, 95% CI 1.6–4.8), prior parathyroidectomy (OR 2.2, 95% CI 1.6–3.0), and non-localizing imaging (OR 1.8, 95% CI 1.5–2.1) were associated with MGD; younger age was not an independent risk factor. In patients with sporadic PHPT (n = 3833), family history was most strongly associated with MGD (OR 4.0, 95% CI 2.2–7.3).
Conclusions
In our population of patients with sporadic PHPT, a positive family history of PHPT was strongly associated with MGD; additional associations were found with prior parathyroidectomy, non-localizing imaging, and male sex. Younger age was not an independent risk factor. Age alone in the absence of a family history should not raise suspicion for MGD nor determine the need for bilateral neck exploration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Primary hyperparathyroidism (PHPT) affects approximately 2% of Americans over the age of 55 years,1 and is less common in younger patients. Until 1982, just 86 cases of pediatric PHPT had been reported in the literature.2,3,4 High rates of multigland disease (MGD) have been reported in pediatric patients with PHPT diagnosed outside the neonatal period, with published incidences of hyperplasia ranging from 16 to 23% in larger pediatric series.2,4 Young adults also have a low prevalence of PHPT; one large institutional series found that approximately 3% of parathyroidectomies performed at a tertiary care center were performed on patients aged 28 years or younger.5 Greater proportions of MGD have also been identified in adolescent and young adult patients, 18.5–27% of whom have hyperplasia on surgical pathology.5,6 Notably, the majority of studies in young patients do not differentiate between sporadic PHPT and inherited PHPT, and include patients with multiple endocrine neoplasia type 1 (MEN1), multiple endocrine neoplasia type 2A (MEN2A), and familial isolated hyperparathyroidism (FIHP). Systemic reviews show that up to half of cases of hyperplasia in patients under the age of 20 years are due to PHPT associated with inherited syndromes.7
Since patients with MGD are not eligible for minimally invasive parathyroidectomy (MIP), patients with MEN or other risk factors for MGD are best managed by bilateral neck exploration and subtotal parathyroidectomy. Classically, inherited endocrinopathies present at an early age, and current guidelines recommend genetic screening for MEN in patients presenting with PHPT at 40 years of age or younger.8 Some authors suggest that younger age alone is a risk factor for MGD and advocate performing bilateral neck exploration routinely in young patients.9 We sought to establish whether young adult patients (18–40 years of age) with PHPT have heightened suspicion for MGD and would benefit from routine bilateral neck exploration and/or subtotal parathyroidectomy.
Methods
Study Population
Consecutive patients who underwent parathyroidectomy for PHPT at our tertiary medical center over a 12-year period (January 2000–April 2013) were identified from our prospectively maintained endocrine surgery database. Children (< 18 years of age), and patients with secondary or tertiary hyperparathyroidism were excluded.
Variables
Data abstracted on retrospective chart review included patient demographics and past medical history (sex, age, positive family history of PHPT, history of prior parathyroidectomy, history of MEN1 or MEN2A), biochemical testing (preoperative serum calcium level, preoperative 24-h urinary calcium level, preoperative serum parathyroid hormone [PTH] level), preoperative signs (nephrolithiasis and loss of bone mineralization as determined by DXA scan), and symptoms (non-specific symptoms included known symptoms of hypercalcemia: bone pain, constipation, abdominal pain, and neurocognitive symptoms), preoperative localization by imaging (technetium-99 sestamibi scan, ultrasound, computed tomography [CT] scan, or magnetic resonance imaging [MRI]), operative approach (MIP or bilateral neck exploration), intraoperative findings (gland location, intraoperative PTH monitoring [IOPTH]), and surgical pathology (gland size, gland mass, final histopathologic diagnosis).
Definitions
Sporadic PHPT was defined as PHPT in the absence of a diagnosis of MEN1 or MEN2A; MIP was defined as directed unilateral exploration via a 2–3 cm incision; bilateral neck exploration was defined as bilateral cervical exploration with the goal of identification of all four parathyroid glands; MGD was defined as more than one parathyroid gland being abnormal, and included both double adenoma and four-gland hyperplasia; and cure was defined as eucalcemia on 6-month postoperative follow-up.
Statistical Analysis
For cohort analysis, patients were divided into Group A (18–40 years of age) and Group B (> 40 years of age), based on the age criteria for current MEN screening recommendations. Statistical analysis was performed using STATA/IC 12.1 software (StataCorp LLC, College Station, TX, USA). Group comparisons were made using the Chi-square test, Student’s t-test, Fisher’s exact test, or Wilcoxon rank-sum test, as appropriate. Data were reported as mean with standard deviation (SD) for normally distributed continuous variables, median with interquartile range (IQR) for non-normally distributed continuous variables, or percentages for dichotomous categorical variables. Subgroup analysis was performed on patients with sporadic PHPT. The primary outcome was MGD on final surgical pathology, while the secondary outcome was cure. A p-value ≤ 0.05 was considered significant. Factors reaching nominal significance (p ≤ 0.20) in univariable logistic regression analysis were incorporated into a multivariable logistic regression model to identify factors independently associated with MGD.
Institutional Review Board approval for this study was obtained from the University of Pennsylvania (protocol #819382).
Results
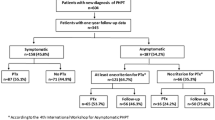
Characteristics of All Patients with Primary Hyperparathyroidism (PHPT)
Of 5152 consecutive parathyroidectomies performed, 3889 patients with PHPT were included in the study (Table 1), with a mean age of 59.0 years (SD 13.0). The population had marked female predominance (77.1% female vs. 22.9% male), with a female to male ratio of 3.4:1. The median preoperative serum calcium level was 10.8 mg/dL (IQR 10.4–11.2) and the median PTH was 86.5 pg/mL (IQR 53.8–124). The majority of patients (67.1%) reported non-specific symptoms of hypercalcemia; 53.7% were found to have loss of bone mineral density by DXA scan, and 16.9% experienced nephrolithiasis. 760 (19.7%) patients in this larger cohort were found to have MGD on final pathology. Median follow-up time after surgery was 6 months (IQR 2–20).
Characteristics of PHPT Patients, by Age Group
To evaluate the profile of young adult patients with PHPT, the study population was divided into Group A (18–40 years of age) and Group B (> 40 years of age). Group A consisted of 352 patients (9.1%), while Group B included 3537 patients (90.9%). The mean age for Group A was 32.4 years (SD 5.9), and 61.7 years (SD 10.2) for Group B. On cohort comparison of patient characteristics, Group A had a greater proportion of male patients (36.4 vs. 21.5%, p < 0.001) compared with Group B; the female to male ratio was 1.8:1 in Group A versus 3.6:1 in Group B. Younger patients were more likely to have a positive family history of PHPT (7.1 vs. 1.3%, p < 0.001), as well as higher rates of MEN (8.2 vs. 0.7%, p < 0.001). Younger patients were also more likely to have undergone a prior parathyroidectomy (9.1 vs. 5.0%, p = 0.001).
Analysis of preoperative signs and symptoms demonstrated higher rates of nephrolithiasis in Group A (22.2 vs. 16.3%, p = 0.020), and Group A also had lower rates of non-specific symptoms (56.0 vs. 68.2%, p < 0.001). Rates of bone demineralization were lower in younger patients (19.6 vs. 57.1%, p < 0.001) consistent with increasing prevalence of osteoporosis with aging. Patients in Group A were less likely to have had a DXA scan performed (34.1 vs. 75.0%, p < 0.001) prior to surgical evaluation.
Comparison of biochemical data between groups was significant for higher median 24-h urinary calcium level (320 vs. 280 mg, p = 0.006) in younger patients; there was no difference in median serum calcium (10.8 vs. 10.8 mg/dL, p < 0.001) or serum PTH levels (85 vs. 87 pg/mL, p = 0.006) between the cohorts. Younger patients had lower rates of successful preoperative localization of affected gland(s) by imaging (51.3 vs. 59.7%, p = 0.002), which was notable for ultrasound (30.7 vs. 35.4%, p = 0.079) but not for sestamibi scan (59.9 vs. 59.7, p = 0.941). Intraoperative findings were not significant for a greater incidence of ectopic gland location in Group A (12.3 vs. 10.2%, p = 0.213). However, young patients were more likely to undergo bilateral neck exploration (78.9 vs. 73.9%, p = 0.044). On final surgical pathology, patients in Group A had lower rates of single adenoma (73.8 vs. 77.9%, p < 0.001), and higher rates of hyperplasia (14.3 vs. 10.3%, p < 0.001). Rates of MGD were similar between both groups (20.4 vs. 19.6%, p < 0.001). The dominant excised gland was smaller in young patients by both median size (1.4 vs. 1.5 cm, p = 0.078) and mass (300 vs. 373 mg, p = 0.682). Negative exploration rates were low (5.8 and 2.4%) and cure rates were high (94.3 and 96.8%), in younger and older patients, respectively.
Characteristics of Multiple Endocrine Neoplasia Patients
We analyzed our population to determine the prevalence of familial endocrinopathies. We identified 53 patients with confirmed diagnoses of MEN (MEN1, n = 48; MEN2A, n = 5) (Table 2). As has been previously described in the literature, these patients were characterized by a young age at presentation (MEN1: median 39.5 years and mean 42.9 years; MEN2A: median 34 years and mean 33.4 years). The majority (76.6%) of patients with MEN1 had hyperplasia on surgical pathology, while the majority of patients with MEN2A were found to have single adenomas (75.0%). Cure rates were 90.2% in MEN1 patients and 100% in MEN2A patients.
Characteristics of Patients with Sporadic PHPT
To determine whether the differences between younger and older patients was due to the disproportionate representation of genetic syndromes in young patients, we performed a subgroup analysis of patients with sporadic PHPT. The 53 patients with MEN described above were excluded, leaving patients with presumed sporadic PHPT. Cohort comparison was performed by age group (Table 3).
The exclusion of MEN patients obviated the statistically significant differences between younger and older patients in rates of prior parathyroidectomy (4.7 vs. 4.7%, p = 0.992), bilateral neck exploration (77.0 vs. 73.8%, p = 0.224), ectopic gland location (12.8 vs. 10.2%, p = 0.145), single adenoma (78.3 vs. 78.4%, p = 0.001), hyperplasia (9.2 vs. 9.9%, p = 0.001), median size of the dominant gland (1.4 vs. 1.5 cm, p = 0.197), and cure rates (95.2 vs. 96.8%, p = 0.377). Median serum PTH became statistically, but not clinically, significantly different between age groups (83 vs. 87 pg/mL, p = 0.007).
Exclusion of patients with MEN did not change the statistically significant difference between groups in terms of male sex (35.4 vs. 22.6%, p < 0.001), family history of hyperparathyroidism (3.1 vs. 1.0%, p = 0.001), median 24-h urinary calcium (320 vs. 280 mg, p = 0.007), bone demineralization (20.2 vs. 57.3%, p < 0.001), non-specific symptoms (56.5 vs. 68.2%, p < 0.001), localization by all imaging (51.6 vs. 59.7%, p = 0.005), or by ultrasound (29.8 vs. 35.4, p = 0.045) and rates of negative exploration (6.1 vs. 2.4%, p = 0.001) between younger and older patients, respectively. Rates of localization by sestambi scan (58.1 vs. 59.5%, p = 0.611) and median mass of dominant excised gland (324.5 vs. 373 mg, p = 0.915) remained similar between groups.
Factors Associated with Increased Risk of MGD
Multivariate logistic regression analysis was performed to identify preoperative factors that conferred increased risk of MGD versus single-gland disease (Table 4) in both the total population of PHPT patients and the subgroup of sporadic PHPT patients. For the entire population with PHPT, MEN conferred the greatest risk of MGD (OR 6.3, 95% CI 3.1–12.7). Other significant risk factors included male sex (OR 1.3, 95% CI 1.0–1.5), a positive family history of PHPT (OR 2.7, 95% CI 1.6–4.8), history of prior parathyroidectomy (OR 2.2, 95% CI 1.6–-3.0), and non-localization by imaging (OR 1.8, 95% CI 1.5–2.1). By univariate and multivariate analysis, younger age was not associated with higher rates of MGD.
In the sporadic PHPT cohort, a positive family history of PHPT in the absence of MEN was associated with the highest risk of MGD (OR 4.0, 95% CI 2.2–7.3). Male sex (OR 1.3, 95% CI 1.0–1.6), prior parathyroidectomy (OR 2.2, 95% CI 1.6–3.0), and non-localization by imaging (OR 1.7, 95% CI 1.5–2.1) also remained significant. Patients with none of these risk factors (n = 1642) had a 14.9% incidence of MGD; one risk factor (n = 2191) increased the rate to 21.7%, two risk factors (n = 424) increased the rate to 25.7%, and three risk factors (n = 24) increased the rate to 33.3% (Fig. 1). To eliminate potential confounding from patients with prior parathyroidectomy, subset analysis was performed in patients undergoing initial parathyroidectomy, and excluding subjects with prior parathyroidectomy. On multivariate regression, we found that a positive family history of PHPT remained associated with the highest risk of MGD (OR 3.8, 95% CI 2.0–7.1). Male sex (OR 1.3, 95% CI 1.0–1.6) and non-localization by imaging (OR 1.8, 95% CI 1.5–2.2) also remained significant.
To investigate the relationship between young age and heritable germline mutations, a subgroup analysis was performed in patients < 30 years of age (n = 121). We found that a diagnosis of MEN syndrome was the only significant risk factor for MGD among all patients with PHPT (OR 39.5, 95% CI 4.3–361). Male sex, positive family history, prior parathyroidectomy, and non-localization by imaging were no longer significant. Among patients < 30 years of age with sporadic hyperparathyroidism (n = 14; i.e. excluding those with a history of MEN), male sex, prior parathyroidectomy, and non-localization by imaging were not associated with an increased risk of MGD.
Impact of a Positive Family History of PHPT
We sought to further determine the impact of a positive family history in sporadic PHPT. Subgroup analysis of patients with a positive family history demonstrated high rates of MGD in both young patients (40 vs. 14.4%, p = 0.524) and older patients (51.3 vs. 18.8%, p = 0.057) compared with corresponding age groups without a family history, although this did not reach statistical significance. Rates of bilateral neck exploration were high in the setting of a family history in both young patients (100% vs. 76.2%, p = 0.205) and older patients (85.7 vs. 73.7%, p = 0.339), although these results were not significantly different between groups.
Discussion
This is the largest published series to analyze the profile of familial and sporadic PHPT in young adults and to identify independent predictors of MGD.
Adult PHPT typically afflicts women in the fifth or sixth decade of life; the female to male ratio was 2.8:1 in patients with sporadic PHPT.10 The literature on sex ratios in young patients is mixed due to inconsistent use of age ranges and the inclusion of patients with genetic syndromes. A slight male predominance (female to male ratio approximately 0.9:1) has been identified in pediatric patient populations with PHPT;2,3,4,11 this literature is inclusive of cases of neonatal hyperparathyroidism and other inherited disorders that have no sex predilection. The slightly higher proportion of affected males observed may reflect the small number of published cases. Large studies of sporadic PHPT in adolescent and young adult patients have found a sex distribution midway between published rates for the pediatric and geriatric populations. One review summarizing 230 published cases of PHPT in patients < 20 years of age found a moderate female predominance of 1.3:1.7 Studies specifically analyzing patients under the age of 40 years have demonstrated comparably high proportions of male patients.12,13 A contemporary analysis of the National Inpatient Sample database found a female to male ratio ranging from 1.17 to 1.83 for patients under age 40 years.10 Our data were consistent with these findings, with a female to male ratio of 1.8:1 in PHPT patients 18–40 years of age, and a 3.6:1 ratio in patients older than 40 years of age. These ratios remained unchanged after exclusion of patients with known inherited endocrinopathies. On multivariate analysis of predictors of MGD, male sex was independently associated with higher rates of MGD in both the total population of PHPT and in sporadic PHPT.
In our study cohort, signs and symptoms of PHPT differed based on age. Younger patients reported lower rates of non-specific symptoms, and had lower rates of bone mineral density loss but higher rates of nephrolithiasis compared with older patients. Prior studies have identified high rates of nephrolithiasis and nephrocalcinosis in pediatric and adolescent populations, compared with the overall population of PHPT patients.7 The relatively elevated incidence of end-organ disease may reflect a delay in diagnosis due to low utilization of routine screening serum chemistries in children. An analogous phenomenon has been well-documented in the changing epidemiology of adult PHPT. Historically, < 20% of adult patients were asymptomatic at diagnosis, with 51–57% experiencing nephrolithiasis, 36% with hypercalciuria, and 10–23% with overt skeletal disease.14 With the introduction of multichannel analysis and automated serum calcium levels in the 1970s, both the incidence of PHPT and the proportion of asymptomatic patients rose dramatically. Today, the majority of adult PHPT patients are identified on routine blood testing and up to 95% of patients are asymptomatic at the time of diagnosis.15
Conflicting literature exists on symptom profiles of adult patients aged 40 years or younger. Consistent with our study, Sneider et al. found higher rates of nephrolithiasis but lower rates of bone pain in young patients.13 Joshua et al. found no statistically significant difference in renal, musculoskeletal, or neurocognitive symptoms between younger and older patients.12 Adam et al. noted higher rates of symptoms in younger patients, but did not differentiate based on organ systems.16 In our study, we identified significantly higher rates of nephrolithiasis in young patients, and young patients were less likely to present with non-specific symptoms or bone demineralization. This may reflect overall better bone mineral density in young patients, or alternatively, may reflect ascertainment bias as fewer young patients underwent DXA scan.
Some series have found lower rates of successful preoperative localization in pediatric populations compared with adults.17 In our patient population, we found lower rates of successful localization by imaging in young patients with PHPT. Non-localization by imaging was an independent risk factor for MGD on multivariate analysis of both PHPT and sporadic PHPT. This finding is consistent with prior studies that have identified a 31% incidence of MGD in patients with negative preoperative imaging studies compared with patients with one positive imaging study (3.6%) or patients with two concordant imaging studies (0%).18 Interestingly, Joshua et al. found that ultrasound was more sensitive than sestamibi (96 vs. 57%, p < 0.05) in patients 40 years of age or younger, and attributed this to lower rates of thyroid pathology to obstruct sonographic imaging of the parathyroid glands.12 We found that although sestamibi was markedly less likely to localize successfully in young patients, more young patients had localizing sestamibi scans than ultrasound studies.
In our population of all patients with PHPT, a known diagnosis of MEN was the strongest predictor of MGD on multivariate analysis. This is consistent with published literature identifying higher rates of MGD in patients with inherited endocrinopathies.19,20 In our population of patients with presumed sporadic PHPT, a positive family history of PHPT was associated with increased incidence of MGD, with an odds ratio of 4.0. Although patients with MEN1 and MEN2A were excluded from the study population, it is possible that our analysis included people with undiagnosed inherited disorders. One large study identified undiagnosed MEN1 in 1.6% of patients presenting for surgical evaluation of PHPT.21 Another rare cause of PHPT is Familial Isolated Primary Hyperparathyroidism (FIHP), defined as inherited PHPT in the absence of other endocrinopathies. FIHP is a clinical diagnosis and is not associated with a single genetic abnormality, although mutations in the MEN1 gene have been identified in some FIHP kindreds.22 Like MEN, FIHP is associated with high rates of MGD;23 the exact incidence of FIHP is difficult to quantify as it has primarily been reported in small series. Because of the diagnostic uncertainty, FIHP was not captured in our dataset and therefore was not excluded from the study population. Given the large number of young patients with a positive family history in our cohort of young patients with sporadic PHPT, it seems unlikely that undiagnosed MEN or FIHP accounts entirely for the higher incidence of MGD in this population. Our results suggest that a positive family history of PHPT may confer an increased risk of MGD even in the absence of known genetic syndromes.
Our data suggest that patients aged 40 years or younger with a positive family history of PHPT may have a 40% rate of MGD. This finding is consistent with prior observations from the Mayo Clinic. In 1997, Barry et al. noted a high prevalence of MGD (70%) as well as recurrent or persistent disease (43%) in ‘familial hyperparathyroidism’, defined as patients with one or more first-degree relatives with PHPT in the absence of MEN.24 Their recommendation was for routine subtotal parathyroidectomy and transcervical thymectomy in all ‘familial’ patients. This approach incurs an elevated risk of hypocalcemia; in patients with high suspicion for MGD, we favor bilateral neck exploration with identification and excision of all affected gland(s). We suggest that young adult PHPT patients with a family history of PHPT should be counseled on their elevated risk of MGD. Testing for genetic susceptibility syndromes should be performed as clinically indicated. This population may benefit from routine bilateral neck exploration performed by an experienced endocrine surgeon; patients with double adenoma should undergo resection of the abnormal glands, while patients with four-gland hyperplasia should undergo debulking surgery with selective three-gland resection or subtotal parathyroidectomy. In contrast, young adult patients without a family history of PHPT do not appear to have higher rates of MGD and may be managed similarly to older adult patients.
Conclusions
In our population, young patients with PHPT did not have increased risk of MGD. However, even in the absence of a known inherited susceptibility gene, young adult patients with a family history of PHPT had a higher incidence of MGD. Age alone in the absence of a positive family history should not determine the need for bilateral neck exploration or subtotal parathyroidectomy. Patients with a positive family history of PHPT in the absence of a genetic syndrome should be counseled regarding their elevated rates of MGD, and may benefit from routine bilateral neck exploration and selective three gland resection or subtotal parathyroidectomy. Additional factors including male sex, prior parathyroidectomy, and non-localization by imaging were associated with increased risk for MGD. Patients with multiple co-occurring risk factors may benefit from counseling.
References
Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol. 2012;33(4):457–68.
Bjernulf A, Hall K, Sjögren I, Werner I. Primary hyperparathyroidism in children. Brief review of the literature and a case report. Acta Paediatr Scand. 1970;59(3):249–58.
Mannix H Jr. Primary hyperparathyroidism in children. Am J Surg. 1975;129(5):528–31.
Girard RM, Belanger A, Hazel B. Primary hyperparathyroidism in children. Can J Surg. 1982;25(1):11–3, 32.
Loh KC, Duh QY, Shoback D, Gee L, Siperstein A, Clark OH. Clinical profile of primary hyperparathyroidism in adolescents and young adults. Clin Endocrinol. 1998;48(4):435–43.
Allo M, Thompson NW, Harness JK, Nishiyama RH. Primary hyperparathyroidism in children, adolescents, and young adults. World J Surg. 1982;6(6):771–6.
Belcher R, Metrailer AM, Bodenner DL, Stack BC Jr. Characterization of hyperparathyroidism in youth and adolescents: a literature review. Int J Pediatr Otorhinolaryngol. 2013;77(3):318–22.
Karges W, Schaaf L, Dralle H, Boehm BO. Concepts for screening and diagnostic follow-up in multiple endocrine neoplasia type 1 (MEN1). Exp Clin Endocrinol Diabetes. 2000;108(5):334–40.
Cupisti K, Raffel A, Dotzenrath C, Krausch M, Röher HD, Schulte KM. Primary hyperparathyroidism in the young age group: particularities of diagnostic and therapeutic schemes. World J Surg. 2004;28(11):1153–6.
Miller BS, Dimick J, Wainess R, Burney RE. Age- and sex-related incidence of surgically treated primary hyperparathyroidism. World J Surg. 2008;32(5):795–9.
Rapaport D, Ziv Y, Rubin M, Huminer D, Dintsman M, Primary hyperparathyroidism in children. J Pediatr Surg. 1986;21(5):395–7.
Joshua B, Feinmesser R, Ulanovski D, Gilat H, Sulkes J, Eshed V, et al. Primary hyperparathyroidism in young adults. Otolaryngol Head Neck Surg. 2004;131(5):628–32.
Sneider MS, Solorzano CC, Montano RE, Anello C, Irvin GL III, Lew JI. Sporadic primary hyperparathyroidism in young individuals: different disease and treatment? J Surg Res. 2009;155(1):100–3.
Fraser WD. Hyperparathyroidism. Lancet. 2009;374(9684):145–58.
Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21(1):171–7.
Adam LA, Smith BJ, Calva-Cerqueira D, Howe JR, Lal G. Role for limited neck exploration in young adults with apparently sporadic primary hyperparathyroidism. World J Surg. 2008;32(7):1518–24.
Lawson ML, Miller SF, Ellis G, Filler RM, Kooh SW. Primary hyperparathyroidism in a paediatric hospital. QJM. 1996;89(12):921–32.
Sebag F, Hubbard JG, Maweja S, Misso C, Tardivet L, Henry JF. Negative preoperative localization studies are highly predictive of multiglandular disease in sporadic primary hyperparathyroidism. Surgery. 2003;134(6):1038–41 (discussion 1041-2).
Kraimps JL, Denizot A, Carnaille B, Henry JF, Proye C, Bacourt F, et al. Primary hyperparathyroidism in multiple endocrine neoplasia type IIa: retrospective French multicentric study. Groupe d’Etude des Tumeurs a Calcitonine (GETC, French Calcitonin Tumors Study Group), French Association of Endocrine Surgeons. World J Surg. 1996;20(7):808–12 (discussion 812-3).
Gertner ME, Kebebew E. Multiple endocrine neoplasia type 2. Curr Treat Options Oncol. 2004;5(4):315–25.
Yip L, Ogilvie JB, Challinor SM, Salata RA, Thull DL, Yim JH, et al. Identification of multiple endocrine neoplasia type 1 in patients with apparent sporadic primary hyperparathyroidism. Surgery. 2008;144(6):1002–6 (discussion 1006-7).
Miedlich S, Lohmann T, Schneyer U, Lamesch P, Paschke R. Familial isolated primary hyperparathyroidism—a multiple endocrine neoplasia type 1 variant? Eur J Endocrinol. 2001;145(2):155–60.
Kandil E, Alabbas HH, Lum YW, Tufaro AP. Familial isolated primary hyperparathyroidism with double adenoma. South Med J. 2010;103(3):236–8.
Barry MK, Van Heerden JA, Grant CS, Thompson GB, Khosla S. Is familial hyperparathyroidism a unique disease? Surgery. 1997;122(6):1028–33.
Acknowledgment
The authors gratefully acknowledge the contributions of Isadora Cerullo, BA, and Jae P. Ermer, BA, to data collection, and Meera Gupta, MD, to data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Julia Gasior, Rachel R. Kelz, Giorgos C. Karakousis, Douglas L. Fraker, and Heather Wachtel have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gasior, J., Kelz, R.R., Karakousis, G.C. et al. Primary Hyperparathyroidism in Young Adult Patients. Ann Surg Oncol 30, 4156–4164 (2023). https://doi.org/10.1245/s10434-023-13344-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13344-3