Abstract
Purpose
Evaluation of the phenotype of primary hyperparathyroidism (PHPT), adherence to International Guidelines for parathyroidectomy (PTx), and rate of surgical cure.
Method
From January 2014–January 2016, we performed a prospective, multicenter study in patients with newly diagnosed PHPT. Biochemical and instrumental data were collected at baseline and during 1-year follow-up.
Results
Over the first year we enrolled 604 patients (age 61 ± 14 years), mostly women (83%), referred for further evaluation and treatment advice. Five hundred sixty-six patients had sporadic PHPT (93.7%, age 63 ± 13 years), the remaining 38 (6.3%, age 41 ± 17 years) had familial PHPT. The majority of patients (59%) were asymptomatic. Surgery was advised in 281 (46.5%). Follow-up data were available in 345 patients. Eighty-seven of 158 (55.1%) symptomatic patients underwent PTx. Sixty-five (53.7%) of 121 asymptomatic patients with at least one criterion for surgery underwent PTx and 56 (46.3%) were followed without surgery. Negative parathyroid imaging studies predicted a conservative approach [symptomatic PHPT: OR 18.0 (95% CI 4.2–81.0) P < 0.001; asymptomatic PHPT: OR 10.8, (95% CI 3.1–37.15) P < 0.001). PTx was also performed in 16 of 66 (25.7%) asymptomatic patients without surgical criteria. Young age, serum calcium concentration, 24 h urinary calcium, positive parathyroid imaging (either ultrasound or MIBI scan positive in 75% vs. 16.7%, P = 0.001) were predictors of parathyroid surgery. Almost all (94%) of patients were cured by PTx.
Conclusions
Italian endocrinologists do not follow guidelines for the management of PHPT. Negative parathyroid imaging studies are strong predictors of a non-surgical approach. PTx is successful in almost all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (PHPT) is a common endocrine disease, characterized by increased serum calcium and high or inappropriately normal serum levels of parathyroid hormone (PTH) [1, 2]. PHPT is prevalent in postmenopausal women and generally due to a single parathyroid adenoma [3]. Clinical presentation of the disease has changed over the last decades in those countries where serum calcium biochemical screening has been introduced. Indeed, in these areas PHPT is commonly diagnosed as an asymptomatic disorder, and a minority of cases are characterized by hypercalcaemic symptoms, nephrolithiasis, bone disease and neuromuscular weakness [4, 5]. Parathyroidectomy (PTx), the only definitive cure for PHPT, should be considered in all patients and recommended in symptomatic patients. The knowledge that even patients with asymptomatic PHPT might experience target organs involvement has led to a long debate about its appropriate management [6, 7]. The discussion about the need for surgery in asymptomatic PHPT was matter of four Workshops in 1990, 2002, 2008 and 2013 [8, 9], which provided internationally accepted guidelines for PTx in patients with asymptomatic PHPT as well as monitoring for those not undergoing surgery. Some important news and recommendations were introduced in the last International Workshop, particularly regarding the evaluation of bone and kidney involvement and the impact on patient’s management [9,10,11,12,13].
Few studies have been focused on the impact of these guidelines on the management of patients with PHPT. In the present study, we prospectively evaluated the phenotype of PHPT in Italy, the adherence to guidelines and the rate of surgical cure.
Materials and methods
Study design
This is a prospective, multicenter study performed in 29 Italian centers for endocrine diseases. Patients with newly diagnosed PHPT in the period January 2014–January 2015 were enrolled and followed for an additional year.
Patients gave their informed consent and the Institutional Review Board of each participating center approved the study.
Patients and data collection
The diagnosis of PHPT was based on elevated ionized or total serum calcium with increased or inappropriately normal intact PTH, according to the normal reference range of each Center.
An ad hoc electronic CRF form was developed and used to record all medical data. The CRF was available online, after registration and login at the web site www.hyperparanet.org. The research was open to all endocrinologists in the whole Italian area.
The following clinical data were collected at the baseline visit: age, gender, age at diagnosis, diagnosis of sporadic or familial PHPT, including diagnosis of multiple endocrine neoplasia (MEN) type 1 (MEN1), 2A (MEN2A) and 4 (MEN4), hyperparathyroidism associated-jaw tumor (HPT-JT), familial isolated hyperparathyroidism (FIHP) and familial hypocalciuric hypercalcemia (FHH). Major PHPT features were also recorded, including (i) hypercalcemic and neuropsychiatric symptoms (ii) symptomatic or asymptomatic nephrolithiasis (iii) osteoporosis (T score < − 2.5 at any skeletal site by DXA according the latest International Guidelines for Osteoporosis [14]) (iv) previous fragility fractures (defined as symptomatic fractures) (v) use of drugs potentially affecting bone metabolism (vi) hypertension and major cerebrovascular events. Finally, data about positive or negative imaging studies (neck ultrasound and/or 99mTc-sestamibi parathyroid scintigraphy), if performed, and information on therapies were also included in the database.
Biochemical serum and urinary data were collected at baseline and at the last follow-up visit for measurement of: albumin-adjusted serum calcium (Alb-Ca), plasma PTH, 25-hydroxyvitamin D [25(OH)D], creatinine, cholesterol, glucose, triglycerides, 24 h urinary calcium excretion.
After the initial evaluation, the therapeutic planning of each patient with PHPT was selected in the electronic CRF, choosing between two options (i) PTx or (ii) surveillance with or without medical treatment. A follow-up information on treatment received and histology, where appropriate, were gathered.
Statistical analysis
Results are expressed as mean ± SD for continuous variables and median (interquartile range) for non-continuous variables. The Student’s t test, and the Mann–Whitney test were used to compare the continuous and non-parametric variables, respectively. The Chi-square test and Fisher’s test were used for comparison of categorical variables, as appropriate. A logistic binary regression model was applied to evaluate if age at diagnosis, Alb-Ca, PTH, 24 h urinary calcium, nephrolithiasis, osteoporosis, fragility fractures and concordant positive parathyroid imaging studies were determinants of the choice of PTx. A P value < 0.05 was considered statistically significant. Statistical analysis was carried out using “SPSS Statistics 17.0.1, Chicago, Illinois, USA” and “R, 3.0.2, Auckland, New Zealand”.
Results
From January 2014 to January 2015, 29 Italian Centers of Endocrinology, equally distributed in Northern, Central and Southern Italy, participated in the study. Clinical, biochemical and instrumental records of 604 patients with a new diagnosis of PHPT were collected on the web site Hyperparanet. Complete clinical, biochemical, instrumental, histological and 1-year follow-up data were available in 345 patients at 18 Centers.
Baseline evaluation of the whole group
The demographic, clinical and biochemical data are summarized in Table 1. The cohort included 604 patients, 502 (83%) females and 102 (17%) males with a female-to-male ratio of 4.9:1. The mean age was 61 ± 14 years, with a percentage of juvenile cases (age ≤ 25 years) of 2.8% (n = 17). In the latter group, the female-to-male ratio was significantly lower than in the whole group (1.4:1, P = 0.009).
Diagnosis of sporadic PHPT was made in 566 (93.7%) patients and familial PHPT in 38 (6.7%), including 23 cases of MEN1, 6 cases of FIHP, 3 cases of HPT-JT and 6 cases of FHH. MEN1 gene mutation data were available in 24 cases and mutations were identified in 20.
At least one of the following features was present in 246 (40.7%) patients: (i) nephrolithiasis either symptomatic or asymptomatic (i.e., discovered at ultrasound evaluation at the initial workout) (n = 177, 29.1%); (ii) clinical fragility fractures (n = 70, 11.6%); (iii) symptoms of hypercalcemia (n = 34, 5.6%) as nausea, vomiting and constipation; for the purpose of the present study these patients were classified as “symptomatic PHPT”. The remaining 358 (59.3%) patients were asymptomatic. Osteoporosis was detected in 264 (43.7%) of patients and defined according to the last International Guidelines for Osteoporosis [14]. A history of hypertension or prior major cerebrovascular events was present in 178 (29.5%) and 9 (1.5%) patients, respectively.
After the initial evaluation, PTx was recommended in 281 (46.5%) patients, namely 180 of the 246 (73%) symptomatic and 101 of the 358 (28%) asymptomatic patients.
Patients with available follow-up
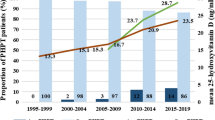
One-year follow-up data were available in 345 patients from 18 Centers which participated the second part of the study (Fig. 1) 289 (83.8%) females and 56 (16.2%) males (F:M = 5.2:1), with a mean age of 63 ± 13 years. One hundred fifty-eight (45.8%) patients had nephrolithiasis, clinical fragility fractures and/or symptoms of hypercalcemia and 187 (54.2%) were asymptomatic PHPT. The majority of patients (n = 331, 95.9%) had sporadic PHPT, and the remaining 14 familial PHPT, including MEN1 (n = 8), FIHP (n = 4), HPT-JT (n = 1) and FHH (n = 1).
In the whole group, osteoporosis was found in 152 (44.1%) patients and 44 (12.7%) patients complained of neuropsychiatric symptoms (fatigue, depression, agitation, apathy, lack of concentration) upon questioning. A history of hypertension or prior major cerebrovascular events was present in 104 (30.1%) and 5 (1.4%) patients, respectively.
Biochemical data at the baseline visit are reported in Table 1. The characteristics of these patients are similar to those of the entire cohort of 604 patients, with the exception of 24 h urinary calcium and serum 25OHD concentration which were lower, and the rate of nephrolithiasis that was higher (Table 1).
PTx was performed in 87 (55.1%) of 158 patients with symptomatic PHPT, the majority (n = 71, 82.6%) of them had nephrolithiasis (Fig. 1). Interestingly, despite the general consensus that patients with symptomatic PHPT should undergo surgery, this treatment was not performed in the remaining 71 (44.9%) patients. To understand why surgery was not performed, we compared patients who underwent PTx and those who did not. We found that the former (PTx), compared to the latter (no PTx), were younger and had significantly higher mean Alb-Ca, plasma PTH, 24 h urinary calcium and rate of nephrolithiasis, but a lower rate of fragility fractures (Table 2A).
In the remaining 187 patients with asymptomatic PHPT, PTx was advised based on the 2013 guidelines in 121 (64.7%), who met at least one criterion for PTx, but surgery was performed only in 65 (53.7%) of them. Criteria for PTX in the latter group were as follows: serum calcium levels 1 mg above the upper limit of normal range (n = 37, 56.9%), osteoporosis (n = 35, 53.8%), age < 50 years (n = 14, 21.5%), 24-h urinary calcium > 400 mg (n = 14, 21.5%). PTx was not performed in the remaining 56 (46.3%) patients, who, compared with patients who did surgery, had a significantly lower rate of serum calcium levels 1 mg above the upper limit of normal range (Table 2B).
PTx group
A total of 279 patients (237 females and 42 males, 158 with symptomatic and 121 with asymptomatic PHPT) had indications for PTx, but surgery was not performed in 127 (45.5%, 71 with symptomatic and 56 with asymptomatic PHPT). The latter patients were older and had a significantly lower mean Alb-Ca, plasma PTH, 24 h urinary calcium and rate of nephrolithiasis, but a higher rate of fragility fractures (Table 2C). It could be hypothesized that in a given patient the decision of not performing surgery was only based upon the above parameters. Interestingly, we found that parathyroid imaging studies were performed in a large proportion of patients [one imaging exam in 251/279 (89.9%) and either ultrasound and MIBI scan in 124/279 (69.3%)] at the initial workout, independently of the therapeutic plan, i.e., PTx or no PTx. Therefore, the question arises as to whether the results of parathyroid imaging studies might have had a role in the decision-making process. To evaluate this hypothesis a multivariate analysis that included also the results of parathyroid imaging studies was performed in the whole group of patients with indications for surgery. The analysis showed that older age, lower Alb-Ca and, particularly, a higher rate of negative parathyroid imaging studies [concordant negative ultrasound and MIBI scan (OR 11.8 95% CI 5.1–27.2, P < 0.0001) were independent predictors for the choice of not performing PTx (Table 3). A concordant negative result of parathyroid imaging studies was also a strong predictor of a conservative approach in the subgroups of patients with either symptomatic [OR 18.0 (95% CI 4.2–81.0) P < 0.001] or asymptomatic [OR 10.821, (95% CI3.1–37.15) P < 0.001)] PHPT (Table 3). We cannot exclude that patient’s refusal and comorbidities also accounted for the decision of not undergoing PTx, but unfortunately participants did not report details on this matter.
PTx was also performed in 16 (25.7%) of 66 patients who did not meet the criteria for surgery. These patients, compared with those who did not undergo surgery, were younger (63 ± 8 vs 69 ± 8 P = 0.012), had higher Alb-Ca concentration (10.5 ± 0.6 vs 9.9 ± 1.3, P = 0.012), 24-h urinary calcium (427 ± 319 vs 201 ± 117, P = 0.04), and rate of positive parathyroid imaging (either ultrasound or MIBI in 75% vs 16.7%, P = 0.001).
A total of 168 patients underwent PTx, 164/331 with sporadic and 4/14 with familial PHPT. In the former group, the histological diagnosis was a single adenoma in 148 cases (90.3%), double adenoma in 6 (3.7%), atypical adenoma in 2 (1.2%), hyperplasia in 5 (3.0%), and carcinoma in 3 (1.8%). In the familial group, a single adenoma was found in one patient with FIHP, hyperplasia in two with MEN1, and carcinoma in one with HPT-JT.
The large majority (n = 158, 94.0%) of patients were cured by PTx. Persistence of PHPT was observed in the remaining 10 patients with apparently sporadic PHPT, in whom the parathyroid histology showed a single adenoma in 7, hyperplasia in 2, and a double adenoma in one.
No-PTx group
The whole group of 177 patients (71 with symptomatic and 106 asymptomatic PHPT) followed without surgery showed a stable clinical and biochemical disease during the 1-year follow-up. Indeed, there was no statistically significant difference between baseline and last visit evaluation in Alb-Ca, PTH, 25(OH)D and 24 h urinary calcium (Table 4). Fourteen patients were treated with cinacalcet and 37 with bisphosphonates.
Discussion
This multicenter study was aimed to evaluate the phenotype of newly diagnosed PHPT in Italy, the adherence to the 2013 International Guidelines for the management of asymptomatic PHPT and the rate of surgical cure of PHPT.
PHPT was more frequent in females than males (M/F = 4.9:1), and most common in the 5th–6th decades of life, confirming the finding of a large (n = 360) retrospective single-center Italian survey [15]. On the other hand, data retrieved from the “Record of Hospital Discharge” between 2006 and 2011 in 46,275 Italian patients under the code “PHPT-related diagnoses and surgical procedures” showed a lower female–male ratio (2.2:1) [16]. It is of note that, under the above code, conditions other than PHPT could have been included, namely “non-tumor-related hypercalcemia”, “not-specified hyperparathyroidism” and “other PTx”, thus making this cohort not completely comparable with our series. In agreement with our data studies carried out in the USA and Brazil report a female-to-male ratio of 3–4:1 [17, 18].
The clinical presentation of PHPT is highly variable all over the world. In industrialized countries, where automatic biochemical screening is routinely available, the disease is mainly asymptomatic and relevant bone and stone manifestations are unusual. In the present study, the majority of patients (54.2%) were asymptomatic, a percentage that is similar to that (47.8%) reported by Castellano et al. in their retrospective study [15] and by Trombetti et al. (57%) in the prospective Swiss PHPT Cohort Study [19]. In USA, the rate of asymptomatic disease is even higher (80%) [3], while in other countries, like India or China, is very low (around 20%) [20].
In the literature, the terms “mild” and “asymptomatic” are often used as synonymous, but not necessarily the latter patients with asymptomatic PHPT have a mild disease, since they may present moderate hypercalcemia, kidney stones, vertebral fractures accidentally discovered during evaluation, and osteoporosis. To overcome this issue, a recent consensus statement of Italian Society of Endocrinology recommends to define as “mild” patients with asymptomatic PHPT without surgical criteria [21].
Recent studies have shown that, despite the change in the clinical profile of PHPT in Western Countries to a less severe disease, nephrolithiasis remains one of the features of classic PHPT in the modern cohorts. In the present study, we found an overall rate of nephrolithiasis of 29.1%, definitely lower than that (55%) reported in an Italian single-center study [22], but similar to the rate reported in the Swiss population (17%) [19]. The latter study also reported renal stones detected at ultrasound in 35% of patients with asymptomatic PHPT, a figure markedly higher than that (11.3%) reported by Castellano et al. in a retrospective study [23]. Unfortunately, in the present study the electronic CRF was not designed for differentiating silent from symptomatic kidney stones, or for evaluation of the urinary stone risk profile [9].
One of the major aim was to evaluate the adherence of Italian endocrinologists, who were directly involved in the decision-making process in this survey, to the international guidelines for the management of symptomatic and asymptomatic PHPT. Despite the availability of such guidelines since 1991, as well as positions statements of the two major Italian endocrine societies [24] with similar indications, we found that only about half of either symptomatic or asymptomatic patients who met the criteria for PTx underwent surgery. Our data confirm that there is still a suboptimal adherence to the guidelines, both in USA and Europe. Sharata et al., in a retrospective chart-review of 350 primary care clinicians in Oregon, USA, over the period 2009–2011, identified 124 patients with PHPT with no history of prior PTx. PTx was performed in 26/76 (34%) of patients who met criteria for surgery, either because symptomatic or asymptomatic with at least one criterion according to the 2013 guidelines, and in 12/48 (25%) who did not meet surgical criteria. In about half of cases endocrinologists participated in the treatment choice of most primary care physicians. Young age hypercalciuria and particularly history of nephrolithiasis were associated with surgery [25]. Yeh et al. identified from the Southern California Kaiser-Permanente Laboratory Management System Patient Database 3388 patients with all the following laboratory values: serum PTH > 65 pg/mL, serum calcium > 10.5 and serum creatinine > 2.5 mg/dl between1995 and 2008. PTx was performed in 134 (50.6%) of 265 patients with symptomatic PHPT (nephrolithiasis) and in 830 (26.6%) of 3123 with asymptomatic PHPT. Of the remaining 3123 with asymptomatic PHPT 569 of 1362 (41.8%) of those who met the Consensus criteria for PTx and 469 of the 1761 (26.6%) who did not were submitted to surgery. Serum calcium > 11.5 mg/dL, 24 h urinary calcium excretion ≥ 400 mg and age > 50 years were predictive of PTx [26]. Finally, even in the Swiss PHPT population, the guidelines adherence was similar to our results. Indeed, authors evaluated 332 patients, 143 (43%) with symptomatic disease and 189 (57%) with asymptomatic and PTx was performed only in 71/143 (49.6%) symptomatic patients and in 82/131 (62.3%) asymptomatic patients with at least one criterion for PTx [19].
In an attempt to understand why the Italian endocrinologists did not advise PTx in about half of patients who met the current guidelines for surgery, either symptomatic or asymptomatic, we evaluated the role of all variables in the decision-making process. The finding of negative parathyroid imaging studies (concordant negative ultrasound and MIBI scan) strongly predicted the conservative approach. Older age and lower serum calcium concentrations were also independent predictors, but with a lower weight. A relevant role of negative parathyroid imaging studies in not advising PTx in patients with PHPT who met surgical criteria was reported by two recent European studies, both based upon questionnaire-based surveys. Villar del Moral et al. found that 11% of institutions considered PTx contraindicated in patients with asymptomatic PHPT and negative parathyroid imaging studies [27]. A similar attitude was adopted by 15% of Spanish Hospital Endocrinology services [28]. It is noteworthy that international guidelines clearly suggest that negative imaging should not inhibit to refer the patient to an experienced parathyroid surgeon, available in Endocrinology third levels centers [13]. Moreover, it was recently demonstrated that preoperative negative imaging is not associated with a decreased surgical cure rate for PHPT in a large population (2185 patients) [29].
As stated by the International Guidelines and the Italian Consensus, PTx should be considered in all patients with asymptomatic PHPT, including those who did not meet the surgical criteria. In this regard it is worth noting that prior randomized clinical trials have shown an improvement in BMD and neuropsychiatric symptoms in those patients who underwent PTx, compared with those who did not PTx [30,31,32]. Of note in our study, 16 of 66 patients without surgical criteria underwent surgery, and interestingly, the majority of them had positive parathyroid imaging studies, likely accounted for recommending PTx in patients who did not meet the surgical criteria. In the study of Trombetti et al. 11/59 patients without PTx criteria underwent surgery; mainly for the severe neuropsychological complains. Unfortunately, they had no data on parathyroid imaging [19].
PTx was successful in almost all patients (94%) and this is in line with the results of a recent meta-analysis, which included 82 observational and 6 randomized studies and found a final cure rate of 97–98% [33] and with the prospective swiss study (97%) [19].
Persistence of PHPT was observed in 10/168 (6.0%) cases. The persistence of PHPT ranges between 2 and 22% when considering all cases of PHPT [34] and 2.5–5%, when considering sporadic PHPT [35, 36]. Interestingly, all these patients had apparently sporadic PHPT, but 3 had a multiglandular disease at the histology: (2 hyperplasia and 1 double adenoma). Accordingly to other studies, hyperplasia and double adenoma are associated with a significantly higher rate of persistence compared to single adenoma [34]. We cannot exclude that these 3 patients might be familial cases with insufficient family history information or “de novo” cases of familial forms of PHPT.
Fourteen patients had hereditary PHPT, and only 4 of them underwent PTx during the 1-year follow-up. This conservative approach in the hereditary forms of PHPT likely depends upon the higher rate of persistence/recurrence compared with sporadic PHPT, unless an extensive surgery, which is associated with a higher risk of complications, is performed. In this regard, Udelsman et al. underline that the surgical approach in hereditary PHPT should aim to achieve normocalcemia for as long as possible, minimizing complications. In this regard the patient’s desire and the surgeon’s experience, rather that the guidelines for surgery could influence the therapeutic decision [13]. Interestingly all 4 patients undergoing PTx were normocalcemic after surgery, even if the 1-year follow-up is too short to consider them cured.
The strengths of the study are: (i) its prospective nature; (ii) the inclusion of a large number of Italian Centers equally distributed in the Country; (iii) the rather complete clinical, biochemical, instrumental data at baseline, and (iv) the 1-year follow-up data after PTx or surveillance.
This study also has some limitations: (i) 11 out 29 centers did not participate in the 1-year follow-up study; (ii) all centers were third level referral centers, (iii) the short follow-up, (iv) the lack of the intra and inter-assay coefficient of variation between the different centers is also a limit for biochemical analyses and densitometric data.
In conclusion, the present study indicates that Italian endocrinologists working in tertiary referral centers do not follow international guidelines for the management of PHPT. Parathyroid imaging studies are very often performed in the initial patient’s workout and negative findings are strong predictors of a non-surgical approach. PTx is successful in almost all patients.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Marcocci C, Cetani F (2011) Clinical practice. Primary hyperparathyroidism. N Engl J Med 365:2389–2397. https://doi.org/10.1056/NEJMcp1106636
Bilezikian JP, Bandeira L, Khan A, Cusano NE (2017) Hyperparathyroidism. Lancet. https://doi.org/10.1016/S0140-6736(17)31430-7
Bandeira L, Bilezikian J (2016) Primary hyperparathyroidism. F1000Research. https://doi.org/10.12688/f1000research.7039.1
Mihai R, Wass JA, Sadler GP (2008) Asymptomatic hyperparathyroidism–need for multicentre studies. Clin Endocrinol 68:155–164. https://doi.org/10.1111/j.1365-2265.2007.02970.x
Albright F (1948) A page out of the history of hyperparathyroidism. J Clin Endocrinol Metab 8:637–657. https://doi.org/10.1210/jcem-8-8-637
Silverberg SJ, Shane E, Jacobs TP et al (1999) A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med 341:1249–1255. https://doi.org/10.1056/NEJM199910213411701
Rubin MR, Bilezikian JP, McMahon DJ et al (2008) The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 93:3462–3470. https://doi.org/10.1210/jc.2007-1215
Bilezikian JP, Khan AA, Potts JT, Hyperthyroidism on B of the TIW on the M of AP (2009) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol 94:335–339. https://doi.org/10.1210/jc.2014-1413
Bilezikian JP, Brandi ML, Eastell R et al (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab 99:3561–3569. https://doi.org/10.1210/jc.2014-1413
Silverberg SJ, Clarke BL, Peacock M et al (2014) Current issues in the presentation of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab 99:3580–3594. https://doi.org/10.1210/jc.2014-1415
Marcocci C, Bollerslev J, Khan AA, Shoback DM (2014) Medical management of primary hyperparathyroidism: proceedings of the fourth international workshop on the management of asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab 99:3607–3618. https://doi.org/10.1210/jc.2014-1417
Eastell R, Brandi ML, Costa AG et al (2014) Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab 99:3570–3579. https://doi.org/10.1210/jc.2014-1414
Udelsman R, Akerström G, Biagini C et al (2014) The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab 99:3595–3606. https://doi.org/10.1210/jc.2014-2000
Kanis JA, McCloskey EV, Johansson H et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57. https://doi.org/10.1007/s00198-012-2074-y
Castellano E, Tassone F, Attanasio R et al (2016) Mild primary hyperparathyroidism as defined in the Italian Society of Endocrinology’s Consensus Statement: prevalence and clinical features. J Endocrinol Invest 39:349–354. https://doi.org/10.1007/s40618-015-0412-6
Cipriani C, Carnevale V, Biamonte F et al (2014) Hospital care for primary hyperparathyroidism in Italy: a 6-year register-based study. Eur J Endocrinol 171:481–487. https://doi.org/10.1530/EJE-14-0493
Wermers RA, Khosla S, Atkinson EJ et al (2005) Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res 21:171–177. https://doi.org/10.1359/JBMR.050910
Oliveira UEM, Ohe MN, Santos RO et al (2007) Analysis of the diagnostic presentation profile, parathyroidectomy indication and bone mineral density follow-up of Brazilian patients with primary hyperparathyroidism. Braz J Med Biol Res 40:519–526. https://doi.org/10.1590/S0100-879X2007000400010
Trombetti A, Christ ER, Henzen C et al (2016) Clinical presentation and management of patients with primary hyperparathyroidism of the Swiss Primary Hyperparathyroidism Cohort: a focus on neuro-behavioral and cognitive symptoms. J Endocrinol Invest 39:567–576. https://doi.org/10.1007/s40618-015-0423-3
Shah VN, Bhadada SK, Bhansali A et al (2014) Changes in clinical & biochemical presentations of primary hyperparathyroidism in India over a period of 20 years. Indian J Med Res 139:694–699
Marcocci C, Brandi ML, Scillitani A et al (2015) Italian Society of Endocrinology Consensus Statement: definition, evaluation and management of patients with mild primary hyperparathyroidism. J Endocrinol Invest 38:577–593. https://doi.org/10.1007/s40618-015-0261-3
Cipriani C, Biamonte F, Costa AG et al (2015) Prevalence of kidney stones and vertebral fractures in primary hyperparathyroidism using imaging technology. J Clin Endocrinol Metab 100:1309–1315. https://doi.org/10.1210/jc.2014-3708
Castellano E, Attanasio R, Latina A et al (2016) Nephrolithiasis in primary hyperparathyroidism: a comparison between silent and symptomatic patients. Endocr Pract 23(2):157–162. https://doi.org/10.4158/EP161476.OR
Zini M, Attanasio R, Cesareo R et al (2012) AME position statement: primary hyperparathyroidism in clinical practice. J Endocrinol Invest 35:2–21
Sharata A, Kelly LT, Rozenfeld Y et al (2017) Management of primary hyperparathyroidism: can we do better? Am Surg 83(1):64–70
Yeh MW, Wiseman JE, Ituarte PHG et al (2012) Surgery for primary hyperparathyroidism. Ann Surg 255:1179–1183. https://doi.org/10.1097/SLA.0b013e31824dad7d
Villar-del-Moral J, Capela-Costa J, Jiménez-García A et al (2016) Compliance with recommendations on surgery for primary hyperparathyroidism—from guidelines to real practice: results from an Iberian survey. Langenbeck’s Arch Surg 401:953–963. https://doi.org/10.1007/s00423-015-1362-3
Muñoz Torres M, Jodar Gimeno E, Reyes Garcia R et al (2012) Results from a national survey on the management of primary hyperparathyroidism. J Endocrinol Invest 35:957–963. https://doi.org/10.3275/8184
Wachtel H, Bartlett EK, Kelz RR et al (2014) Primary hyperparathyroidism with negative imaging: a significant clinical problem. Ann Surg 260:474–482. https://doi.org/10.1097/SLA.0000000000000875
Bollerslev J, Jansson S, Mollerup CL et al (2007) Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial. J Clin Endocrinol Metab 92:1687–1692. https://doi.org/10.1210/jc.2006-1836
Rao DS, Phillips ER, Divine GW, Talpos GB (2004) Randomized controlled clinical trial of surgery versus no surgery in patients with mild asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab 89:5415–5422
Walker MD, McMahon DJ, Inabnet WB et al (2009) Neuropsychological features in primary hyperparathyroidism: a prospective study. J Clin Endocrinol Metab 94:1951–1958. https://doi.org/10.1210/jc.2008-2574
Singh Ospina NM, Rodriguez-Gutierrez R, Maraka S et al (2016) Outcomes of parathyroidectomy in patients with primary hyperparathyroidism: a systematic review and meta-analysis. World J Surg 40:2359–2377. https://doi.org/10.1007/s00268-016-3514-1
Alhefdhi A, Schneider DF, Sippel R, Chen H (2014) Recurrent and persistence primary hyperparathyroidism occurs more frequently in patients with double adenomas. J Surg Res 190:198–202. https://doi.org/10.1016/j.jss.2014.02.024
Yeh MW, Wiseman JE, Chu SD et al (2011) Population-level predictors of persistent hyperparathyroidism. Surgery 150(6):1113–1119
Venkat R, Kouniavsky G, Tufano RP et al (2012) Long-term outcome in patients with primary hyperparathyroidism who underwent minimally invasive parathyroidectomy. World J Surg 36:55–60. https://doi.org/10.1007/s00268-011-1344-8
Acknowledgements
The authors are very grateful to the participating patients for their cooperation. We wish to thank Drs Carmela Ostuni, Bari; Massimo Procopio, Torino; Alessandro Piovesan, Torino; Fochesato Elena Maria, Sondrio; Lettina Gabriele, Messina; Turiano Giuseppe, Messina; Roberto Allara, Vercelli; Vanessa Roncoroni, Ancona; Loredana Pagano, Novara; Federico Arecco, Torino; Marchese Lorenzo, Torino; Falcone Yolanda, Torino; Michele Zini, Reggio Emilia; Anna Ciampolillo, Bari; Fabio Ulivieri, Milano; Roberto Attanasio, Milano; Marco Sergio Massarotti, Milano; Andrea Lania, Milano; Valentina Albertino, Milano; Alberto Falchetti, Firenze; Vania Braga, Verona; Rizzato Margerita Treviso for participating in the study. This study has been conducted as part of the research projects of the Mineral and Bone Club of the Italian Society of Endocrinology.
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human research
This study has been approved by the appropriate institutional and/or national research ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Saponaro, F., Cetani, F., Repaci, A. et al. Clinical presentation and management of patients with primary hyperparathyroidism in Italy. J Endocrinol Invest 41, 1339–1348 (2018). https://doi.org/10.1007/s40618-018-0879-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0879-z