Abstract
Background
Primary hyperparathyroidism (1° HPT) is reported most often in women over the age of 50. Beyond that, little is known about the epidemiology of this condition, and no studies have specifically examined the age and gender distribution of patients with 1° HPT.
Methods
We analyzed patients from the Nationwide Inpatient Sample (NIS), a 20% random sample of all hospital stays from 2000–2004, and also from the University of Michigan endocrine surgery database from 1999–2005. Surgically treated 1° HPT was used as a surrogate marker for 1° HPT. An age- and sex-based frequency distribution was computed for each dataset.
Results
A total of 7,513 females and 2,677 males who underwent surgery for 1° HPT in the 5-year period 2000 through 2004 were reported in the NIS. At the University of Michigan from 1999 through 2005, 790 females and 276 males underwent parathyroidectomy for 1° HPT. In both datasets, the frequency of 1° HPT began to rise slowly in both sexes at age 11 and increased more rapidly among females than males beginning at age 21–25 (NIS) and 26–30 (UM). Incidence curves for both women and men in both databases were similar in shape and unipolar in configuration. Peak incidence was at age 56–60 (NIS) and 61–65 (UM) in females and age 56–60 in males (both datasets). The female:male ratio was noted to rise steadily among the NIS patients until perimenopausal age, after which it became stable for the next 20 years before decreasing again. No change in the female:male ratio over time was seen among the UM patients.
Conclusions
Primary HPT occurs more frequently in females than in males at all ages. The incidence increases steadily after age 25 in both sexes. The female:male ratio does not change during the peri- and postmenopausal years. This information should stimulate new hypotheses to explain the difference in the incidence of 1°HPT between men and women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is generally accepted that the incidence of primary hyperparathyroidism (1° HPT) increases with age and that more women than men are affected[1–8]. Nevertheless, as pointed out by Melton in remarks at the last NIH consensus conference on 1° HPT, many epidemiologic aspects of this condition, including its age- and sex-related incidence and distribution, remain unknown. Previous studies of 1° HPT have reported anywhere from a 3:1 to a 5:1 ratio of females to males. The disproportionate number of women over age 50 with this condition has been attributed, at least in part, to changes in estrogen and other hormone levels that occur with the onset of menopause [9]. Other possible epidemiologic characteristics of 1° HPT remain unknown because no studies have specifically examined the age and sex-related incidence of 1° HPT in a large population.
The purpose of the present study was to determine and describe the age- and sex-related incidence of 1° HPT. We also sought to find out if in fact there is a disproportionate increase in the incidence of 1° HPT in women in the peri- or postmenopausal age range, and to compare the age-related incidence in men and women. If the perceived increased incidence of 1° HPT in women is hormone-related, then the incidence of the disease in men and women should begin to diverge at about 45–50 years of age.
Methods
Because there is no national database that can accurately reflect the incidence of primary hyperparathyroidism across the United States, we used surgically treated 1° HPT as a surrogate marker for the overall incidence of this condition. Two data sources were queried. The Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality maintains the NIS database, which is composed of multiple data points extracted from a 20% random sample of all hospital discharges [10]. The HCUP NIS database was searched with ICD-9 CM and CPT codes for all patients with hyperparathyroidism undergoing parathyroidectomy for the 5-year period 2000–2004. The dataset was further refined by excluding patients with a diagnosis of renal failure, secondary hyperparathyroidism, or tertiary hyperparathyroidism. The endocrine surgery database at the University of Michigan (UM) was searched for the years 1999–2005 for patients having undergone parathyroidectomy for primary hyperparathyroidism. Age and sex of all patients was recorded and an age-based frequency distribution using 5-year intervals was constructed for each dataset. The age distributions of men and women in each dataset were examined for any differences that might offer clues to the etiology of 1° HPT.
Results
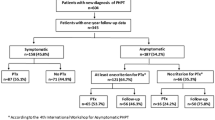
10,190 patients—7,513 females (74%) and 2,677 males (26%)—who underwent parathyroidectomy for 1° HPT between 2000 and the end of 2004 were identified in the NIS database (Table 1). These patients accounted for 0.026% of hospital discharges in the NIS database. The reader should remember that the number of patients identified in the NIS database are based on a 20% random sample of the total number of discharged patients who underwent parathyroidectomy at hospitals participating in the NIS database. Actual patients undergoing parathyroidectomy would be approximately five times higher. Urgency of admission and admission type were also extracted from the dataset for 2004. Of 2,295 patients admitted in 2004 and undergoing parathyroidectomy for 1° HPT, 107 (4.6%) were admitted emergently, 172 (7.5%) were admitted urgently, and 1,732 (75.4%) were admitted electively. No data were available for the remaining 287 (12.5%) patients.
Data were also examined by race. Caucasians and Blacks accounted for 60% and 12.5%, respectively, of patients undergoing parathyroidectomy for 1° HPT. Hispanics, Asian/Pacific Islanders, Native Americans, and Others accounted for 3.5%, 1.3%, 0.001%, and 1.1% of patients. There were no available racial data for 493 (21.4%) patients.
The number of women undergoing parathyroidectomy was greater than the number of men. The mean age of women was 56 (± 12) years and that of men was 61 (± 14) years. The female to male ratio was 2.8:1 overall. The incidence in both men and women rose slowly after age 11 and increased steadily until age 50. A plateau was seen between ages 50 and 75, and then a decrease in the number of patients occurs as average male and female life expectancy is reached (Table 1 and Fig. 1). As is evident in Figure 1, a much steeper slope in the incidence plot for women with 1° HPT begins at about age 26. Men show a similar increase but with a less pronounced change in slope. The peak incidence among females was seen in the 56–60-year age group, in which there were 1,009 patients (13.4%). The peak incidence among males also occurred in the 56–60-year age group, in which there were 326 patients (12.2%). The female:male ratio slowly rises between ages 26 and 50 as overall incidence in both groups rises from 1.66 to 3.18.
In men, a sustained increase in incidence occurred in the 51–75-year age range, in which the mean number of cases per 5-year interval was 302 (11.28% of all male cases) and accounted for 56% of the total number of cases in the male group (Table 1). In women, a similar sustained increase in incidence was seen in the 50–80-year age range, in which the mean number of cases per 5-year interval was 892 (11.9% of all female cases) and accounted for 71.3% of the total number of female cases.
The data extracted from the Endocrine Surgery database at UM were quite similar to the data obtained from the NIS database. In all, 1,066 patients were identified as having undergone parathyroidectomy for 1° HPT over the 6-year period 1999 through 2005 (Table 2 and Fig. 2). There were 790 females (74%) and 276 males (26%). Mean age of women was 58 (± 13) years, and that of men was 55 (± 15) years. The peak incidence in both groups was in the 51–55 year age group, which contained 15.9% of the males and 17.2% of the females. As in the NIS data, a slow rise in frequency of operations for 1° HPT was seen beginning at 11–15 years of age, with a more dramatic increase in frequency seen in females beginning at 26–30 years of age. Frequency among the males increased beginning with the 31–35-year age group, but, again, at a slower rate.
The ratio of men to women undergoing parathyroidectomy at UM during this time period was 2.8:1, which is identical to that of the NIS data. As shown in Table 2, the proportional differences in incidence between men and women remained similar across most age groups. In Tables 1 and 2, the ratios for age groups with small numbers of patients (fewer than 25) are not shown because of the inherent lack of reliability of such small numbers.
Discussion
This study sheds new light on the age- and sex-related incidence of 1° HPT. The chief findings are that, as expected, more women than men are affected. Men and women appear to experience the onset of disease at about the same age. The female to male ratio gradually rises to 3:1 at age 50 and then plateaus for approximately 20 years prior to decreasing. Both male and female age and sex distribution curves are very similar, indicating similar disease experiences across a lifetime. These data do not support the current hypotheses that the incidence of primary hyperparathyroidism increases at the time of menopause in women. Rather, the curves suggest that hyperparathyroidism develops near the same age in both men and women and the incidence appears to be higher in women in every age group. Both the NIS data and the UM data are remarkably similar in this regard.
The disparity in incidence of 1° HPT between women and men remains unexplained. The formation of tentative hypotheses related to the role of gender and the effect of hormonal changes on the development of 1° HPT in the past are understandable. Estrogen appears to slow bone resorption by blocking cytokine signaling to the osteoclast, increasing bone mineral density, and reducing the incidence of new vertebral fractures by nearly 50% [11]. Some studies report that in the parathyroid glands, estrogen receptors are present in parathyroid cells and act to increase the parathyroid (PTH) mRNA levels. Some investigators believe that as longer periods of amenorrhea develop, the unopposed estrogen stimulation of the parathyroid glands may lead to HPT. The metabolic effect of estrogen on bone metabolism notwithstanding, our dataset makes these hypotheses less plausible. Other studies [12] have noted conflicting attempts to characterize estrogen receptor expression in human parathyroid glands. Some report expression of estrogen receptors, whereas others do not. The insulin-like growth factor (IGF) system has also been suggested as playing a role in tumorigenesis in other organ systems. Several study groups have demonstrated IGF reactivity in parathyroid tissue, allowing another possible pathway explaining adenoma/hyperplasia formation.
Other studies, also based on hormonal hypotheses, have looked at 1° HPT in relation to pregnancy or degree of parity. While 1° HPT diagnosed during pregnancy is rare, it is still unclear what the true incidence is. One estimate is 8 per 100,000 [13]. However, this may be a gross underestimation, because most reports have only emphasized cases associated with fetal complications. Multiparity has also been weakly associated with an increased risk of 1° HPT [14]. Those diagnosed prior to menopause were found to have had their first child at a younger age. Nulliparous women were at an increased risk to have 1° HPT diagnosed prior to menopause and a decreased risk after menopause. Compared to uniparity, multiparity was associated with an increased risk for 1° HPT in women both before and after menopause. Our data contradict the findings of these smaller studies.
There are limitations inherent in the present study. We used a surgical procedure, parathyroidectomy, as a surrogate marker of the disease itself to estimate the incidence of primary hyperparathyroidism. Neither database allows one to determine how long patients may have been followed for their disease prior to operation. The datasets do not capture patients with 1° HPT who are either never identified or are managed medically or by observation rather than by surgical means. During the period under study, however, surgery remained the only effective treatment for 1° HPT and the only means of curing the disease. While the UM sample might be subject to geographic variation, the nationwide sample available to us minimizes the likelihood that regional variation in referral patterns for operation affects our results. Parathyroidectomy performed in outpatient surgery centers is increasing and would not be captured in the NIS database. Unfortunately, the State Ambulatory Surgery Database (SASD) [15], which would capture this information, only includes 23 participating states and would grossly underestimate the number of outpatient procedures performed. Many of these states do not capture both hospital-based and free-standing ambulatory surgery centers in the data.
Another possible bias might be introduced by the differences in likelihood that men and women will undergo comprehensive metabolic testing at a given age. It is well known that women see primary care providers more frequently than men. This might lead to under-diagnosis among men and therefore not accurately reflect their incidence of 1° HPT. We do not have a way to estimate the magnitude of such an effect, if any exists. Routine metabolic testing is more common in older patients, and nothing in our data suggests the relative incidence is different among younger and older patients. We believe therefore that the data in this study likely reflect fairly accurately the age- and sex-related incidence of this condition in the United States.
Conclusions
Surgically treated 1° HPT occurs more frequently in females than in males at all ages. Age-related incidence curves, however, appear to be quite similar. There is no difference in age- or sex-related incidence to support the hypothesis that hormonal changes, such as those that occur during menopause or childbearing, account for the higher incidence of 1° HPT in women. The true reasons for the difference in incidence of 1° HPT between men and women remain to be discovered. New hypotheses regarding the etiology of 1° HPT should take these data into account.
References
Heath H III, Hodgson SF, Kennedy M (1980) Primary hyperparathyroidism: incidence, morbidity and potential economic impact in a community. N Engl J Med 302:189–193
Melton LJ III (1991) Epidemiology of primary hyperparathyroidism. J Bone Miner Res 6(Suppl 2):S25–S30
Wermers RA, Khosla S, Atkinson EJ (1997) The rise and fall of primary hyperparathyroidism: a population-based study in Rochester, Minnesota 1965–1992. Ann Intern Med 126:433–440
Melton LJ III (2002) The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res 17(Suppl 2):N12–17
Wermers RA, Khosla S, Atkinson EJ et al. (2006) Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of disease. J Bone Miner Res 21:171–177
Bilezikian JP, Silverberg SJ (2000) The clinical spectrum of primary hyperparathryoidism. Rev Endocr Metab Disord 1:237–245
Adami S, Marcocci C, Gatti D (2002) Epidemiology of hyperparathyroidism in Europe. J Bone Miner Res 17–2:N18–23
Ljunghall S, Hellman P, Rastad J et al. (1991) Primary hyperparathyroidism: epidemiology, diagnosis and clinical picture. World J Surg 15:681–687
Joborn C, Ljunghall S, Larsson K et al. (1991) Skeletal responsiveness to parathyroid hormone in healthy females: relationship to menopause and estrogen replacement. Clin Endocrinol 34:335
HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2000–2001. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/nisoverview.jsp
Wells G, Tugwell P, Shea B et al. (2002) Metaanalyses of therapies for postmenopausal osteoporosis. V. Meta-analysis of the efficacy of hormone replacement therapy in treating and preventing osteoporosis in postmenopausal women. Endocr Rev 23:529–539
Wong C, Lai T, Hilly JM et al. (2002) Selective estrogen receptor modulators inhibit the effects of insulin-like growth factors in hyperparathyroidism. Surgery 132:998–1006; discussion 1006–1007
Kort KC, Schiller HJ, Numann PJ (1999) Hyperparathyroidism and pregnancy. Am J Surg 177:66–68
Rastad J, Ekbom A, Hultin H et al. (2001) Childbearing and the risk of parathyroid adenoma—a dominant cause for primary hyperparathyroidism. J Intern Med 250:43–49
HCUP State Ambulatory Surgery Databases (SASD). Healthcare Cost and Utilization Project (HCUP). 2000–2004. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/sasdoverview.jsp
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, B.S., Dimick, J., Wainess, R. et al. Age- and Sex-Related Incidence of Surgically Treated Primary Hyperparathyroidism. World J Surg 32, 795–799 (2008). https://doi.org/10.1007/s00268-007-9427-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9427-2