Abstract
Food effects on oral drug bioavailability are a consequence of the complex interplay between drug, formulation and human gastrointestinal (GI) physiology. Accordingly, the prediction of the direction and the extent of food effects is often difficult. With respect to novel formulations, biorelevant in vitro methods can be extremely powerful tools to simulate the effect of food-induced changes on the physiological GI conditions on drug release and absorption. However, the selection of suitable in vitro methods should be based on a thorough understanding not only of human GI physiology but also of the drug and formulation properties. This review focuses on in vitro methods that can be applied to evaluate the effect of food intake on drug release from extended release (ER) products during preclinical formulation development. With the aid of different examples, it will be demonstrated that the combined and targeted use of various biorelevant in vitro methods can be extremely useful for understanding drug release from ER products in the fed state and to be able to forecast formulation-associated risks such as dose dumping in early stages of formulation development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
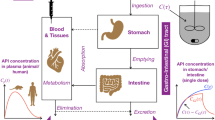
Interactions between food intake and drug administration are one of the major challenges in oral biopharmaceutics as concomitant intake of food can affect the pharmacokinetic profile of an orally administered drug by changing its dissolution, absorption, metabolism, and/or elimination behaviour (1). The reasons for the occurrence of these food effects on oral bioavailability are manifold, and the resulting food effect can be regarded as the sum of all these processes. In general, food effects are based on interactions between the drug, the formulation and the physiological conditions inside the human gastrointestinal (GI) tract (1,2). In the case of oral extended release (ER) dosage forms where drug release is limiting absorption, the formulation has a much greater effect on bioavailability compared to immediate release drug products (Table I). Typically, ER dosage forms release the drug constantly over several hours irrespective of the nutritional state. In this regard, one of the greatest threats to the safety and efficacy of oral pharmacotherapy is dose dumping. This describes the loss of controlled release behaviour resulting in the absorption of large amounts of drug within a relatively short time (3). Owing to higher drug loading of ER dosage forms, this undesired drug release behaviour can lead to overdosing of the patient. In case of drugs with a narrow therapeutic index such as theophylline, this may have dramatic consequences (4). On the other hand, poorly formulated ER dosage forms may cause sub-therapeutic plasma concentrations if the drug is not released in the desired manner, which may also lead to therapy failure.
In this review, we will describe how the interactions between the drug, the formulation and physiology can be considered in biorelevant in vitro approaches with the aim to forecast food effects on oral bioavailability during preclinical formulation development. Particular attention will be paid to the sensitivity of commonly used ER concepts to certain physiological parameters. Since the evaluation of food effects is not possible without the understanding of human GI physiology, the physiological variations present under postprandial conditions will be briefly described at the beginning of this work and considered throughout the whole review. Moreover, we will try to explain how the selection of appropriate in vitro tools can aid the forecast of food effects on the pharmacokinetic profile of ER dosage forms.
PHYSIOLOGY-RELATED FACTORS CONTRIBUTING TO FOOD EFFECTS
The intake of food leads to various changes in GI physiology, in particular in the stomach and the proximal small intestine. The presence of food itself, as well as the altered motility and secretion patterns required for efficient digestion, results in a dramatic alteration of the environment, in which the drug is released and absorbed. Amongst others, these changes have a significant effect on the relevant parameters such as residence times, fluid volumes, pH profiles and shear stresses arising during GI transit (5,6).
Transit Times
With the aid of different techniques such as scintigraphy, Magnetic Marker Monitoring (MMM) or telemetric capsules, the gastric residence times (GRT) of non-digestible objects have been investigated in recent years. As can be seen from Fig. 1, the GRT in the fed state is clearly prolonged compared to the fasted state. Interestingly, the small intestinal transit time is almost unaffected by the nutritional state and amounts to 2–5 h in both fasted and fed state.
Box plot of time points of gastric emptying (GE) under fasting and fed conditions as well as small intestinal transit times (SITT, calculated as difference between the time point of arrival in colon and gastric emptying) of non-disintegrating capsules and tablets with a diameter of at least 5 mm as determined in several MMM studies. Reprinted from (7) with permission from Elsevier
Generally, the dosage form dimensions in combination with the disintegration behaviour are of paramount importance for the GRT of oral ER dosage forms. Whereas multi-particulate or quickly disintegrating dosage forms can leave the stomach together with the meal even in the fed state, larger non-digestible objects such as hydrogel matrix tablets are retained until recurrence of the fasted state motility (7,8). However, a clear cut-off diameter that prohibits emptying in fed state cannot be defined (8). In general, the gastric emptying time of non-digestible objects is not only affected by the size of the objects tested but also by the caloric value of the meal (Table II).
The higher the caloric value of the test meal, the longer the gastric residence time of non-disintegrating, monolithic dosage forms. The fasted state motility pattern which allows the emptying of large, non-digestible objects by strong peristalsis, only returns if at least 90% of the meal is emptied from the stomach (19). In case of the high-caloric (800–1000 kcal), high-fat FDA standard breakfast, this may take up to 5 h and longer. The intake of lunch, which is typically served 4–6 h after drug administration, can lead to a further delay of gastric emptying (18). This effect was nicely demonstrated in a publication by Ewe and co-workers, who showed that the steady intake of meals (i.e. breakfast, lunch, supper) delayed the gastric emptying of non-digestible tablets to up 509 ± 220 min (20). Therefore, great care has to be taken to the nutritional regime described in the study protocol as this can potentially influence the food effect of the ER dosage form (18).
Due to the delayed gastric residence time of non-digestible ER dosage forms in the fed state, there is a clear need to consider the gastric environment in order to be able to forecast food effects (5). It must be kept in mind that a long GRT is not per se a threat to oral drug delivery. It can also be advantageous, especially for drugs with an absorption window in the proximal small intestine (21).
Motility
The dependence of gastric residence times on the prandial state is the result of motility patterns specific for fasted and fed state. These motility patterns also lead to the situation that ER dosage forms are exposed to distinct mechanical conditions during their GI transit. The so-called Migrating Motor Complex (MMC) is characteristic for the fasted state (22). This cyclic pattern consists of three different phases. MMC phase I, a period of quiescence, is followed by MMC phases II and III as phases of peristaltic activity. Especially during the short MMC phase III, strong peristaltic contractions are present that enable the general cleansing of the stomach. Typically, the gastric residence time of large non-digestible objects in the fasted state is determined by the occurrence of these so-called housekeeping waves. During MMC phase III, pressure values of up to 500 mbar can arise, as was previously revealed using the SmartPill (18). These high pressure values can destroy ER dosage form integrity resulting in potential dose dumping (23). However, owing to the circular nature of the antral contraction waves, the magnitude of the applied pressure depends on the size of the object. Thus, the smaller the object, the smaller is the pressure applied. In the small intestine, the shear forces generated by peristalsis are typically low (18).
Apart from the forceful contractions caused by the MMC phase III activity, an ER dosage form is exposed to rather low shear stresses in the fasted state (24). This situation changes dramatically in the fed stomach, in which the fed state motility pattern causes continuous peristaltic activity. Jain and colleagues showed that these differences can cause faster erosion of HPMC matrix tablets (25). In the fed state, peristaltic waves are generated in the corpus with a frequency of 3 per minute and move towards the pylorus. In the small intestine, these contractions are continued with a frequency of 12 per minute (26). However, the intragastric localisation determines the exposition to mechanical stresses as the fundus is unaffected by the peristaltic contractions, whilst the antrum is a high shear zone. This was demonstrated with the help of MMM (27,28). As can be seen in Fig. 2, the hydrogel matrix tablet investigated is very sensitive to the different mechanical conditions in the stomach and small intestine. Localisation in the antrum causes drug release and also the transfer of the released drug to the site of absorption. In contrast, localisation in the fundus does not trigger the onset of drug plasma levels.
Comparison of plasma concentrations (black circle), gastrointestinal tablet localization (gastric emptying: dashed blue line; grey areas indicate residence in the fundus), measured drug release profiles (white square, normalised to last value) and deconvoluted fractional bioavailability profiles (dashed line, normalised to last value as for measured drug release) after fed state administration of a hydrogel matrix tablet containing felodipine by two different subjects (27)
Gastrointestinal Contents
During gastric transit, an orally administered drug is exposed to highly dynamic conditions that arise from simultaneous secretion, digestion and emptying processes (5). Thus, it must be kept in mind that important parameters such as fluid volumes, luminal pH and surface tension are not static and change over time (5). In the last years, the physicochemical characteristics of the GI contents in the fed state have been evaluated with the aid of different techniques such as aspiration of luminal contents or telemetric capsules (18,29,30). However, in many cases, these studies were performed with liquid test meals, which have different physicochemical properties compared to solid test meals such as the test meal proposed by FDA and EMA for food-effect bioavailability and fed bioequivalence studies—the so-called FDA standard meal (31).
The initial gastric content is highly heterogeneous and composed of the ingested meal, residual fasted state contents, and oral and gastric secretions. The initial conditions in stomach, duodenum and ascending colon of fasted and fed state (measured after administration of Ensure® Plus or the FDA standard meal) are summarised in Table III. One should note that this overview does neither highlight the inter- and intraindividual variability nor the dynamic changes of all these parameters, which were demonstrated in various studies (18,29,32,34,35,36).
One of the main differences between fasted and fed state and a major contributor to food effects are the hydrodynamics in the stomach. The fluid volume in the stomach after an overnight fast is typically low and amounts to 10–50 mL. Directly after drug administration, the fluid volume increases owing to the co-administered water. However, this volume is typically emptied within 15–45 min (37). In contrast, after administration of the FDA standard breakfast, the gastric content volume amounts to about 580 mL. Even 4.5 h later, more than 150 mL is present in the stomach. Interestingly, water administered after meal intake (e.g. during drug administration) can be emptied even from the fed stomach via a physiological shortcut (stomach road or Magenstrasse) (32).
Mechanical, chemical and enzymatical digestion processes prepare the gastric content for intestinal nutrient absorption, which results in various changes in the physiological conditions (e.g. pH value, viscosity and surface tension). Both the intragastric solubility of a drug and the drug release behaviour from the ER dosage form are affected by the complex interplay of all these parameters. Thereby, the intragastric location of the dosage form can again be highly important, as the conditions in the proximal and distal parts of the stomach can differ significantly in terms of pH or fat fraction (18,32). Unfortunately, the time-dependent changes of other important parameters such as viscosity have not been investigated in vivo to date.
With respect to intestinal conditions, the dimensions and the disintegration behaviour of the dosage form must be considered. A large non-digestible object such as a hydrogel matrix tablet will be emptied only after recurrence of the fasted state motility and thus will be exposed to fasted conditions in the small intestine. In contrast, multi-particulate ER dosage forms will experience fed intestinal conditions. The luminal conditions within the fasted and fed small intestine differ significantly, especially in terms of bile salt concentration and the presence of digestive enzymes (38). Food lipids emptied from the stomach and bile salts can form mixed micelles, which can aid the solubilisation of drugs (39,40). In regard to the lower intestine, information on the physicochemical characteristics of its contents is mainly provided from studies in which the FDA standard meal was administered to healthy adults (33,41). In these studies, contents from the distal ileum and the ascending colon were collected 5 h after the administration of the FDA meal, which was the time by which the multiparticulate ER products were expected to arrive at the lower intestine. At this time, the pH values in the distal ileum were found to be slightly alkaline with a mean pH value around pH 8, which is similar to the fasted state. On the other hand, the pH value in the proximal colon (i.e. caecum and ascending colon) pH is only about pH 6. However, recent studies with telemetric capsules have demonstrated that the colonic pH is highly variable with pH values ranging from pH 5 to pH 8 (18,42).
DRUG-RELATED FACTORS CONTRIBUTING TO FOOD EFFECTS
In the majority of cases, a food effect is based on the physicochemical properties of the drug (1). Therefore, basic information about the drug such as data on pH-dependent solubility, solubility in biorelevant media and stability in GI fluids along with information on absorption rate and site-specific absorption are generally inevitable for the prediction of food effects (43). The contribution of drug-related factors to food effects of ER dosage forms can be assessed by thorough evaluation of the data generated by use of standard and biorelevant in vitro methods as well as the in vivo data obtained from food effect studies with the respective immediate release (IR) product. Given that the mechanism behind the food effect of a drug or a particular formulation thereof is known, a well-designed ER dosage form can help to reduce the food effect and thus increase efficacy and safety of oral drug therapy.
In the case of IR dosage forms, a rough assessment of possible food effects can be achieved using the Biopharmaceutical Classification System (BCS), which classifies drugs based on solubility and permeability into four categories (1,43,44,45). BCS class I drugs typically possess no food effect as they are regarded as highly soluble and permeable. However, the onset of action is determined by the gastric emptying rate and thus can be controlled by using ER dosage forms containing BCS class I drugs. In contrast, BCS class II drugs often show positive food effects, as the increase in fluid volume, the presence of lipids and the secretion of bile salts can enhance the solubility in fed state compared to the solubility in fasted state fluids. For BCS class III drugs, concomitant food intake often causes a drop in oral bioavailability. It is assumed that food present in the small intestine interferes with drug absorption. Some authors postulated that certain nutrients such as lipids can interact with uptake transporters (45). In case of BCS class IV drugs, the magnitude and the direction of the food effects are highly erratic.
Based on the information from the food effect studies performed with the immediate release product, a primary assessment of the possible risk for food-drug interactions for the ER dosage form can be made.
FORMULATION-RELATED FACTORS CONTRIBUTING TO FOOD EFFECTS
Interestingly, the food effect of an IR product does not necessarily correlate with the one of the respective ER product. Hence, the formulation design of the ER product seems to play an important role for the presence of food effects on oral bioavailability. In the following paragraph, we will explain how food can affect the drug release behaviour from solid oral dosage forms based on common ER principles.
Before describing formulation-specific interactions, it should be mentioned that the dimensions of an ER dosage form can be a very important factor leading to food effects. As described above, large non-digestible objects such as hydrogel matrix tablets or OROS will be retained in the stomach until recurrence of the fasted state motility owing to the physiological phenomenon of gastric sieving (2). On the other hand, multi-particulate dosage forms can leave the stomach even under fed conditions. The resulting gastric transit times do inherently determine the time of exposure to certain conditions, which may affect important parameters including drug solubility and intestinal absorption. In the case of drugs with limited or pH-dependent aqueous solubility or for drugs with an absorption window in the upper small intestine, these changes may be highly relevant. However, it must be kept in mind that the dimensions of eroding extended release tablets typically decrease within the stomach, which may already enable gastric emptying in fed state.
Hydrogel Matrix Tablets
Matrix tablets based on hydrophilic matrices such as hydroxypropyl methylcellulose (HPMC) represent the most popular way for controlled oral drug delivery as they can be manufactured in a relatively simple and cost-effective way. On the other hand, they also belong to the most sensitive systems towards food-induced changes of the human GI tract since drug release from these systems is the result of a complex interplay between hydration, swelling, drug dissolution, diffusion and erosion (46). Typically, drug release is controlled either by diffusion through the hydrated polymer layer or by the erosion of this layer. All these processes can be affected by concomitant food intake (25,47). Thereby, the direction and the magnitude of food effects depend on various formulation and processing parameters and cannot be easily predicted.
The hydration of the matrix is the prerequisite for drug release but depends on several factors. Owing to higher luminal fluid volumes after food intake (32), matrix hydration should be faster in the fed state. However, the presence of certain food components such as proteins and lipids can have detrimental effects. Abrahamsson and co-workers showed that precipitation of a film at the tablet’s surface, which was mainly composed of proteins, delayed drug release in biorelevant media simulating the fed stomach (48). In another study, Williams and colleagues observed the formation of a fat layer at the surface of HPMC matrix tablets in fat-rich emulsions, which also caused altered drug release (49). Besides, it must also be noted that the high osmolality of the fed gastric content can affect the properties of the formed gel layer. Depending on the polymer used, higher salt and sugar concentrations may accelerate drug release due to loss of the integrity of the gel layer (50).
It must be further noted that the swollen hydrogel matrices are often sensitive to mechanical forces. In the fed stomach, the increased gastric transit time along with higher shear stresses may accelerate the erosion of the hydrogel matrix in the fed state as was shown by Jain and co-workers (25). It is therefore not surprising that different authors describe complete disintegration of hydrogel matrix tablets already in the stomach (25,51). As a result, maximum plasma concentrations are observed after around 2–6 h in form of relatively sharp peaks (51). In the worst-case, the accumulation of released drug in the stomach can lead to dose dumping-like plasma peaks, which in this case do not reflect failure of the drug release mechanism but rapid absorption of high amounts of a drug which has accumulated within the stomach (27). Additionally, the high shear stresses arising during the passage of the pyloric sphincter may also cause the destruction of the hydrogel matrix and thus, dose dumping (18). It must be kept in mind that due to higher drug loading of ER dosage forms, dose dumping can have dramatic consequences (e.g. overdosing) for the patient and should be avoided in any case.
Osmotic-Release Oral System (OROS)
Osmotic-release oral systems are regarded as relatively robust towards food-induced changes of the gastrointestinal conditions. Several studies demonstrated the superiority of OROS over other ER dosage forms (52,53). Schug and colleagues investigated two different ER formulations of the BCS class II drug nifedipine (Fig. 3). In contrast to the test product (NIFEDICRON), the OROS (osmotic-release oral system) was less susceptible to food-induced changes in the GI tract and thus, released the drug almost independent of food intake. In the literature, no cases could be identified describing significant food effects with OROS (54).
Mean plasma concentration versus time curves of nifedipine (given as geometric means and standard deviations) determined after oral administration of Adalat OROS and Nifedicron under fasting conditions (a) and after a high-fat breakfast (b) in 24 healthy young volunteers. Reprinted by permission from Springer Nature (54)
Owing to a lag time of drug release in the range of 1–3 h, the accumulation of released drug in the stomach is less likely and thus, OROS is therefore less prone to dose dumping (27). However, owing to the large dimensions and the non-disintegrating character of OROS, long gastric residence times can be expected when OROS is administered together with food (55).
Multi-Particulate ER Dosage Forms
Multi-particulate dosage forms with particle sizes below 2–3 mm have the advantage that they can leave the stomach even in the fed state due to the small dimensions of the individual particulates. Thus, they typically do not accumulate in the stomach and are emptied together with food. O’Reilly and colleagues demonstrated that multi-particulates, which are administered after a meal, follow a linear emptying pattern (56). Based on these data, it was believed that the use of multi-particulates is superior in generating a sustained release and minimising the variability of drug plasma levels. However, different studies have shown that the application of multi-particulate dosage forms can cause dramatic food effects (55). In contrast to monolithic ER dosage forms, multi-particulates can be emptied into the fed duodenum. In particular for poorly water-soluble drugs, the increased bile salt levels may aid solubilisation (39). Therefore, the rate by which multi-particulate dosage forms are emptied into the small intestine and the interaction with hepatic and pancreatic secretions will dictate the magnitude and direction of food effects.
PHYSIOLOGICALLY RELEVANT IN VITRO DISSOLUTION TEST METHODS
As described in the previous sections, the absorption of a drug can be highly dependent upon a plethora of factors not only related to the design of the formulation itself but also the prevailing conditions along the GI tract which can be significantly influenced by the presence of food. In order to evaluate the performance of these different formulation types under relevant conditions in vitro, these factors, especially in terms of how food can impact on the drug release behaviour, need to be considered in the in vitro test used.
In this section, we will summarise which in vitro tools can be used to forecast the in vivo performance of ER dosage forms in the fed state. At the moment, numerous physiologically relevant test media and test apparatuses can potentially be used for the simulation of fed state conditions in the stomach and small intestine (57). Based on their complexity, the current approaches can be classified into four major categories (Table IV).
Category A Test Methods
For the prediction of the in vivo performance of ER dosage forms in the fed state, standard dissolution test methods allow the initial characterisation of new formulations and the investigation of the impact of basic parameters such as pH or shear rate. Based on this information, the formulation can be further optimised. The main advantage of these methods is the high level of standardisation, broad application and experience as well as the fact that they are typically available in every formulation laboratory. They are often applied to generate helpful reference data.
As the standard USP dissolution apparatuses does not reflect the physiologically relevant shear conditions, their informative value is often limited and the forecast of the in vivo performance can hardly be based solely on applying category A test methods (58,59).
Category B Test Methods
Category B test methods describe the use of physiologically relevant media in USP standard dissolution test apparatuses. Typically, such experiments can be performed in every laboratory but require more sophisticated analytics, which may cause a significant increase in time and efforts. Nonetheless, these methods can give valuable information about the behaviour of oral ER dosage forms in complex media. For instance, it was demonstrated that for hydrogel matrix tablets, drug release and disintegration behaviour are changed in the presence of certain food components (48,49). As was described by Markopoulos and colleagues, the complexity of the media can be increased by certain additives such as lipids, digestive enzymes or viscosity-increasing agents (Fig. 4) (60). By this, the effect of media-related aspects (e.g. bile salts, lipids, proteins) can be specifically investigated. For instance, the ratio of drug release in FeSSIF/FaSSIF can give an early indication about the probability of a food effect related to the intestinal conditions.
The four levels of biorelevant media recommended for the simulation of the luminal environment. Reprinted from (60) with permission from Elsevier
Typically, laboratories use their own physiologically relevant medium for the simulation of fed conditions. For the simulation of the conditions in the stomach, a generally accepted standard medium does not exist (61). For the simulation of intestinal conditions, some fed state simulation media have gained a broader acceptance (e.g. FeSSIF) (60).
For gastric conditions, the use of the homogenised FDA standard meal would be the best representation of the initial fed state, but it poses several analytical and technical problems (40). Moreover, many physiological variables such as oral and gastric secretion rates, digestion rates by pepsin or gastric lipase, or viscosity changes are still unknown for this particular meal. Therefore, most groups use either milk-based media, nutrient drinks such as Ensure® Plus or media based on parenteral emulsions (61,62). However, these media are not fully reflective of the complex situation in the stomach, and in particular, the aspect of gastric digestion is mostly neglected. Diakidou and colleagues nicely indicated that these processes may play an important role for the investigation of food effects of oral ER dosage forms, as was shown for a felodipine hydrogel matrix tablet (63).
With respect to intestinal conditions, especially the increased bile salt and phospholipid concentrations in the fed state as well as elevated enzyme levels have to be considered, as the solubilisation by mixed micelles is regarded as one of the major contributor to food effects (64). Popular media for the simulation of fed conditions in the small intestine are FeSSIF and FeSSIF-V2. The two versions of FeSSIF differ in terms of pH, buffer capacity, osmolality, bile salt concentration, buffer species and most importantly, the presence of monoacylglycerols and free fatty acids (65). In FeSSIF-V2, glycerol monoolein and sodium oleate are used to simulate the presence of lipid digestion products. For more distal parts of the small intestine, FeSSIFmidgut and SIFIleum can be used (60,66). For the simulation of the contents of the lower intestine, Georgaka and colleagues have proposed the use of FeSSCoF-V2 (66). Media simulating the fed small intestine are mainly useful for immediate-release products, or multi-particulate ER dosage forms as large, non-digestible objects can only be emptied into the duodenum in the fasted state. The usefulness of these media was demonstrated in different studies in which a controlled change of the dissolution medium was made possible by use of the Bio-Dis (USP apparatus III) or the flow-through cell (USP apparatus IV). This media-change approach was used to study drug release from mesalamine modified-release (MR) tablets, from different ER products containing theophylline as well as from hydrogel matrix tablets containing caffeine (67,68,69).
It should be noted that the effect of the buffer species is often not fully considered. Whilst most in vitro methods are based on compendial phosphate or maleate buffer systems, these, however, have limited physiological significance. To improve the physiological relevance, different groups have proposed the use of using carbonate buffers (70,71,72). Fadda and colleagues showed that the choice of buffer species can have a significant impact on the release of mesalamine from MR dosage forms (70). In another study, Shibata and colleagues demonstrated that drug release from enteric-coated tablets containing omeprazole and rabeprazol was different in phosphate buffer compared to bicarbonate-based buffer systems (73).
A formulation that shows the same in vitro drug release profile irrespective of the medium may also be robust towards changes of the luminal conditions in vivo. However, it must be kept in mind that the dynamic changes of the composition and the properties of luminal fluids in the fed human GI tract are not fully understood. Therefore, the situation created by use of media such as either milk or Ensure® Plus does not necessarily reflect the in vivo situation. Therefore, the results from such experiments should always be evaluated carefully. In line with this, Williams and colleagues showed that the use of fat-rich emulsions may cause physiologically irrelevant problems (49). The formation of a fat film on the surface of hydrogel matrix tablets may play a role in vitro, but in vivo, higher shear stresses, the presence of bile salts and the action of digestive enzymes probably prevent the film formation.
Category C Test Methods
In recent years, several in vitro test devices were developed with the aim to simulate certain aspects of human GI physiology (57). In contrast to biorelevant dissolution media, they allow the simulation of physiological relevant parameters such as luminal dosage form movement, shear rates and stresses, secretion and gastric emptying patterns. The systems can be classified based on their complexity and functionality (Table V).
Category C test methods allow the abstract and reproducible simulation of certain gastrointestinal parameters. These devices are based on different modifications of the standard dissolution test apparatuses with the aim to increase physiological relevance. Their advantage is the capability to specifically investigate the effects of certain aspects of GI transit such as shear stress or dosage form movement on drug release from oral ER dosage forms. In this way, the robustness of novel ER dosage forms towards physiological conditions can be tested. For instance, Garbacz and co-workers investigated the sensitivity of various oral ER dosage forms towards gastrointestinal pressure by using the Dissolution StressTest device (Fig. 5, bottom left) (23). Another biorelevant test device, the Fed Stomach Model (FSM, Fig. 5, top middle) was designed to specifically simulate the mechanical conditions within the fed stomach. The different shear conditions in the stomach are considered by test programs specific for fundus, antrum and gastric emptying (27,74). In order to simulate the effects of the intragastric location of an ER dosage form in the fed stomach, different test scenarios can be simulated that are based on deposition data from previous MMM studies. In this way, the robustness of different formulations towards certain parameters present under fed conditions can be assessed. It was shown in a recent study that the simulation of intragastric shear stresses can be crucial for drug release from bilayer ER diclofenac tablets (74).
The drawbacks of these systems are their limited availability and the fact that valid information can only be generated if a larger set of experiments is performed. However, simpler systems such as the FSM allow the simultaneous investigation of up to six tablets at a time, and thus, the experiments are typically time and cost-effective. Theoretically, they could be applied in parallel to formulation development in order to allow a quick assessment of robustness towards physiological conditions. In this way, novel ER dosage forms could be optimised in a targeted fashion offering a possible reduction of development time and costs.
Category D Test Methods
Category D test methods are in vitro test systems with a high degree of complexity that allows one to study drug release in a simulated GI environment. As can be seen from Table V, the most advanced systems at the moment include the Dynamic Gastric Model (DGM) and the TNO TIM-1 (75). Both systems were initially designed to study food digestion in vitro but found their way into oral biopharmaceutics in recent years. Whereas the DGM is useful to study the effect of gastric processing, the TNO TIM-1 aims at the simulation of both gastric and intestinal processes.
Since the DGM (Fig. 5, bottom right) is currently the most advanced model for the simulation of the human stomach, this system might be particularly helpful to study the gastric drug release of ER dosage forms with long residence times in the fed stomach (e.g. hydrogel matrix tablets, OROS). However, the system was developed to study gastric food processing and is therefore not dedicated to aid the development of novel ER dosage forms. In particular, the simulation of shear stresses by the DGM does not adequately replicate the nature of peristalsis of the human stomach. In a recent publication by Chessa, the DGM was used to study the hydration of hydrogel matrix tablets under fasted and fed intake conditions (75).
The TNO TIM-1 system (Fig. 5, top right) is a complex representation of the upper human GI tract that considers various aspects of GI physiology. Although it was used to study the drug release of enteric-coated mesalamine tablets in the fed state, it is also not dedicated to test slowly or non-disintegrating dosage forms (76). However, by using an advanced version of the gastric compartment, the so-called TIM-agc (advanced gastric compartment), the food effect of ER dosage forms could potentially be investigated (77).
For formulation scientists, these highly complex systems may seem scientifically appealing, but a number of drawbacks limit their suitability for routine experiments to evaluate the behaviour of oral ER dosage forms. These limitations are related to the complex nature of the experiments with regard not only to the high degree of effort needed and additional costs involved, but also limited availability of these devices to formulation scientists. Additionally, this is further compounded by the fact that there is limited control of the localization of the dosage forms within these models. Thus, the dosage forms can be exposed to variable conditions in terms of mechanical stresses and hydrodynamics, which may be an explanation for the highly variable results observed. Thus, these systems are difficult for routine experiments involving oral ER dosage forms but may be helpful for gaining a mechanistic understanding of the factors influencing drug release in the fed state.
A common limitation of all available systems is the lack of an appropriate simulation of gastric emptying. As far as we know, none of these systems enable the transfer of a large object from the gastric to the intestinal compartment. Thus, the dynamics of the human GI tract can hardly be simulated. In addition, most of the in vitro systems are based on fluid volumes that are unrealistically high. In particular, the intestinal fluid volume is much lower than simulated in the in vitro method (2). It must also be considered that there is no continual contact of the formulation to fluid in vivo and the absence of a continual contact to GI fluids can cause altered drug release, especially from systems that require certain fluid volumes for hydration.
IN VITRO STRATEGIES FOR THE PREDICTION OF FOOD EFFECTS
Although various in vitro test systems with different degrees of complexity can be used to study drug release under simulated postprandial conditions (Fig. 5), the best and safest way to determine the food effect of ER dosage forms today would still be a clinical trial. However, the selection of appropriate in vitro test methods that assist the formulation development can aid the targeted optimisation of the dosage form and by this, save time and money. Increasing the robustness of a dosage form towards a variety of conditions will also increase the probability for a successful clinical trial. Ideally, the selection of the most appropriate in vitro test method/s would be based on the ER concept and recent experiences with the drug, but often, the choice is limited by availability. Therefore, in most cases, category A and B test methods are used to assist formulation development, as standard dissolution test equipment is generally available and biorelevant media can be prepared easily. In certain cases, the media change approach can be advantageous as it allows to study drug release under more dynamic conditions. Moreover, the interaction between transit times as well as luminal conditions in stomach and small intestine can be studied as well. The more complex category C and D systems are typically used in a scientific context, or applied to gain a mechanistic understanding of food effects after failed clinical trials.
Based on recent experience, certain aspects are key to the development of an ER dosage form where drug release should not to be influenced by food intake. First of all, possible risks associated with the drug (e.g. stability in GI fluids, absorption window, solubility issues) and the formulation (e.g. ER concept, assumed gastric transit time) must be identified. The consequences of a long gastric residence time were demonstrated for an ER tablet containing amoxicillin and clavulanic acid (28). Due to an absorption window in the upper small intestine, a long gastric residence time was beneficial for the bioavailability of amoxicillin. In contrast, clavulanic acid which is not stable in the gastric environment demonstrates a reduction in AUC with increased gastric residence.
Following this initial risk assessment, the most suitable in vitro methods should be selected. With the help of these models, the dosage form can be optimised. Typically, this would include a number of basic experiments (i.e. aqueous media of different pH in standard dissolution test apparatuses) and various formulation-specific in vitro tests. For instance, in the case of hydrogel matrix tablets, the investigation of drug release under physiological shear conditions (e.g. by use of the StressTest or the FSM) can aid to prevent dose dumping. In contrast, for multi-particulate dosage forms, the application of these methods seems less appropriate. With respect to simulated transit times in stomach and small intestine, it must be considered that large, non-disintegrating objects can have extremely long gastric transit times in the fed state. Thus, simulating gastric conditions for only 2 h does not seem justified.
The aim of in vitro test methods would be the demonstration of the robustness of novel ER formulations towards different conditions. An ER dosage form that releases the drug irrespective of the test conditions would be expected to be more robust towards the in vivo conditions. Although this approach does not fully guarantee the absence of food effects on oral bioavailability, it enables the selection of the most robust formulation and thus increases the probability of a successful outcome of the clinical trial.
In summary, the following aspects should be considered for determining the most appropriate in vitro test condition:
-
1.
The robustness of a dosage forms towards certain physiological parameters should never be based on a single level only. For instance, in dependence on the type of food and the gastric residence time, gastric pH values can vary widely between pH 1 and 7, and thus, in vitro experiments should always cover the whole range (18). The risk of unwanted drug release behaviour can be significantly decreased if the dosage form shows the desired drug release not only under ‘average conditions’ but also under physiologically extreme conditions.
-
2.
The assessment of a food effect is based on the comparison with the fasted state, and thus, attention must be paid to the test conditions applied for simulation of the fasted state. Aspects such as gastric and intestinal fluid volumes, gastric residence time or gastric pH should represent the physiological situation in fasted state. Otherwise, drug release in fasted state may be either over- or underestimated, which would impact the assessment of food effects.
-
3.
The in vitro test should consider the protocol of the clinical trial. Parameters such as the caloric value and composition of the test meal, the time point of lunch, and further fluid intake can all affect the outcome of a clinical trial and ideally are considered by the in vitro test conditions. For instance, this can be done by the selection of an appropriate time for the simulation of gastric conditions.
Although in vitro test methods are valuable tools for formulation development, an oral ER dosage form should never be optimised to obtain the perfect in vitro profile. Instead, the aim should always be the best possible plasma concentration profile in vivo, and thus, the results from in vitro experiments need to be always critically assessed under consideration of the current understanding of human GI physiology. In this context, the application of physiologically based pharmacokinetic (PBPK) models can be very useful, as in silico tools such as GastroPlus™, PK-Sim® or Simcyp® allow to combine data form biorelevant in vitro experiments with human in vivo information. This combination of information from various sources can aid to enhance the comprehension of the effect of food intake on the in vivo performance of drug products administered in the fed state. The potential of this concept was nicely demonstrated in a recent work published by Andreas and colleagues, in which the negative food effect of zolpidem was successfully predicted by combing biorelevant in vitro testing with PBPK (Simcyp® and GastroPlus®) (78).
CONCLUSION
At the moment, it is impossible to define a strategy that will always be successful for predicting food effects for ER products. However, the combination of in vitro data obtained by standard and biorelevant dissolution test methods along with a thorough understanding of the in vivo behaviour (i.e. absorption, metabolism, elimination) of the drug as well as human GI physiology can aid to define the risk of possible food-drug interactions for oral ER dosage forms already during preclinical evaluation. The application of powerful in vitro tools allows the development and targeted optimisation of ER dosage forms that are robust towards the altered physiological conditions in the fed state.
References
Fleisher D, Li C, Zhou Y, Pao L-H, Karim A. Drug, meal and formulation interactions influencing drug absorption after oral administration: clinical implications. Clin Pharmacokinet. 1999;36(3):233–54.
Koziolek M, Grimm M, Schneider F, Jedamzik P, Sager M, Kühn JP, et al. Navigating the human gastrointestinal tract for oral drug delivery: uncharted waters and new frontiers. Adv Drug Deliv Rev. 2016;101:75–88.
Schug BS, Brendel E, Wolf D, Wonnemann M, Wargenau M, Blume HH. Formulation-dependent food effects demonstrated for nifedipine modified-release preparations marketed in the European Union. Eur J Pharm Sci. 2002;15(3):279–85.
Hendeles L, Weinberger M, Milavetz G, Hill M, Vaughan L. Food-induced “dose-dumping” from a once-a-day theophylline product as a cause of theophylline toxicity. Chest J. 1985;87(6):758–65.
Koziolek M, Garbacz G, Neumann M, Weitschies W. Simulating the postprandial stomach: physiological considerations for dissolution and release testing. Mol Pharm. 2013;10(5):1610–22.
Varum FJ, Hatton GB, Basit AW. Food, physiology and drug delivery. Int J Pharm. 2013;457(2):446–60.
Weitschies W, Blume H, Mönnikes H. Magnetic marker monitoring: high resolution real-time tracking of oral solid dosage forms in the gastrointestinal tract. Eur J Pharm Biopharm. 2010;74(1):93–101.
Newton JM. Gastric emptying of multi-particulate dosage forms. Int J Pharm. 2010;395(1–2):2–8.
Fadda H, McConnell E, Short MB, Basit AW. Meal-induced acceleration of tablet transit through the human small intestine. Pharm Res. 2009;26(2):356–60.
Coupe AJ, Davis SS, Evans DF, Wilding IR. Correlation of the gastric emptying of nondisintegrating tablets with gastrointestinal motility. Pharm Res. 1991;8(10):1281–5.
Khosla R, Davis SS. The effect of tablet size on the gastric emptying of non-disintegrating tablets. Int J Pharm. 1990;62(2–3):R9–11.
Khosla R, Feely LC, Davis SS. Gastrointestinal transit of non-disintegrating tablets in fed subjects. Int J Pharm. 1989;53(2):107–17.
Katsuma M, Watanabe S, Takemura S, Sako K, Sawada T, Masuda Y, et al. Scintigraphic evaluation of a novel colon-targeted delivery system (CODES™) in healthy volunteers. J Pharm Sci. 2004;93(5):1287–99.
Zimmermann T, Yeates RA, Laufen H, Pfaff G, Wildfeuer A. Influence of concomitant food intake on the oral absorption of two triazole antifungal agents, itraconazole and fluconazole. Eur J Clin Pharmacol. 1994;46(2):147–50.
Davis SS, Hardy JG, Taylor MJ, Whalley DR, Wilson CG. The effect of food on the gastrointestinal transit of pellets and an osmotic device (Osmet). Int J Pharm. 1984;21:331–40.
Rao SSC, Kuo B, McCallum RW, Chey WD, DiBaise JK, Hasler WL, et al. Investigation of colonic and whole-gut transit with wireless motility capsule and radiopaque markers in constipation. Clin Gastroenterol Hepatol. 2009;7(5):537–44.
Sarosiek I, Selover KH, Katz LA, Semler JR, Wilding GE, Lackner JM, et al. The assessment of regional gut transit times in healthy controls and patients with gastroparesis using wireless motility technology. Aliment Pharmacol Ther. 2010;31(2):313–22.
Koziolek M, Schneider F, Grimm M, Modeβ C, Seekamp A, Roustom T, et al. Intragastric pH and pressure profiles after intake of the high-caloric, high-fat meal as used for food effect studies. J Control Release. 2015;220(Part A):71–8.
Cassilly D, Kantor S, Knight LC, Maurer AH, Fisher RS, Semler J, et al. Gastric emptying of a non-digestible solid: assessment with simultaneous SmartPill pH and pressure capsule, antroduodenal manometry, gastric emptying scintigraphy. Neurogastroenterol Motil. 2008;20(4):311–9.
Ewe K, Press AG, Bollen S, Schuhn I. Gastric emptying of indigestible tablets in relation to composition and time of ingestion of meals studied by metal detector. Dig Dis Sci. 1991;36(2):146–52.
Davis SS. Formulation strategies for absorption windows. Drug Discov Today. 2005;10(4):249–57.
Deloose E, Janssen P, Depoortere I, Tack J. The migrating motor complex: control mechanisms and its role in health and disease. Nat Rev Gastroenterol Hepatol. 2012;9(5):271–85.
Garbacz G, Klein S, Weitschies WA. Biorelevant dissolution stress test device—background and experiences. Expert Opin Drug Deliv. 2010;7(11):1251–61.
Schneider F, Grimm M, Koziolek M, Modeß C, Dokter A, Roustom T, et al. Resolving the physiological conditions in bioavailability and bioequivalence studies: comparison of fasted and fed state. Eur J Pharm Biopharm. 2016;108:214–9.
Jain AK, Söderlind E, Viridén A, Schug B, Abrahamsson B, Knopke C, et al. The influence of hydroxypropyl methylcellulose (HPMC) molecular weight, concentration and effect of food on in vivo erosion behavior of HPMC matrix tablets. J Control Release. 2014;187:50–8.
Schulze K. Imaging and modelling of digestion in the stomach and the duodenum. Neurogastroenterol Motil. 2006;18(3):172–83.
Weitschies W, Wedemeyer RS, Kosch O, Fach K, Nagel S, Söderlind E, et al. Impact of the intragastric location of extended release tablets on food interactions. J Control Release. 2005;108(2–3):375–85.
Weitschies W, Friedrich C, Wedemeyer RS, Schmidtmann M, Kosch O, Kinzig M, et al. Bioavailability of amoxicillin and clavulanic acid from extended release tablets depends on intragastric tablet deposition and gastric emptying. Eur J Pharm Biopharm. 2008;70(2):641–8.
Kalantzi L, Goumas K, Kalioras V, Abrahamsson B, Dressman JB, Reppas C. Characterization of the human upper gastrointestinal contents under conditions simulating bioavailability/bioequivalence studies. Pharm Res. 2006;23(1):165–76.
Riethorst D, Mols R, Duchateau G, Tack J, Brouwers J, Augustijns P. Characterization of human duodenal fluids in fasted and fed state conditions. J Pharm Sci. 2015:1–10.
FDA. Guidance for industry: food-effect bioavailability and fed bioequivalence studies. 2002.
Koziolek M, Grimm M, Garbacz G, Kühn JP, Weitschies W. Intragastric volume changes after intake of a high-caloric, high-fat standard breakfast in healthy human subjects investigated by MRI. Mol Pharm. 2014;11(5):1632–9.
Diakidou A, Vertzoni M, Goumas K, Söderlind E, Abrahamsson B, Dressman J, et al. Characterization of the contents of ascending colon to which drugs are exposed after oral administration to healthy adults. Pharm Res. 2009;26(9):2141–51.
Vertzoni M, Markopoulos C, Symillides M, Goumas C, Imanidis G, Reppas C. Luminal lipid phases after administration of a triglyceride solution of danazol in the fed state and their contribution to the flux of danazol across Caco-2 cell monolayers. Mol Pharm. 2012;9(5):1189–98.
Litou C, Vertzoni M, Goumas C, Vasdekis V, Xu W, Kesisoglou F, et al. Characteristics of the human upper gastrointestinal contents in the fasted state under hypo- and a-chlorhydric gastric conditions under conditions of typical drug – drug interaction studies. Pharm Res. 2016;33(6):1399–412.
Mudie DM, Amidon GL, Amidon GE. Physiological parameters for oral delivery and in vitro testing. Mol Pharm. 2010;7(5):1388–405.
Grimm M, Koziolek M, Kühn J-P, Weitschies W. Interindividual and intraindividual variability of fasted state gastric fluid volume and gastric emptying of water. Eur J Pharm Biopharm. 2018;127(February):309–17.
Bergström CAS, Holm R, Jørgensen SA, Andersson SBE, Artursson P, Beato S, et al. Early pharmaceutical profiling to predict oral drug absorption: current status and unmet needs. Eur J Pharm Sci. 2014;57:173–99.
Porter CJH, Trevaskis NL, Charman WN. Lipids and lipid-based formulations: optimizing the oral delivery of lipophilic drugs. Nat Rev Drug Discov. 2007;6(3):231–48.
Koziolek M, Carrière F, Porter CJH. Lipids in the stomach—implications for the evaluation of food effects on oral drug absorption. Pharm Res. 2018;35(3):55.
Reppas C, Karatza E, Goumas C, Markopoulos C, Vertzoni M. Characterization of contents of distal ileum and cecum to which drugs/drug products are exposed during bioavailability/bioequivalence studies in healthy adults. Pharm Res. 2015;32(10):3338–49.
Koziolek M, Grimm M, Becker D, Iordanov V, Zou H, Shimizu J, et al. Investigation of pH and temperature profiles in the GI tract of fasted human subjects using the Intellicap® system. J Pharm Sci. 2015;104(9):2855–63.
Raman S, Polli JE. Prediction of positive food effect: bioavailability enhancement of BCS class II drugs. Int J Pharm. 2016;506(1–2):110–5.
Amidon GL, Lennernäs H, Shah VP, Crison JRA. Theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12(3):413–20.
Custodio JM, Wu C-Y, Benet LZ. Predicting drug disposition, absorption/elimination/transporter interplay and the role of food on drug absorption. Adv Drug Deliv Rev. 2008;60(6):717–33.
Siepmann J, Peppas NA. Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv Drug Deliv Rev. 2012;64(SUPPL):163–74.
Guiastrennec B, Söderlind E, Richardson S, Peric A, Bergstrand M. In vitro and in vivo modeling of hydroxypropyl methylcellulose (HPMC) matrix tablet erosion under fasting and postprandial status. Pharm Res. 2017;34(4):847–59.
Abrahamsson B, Albery T, Eriksson A, Gustafsson I, Sjöberg M. Food effects on tablet disintegration. Eur J Pharm Sci. 2004;22(2–3):165–72.
Williams HD, Nott KP, Barrett DA, Ward R, Hardy IJ, Melia CD. Drug release from HPMC matrices in milk and fat-rich emulsions. J Pharm Sci. 2011;100(11):4823–35.
Williams HD, Ward R, Hardy IJ, Melia CD. The effect of sucrose and salts in combination on the drug release behaviour of an HPMC matrix. Eur J Pharm Biopharm. 2010;76(3):433–6.
Davis J, Burton J, Connor AL, Macrae R, Wilding IR. Scintigraphic study to investigate the effect of food on a HPMC modified release formulation of UK-294,315. J Pharm Sci. 2009;98(4):1568–76.
Schug BS, Brendel E, Chantraine E, Wolf D, Martin W, Schall R, et al. The effect of food on the pharmacokinetics of nifedipine in two slow release formulations: pronounced lag-time after a high fat breakfast. Br J Clin Pharmacol. 2002;53(6):582–8.
Auiler JF, Liu K, Lynch JM, Gelotte CK. Effect of food on early drug exposure from extended-release stimulants: results from the Concerta®, Adderall XR™ food evaluation (CAFÉ) study. Curr Med Res Opin. 2002;18(5):311–6.
Schug BS, Brendel E, Wonnemann M, Wolf D, Wargenau M, Dingler A, et al. Dosage form-related food interaction observed in a marketed once-daily nifedipine formulation after a high-fat American breakfast. Eur J Clin Pharmacol. 2002;58(2):119–25.
Malaterre V, Ogorka J, Loggia N, Gurny R. Oral osmotically driven systems: 30 years of development and clinical use. Eur J Pharm Biopharm. 2009;73(3):311–23.
O’Reilly S, Wilson CG, Hardy JG. The influence of food on the gastric emptying of multiparticulate dosage forms. Int J Pharm. 1987;34(3):213–6.
Koziolek M, Garbacz G, Neumann M, Weitschies W. Simulating the postprandial stomach: biorelevant test methods for the estimation of intragastric drug dissolution. Mol Pharm. 2013;10(6):2211–21.
Vardakou M, Mercuri A, Barker SA, Craig DQ, Faulks RM, Wickham MSJ. Achieving antral grinding forces in biorelevant in vitro models: comparing the USP dissolution apparatus II and the dynamic gastric model with human in vivo data. AAPS PharmSciTech. 2011;12(2):620–6.
Schneider F, Beeck R, Hoppe M, Koziolek M, Weitschies W. In vitro simulation of realistic gastric pressure profiles. Eur J Pharm Sci. 2017;107:71–7.
Markopoulos C, Andreas CJ, Vertzoni M, Dressman JB, Reppas C. In-vitro simulation of luminal conditions for evaluation of performance of oral drug products: choosing the appropriate test media. Eur J Pharm Biopharm. 2015;93:173–82.
Baxevanis F, Kuiper J, Fotaki N. Fed-state gastric media and drug analysis techniques: current status and points to consider. Eur J Pharm Biopharm. 2016;107:234–48.
Berlin M, Ruff A, Kesisoglou F, Xu W, Wang MH, Dressman JB. Advances and challenges in PBPK modeling—analysis of factors contributing to the oral absorption of atazanavir, a poorly soluble weak base. Eur J Pharm Biopharm. 2015;93:267–80.
Diakidou A, Vertzoni M, Abrahamsson B, Dressman JB, Reppas C. Simulation of gastric lipolysis and prediction of felodipine release from a matrix tablet in the fed stomach. Eur J Pharm Sci. 2009;37(2):133–40.
Persson E, Gustafsson A-S, Carlsson A, Nilsson R, Knutson L, Forsell P, et al. The effects of food on the dissolution of poorly soluble drugs in human and in model small intestinal fluids. Pharm Res. 2005;22(12):2141–51.
Jantratid E, Janssen N, Reppas C, Dressman JB. Dissolution media simulating conditions in the proximal human gastrointestinal tract: an update. Pharm Res. 2008;25(7):1663–76.
Georgaka D, Butler J, Kesisoglou F, Reppas C, Vertzoni M. Evaluation of dissolution in the lower intestine and its impact on the absorption process of high dose low solubility drugs. Mol Pharm. 2017;14(12):4181–91.
Andreas CJ, Chen YC, Markopoulos C, Reppas C, Dressman J. In vitro biorelevant models for evaluating modified release mesalamine products to forecast the effect of formulation and meal intake on drug release. Eur J Pharm Biopharm. 2015;97:39–50.
Franek F, Holm P, Larsen F, Steffansen B. Interaction between fed gastric media (Ensure Plus®) and different hypromellose based caffeine controlled release tablets: comparison and mechanistic study of caffeine release in fed and fasted media versus water using the USP dissolution apparatus 3. Int J Pharm. 2014;461(1–2):419–26.
Klein S. Predicting food effects on drug release from extended-release oral dosage forms containing a narrow therapeutic index drug. Dissol Technol. 2009;8:28–40.
Fadda HM, Merchant HA, Arafat BT, Basit AW. Physiological bicarbonate buffers: stabilisation and use as dissolution media for modified release systems. Int J Pharm. 2009;382(1–2):56–60.
Garbacz G, Kolodziej B, Koziolek M, Weitschies W, Klein S. An automated system for monitoring and regulating the pH of bicarbonate buffers. AAPS PharmSciTech. 2013;14(2):517–22.
Sheng JJ, McNamara DP, Amidon GL. Toward an in vivo dissolution methodology: a comparison of phosphate and bicarbonate buffers. Mol Pharm. 2009;6(1):29–39.
Shibata H, Yoshida H, Izutsu KI, Goda Y. Use of bicarbonate buffer systems for dissolution characterization of enteric-coated proton pump inhibitor tablets. J Pharm Pharmacol. 2016;68(4):467–74.
Koziolek M, Görke K, Neumann M, Garbacz G, Weitschies W. Development of a bio-relevant dissolution test device simulating mechanical aspects present in the fed stomach. Eur J Pharm Sci. 2014;57:250–6.
Chessa S, Huatan H, Levina M, Mehta RY, Ferrizzi D, Rajabi-Siahboomi AR. Application of the dynamic gastric model to evaluate the effect of food on the drug release characteristics of a hydrophilic matrix formulation. Int J Pharm. 2014;466(1–2):359–67.
Tenjarla S, Romasanta V, Zeijdner E. Release of 5-aminosalicylate from an MMX mesalamine tablet during transit through a simulated gastrointestinal tract system. Adv Ther. 2007;24(4):826–39.
Bellmann S, Lelieveld J, Gorissen T, Minekus M, Havenaar R. Development of an advanced in vitro model of the stomach and its evaluation versus human gastric physiology. Food Res Int. 2016:1–8.
Andreas CJ, Pepin X, Markopoulos C, Vertzoni M, Reppas C, Dressman JB. Mechanistic investigation of the negative food effect of modified release zolpidem. Eur J Pharm Sci. 2017;102:284–98.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: Sandra Klein
Rights and permissions
About this article
Cite this article
Koziolek, M., Kostewicz, E. & Vertzoni, M. Physiological Considerations and In Vitro Strategies for Evaluating the Influence of Food on Drug Release from Extended-Release Formulations. AAPS PharmSciTech 19, 2885–2897 (2018). https://doi.org/10.1208/s12249-018-1159-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-018-1159-0