Abstract
Understanding inter-subject variability in drug pharmacokinetics and pharmacodynamics is important to ensure that all patients attain suitable drug exposure to achieve efficacy and avoid toxicity. Inter-subject variability in the pharmacokinetics of therapeutic monoclonal antibodies (mAbs) is generally moderate to high; however, the factors responsible for the high inter-subject variability have not been comprehensively reviewed. In this review, the extent of inter-subject variability for mAb pharmacokinetics is presented and potential factors contributing to this variability are explored and summarised. Disease status, age, sex, ethnicity, body size, genetic polymorphisms, concomitant medication, co-morbidities, immune status and multiple other patient-specific details have been considered. The inter-subject variability for mAb pharmacokinetics most likely depends on the complex interplay of multiple factors. However, studies aimed at investigating the reasons for the inter-subject variability are sparse. Population pharmacokinetic models and physiologically based pharmacokinetic models are useful tools to identify important covariates, aiding in the understanding of factors contributing to inter-subject variability. Further understanding of inter-subject variability in pharmacokinetics should aid in development of dosing regimens that are more appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
High inter-subject variability has been reported for monoclonal antibody (mAb) pharmacokinetics. |
The causes of inter-subject variability in mAb pharmacokinetics are often unexplained or unexplored in clinical studies. |
The physiological reasons for inter-subject variability in mAb pharmacokinetics are still poorly understood and further investigation is required. |
1 Introduction
Optimal drug dosing requires an understanding of the inter-subject variability in drug pharmacokinetics and pharmacodynamics to ensure efficacy and to minimise toxicity in all patients. Information on variability in the pharmacokinetics of therapeutic monoclonal antibodies (mAbs) is still emerging [1]. For example, trough concentrations following multiple dosing of palivizumab, cetuximab and infliximab differed by <10.9-, 18.2- and >70-fold between subjects, respectively [2–4]. The clearance of endogenous immunoglobulin also varies widely between populations, with the reported elimination half-life (t ½) ranging from 13 to 32 days in healthy subjects and 7 to 68 days in patients with various diseases [5–8]. Observed variability in the pharmacokinetics of selected mAbs are presented in the Electronic Supplementary Material.
A multitude of factors can play a role in the observed inter-subject variability in mAb pharmacokinetics, many of which are still poorly defined. There have been limited reports dedicated to describing the sources of variability for mAb pharmacokinetics [9–11]. The properties governing exposure to mAbs can be broadly divided into the same areas as small-molecule drugs, i.e. absorption, distribution, metabolism and elimination (ADME). However, the ADME of mAbs differs from that of small-molecule drugs and has been reviewed extensively [1, 9, 10, 12]. The aim of this study is to provide a comprehensive review of the factors that may contribute to the observed high inter-subject variability in mAb pharmacokinetics.
2 Data Sources
PubMed was used to conduct a structured literature search on the ADME of mAbs. The aim of the search was to identify pharmacokinetic parameters that could vary between subjects and the factors that influence this variability. Clinical studies as well as population pharmacokinetic studies were included. No date restriction was applied. Additional sources of information included the manufacturers’ product information as well as Simcyp data resources.
3 Factors Contributing to Inter-Subject Variability in Monoclonal Antibody (mAb) Pharmacokinetics
Body weight/surface area has been correlated with linear clearance of mAbs, suggesting that smaller subjects clear mAbs more slowly than larger individuals [13]. However, the impact of other demographic factors such as age, sex, and renal or hepatic impairment on mAb pharmacokinetics is controversial [14]. Age has been inversely correlated with clearance of adalimumab [15] and efalizumab [16]; however, no correlation has been reported for trastuzumab or bevacizumab [14]. In addition, age, sex, disease status, baseline IgG, rheumatoid factors and serum antigen levels were not correlated with differences in the clearance of an anti-interleukin (IL)-8 antibody [14]. Alteration in mAb clearance between ethnic groups [10] and sexes [17, 18] have been reported, but these may be explained by differences in body weight [13, 18]. Various stages and processes during ADME of mAbs present the potential for inter-subject variability. These are depicted in Fig. 1 and discussed below.
3.1 Lymph and the Interstitial Fluid
The rate of lymph flow influences mAb distribution and the rate of absorption following subcutaneous or intramuscular administration. In addition, the volume of lymph may have an impact on the apparent volume of distribution at steady state (V ss) of mAbs, where distribution is confined to the blood, lymph and interstitial space. There are multiple factors that may lead to differences in the lymph flow rate and/or volume between subjects. However, data relating to inter-subject variability in lymph flow and volume are scarce. Lymph flow rate and volume are altered in several disease conditions such as rheumatoid arthritis (RA) and cancers [19–26], and hence differences in the co-morbidities of the patients may contribute to inter-subject variability in mAb pharmacokinetics. No data could be found directly comparing lymph flows or volumes in males and females. The blood flow to and number and size of cervical lymph nodes are reported to be similar in Chinese and Caucasian adults [27]. However, inter-subject differences in pharmacokinetics due to ethnicity- and sex-dependent lymph flow rate and volume cannot be ruled out.
Decreased lymph flow has been observed in older adults [28–30]. However, little is currently known about differences in subcutaneous lymph drainage between adults and children and the resultant impact on absorption rate and bioavailability of mAbs [31, 32]. It has been suggested that the biodistribution of therapeutic proteins (TPs) may not be significantly affected by developmental changes in body composition [31, 33]. However, total body water decreases with age in young children, due to a sharp reduction in interstitial fluid volume [34–36], and hence the absorption rate of mAbs may be higher in very young children than in adolescents and adults, as observed for palivizumab [37]. Body weight-normalised mAb V ss may also be higher in young children due to the higher interstitial fluid volume in paediatric patients [32, 34–36].
For subcutaneous dosing, the site and depth of injection can influence the absorption and distribution of the mAb [38, 39]. Therefore, inconsistencies in dosing between individuals may contribute to the observed variability in the time to maximum concentration (t max) and the maximum concentration (C max). The extent of absorption generally does not differ significantly between dosing sites [40], but the rate of absorption may vary. Regional differences in blood and/or lymph flow may contribute to this variability. Exercise, heating and rubbing also increase the local lymph flow rate [41, 42]. In addition, as the rate of distribution within the interstitial space following dose administration is dictated by molecular size and physical and electrostatic interaction with the various components of the interstitium (e.g. fibrous collagen network and glycosaminoglycanes) [10, 43, 44], regional alterations in the structure of the interstitium may also contribute to variability in mAb absorption from different dosing sites. Population pharmacokinetic studies following subcutaneous administration of various mAbs (efalizumab, denosumab, omalizumab, ustekinumab) indicated high between-subject variability in bioavailability and the absorption rate constant, with coefficient of variation (CV) percentages ranging from 40 to 53 % [45–49].
3.2 Movement of mAbs Through the Endothelial Wall
As convection is the main driving force for distribution of mAbs from the capillaries into the interstitial space, any differences in the endothelial pore size, their abundance and the structure of the glycocalyx layer between subjects may contribute to inter-subject variability in mAb absorption and distribution. Reduced V ss and clearance of mAbs may be observed in the elderly due to a reduction in the number of liver endothelial fenestrae, a decrease in endocytosis in the liver endothelium and reduced penetration of mAbs into the liver endothelial cells [50]. Developmental changes in the abundance of receptors, such as low-density lipoprotein receptor-related proteins, asialoglycoprotein receptors and mannose receptors, which are responsible for endocytosis of certain TPs in the liver, have been reported [51–53] and can lead to reduced clearance in newborn infants compared with older children and adults. Currently, there are no reports describing paracellular movement of mAbs in different ethnicities [10] or sexes. Data describing the size and abundance of pores in endothelial membranes is currently very limited [54].
Inter-subject variability in the distribution of radiolabelled IgG has been reported in healthy subjects and patients with a range of diseases [6]. Disease conditions can disrupt the endothelial membrane, e.g. the glycocalyx is shed in inflammation and ischaemia, which will increase the endothelial permeability and distribution of mAbs [10, 55]. In addition, disease conditions can alter the glycosaminoglycan composition of the glycocalyx [55] and hence the movement of proteins through the endothelial membranes. New blood vessel formation at the site of inflammation may contribute to the apparent increased vascular permeability of mAbs in inflammatory disease [56]. Disease has also been shown to change the abundance of asialoglycoprotein receptors on hepatocytes and hence endocytosis [57–59]. It is reasonable to assume that disease state may also affect endocytosis and thus clearance of mAbs. Disruption of the glomerular or intestinal membrane in disease can lead to increased renal filtration or loss from the intestine [15, 26].
Individual variation in tumour anatomy, physiology and antigen load may influence the local distribution of mAbs between cancer patients. The hydrostatic pressure in the interstitial fluid of tumours is raised and highly variable, leading to reduced distribution of mAbs into the tumour interstitium [60, 61]. A high concentration of the target antigen on the cells at the surface of the tumour can also lead to a ‘binding barrier’, where antigen on the peripheral tumour cells binds to the mAb and prevents distribution of the drug further into the interior of the tumour, resulting in heterogeneous distribution of mAbs in tumours [9, 62, 63]. Differences in antigen concentration on tumour cells between patients may therefore lead to variability in local mAb distribution.
3.3 Neonatal Fc-Receptor Binding and Abundance
The neonatal Fc-receptor (FcRn) is important for absorption of IgG in the suckling rat, accounting for approximately 80 % of the circulating IgG concentration in rat pups [64, 65]. FcRn expression in the gut and absorption of enteral administered IgG changes with age in young rats [65]. In contrast, FcRn is expressed in the gut throughout adulthood in primates [66]. FcRn expression in the gut has only been determined qualitatively in adult and fetal humans [67, 68]. Changes in FcRn abundance with age could contribute to variability in mAb pharmacokinetics between young and adult subjects; however, the limited data available suggests this may only be important in very early childhood. Infants have lower serum IgG concentrations and a prolonged t ½ of IgG absorbed from the mother (~48 days [69]) than adult values. Therefore, therapeutic mAbs may also have lower clearance in children [26, 31]. Total clearance of mAbs generally increases in a sub-proportional manner when compared with body weight (i.e. the increase in clearance is greater than the proportional increase in body weight); hence, dosage of mAbs on a mg/kg basis results in lower exposure in paediatric patients than in adults [31]. This suggests that the non-specific catabolic clearance of mAbs varies with age, potentially because of the ontology of FcRn abundance. Unfortunately, there is very limited pharmacokinetic data published for mAbs in very young paediatric patients (<2 years) to allow confirmation of this. There are no reports of FcRn abundance in elderly subjects and hence its importance for mAb pharmacokinetic variability in studies that include elderly patients cannot currently be assessed.
Several disorders affect the elimination of endogenous IgG [26], e.g. the serum and lymph concentration of endogenous IgG is 1.6- and 1.9-fold higher in RA patients than in healthy volunteers [19]. High IgG concentrations correlate with faster elimination of IgG, presumably due to saturation of FcRn, and consequently reduced protection from catabolism [26, 70]. Therefore, in disorders where endogenous IgG concentrations are high, the t ½ of endogenous IgG is short [26]. A similar reduction in mAb t ½ values would be expected in patients with high endogenous IgG levels and saturated FcRn receptors. In addition, increasing the dose for subcutaneous administration may lead to saturation of FcRn binding and subsequent protection from degradation at the absorption site [38, 39].
Currently, the absolute abundance of FcRn and its variability in the population is unknown [71]. The first quantitative study of human FcRn messenger RNA and protein abundance in the intestine showed high inter-subject variability and also differences in regional expression along the gut [66]. However, tissue from only three donors was analysed. Polymorphisms affecting critical amino acids (E115, E116, D130, W131, L135 and I1, in the α2 domain of human FcRn) necessary for binding to IgG [72] will lead to inter-subject differences in the binding affinity of FcRn to mAbs and consequently differences in clearance [73]. In addition, polymorphisms of the FcRn gene leading to reduced transcription or translation will result in lower FcRn abundance. A non-synonymous mutation of B2M leads to a lack of functional FcRn [74]. This causes reduced serum IgG (<28 % of normal), due to an increase in catabolism, rather than a decrease in protein synthesis [26]. These patients showed a much faster IgG elimination rate than healthy individuals. Thirty-three genetic variants of the FcRn gene have been identified in the Japanese population, with the prevalence of some polymorphism differing between Japanese and Caucasian populations [75]. However, the majority of the polymorphisms identified in Japanese subjects were at locations distinct from the IgG binding region and hence are not expected to cause differences between subjects in FcRn binding capacity [75]. Although binding affinity may not be altered due to these polymorphisms, it is unclear whether other changes such as alterations in protein stability, turnover or transport within the cell could occur and influence the efficiency of the FcRn recycling mechanism. Ethnic differences in FcRn-mediated clearance of endogenous IgG have been observed; however, these can generally be explained by differing body size [10].
3.4 Target Levels
The pharmacokinetics of mAb are often non-linear, where clearance is lower at higher dose levels due to saturation of the target, and hence the target-mediated drug disposition (TMDD) elimination pathway [46, 76]. Inter-subject differences in target abundance may therefore affect the distribution and elimination of mAbs where TMDD has a large impact on their disposition. Increased target levels are usually found in patients compared with healthy volunteers, and hence the importance of TMDD to mAb pharmacokinetics at a set dose level may differ between the two populations. In addition, differences in target levels between disease types, e.g. RA and inflammatory bowel disease, may lead to variability in mAb clearance between patients [77, 78].
Many currently approved mAbs are targeted against antigens where a circulating form is present in the bloodstream in addition to the membrane-bound antigen; for example, trastuzumab, which targets HER2 in the primary tumour and circulating tumour cells, and rituximab, which is directed against transmembrane and plasma CD20 [79]. Indeed, it has been hypothesised that most membrane-bound proteins shed their ectodomains [80]. The shed form of the target in the systemic circulation may bind to the mAb and reduce the number of antigen binding sites available to bind to the cell surface target, reducing efficacy [79, 81, 82]. Due to the increased total target levels (membrane bound and soluble), non-linear pharmacokinetics may be observed at higher dose levels. Increased soluble target levels are usually found in patients compared with healthy volunteers; thus, the importance of TMDD to mAb pharmacokinetics may differ between the two populations. In addition, soluble antigen levels are often highly variable in patients and for certain conditions are correlated with disease progression [79, 81–85]. In accordance, mAb exposures are often lower and clearance is higher in patients than in healthy volunteers [78, 82, 84–87].
Small differences in protein structure/post-translational modifications can affect the binding affinity of mAbs to their target antigen, e.g. glycosylation [10, 88]. These may occur during production or as a result of the patient’s disease state. The majority of mAb formulations are not homogeneous and instead contain proteins with varying post-translational modifications, which could contribute to variability in mAb pharmacokinetics between subjects administered different amounts of drug. Binding affinity of mAbs and internalisation/elimination rates of the bound mAb–target complex are usually determined in vitro or can be allometrically scaled from pre-clinical data; hence, the extent and impact of inter-subject variability on mAb pharmacokinetics cannot be assessed. In addition, changes in the target protein due to polymorphisms are likely to influence TMDD and efficacy of mAbs [11]. However, supportive data are extremely limited. A recent study demonstrated a significant impact of IL-6 receptor single nucleotide polymorphisms on tocilizumab efficacy [89]. Unfortunately, tocilizumab pharmacokinetic data were not reported, and hence the importance of target polymorphisms on inter-subject variability in mAb pharmacokinetics cannot be assessed.
Data on the differences in target-mediated clearance of therapeutic mAbs in paediatric patients compared with adults are lacking [31]. In addition, differences in target levels between sexes or ethnic groups and the impact on mAb TMDD have not been widely studied. No difference in sCD20 levels were observed between male and female chronic lymphocytic leukaemia patients with various stages of disease [81]. However, it is unknown whether this may apply to other diseases.
Although target levels are highly variable [90, 91], this may not always be the cause of high variability in mAb pharmacokinetics. Mean serum tumour necrosis factor (TNF)-α levels were 0.0034 ± 0.00018 versus 0.0011 ± 0.00006 pmol/L in early RA patients and age- and sex-matched healthy donors, respectively [92]. Several mAbs directed against TNF-α have been approved for treating RA patients. At recommended therapeutic doses, the mean steady-state trough concentrations for adalimumab ranged from ~60 to 80 nmol/L [15], and from 3 to 5 nmol/L for golimumab [60]. Trough concentrations of infliximab were more variable, with a reported range of <0.1–80 nmol/L in 84 RA patients [77]. The trough concentration of adalimumab, golimumab and infliximab are therefore in significant molar excess to TNF-α levels, and hence the higher pharmacokinetic variability observed for infliximab is not likely to be due solely to inter-patient differences in target levels [79]. However, pre-treatment TNF-α levels were significantly correlated with infliximab serum trough concentrations in RA patients in another study [91]. Due to the importance of target levels for mAb clearance for certain indications, assessment of target levels in the population of interest is recommended.
3.5 Immunogenicity
Antidrug antibody (ADA) formation is highly subject dependent and is thought to be a major contributor to the high inter-subject variability observed for mAb clearance [99]. The patient’s immune status, genetic background, underlying disease, previous exposure to mAbs and concomitant medication may influence the potential for ADA production (Table 1). Reported ADA incidences can vary substantially, even for the same product within the same disease population. mAb trough concentrations as well as efficacy are reported to be lower and clearance is higher in ADA-positive patients [18, 93–96]. It should be noted that due to the current limitations in the bioanalytical methods available for quantification of ADA it is difficult to compare ADA effects between different studies and mAbs [31, 97, 98].
The immune response to mAbs at any one time is likely to be polyclonal, where multiple ADA species are produced, with variable concentrations, affinities and directed against different epitopes on the mAb, eliciting different responses [99]. These multiple ADA species may have differing impacts on mAb pharmacokinetics and the net effect of the combination of these different ADA species will be observed [99]. Hence, differences in the production of specific ADA species can contribute to inter-subject variability for ADA-dependent mAb clearance. Not only are ADA levels highly variable between subjects, they can also be transient (occurring anytime during treatment and disappearing again spontaneously), further adding to the potential to contribute to mAb clearance variability [100, 101]. ‘Affinity maturation’ leads to production of ADA with higher binding affinity over time and with repeated drug administration, therefore increasing mAb clearance over time [97] and potentially contributing to variability in mAb pharmacokinetics between patients at different stages of treatment.
Factors relating to the drug formulation (aggregates, contaminants, etc.) and the structure of the mAb (e.g. glycosylation) may also affect immunogenicity potential and contribute to the variability in ADA-dependent clearance of mAbs as evident from Table 1. Production processes can influence the extent of glycosylation, impurities and aggregation of mAbs, which in turn can lead to differences in clearance by reticuloendothelial system and ADA production [98, 102, 103]. Approximately 0.1 % of patients suffer anaphylaxis when treated with omalizumab, although the exact mechanism has not been elucidated. Interestingly, the polysorbate excipient used in the formulation has been linked to hypersensitivity reactions [104, 105]. In addition, formulations of mAbs are not pure and instead contain multiple isomers of the TP (due to production processes). Each isomer may have slight differences in its pharmacokinetics and ADA potential, and hence administration of different formulations may add to the observed inter-subject variability. Without proper controls, variability due to these external factors may appear to be inter-subject variability.
A patient’s disease status can influence the immune response towards a specific mAb. Healthy subjects display immune tolerance, where their immune system has developed the ability to ignore minor differences in proteins and hence less immunogenicity would be anticipated. On the other hand, patients with a missing gene may also lack the immune tolerance towards that protein and would have increased immunogenicity to the TP [98]. In patients with certain diseases, the immune system is already activated or suppressed and can influence the likelihood of ADA production [99, 106]. Indeed, induction of post-treatment ADA is more prevalent in disease populations, particularly RA patients [107]. In contrast, cancer patients are less likely than patients with other diseases to produce ADA due to their immune systems being depressed by the disease or chemotherapy [108].
Pre-existing ADA, observed for several mAbs, have been linked to differences in mAb pharmacokinetics, toxicity and efficacy [107]. However, induction of post-treatment ADA is generally not linked to pre-existing ADA [101]. Patients who had previously been treated with infliximab and produced anti-infliximab antibodies were more likely to also produce ADA again and have reduced efficacy when treated with adalimumab, which suggests a genetic predisposition for the immune response [108, 109]. However, due to the inconsistencies between reports, the importance of pre-existing antibodies for mAb pharmacokinetic variability is not clear.
Compared to adults and older children, newborns have a limited capacity to produce an immune response [32, 110]. Notably, higher ADA incidence was observed in children than in adults (with the same or adult version of the disease) for adalimumab, abatacept and daclizumab, while similar ADA incidences in children and adults were reported for etanercept, infliximab and tocilizumab [31]. Inclusion of paediatric patient data may therefore increase the inter-subject variability in clearance of certain mAbs. However, differences in the design of adult and paediatric studies and improvements in assay sensitivity prior to the paediatric studies commencing may contribute to the apparent increased abundance of ADA in paediatric patients [31]. In addition, the lower mAb concentrations in paediatric patients than in adult subjects is likely to cause less assay interference with ADA detection [31]. The limited availability of immunogenicity data for mAbs in paediatric patients and issues with the current bioanalytical methods for ADA detection prevents definitive assessment of the impact of age on inter-subject variability in immunogenicity-dependent mAb clearance.
3.6 Fcγ Abundance
The expression of the Fcγ receptors (FcγRs) on various cell types is heterogenous and the receptors display varied affinity and specificity for different IgG isotypes [14, 111]. In addition, genetic polymorphisms of the FcγRs vary the abundance and/or alter the affinity of FcγR binding to IgG (Table 2). Psoriasis patients with the low-affinity FcγRIIIa genotype (FcγRIIIa-176F, also known as FcγRIIIa-158F) had a better response to anti-TNF therapy following 3 months of treatment. This may in part be due to lower FcγR-mediated mAb clearance in patients with the low-affinity alleles, and hence higher mAb concentrations and efficacy over time [112, 113]. The FcγRIIIa-176F polymorphism reduces the affinity for IgG compared with the wild-type gene (FcγRIIIa-176V, also known as FcγRIIIa-158V) and hence mAb clearance may also be reduced. Accordingly, a slower elimination rate was observed for infliximab in patients with the low-affinity allele (>245 vs 160 h) [114, 115]. The impact of the FcγRIIIa genotype on the elimination of infliximab may be twofold: increased affinity for FcγRIIIa leads to increased elimination of infliximab by the reticuloendothelial system and also an increase in recruitment of cytotoxic cells by infliximab bound to TNF-α-expressing cells, leading to increased cell lysis and elimination of infliximab via TMDD [115]. Presence of high- or low-affinity FcγR alleles may increase or decrease the elimination of mAbs, respectively, and hence contribute to inter-subject variability in mAb clearance.
Ethnic differences in the distribution of FcγR polymorphisms have been reported (refer to Table 2) but the impact on mAb pharmacokinetics is currently unknown [10, 111]. Therefore, inclusion of subjects from different ethnicities may lead to inter-subject variability in FcγR-dependent mAb pharmacokinetics. Expression of FcγRs may also vary with age and sex. Abundance of inhibitory Fcγ receptor FcγRIIb-positive B cells is similar in male and female RA patients [116]. However, the expression of FcγRIIb on these B cells was significantly lower in women than in men with RA (~40 %) [116]. Age-related changes in the populations of mature immune cells expressing FcγR have been shown in early life [110]. In addition, expression of FcγRIIb decreased with increasing age in women but not in men [116]. Abundance of FcγRs also differs in disease. RA patients have significantly lower numbers of B cells, with decreased expression of inhibitory FcγRIIb, than the healthy controls [116]. In contrast, patients with juvenile idiopathic arthritis have increased numbers of monocytes, with higher expression of activating FcγRII and FcγRIII, compared with age- and sex-matched healthy controls [117]. Thermal injury and injection of endotoxins has been shown to reduce the FcγR-mediated uptake of IgG-coated erythrocytes by Kuppfer cells in the liver, both in vivo and in vitro [118]. Hepatic impairment or injury may therefore lead to decreased expression/functionality of FcγR and consequently differences in mAb clearance [13]. Variability in expression levels of FcγRs in tumours, the liver and the general immune system between individual patients with differing disease states may influence mAb exposure and efficacy [119].
3.7 Disease
Renal impairment is not anticipated to influence mAb clearance due to the high molecular weight of mAbs (unless renal impairment affects target levels) [120]; however, other disease conditions may contribute to differences in mAb pharmacokinetics. For example, population pharmacokinetic studies in patients with kidney [121] and liver [122] transplants indicated that the basiliximab clearance was faster in liver recipients. This may be due to the additional route of basiliximab clearance through drained ascites fluid in liver transplant patients [122, 123]. In addition to the influence of disease on factors such as target abundance, immune status and lymph flow, disease status has also been shown to impact mAb pharmacokinetics in other ways. Increased circulating thyroxine in experimental animals is correlated with an increase in the catabolic clearance of IgG; similarly, hypermetabolism due to fever and infection has been associated with increased IgG catabolism in man [26]. A decrease in mAb t ½ from 182.3 ± 28.2 to 59.4 ± 14.9 h, in combination with increased endogenous IgG concentrations, has been reported in mice with induced lupus, which is thought to be due to an alteration in IgG-FcRn binding or in the FcRn recycling mechanism [124]. In subjects with normal IgG levels, inter-subject variability in endogenous IgG concentrations is not expected to have an impact on mAb elimination as the doses of mAbs usually administered are too low to increase the total IgG concentration to a level where its elimination is increased [14]. Endogenous IgG concentrations are raised and highly variable in inflammatory conditions; however, even in such patients a correlation between steady-state mAb clearance and the serum IgG concentration was not found [14], again suggesting that the impact of disease on mAb clearance may not be due to saturation of FcRn protection.
Measures of disease activity in RA and ankylosing spondylitis patients were correlated with mAb exposure and efficacy [15, 125, 126], although similar findings were not reported in all studies [14]. Target levels were not measured in these studies. Although increased target levels with disease severity may be the reason for the increased clearance, other physiological and biochemical variations associated with differences in disease status cannot be ruled out. Physical performance and disease severity scores (assessed using scoring systems such as the Karnofsky Performance Scale, the Psoriasis Area and Severity Index [PASI] and the Bath Ankylosing Spondylitis Disease Activity Index) are commonly evaluated as covariates in population pharmacokinetic studies of mAbs used in areas of oncology and immunology [127–130].
In clinical trials, where the inclusion of subjects with fever, underlying infections and disease status is tightly controlled, variability due to these factors may not be noticeable. For example, blood chemistry tests related to hepatic and renal function were often evaluated as potential covariates in the population pharmacokinetic analyses but were rarely identified as relevant covariates. Interestingly, population pharmacokinetic analysis of infliximab, pertuzumab and ustekinumab in patients found that albumin was a negative predictor of clearance [131–133]. In addition to IgG, FcRn also binds and protects albumin from intracellular catabolism, thereby playing an important role in the homeostasis of both IgG and albumin [134, 135]. The binding site of albumin is distinct from that for IgG and hence their binding is non-competitive [134, 135]. The authors of the infliximab analysis suggested that a higher albumin concentration could be an indicator of an increased number of FcRns and a related reduction in the infliximab t ½ [131]; however, several other factors may also alter albumin levels.
In general medical use and larger phase III studies, patient co-morbidities may vary widely and contribute to the inter-subject variability in mAb pharmacokinetics. A number of co-morbidities, including diabetes mellitus, hypertension and hyperlipidaemia, were investigated as covariates in a population pharmacokinetic analysis of ustekinumab in psoriasis patients [133]. This study found that patients with diabetes had 28.7 % faster clearance and a 13.2 % larger V ss. The reason behind the effect of diabetes on the pharmacokinetics of ustekinumab is uncertain, but the authors suggested that altered lymphatic flow and particle transport, altered capillary permeability, increased interstitial fluid volume and accelerated clearance of the antibody resulting from increased glycation, could be potential mechanisms [133]. The potential effect of cancer type was investigated in a population pharmacokinetic analysis of panitumumab in patients with various solid tumours [38]. Patients with non-small-cell lung cancer or other types of cancer had ~13–14 % lower clearance than patients with colorectal or renal cancer [136]. The reason for the difference in clearance between the different types of cancer is unclear.
Time or the duration of treatment may be related to the target level if administration of a mAb results in down-regulation of its target over time. A population pharmacokinetic/pharmacodynamic analysis in patients with chronic B cell lymphocytic leukaemia found that alemtuzumab exhibited non-linear clearance attributable to saturation of target-mediated clearance mechanisms [137]. The white blood cell (WBC) count was found to influence the pharmacokinetics of alemtuzumab, and was a strong positive predictor of the maximum capacity of the target (V max). Alemtuzumab exhibited both time- and concentration-dependent clearance [137]. The WBC counts decreased following repeated administration of alemtuzumab. This might be expected, as alemtuzumab targets CD52, an antigen present on the cell surface of WBCs (including lymphocytes and monocytes). Reduction of the WBC count after alemtuzumab treatment leads to a corresponding reduction in CD52 density within the body and hence a change in V max, a parameter associated with the non-linear target-mediated clearance rather than linear catabolic clearance.
3.8 Concomitant Medication
In general, variability in mAb concentrations due to other concomitant medications is relatively low when compared with small molecules, although concentrations of small molecules may be influenced by mAbs by means of reversing cytokine (i.e. IL-6)-mediated suppression of cytochrome P450 (CYP) activities in inflammatory disease conditions [138, 139]. For example, decreased exposure of simvastatin and omeprazole by 57 and 28 %, respectively, after co-administration with tocilizumab has been reported in patients with RA [140]. Similarly, there was a decrease in the area under the plasma concentration–time curve for midazolam, omeprazole and S-warfarin by 30–35, 37–45 and 18–19 %, respectively, after sirukumab administration in patients with RA [138]. The drug interactions mediated by cytokines and the potential impact of other endogenous substances on drug-metabolising enzymes have been reviewed in depth [141–145] and hence are not in the scope of this review.
Examples of clinically observed drug interactions where the mAb is the victim have also been reported. Altered clearance of mAbs may result from changes in the target levels due to the concomitant medication, modulation of FcγR expression, altered immunogenicity by a mAb or small molecule, and altered catabolic clearance [146, 147]. Some evidence exists suggesting an impact of immunosuppressive agents on mAb pharmacokinetics, possibly due to an alteration in the target (expression or cell number) and/or reduced immunogenicity. An apparent decrease in mAb clearance was noted when methotrexate was concomitantly administered with infliximab [148] and adalimumab [15]. It should be noted that the patients treated with concomitant methotrexate had a lower rate of ADA development than patients on adalimumab monotherapy (1 vs. 12 %). The higher incidence of adalimumab ADA resulted in higher clearance of adalimumab, which was reduced during co-administration with methotrexate, although a possible role of the FcγR in this interaction cannot be ruled out. It is worth noting that a down-regulation of FcγR by methotrexate is observed in patients with RA, which may affect mAb clearance during combination treatment [146–149]. Administration of methotrexate in combination with infliximab has been shown to markedly suppress the inflammatory disease activity in RA patients and the combination therapy also appears to promote immunologic tolerance to infliximab therapy [148]. Similarly, a combination of azathioprine and cyclosporine (ciclosporin) or mycophenolate and cyclosporine decreased the clearance of basiliximab by 22 and 51 %, respectively [122]. Drug interactions could be possible via altered expression of target levels by small molecules, e.g. administration of paclitaxel in combination with trastuzumab resulted in a 1.5-fold increase in trastuzumab serum concentrations [150]. This type of interaction could be possible via both drugs competing for the same target; however, the mechanism remains to be fully elucidated. To date, there has been no evidence of any clinical TP drug interactions via altered catabolic clearance pathways. This is a high capacity clearance pathway for mAbs and is unlikely to be affected by small molecules.
There appears to be limited evidence of drug interactions mediated by non-specific clearance mechanism for mAbs in combination, e.g. there was no alteration in pharmacokinetics when rituximab was combined with bevacizumab [151]. In contrast, tumour uptake of trastuzumab was decreased with concomitant administration of an anti-VEGF antibody. However, mechanistic studies suggest that the observed changes in tumour uptake were attributable to the reduction in both tumour blood flow and vascular permeability to macromolecules [152] rather than changes to non-specific clearance. Understanding many of these pharmacokinetic drug interaction mechanisms is still evolving and an in-depth understanding of the clearance pathways involved in the disposition of victim drugs and the pharmacological effects of perpetrator drugs in the specific disease setting is needed to get more insight into this emerging field. There have been some retrospective attempts to quantitatively predict TP drug interactions using in vitro–in vivo extrapolation-linked physiologically based pharmacokinetic/pharmacodynamic modelling in patients with RA, surgical trauma and leukaemia [90, 153]. In population pharmacokinetic studies, with the exception of bevacizumab [17], concomitant medication was not identified as a covariate for many mAbs [127, 128, 130, 154]. When bevacizumab was administered with the bolus irinotecan/fluorouracil/leucovorin regimen, its clearance was 17 % lower than when it was used concomitantly with other chemotherapy regimens, but no different from when it was used as monotherapy.
4 Key Demographic Factors Evaluated in Population Pharmacokinetic Studies
4.1 Body Size
Since pharmacokinetic parameters such as clearance and volume are often functions of body size [155], the measures of body size (i.e. body weight, body surface area) could influence the pharmacokinetics of therapeutic mAbs and lead to pharmacokinetic variability observed in many population pharmacokinetic studies [156]. For example, smaller subjects have lower linear clearance of mAbs than larger individuals [13]. In addition, body size was reported to be positively correlated with panitumumab V max, suggesting that body weight can influence the non-linear target-mediated clearance as well as linear clearance [136]. In larger subjects, the volume of plasma and interstitial fluid will be greater than in smaller subjects, contributing to an increased volume of distribution. Hence, body size is tested as a covariate in the majority of population pharmacokinetic analyses performed for mAbs [11, 156] and it is identified as a significant covariate more frequently [11, 156]. Body size-normalised dosing is often used to reduce variability in pharmacokinetics and pharmacodynamics. However, a population pharmacokinetic analysis comparing pharmacokinetic variability following simulations using fixed dosing or body size-normalised dosing in adults for 12 mAbs found similar results for both dosing strategies [157].
4.2 Sex
The effect of sex on the pharmacokinetic variability of mAbs does not appear to be clinically significant in some studies, e.g. sex had only a small influence on the pharmacokinetics of ustekinumab and infliximab [128, 133, 158]. In contrast, in the population pharmacokinetic analyses of bevacizumab and rituximab, the evaluation of sex as a covariate showed that males had higher clearance and volume of distribution (i.e. apparent volume of the central compartment in a two-compartment model), ranging from 17 to 39 % higher [17, 154]. In contrast, another larger analysis with more than 2000 RA patients did not find an effect of sex on rituximab pharmacokinetics [158]. Currently, no dose adjustments for sex are recommended [158, 159]. Differences in mAb pharmacokinetics between the sexes may stem from multiple sources, including differences in lymphatic drainage, endocytosis, immunogenicity and FcγR-mediated clearance. However, the data relating to these aspects are either very limited or currently unavailable (see Sects. 3.1, 3.2, 3.5, 3.6) [13, 17, 18]. In addition, target levels in specific diseases could differ between the sexes, which would lead to variability in non-linear clearance, although there is no direct evidence for this to date (see Sect. 3.4).
4.3 Ethnicity
Although limited data are available, population pharmacokinetic studies using bevacizumab, cetuximab, pertuzumab, alemtuzumab and palavizumab suggest that ethnicity does not influence the pharmacokinetics of the studied mAbs. However, the number of non-Caucasian subjects in these studies was small. Similarly to issues with explaining differences in mAb pharmacokinetics between the sexes, data for ethnic differences in lymphatic drainage, endocytosis, immunogenicity and target-mediated clearance are sparse (see Sects. 3.1, 3.2, 3.4, 3.5). Ethnic differences in the distribution of FcγR polymorphisms have been reported, but the impact on mAb pharmacokinetics is currently unknown [10, 111]. Any reported differences in mAb clearance between ethnic groups [10] can generally be explained by differences in body weight [13, 18], suggesting ethnic differences in these clearance mechanisms are minor. In the population pharmacokinetic analysis of ustekinumab in psoriasis patients [133], volume of distribution was found to be 11.1 % smaller in non-Caucasian patients than in Caucasians after accounting for body weight, but this effect was not clinically relevant.
4.4 Age
Age was found to have an opposite effect in population pharmacokinetic studies of efalizumab and panitumumab [46, 136]. Age was positively correlated with clearance in the efalizumab analysis, but negatively correlated with V max in the panitumumab analysis. However, these studies did not include data from paediatric patients <18 years of age. As discussed in Sects. 3.1 and 3.2, the lymph flow rate and endocytosis rate may decrease in old age, leading to reduced distribution and clearance in the elderly; however, this was not found in the population pharmacokinetic studies to date. Physiological changes in early life are more pronounced due to the maturation of the immune system, receptor abundance and changes in body composition (see Sects. 3.1, 3.2, 3.3, 3.4, 3.5, 3.6). Nonetheless, clearance appears to be similar in paediatric patients and adults once body weight has been accounted for [31].
5 Physiologically-Based Pharmacokinetic Modelling of Variability in mAb Disposition
Several physiologically-based pharmacokinetic models have been developed for describing mAb disposition in man and experimental animals. Published models include both whole-body [152, 160–171] and minimal or lumped models [172–177], incorporating distribution via convection through endothelial pores with or without diffusion and endosomal uptake with FcRn recycling. The complexity of the models varies, with the tissue compartments often being split into sub-compartments representing the vascular, endothelial and interstitial spaces. In addition, the impact of TMDD in the plasma and/or interstitial space of target-containing tissues (i.e. tumours) has been incorporated into several of the models [152, 161, 162, 166, 167, 172, 176]. Mechanistic models to describe mAb absorption following subcutaneous and intramuscular administration have also been reported [38, 39, 178, 179].
Of the published models only two [152, 176] have simulated mAb (and endogenous IgG) pharmacokinetics in multiple individuals taking into account population variability in physiological parameters. Abuqayyas and Balthasar [152] incorporated variability for the target concentration (100–106 %), mAb–target complex elimination rate (28 %), binding affinity of mAb for target (55 %) and the vascular reflection coefficient governing convective distribution in the tumour (26 %). However, no variability was included for body weight, tissue volumes and flows, parameters describing mAb distribution into normal tissues or linear clearance. Li et al. [176] set the body weight, age, height, tissue volumes and flows using population distribution and appropriate covariates [180, 181]. In addition, variability for mAb-/IgG-specific parameters were assigned randomly using lognormal distribution, as covariates between these parameters are currently unknown. The IgG-specific parameters and their assigned variability include endogenous IgG concentration (12.6 %), binding affinity to FcRn (10 %) and clearance of endogenous IgG not bound to FcRn from endosome (10 %) [176]. To recover the observed variability in endogenous IgG concentrations and t ½, an imposed correlation was required between a simulated individual’s baseline endogenous IgG concentration and their FcRn abundance [176]. For therapeutic mAbs, 20–30 % variability was also assigned to the association and dissociation rates of the mAb for its target, baseline target concentrations, the degradation rate of the targets and mAb-target complexes [176]. The simulated values and variability for clearance and t ½ for two mAbs were similar to the observed values from clinical studies.
Although population variability for physiological parameters has not been included in the other published physiologically based pharmacokinetic models for mAbs, many have explored the sensitivity of the predicted plasma concentration profiles to various parameters. Such analysis has shown that predicted plasma concentrations are sensitive to the proportion of mAb that is recycled by FcRn, vascular reflection coefficients for tissue distribution, endosomal uptake rates, clearance rate of mAbs in the lysosome, binding affinity to FcRn, lymph flows, target concentration (and tumour volume for oncology targets) and target–mAb binding affinity [160–163, 167]. This would suggest that inter-subject variability in mAb pharmacokinetics may stem from differences in target abundance, endosomal endocytosis and transcytosis processes, FcRn abundance and lymph flows. The simulated t max following subcutaneous administration was sensitive to the rate of lymph flow from the dosing site; bioavailability was also sensitive to mAb clearance during lymph transit from the dosing site to the plasma [178]. These data imply that differences in lymph flow and endogenous catabolic protein clearance in the lymphatics may contribute to inter-subject variability in mAb subcutaneous absorption.
6 Conclusions
Inter-subject variability in mAb pharmacokinetics is generally moderate to high and often differs between clinical studies. Many factors can potentially contribute to the observed inter-subject variability, including, but not limited to, body size, age, sex, ethnicity, disease status, immune status, co-morbidities, endogenous IgG, concomitant medication and genetic polymorphisms (e.g. FcRn or FcγR). In addition, differences in target antigen concentration can be a major determinant of inter-subject variability in mAb pharmacokinetics, in which increased antigenic burden is associated with decreased mAb exposure, particularly for mAbs that display non-linear pharmacokinetics at therapeutic dose levels. For all mAbs, even those without evident non-linear clearance, ADA concentrations may also have a large impact on inter- and intra-subject pharmacokinetic variability. The complex interplay of these factors and their clinical impact remains to be elucidated. Use of population pharmacokinetics and physiologically based pharmacokinetic models can aid understanding of the physiological and pathophysiological processes which contribute to variability in exposure and response to mAb treatment. Further studies are required to increase understanding of certain patient characteristics before they can be linked to patient variability in pharmacokinetics; for example, the variability in FcRn abundance in the population has not been determined to date. Further understanding of the mechanisms causing variability will aid with accurate predictions of mAb pharmacokinetics during clinical development and for selecting suitable doses for specific patients in the clinic.
References
Dostalek M, Gardner I, Gurbaxani B, Rose R, Chetty M. Pharmacokinetics, pharmacodynamics and physiologically-based pharmacokinetic modelling of monoclonal antibodies. Clin Pharmacokinet. 2013;52(2):83–124.
Subramanian KN, Weisman LE, Rhodes T, Ariagno R, Sanchez PJ, Steichen J, et al. Safety, tolerance and pharmacokinetics of a humanized monoclonal antibody to respiratory syncytial virus in premature infants and infants with bronchopulmonary dysplasia. MEDI-493 Study Group. Pediatr Infect Dis J. 1998;17(2):110–5.
Cézé N, Ternant D, Piller F, Degenne D, Azzopardi N, Dorval E, et al. An enzyme-linked immunosorbent assay for therapeutic drug monitoring of cetuximab. Ther Drug Monit. 2009;31(5):597–601.
St.Clair EW, Wagner CL, Fasanmade AA, Wang B, Schaible T, Kavanaugh A, et al. The relationship of serum infliximab concentrations to clinical improvement in rheumatoid arthritis: results from ATTRACT, a multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2002;46(6):1451–9.
Cohen S, Freeman T. Metabolic heterogeneity of human gamma-globulin. Biochem J. 1960;76:475–87.
Solomon A, Waldmann TA, Fahey JL. Clinical and experimental metabolism of normal 6.6s gamma-globulin in normal subjects and in patients with macroglobulinemia and multiple myeloma. J Lab Clin Med. 1963;62:1–17.
Wochner RD, Drews G, Strober W, Waldmann TA. Accelerated breakdown of immunoglobulin G (IgG) in myotonic dystrophy: a hereditary error of immunoglobulin catabolism. J Clin Invest. 1966;45(3):321–9.
Birke G, Liljedahl SO, Olhagen B, Plantin LO, Ahlinder S. Catabolism and distribution of gamma-globulin. A preliminary study with 131 I-labelled gammaglobulin. Acta Med Scand. 1963;173:589–603.
Keizer R, Huitema AR, Schellens JM, Beijnen J. Clinical pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(8):493–507.
Chiba K, Yoshitsugu H, Kyosaka Y, Iida S, Yoneyama K, Tanigawa T, et al. A comprehensive review of the pharmacokinetics of approved therapeutic monoclonal antibodies in Japan: are Japanese phase I studies still needed? J Clin Pharmacol. 2014;54(5):483–94.
Dirks N, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(10):633–59.
Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–58.
Mould D, Green B. Pharmacokinetics and pharmacodynamics of monoclonal antibodies. BioDrugs. 2010;24(1):23–39.
Tabrizi MA, Tseng C-ML, Roskos LK. Elimination mechanisms of therapeutic monoclonal antibodies. Drug Discov Today. 2006;11(1–2):81–8.
Roberts BV, Susano I, Gipson DS, Trachtman H, Joy MS. Contribution of renal and non-renal clearance on increased total clearance of adalimumab in glomerular disease. J Clin Pharmacol. 2013;53(9):919–24.
Mortensen DL, Walicke PA, Wang X, Kwon P, Kuebler P, Gottlieb AB, et al. Pharmacokinetics and pharmacodynamics of multiple weekly subcutaneous efalizumab doses in patients with plaque psoriasis. J Clin Pharmacol. 2005;45(3):286–98.
Lu J-F, Bruno R, Eppler S, Novotny W, Lum B, Gaudreault J. Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother Pharmacol. 2008;62(5):779–86.
Xu ZH, Lee H, Vu T, Hu C, Yan H, Baker D, et al. Population pharmacokinetics of golimumab in patients with ankylosing spondylitis: impact of body weight and immunogenicity. Int J Clin Pharmacol Ther. 2010;48(9):596–607.
Olszewski WL, Pazdur J, Kubasiewicz E, Zaleska M, Cooke CJ, Miller NE. Lymph draining from foot joints in rheumatoid arthritis provides insight into local cytokine and chemokine production and transport to lymph nodes. Arthritis Rheum. 2001;44(3):541–9.
Rane S, Donahue PMC, Towse T, Ridner S, Chappell M, Jordi J, et al. Clinical feasibility of noninvasive visualization of lymphatic flow with principles of spin labeling MR imaging: implications for lymphedema assessment. Radiology. 2013;269(3):893–902.
Stanton AW, Svensson WE, Mellor RH, Peters AM, Levick JR, Mortimer PS. Differences in lymph drainage between swollen and non-swollen regions in arms with breast-cancer-related lymphoedema. Clin Sci. 2001;101(2):131–40.
Stanton AWB, Modi S, Mellor RH, Peters AM, Svensson WE, Levick JR, et al. A quantitative lymphoscintigraphic evaluation of lymphatic function in the swollen hands of women with lymphoedema following breast cancer treatment. Clin Sci. 2006;110(5):553–61.
Hollander W, Reilly P, Burrows BA. Lymphatic flow in human subjects as indicated by the disappearance of i131-labeled albumin from the subcutaneous tissue. J Clin Invest. 1961;40(2):222–33.
Lamka J, Kolarova H, Maresova J, Kvetina J. The influence of experimentally induced pathological states on the flow and composition of central lymph in the rat. Physiol Bohemoslov. 1986;35(4):328–33.
Semaeva E, Tenstad O, Skavland J, Enger M, Iversen PO, Gjertsen BT, et al. Access to the spleen microenvironment through lymph shows local cytokine production, increased cell flux, and altered signaling of immune cells during lipopolysaccharide-induced acute inflammation. J Immunol. 2010;184(8):4547–56.
Waldmann TA, Strober W. Metabolism of immunoglobulins. Prog Allergy. 1969;13:1–110.
Ying M, Ahuja A, Brook F. Gray scale and power doppler sonography of normal cervical lymph nodes: comparison between Chinese and white subjects. J Ultrasound Med. 2002;21(1):59–65.
Conway WC, Faries M, Nicholl M, Terando A, Glass E, Sim M, et al. Age-related lymphatic dysfunction in melanoma patients. Ann Surg Oncol. 2009;16(6):1548–52.
Kennedy C, Bastiaens MT, Bajdik CD, Willemze R, Westendorp RGJ, Bouwes Bavinck JN. Effect of smoking and sun on the aging skin. J Investig Dermatol. 2003;120(4):548–54.
Luscieti P, Hubschmid T, Cottier H, Hess MW, Sobin LH. Human lymph node morphology as a function of age and site. J Clin Pathol. 1980;33(5):454–61.
Xu Z, Davis HM, Zhou H. Rational development and utilization of antibody-based therapeutic proteins in pediatrics. Pharmacol Ther. 2013;137(2):225–47.
Edlund H, Melin J, Parra-Guillen ZP, Kloft C. Pharmacokinetics and pharmacokinetic-pharmacodynamic relationships of monoclonal antibodies in children. Clin Pharmacokinet. 2015;54(1):35–80.
Tabrizi M, Bornstein GG, Suria H. Biodistribution mechanisms of therapeutic monoclonal antibodies in health and disease. AAPS J. 2010;12(1):33–43.
Lentner C. Geigy scientific tables, vol. 1: units of measurement, body fluids, composition of the body, and nutrition. 8th ed. Basel: Wiley; 1981. pp. 217–27.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982;35(5):1169–75.
Kauffman R. Drug therapeutics in the infant and child. In: Yaffe S, Aranda J, editors. Pediatric pharmacology: therapeutic principles in practise. Philadelphia: WB Saunders; 1992. p. 212–9.
Robbie GJ, Zhao L, Mondick J, Losonsky G, Roskos LK. Population pharmacokinetics of palivizumab, a humanized anti-respiratory syncytial virus monoclonal antibody, in adults and children. Antimicrob Agents Chemother. 2012;56(9):4927–36.
Kagan L, Mager DE. Mechanisms of subcutaneous absorption of rituximab in rats. Drug Metab Dispos. 2013;41(1):248–55.
Kagan L, Turner MR, Balu-Iyer SV, Mager DE. Subcutaneous absorption of monoclonal antibodies: role of dose, site of injection, and injection volume on rituximab pharmacokinetics in rats. Pharm Res. 2012;29(2):490–9.
Xu Z, Wang Q, Zhuang Y, Frederick B, Yan H, Bouman-Thio E, et al. Subcutaneous bioavailability of golimumab at 3 different injection sites in healthy subjects. J Clin Pharmacol. 2010;50(3):276–84.
Havas E, Parviainen T, Vuorela J, Toivanen J, Nikula T, Vihko V. Lymph flow dynamics in exercising human skeletal muscle as detected by scintography. J Physiol (Lond). 1997;504(Pt 1):233–9.
Richter W, Bhansali S, Morris M. Mechanistic determinants of biotherapeutics absorption following SC administration. AAPS J. 2012;14(3):559–70.
Porter CJH, Charman SA. Lymphatic transport of proteins after subcutaneous administration. J Pharm Sci. 2000;89(3):297–310.
Swartz MA. The physiology of the lymphatic system. Adv Drug Deliv Rev. 2001;50(1–2):3–20.
Ng CM, Joshi A, Dedrick RL, Garovoy MR, Bauer RJ. Pharmacokinetic-pharmacodynamic-efficacy analysis of efalizumab in patients with moderate to severe psoriasis. Pharm Res. 2005;22(7):1088–100.
Sun Y-N, Lu J-F, Joshi A, Compton P, Kwon P, Bruno RA. Population pharmacokinetics of efalizumab (humanized monoclonal anti-CD11a antibody) following long-term subcutaneous weekly dosing in psoriasis subjects. J Clin Pharmacol. 2005;45(4):468–76.
Hayashi N, Tsukamoto Y, Sallas WM, Lowe PJ. A mechanism-based binding model for the population pharmacokinetics and pharmacodynamics of omalizumab. Br J Clin Pharmacol. 2007;63(5):548–61.
Peterson MC, Stouch BJ, Chen D, et al. A population PK/PD model describes the rapid, and sustained suppression of urinary N-telopeptide following administration of AMG 162, a fully human monoclonal antibody against RANKL, to healthy postmenopausal women. AAPS J. 2004;6(S1). http://abstracts.aaps.org/SecureView/AAPSJournal/radb51lv0bx.pdf
Peterson MC, Jang G, Kim W, Gurrola E, Kinsey A, Dansey R. Selection of a phase 3 dose regimen for denosumab based on pharmacokinetic (PK), pharmacodynamic (PD), and safety data from multiple subcutaneous (SC) dosing regimens in breast cancer patients (pts) with bone metastases (BM). J Clin Oncol. 2006;24(18S):3086.
Le Couteur DG, Cogger VC, McCuskey RS, De Cabo R, Smedsrød B, Sorensen KK, et al. Age-related changes in the liver sinusoidal endothelium. Ann N Y Acad Sci. 2007;1114(1):79–87.
Collins JC, Stockert RJ, Morell AG. Asialoglycoprotein receptor expression in murine pregnancy and development. Hepatology. 1984;4(1):80–3.
Stockert RJ, Gärtner U, Morell AG, Wolkoff AW. Effects of receptor-specific antibody on the uptake of desialylated glycoproteins in the isolated perfused rat liver. J Biol Chem. 1980;255(9):3830–1.
Poulin P. A single-species approach considering additional physiological information for prediction of hepatic clearance of glycoprotein derivate therapeutics. Clin Pharmacokinet. 2011;50(10):665–74.
Sarin H. Physiologic upper limits of pore size of different blood capillary types and another perspective on the dual pore theory of microvascular permeability. J Angiogenes Res. 2010;2:14.
Mulivor AW, Lipowsky HH. Inflammation- and ischemia-induced shedding of venular glycocalyx. Am J Physiol Heart Circ Physiol. 2004;286(5):H1672–80.
Vugmeyster Y, Harrold J, Xu X. Absorption, distribution, metabolism, and excretion (ADME) studies of biotherapeutics for autoimmune and inflammatory conditions. AAPS J. 2012;14(4):714–27.
Eisenberg C, Seta N, Appel M, Feldmann G, Durand G, Feger J. Asialoglycoprotein receptor in human isolated hepatocytes from normal liver and its apparent increase in liver with histological alterations. J Hepatol. 1991;13(3):305–9.
Slama A, Zinbi H, Feger J, Dodeur M. Comparative determination of the asialoglycoprotein receptor by ligand and antibody binding in hepatocytes from normal and diabetic rats. Biol Cell. 1988;63(3):367–9.
Dodeur M, Coumoul S, Scarmato P, Durand G, Feger J, Agneray J. Asialoorosomucoid degradation by normal and diabetic rat hepatocytes. Eur J Biochem. 1984;140(3):577–81.
Stohrer M, Boucher Y, Stangassinger M, Jain RK. Oncotic pressure in solid tumors is elevated. Cancer Res. 2000;60(15):4251–5.
Jain RK. Transport of molecules, particles, and cells in solid tumors. Annu Rev Biomed Eng. 1999;1(1):241–63.
Brown RS, Kaminski MS, Fisher SJ, Chang AE, Wahl RL. Intratumoral microdistribution of [131I]MB-1 in patients with B-cell lymphoma following radioimmunotherapy. Nucl Med Biol. 1997;24(7):657–63.
Shockley TR, Lin K, Nagy JA, Tompkins RG, Yarmush ML, Dvorak HF. Spatial distribution of tumor-specific monoclonal antibodies in human melanoma xenografts. Cancer Res. 1992;52(2):367–76.
Kliwinski C, Cooper PR, Perkinson R, Mabus JR, Tam SH, Wilkinson TM, et al. Contribution of FcRn binding to intestinal uptake of IgG in suckling rat pups and human FcRn-transgenic mice. Am J Physiol Gastrointest Liver Physiol. 2013;304(3):262–70.
Martin MG, Wu SV, Walsh JH. Ontogenetic development and distribution of antibody transport and Fc receptor mRNA expression in rat intestine. Dig Dis Sci. 1997;42(5):1062–9.
Hornby P, Cooper P, Kliwinski C, Ragwan E, Mabus J, Harman B, et al. Human and non-human primate intestinal FcRn expression and immunoglobulin G transcytosis. Pharm Res. 2014;31(4):908–22.
Israel EJ, Taylor S, Wu Z, Mizoguchi E, Blumberg RS, Bhan A, et al. Expression of the neonatal Fc receptor, FcRn, on human intestinal epithelial cells. Immunology. 1997;92(1):69–74.
Shah U, Dickinson BL, Blumberg RS, Simister NE, Lencer WI, Walker WA. Distribution of the IgG Fc receptor, FcRn, in the human fetal intestine. Pediatr Res. 2003;53(2):295–301.
Sarvas H, Seppälä I, Kurikka S, Siegberg R, Mäkelä O. Half-life of the maternal IgG1 allotype in infants. J Clin Immunol. 1993;13(2):145–51.
Freeman T. Gamma globulin metabolism in normal humans and in patients. Ser Haematol. 1965;4:76–86.
Gurbaxani B, Dostalek M, Gardner I. Are endosomal trafficking parameters better targets for improving mAb pharmacokinetics than FcRn binding affinity? Mol Immunol. 2013;56(4):660–74.
Andersen JT, Sandlie I. The versatile MHC class I-related FcRn protects IgG and albumin from degradation: implications for development of new diagnostics and therapeutics. Drug Metab Pharmacokinet. 2009;24(4):318–32.
Uno Y, Utoh M, Iwasaki K. Polymorphisms of neonatal Fc receptor in cynomolgus and rhesus macaques. Drug Metab Pharmacokinet. 2014;29(5):427–30.
Wani MA, Haynes LD, Kim J, Bronson CL, Chaudhury C, Mohanty S, et al. Familial hypercatabolic hypoproteinemia caused by deficiency of the neonatal Fc receptor, FcRn, due to a mutant β2-microglobulin gene. Proc Natl Acad Sci USA. 2006;103(13):5084–9.
Ishii-Watabe A, Saito Y, Suzuki T, Tada M, Ukaji M, Maekawa K, et al. Genetic polymorphisms of FCGRT encoding FcRn in a Japanese population and their functional analysis. Drug Metab Pharmacokinet. 2010;25(6):578–87.
de Bono JS, Tolcher AW, Forero A, Vanhove GFA, Takimoto C, Bauer RJ, et al. ING-1, a monoclonal antibody targeting Ep-CAM in patients with advanced adenocarcinomas. Clin Cancer Res. 2004;10(22):7555–65.
Ternant D, Ducourau E, Perdriger A, Corondan A, Le Goff B, Devauchelle-Pensec V, et al. Relationship between inflammation and infliximab pharmacokinetics in rheumatoid arthritis. Br J Clin Pharmacol. 2014;78(1):118–28.
Beum PV, Kennedy AD, Taylor RP. Three new assays for rituximab based on its immunological activity or antigenic properties: analyses of sera and plasmas of RTX-treated patients with chronic lymphocytic leukemia and other B cell lymphomas. J Immunol Methods. 2004;289(1–2):97–109.
Kuang B, King L, Wang HF. Therapeutic monoclonal antibody concentration monitoring: free or total? Bioanalysis. 2010;2(6):1125–40.
Arribas J, Borroto A. Protein ectodomain shedding. Chem Rev. 2002;102(12):4627–38.
Manshouri T, K-a Do, Wang X, Giles FJ, O’Brien SM, Saffer H, et al. Circulating CD20 is detectable in the plasma of patients with chronic lymphocytic leukemia and is of prognostic significance. Blood. 2003;101(7):2507–13.
Albitar M, Do K-A, Johnson MM, Giles FJ, Jilani I, O’Brien S, et al. Free circulating soluble CD52 as a tumor marker in chronic lymphocytic leukemia and its implication in therapy with anti-CD52 antibodies. Cancer. 2004;101(5):999–1008.
Lennon S, Barton C, Banken L, Gianni L, Marty M, Baselga J, et al. Utility of serum HER2 extracellular domain assessment in clinical decision making: pooled analysis of four trials of trastuzumab in metastatic breast cancer. J Clin Oncol. 2009;27(10):1685–93.
Moreno-Aspitia A, Hillman DW, Dyar SH, Tenner KS, Gralow J, Kaufman PA, et al. Soluble human epidermal growth factor receptor 2 (HER2) levels in patients with HER2-positive breast cancer receiving chemotherapy with or without trastuzumab: results from North Central Cancer Treatment Group adjuvant trial N9831. Cancer. 2013;119(15):2675–82.
Tokuda Y, Watanabe T, Omuro Y, Ando M, Katsumata N, Okumura A, et al. Dose escalation and pharmacokinetic study of a humanized anti-HER2 monoclonal antibody in patients with HER2/neu-overexpressing metastatic breast cancer. Br J Cancer. 1999;81(8):1419–25.
Baselga J, Tripathy D, Mendelsohn J, Baughman S, Benz CC, Dantis L, et al. Phase II study of weekly intravenous recombinant humanized anti-p185HER2 monoclonal antibody in patients with HER2/neu-overexpressing metastatic breast cancer. J Clin Oncol. 1996;14(3):737–44.
Pegram MD, Lipton A, Hayes DF, Weber BL, Baselga JM, Tripathy D, et al. Phase II study of receptor-enhanced chemosensitivity using recombinant humanized anti-p185HER2/neu monoclonal antibody plus cisplatin in patients with HER2/neu-overexpressing metastatic breast cancer refractory to chemotherapy treatment. J Clin Oncol. 1998;16(8):2659–71.
Mahmood I, Green M. Pharmacokinetic and pharmacodynamic considerations in the development of therapeutic proteins. Clin Pharmacokinet. 2005;44(4):331–47.
Enevold C, Baslund B, Linde L, Josephsen NL, Tarp U, Lindegaard H, et al. Interleukin-6-receptor polymorphisms rs12083537, rs2228145, and rs4329505 as predictors of response to tocilizumab in rheumatoid arthritis. Pharmacogenet Genomics. 2014;24(8):401–5.
Machavaram KK, Almond LM, Rostami-Hodjegan A, Gardner I, Jamei M, Tay S, et al. A physiologically based pharmacokinetic modeling approach to predict disease-drug interactions: suppression of CYP3A by IL-6. Clin Pharmacol Ther. 2013;94(2):260–8.
Takeuchi T, Miyasaka N, Tatsuki Y, Yano T, Yoshinari T, Abe T, et al. Baseline tumour necrosis factor alpha levels predict the necessity for dose escalation of infliximab therapy in patients with rheumatoid arthritis. Ann Rheum Dis. 2011;70(7):1208–15.
Straub RH, Paimela L, Peltomaa R, Schölmerich J, Leirisalo-Repo M. Inadequately low serum levels of steroid hormones in relation to interleukin-6 and tumor necrosis factor in untreated patients with early rheumatoid arthritis and reactive arthritis. Arthritis Rheum. 2002;46(3):654–62.
Lecluse LA, Driessen RB, Spuls PI, et al. Extent and clinical consequences of antibody formation against adalimumab in patients with plaque psoriasis. Arch Dermatol. 2010;146(2):127–32.
Zhou L, Hoofring S, Wu Y, Vu T, Ma P, Swanson S, et al. Stratification of antibody-positive subjects by antibody level reveals an impact of immunogenicity on pharmacokinetics. AAPS J. 2013;15(1):30–40.
Bendtzen K, Geborek P, Svenson M, Larsson L, Kapetanovic MC, Saxne T. Individualized monitoring of drug bioavailability and immunogenicity in rheumatoid arthritis patients treated with the tumor necrosis factor α inhibitor infliximab. Arthritis Rheum. 2006;54(12):3782–9.
de Vries MK, Wolbink GJ, Stapel SO, de Groot ER, Dijkmans BAC, Aarden LA, et al. Inefficacy of infliximab in ankylosing spondylitis is correlated with antibody formation. Ann Rheum Dis. 2007;66(1):133–4.
Chen X, Hickling T, Kraynov E, Kuang B, Parng C, Vicini P. A mathematical model of the effect of immunogenicity on therapeutic protein pharmacokinetics. AAPS J. 2013;15(4):1141–54.
Schellekens H. Factors influencing the immunogenicity of therapeutic proteins. Nephrol Dial Transpl. 2005;20(suppl 6):vi3–vi9.
Chirmule N, Jawa V, Meibohm B. Immunogenicity to therapeutic proteins: impact on PK/PD and efficacy. AAPS J. 2012;14(2):296–302.
van der Maas A, van den Bemt BJ, Wolbink G, van den Hoogen FH, van Riel PL, den Broeder AA. Low infliximab serum trough levels and anti-infliximab antibodies are prevalent in rheumatoid arthritis patients treated with infliximab in daily clinical practice: results of an observational cohort study. BMC Musculoskelet Disord. 2012;13:184.
Shen J, Townsend R, You X, Shen Y, Zhan P, Zhou Z, et al. Pharmacokinetics, pharmacodynamics, and immunogenicity of belatacept in adult kidney transplant recipients. Clin Drug Investig. 2014;34(2):117–26.
Vugmeyster Y, Xu X, Theil FP, Khawli LA, Leach MW. Pharmacokinetics and toxicology of therapeutic proteins: advances and challenges. World J Biol Chem. 2012;3(4):73–92.
Rosenberg A. Effects of protein aggregates: an immunologic perspective. AAPS J. 2006;8(3):E501–7.
Ratanji KD, Derrick JP, Dearman RJ, Kimber I. Immunogenicity of therapeutic proteins: influence of aggregation. J Immunotoxicol. 2014;11(2):99–109.
Price KS, Hamilton RG. Anaphylactoid reactions in two patients after omalizumab administration after successful long-term therapy. Allergy Asthma Proc. 2007;28(3):313–9.
Ruixo JP, Ma P, Chow A. The utility of modeling and simulation approaches to evaluate immunogenicity effect on the therapeutic protein pharmacokinetics. AAPS J. 2013;15(1):172–82.
Xue L, Rup B. Evaluation of pre-existing antibody presence as a risk factor for posttreatment anti-drug antibody induction: analysis of human clinical study data for multiple biotherapeutics. AAPS J. 2013;15(3):893–6.
Schellekens H. The immunogenicity of therapeutic proteins. Discov Med. 2010;9(49):560–4.
Bartelds GM, Wijbrandts CA, Nurmohamed MT, Stapel S, Lems WF, Aarden L, et al. Anti-infliximab and anti-adalimumab antibodies in relation to response to adalimumab in infliximab switchers and anti-tumour necrosis factor naive patients: a cohort study. Ann Rheum Dis. 2010;69(5):817–21.
Dowling DJ, Levy O. Ontogeny of early life immunity. Trends Immunol. 2014;35(7):299–310.
Rascu A, Repp R, Westerdaal NAC, Kalden JR, van de Winkel JGJ. Clinical relevance of Fcγ receptor polymorphisms. Ann N Y Acad Sci. 1997;815(1):282–95.
Julià M, Guilabert A, Lozano F, et al. The role of fcγ receptor polymorphisms in the response to anti–tumor necrosis factor therapy in psoriasis: a pharmacogenetic study. JAMA Dermatol. 2013;149(9):1033–9.
Tutuncu Z, Kavanaugh A, Zvaifler N, Corr M, Deutsch R, Boyle D. Fcγ receptor type IIIA polymorphisms influence treatment outcomes in patients with inflammatory arthritis treated with tumor necrosis factor α-blocking agents. Arthritis Rheum. 2005;52(9):2693–6.
Nishio S, Yamamoto T, Kaneko K, Tanaka-Matsumoto N, Muraoka S, Kaburaki M, et al. Pharmacokinetic study and Fcgamma receptor gene analysis in two patients with rheumatoid arthritis controlled by low-dose infliximab. Mod Rheumatol. 2009;19(3):329–33.
Ternant D, Berkane Z, Picon L, Gouilleux-Gruart V, Colombel JF, Allez M, et al. Assessment of the influence of inflammation and FCGR3A genotype on infliximab pharmacokinetics and time to relapse in patients with Crohn’s disease. Clin Pharmacokinet. 2015;54(5):551–62.
Prokopec KE, Rhodiner M, Matt P, Lindqvist U, Kleinau S. Down regulation of Fc and complement receptors on B cells in rheumatoid arthritis. Clin Immunol. 2010;137(3):322–9.
Prokopec K, Berntson L, Öman A, Kleinau S. Up regulated complement and Fc receptors in juvenile idiopathic arthritis and correlation with disease phenotype. J Clin Immunol. 2012;32(3):540–50.
Loegering DJ, Blumenstock FA, Cuddy BG. Determination of Kupffer cell Fc receptor function in vivo following injury. Proc Soc Exp Biol Med. 1989;192(3):255–60.
Dall’Ozzo S, Tartas S, Paintaud G, Cartron G, Colombat P, Bardos P, et al. Rituximab-dependent cytotoxicity by natural killer cells: influence of FCGR3A polymorphism on the concentration-effect relationship. Cancer Res. 2004;64(13):4664–9.
Meibohm B, Zhou H. Characterizing the impact of renal impairment on the clinical pharmacology of biologics. J Clin Pharmacol. 2012;52:54S–62S.
Mentre F, Kovarik J, Gerbeau C. Constructing a prediction interval for time to reach a threshold concentration based on a population pharmacokinetic analysis: an application to basiliximab in renal transplantation. J Pharmacokinet Biopharm. 1999;27(2):213–30.
Kovarik JM, Nashan B, Neuhaus P, Clavien PA, Gerbeau C, Hall ML, et al. A population pharmacokinetic screen to identify demographic-clinical covariates of basiliximab in liver transplantation. Clin Pharmacol Ther. 2001;69(4):201–9.
Kovarik J, Breidenbach T, Gerbeau C, Korn A, Schmidt AG, Nashan B. Disposition and immunodynamics of basiliximab in liver allograft recipients. Clin Pharmacol Ther. 1998;64(1):66–72.
Zhou J, Pop LM, Ghetie V. Hypercatabolism of IgG in mice with lupus-like syndrome. Lupus. 2005;14(6):458–66.
Kneepkens EL, Krieckaert CLM, van der Kleij D, Nurmohamed MT, van der Horst-Bruinsma IE, Rispens T, et al. Lower etanercept levels are associated with high disease activity in ankylosing spondylitis patients at 24 weeks of follow-up. Ann Rheum Dis. 2014;74(10):1825–9.
Wolbink GJ, Voskuyl AE, Lems WF, de Groot E, Nurmohamed MT, Tak PP, et al. Relationship between serum trough infliximab levels, pretreatment C reactive protein levels, and clinical response to infliximab treatment in patients with rheumatoid arthritis. Ann Rheum Dis. 2005;64(5):704–7.
Dirks NL, Nolting A, Kovar A, Meibohm B. Population pharmacokinetics of cetuximab in patients with squamous cell carcinoma of the head and neck. J Clin Pharmacol. 2008;48(3):267–78.
Xu Z, Seitz K, Fasanmade A, Ford J, Williamson P, Xu W, et al. Population pharmacokinetics of infliximab in patients with ankylosing spondylitis. J Clin Pharmacol. 2008;48(6):681–95.
Kuester K, Kovar A, Lupfert C, Brockhaus B, Kloft C. Population pharmacokinetic data analysis of three phase I studies of matuzumab, a humanised anti-EGFR monoclonal antibody in clinical cancer development. Br J Cancer. 2008;98(5):900–6.
Bruno R, Washington CB, Lu JF, Lieberman G, Banken L, Klein P. Population pharmacokinetics of trastuzumab in patients with HER2+ metastatic breast cancer. Cancer Chemother Pharmacol. 2005;56(4):361–9.
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, et al. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol. 2009;65(12):1211–28.
Ng CM, Lum BL, Gimenez V, Kelsey S, Allison D. Rationale for fixed dosing of pertuzumab in cancer patients based on population pharmacokinetic analysis. Pharm Res. 2006;23(6):1275–84.
Zhu Y, Hu C, Lu M, Liao S, Marini JC, Yohrling J, et al. Population pharmacokinetic modeling of ustekinumab, a human monoclonal antibody targeting IL-12/23p40, in patients with moderate to severe plaque psoriasis. J Clin Pharmacol. 2009;49(2):162–75.
Kim J, Hayton WL, Robinson JM, Anderson CL. Kinetics of FcRn-mediated recycling of IgG and albumin in human: pathophysiology and therapeutic implications using a simplified mechanism-based model. Clin Immunol. 2007;122(2):146–55.
Anderson CL, Chaudhury C, Kim J, Bronson CL, Wani MA, Mohanty S. Perspective—FcRn transports albumin: relevance to immunology and medicine. Trends Immunol. 2006;27(7):343–8.
Ma P, Yang BB, Wang YM, Peterson M, Narayanan A, Sutjandra L, et al. Population pharmacokinetic analysis of panitumumab in patients with advanced solid tumors. J Clin Pharmacol. 2009;49(10):1142–56.
Mould DR, Baumann A, Kuhlmann J, Keating MJ, Weitman S, Hillmen P, et al. Population pharmacokinetics-pharmacodynamics of alemtuzumab (Campath) in patients with chronic lymphocytic leukaemia and its link to treatment response. Br J Clin Pharmacol. 2007;64(3):278–91.
Zhuang Y, de Vries DE, Xu Z, Marciniak SJ Jr, Chen D, Leon F, et al. Evaluation of disease-mediated therapeutic protein-drug interactions between an anti-interleukin-6 monoclonal antibody (sirukumab) and cytochrome P450 activities in a phase 1 study in patients with rheumatoid arthritis using a cocktail approach. J Clin Pharmacol. 2015;55(12):1386–1394. doi:10.1002/jcph.561
Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S. Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther. 2011;89(5):735–40.
Zhou H, Davis HM. Risk-based strategy for the assessment of pharmacokinetic drug-drug interactions for therapeutic monoclonal antibodies. Drug Discov Today. 2009;14(17–18):891–8.
Kenny JR, Liu MM, Chow AT, Earp JC, Evers R, Slatter JG, et al. Therapeutic protein drug-drug interactions: navigating the knowledge gaps-highlights from the 2012 AAPS NBC Roundtable and IQ Consortium/FDA workshop. AAPS J. 2013;15(4):933–40.
Evers R, Dallas S, Dickmann LJ, Fahmi OA, Kenny JR, Kraynov E, et al. Critical review of preclinical approaches to investigate cytochrome p450-mediated therapeutic protein drug-drug interactions and recommendations for best practices: a white paper. Drug Metab Dispos. 2013;41(9):1598–609.
Kraynov E, Martin SW, Hurst S, Fahmi OA, Dowty M, Cronenberger C, et al. How current understanding of clearance mechanisms and pharmacodynamics of therapeutic proteins can be applied for evaluation of their drug-drug interaction potential. Drug Metab Dispos. 2011;39(10):1779–83.
Girish S, Martin SW, Peterson MC, Zhang LK, Zhao H, Balthasar J, et al. AAPS workshop report: strategies to address therapeutic protein-drug interactions during clinical development. AAPS J. 2011;13(3):405–16.
Azam YJ, Machavaram KK, Rostami-Hodjegan A. The modulating effects of endogenous substances on drug metabolising enzymes and implications for inter-individual variability and quantitative prediction. Curr Drug Metab. 2014;15(6):599–619.
Weisman MH, Moreland LW, Furst DE, Weinblatt ME, Keystone EC, Paulus HE, et al. Efficacy, pharmacokinetic, and safety assessment of adalimumab, a fully human anti-tumor necrosis factor-alpha monoclonal antibody, in adults with rheumatoid arthritis receiving concomitant methotrexate: a pilot study. Clin Ther. 2003;25(6):1700–21.
Bunescu A, Seideman P, Lenkei R, Levin K, Egberg N. Enhanced Fcgamma receptor I, alphaMbeta2 integrin receptor expression by monocytes and neutrophils in rheumatoid arthritis: interaction with platelets. J Rheumatol. 2004;31(12):2347–55.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41(9):1552–63.
Wijngaarden S, van Roon JA, van de Winkel JG, Bijlsma JW, Lafeber FP. Down-regulation of activating Fcgamma receptors on monocytes of patients with rheumatoid arthritis upon methotrexate treatment. Rheumatology (Oxford). 2005;44(6):729–34.
Herceptin (trastuzumab): US prescribing information. 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/103792s5250lbl.pdf. Accessed 12 Dec 2015.
Ganjoo KN, An CS, Robertson MJ, Gordon LI, Sen JA, Weisenbach J, et al. Rituximab, bevacizumab and CHOP (RA-CHOP) in untreated diffuse large B-cell lymphoma: safety, biomarker and pharmacokinetic analysis. Leuk Lymphoma. 2006;47(6):998–1005.
Abuqayyas L, Balthasar JP. Pharmacokinetic mAb-mAb interaction: anti-VEGF mAb decreases the distribution of anti-CEA mAb into colorectal tumor xenografts. AAPS J. 2012;14(3):445–55.
Xu Y, Hijazi Y, Wolf A, Wu B, Sun YN, Zhu M. Physiologically based pharmacokinetic model to assess the influence of blinatumomab-mediated cytokine elevations on cytochrome P450 enzyme activity. CPT Pharmacomet Syst Pharmacol. 2015;4(9):507–15.
Ng CM, Bruno R, Combs D, Davies B. Population pharmacokinetics of rituximab (anti-CD20 monoclonal antibody) in rheumatoid arthritis patients during a phase II clinical trial. J Clin Pharmacol. 2005;45(7):792–801.
Meibohm B, Laer S, Panetta JC, Barrett JS. Population pharmacokinetic studies in pediatrics: issues in design and analysis. AAPS J. 2005;7(2):E475–87.
Chetty M, Gill K, Machavaram K, Li L, Gardner I, Rostami A, et al. Emerging covariates on the pharmacokinetics of monoclonal antibodies: do current PBPK models account for the covariates identified in POPPK studies? [abstract no. 3680]. Hersonissos: PAGE (Population Approach Group Europe); 2–5 Jun 2015.
Wang DD, Zhang S, Zhao H, Men AY, Parivar K. Fixed dosing versus body size—based dosing of monoclonal antibodies in adult clinical trials. J Clin Pharmacol. 2009;49(9):1012–24.
Rituxan (rituximab): US prescribing information. 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/103705s5311lbl.pdf. Accessed 12 Dec 2015.
Avastin (bevacizumab): US prescribing information. 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/125085s225lbl.pdf. Accessed 12 Dec 2015.
Garg A, Balthasar J. Physiologically-based pharmacokinetic (PBPK) model to predict IgG tissue kinetics in wild-type and FcRn-knockout mice. J Pharmacokinet Pharmacodyn. 2007;34(5):687–709.
Baxter LT, Zhu H, Mackensen DG, Jain RK. Physiologically based pharmacokinetic model for specific and nonspecific monoclonal antibodies and fragments in normal tissues and human tumor xenografts in nude mice. Cancer Res. 1994;54(6):1517–28.
Baxter LT, Zhu H, Mackensen DG, Butler WF, Jain RK. Biodistribution of monoclonal antibodies: scale-up from mouse to human using a physiologically based pharmacokinetic model. Cancer Res. 1995;55(20):4611–22.
Shah DK, Betts AM. Towards a platform PBPK model to characterize the plasma and tissue disposition of monoclonal antibodies in preclinical species and human. J Pharmacokinet Pharmacodyn. 2012;39(1):67–86.
Ferl GZ, Wu AM, DiStefano JJ 3rd. A predictive model of therapeutic monoclonal antibody dynamics and regulation by the neonatal Fc receptor (FcRn). Ann Biomed Eng. 2005;33(11):1640–52.
Chen Y, Balthasar JP. Evaluation of a catenary PBPK model for predicting the in vivo disposition of mAbs engineered for high-affinity binding to FcRn. AAPS J. 2012;14(4):850–9.
Davda JP, Jain M, Batra SK, Gwilt PR, Robinson DH. A physiologically based pharmacokinetic (PBPK) model to characterize and predict the disposition of monoclonal antibody CC49 and its single chain Fv constructs. Int Immunopharmacol. 2008;8(3):401–13.
Urva SR, Yang VC, Balthasar JP. Physiologically based pharmacokinetic model for T84.66: a monoclonal anti-CEA antibody. J Pharm Sci. 2010;99(3):1582–600.
Covell DG, Barbet J, Holton OD, Black CD, Parker RJ, Weinstein JN. Pharmacokinetics of monoclonal immunoglobulin G1, F(ab’)2, and Fab’ in mice. Cancer Res. 1986;46(8):3969–78.
Heiskanen T, Kairemo K. Development of a PBPK model for monoclonal antibodies and simulation of human and mice PBPK of a radiolabelled monoclonal antibody. Curr Pharm Des. 2009;15(9):988–1007.
Fang L, Sun D. Predictive physiologically based pharmacokinetic model for antibody-directed enzyme prodrug therapy. Drug Metab Dispos. 2008;36(6):1153–65.
Chabot JR, Dettling DE, Jasper PJ, Gomes BC. Comprehensive mechanism-based antibody pharmacokinetic modeling. Conf Proc IEEE Eng Med Biol Soc. 2011:4318–23.
Li L, Gardner I, Rose R, Jamei M. Incorporating target shedding into a minimal PBPK-TMDD model for monoclonal antibodies. CPT Pharmacomet Syst Pharmacol. 2014;3:e96.
Cao Y, Balthasar JP, Jusko WJ. Second-generation minimal physiologically-based pharmacokinetic model for monoclonal antibodies. J Pharmacokinet Pharmacodyn. 2013;40(5):597–607.
Cao Y, Jusko WJ. Applications of minimal physiologically-based pharmacokinetic models. J Pharmacokinet Pharmacodyn. 2012;39(6):711–23.
Fronton L, Pilari S, Huisinga W. Monoclonal antibody disposition: a simplified PBPK model and its implications for the derivation and interpretation of classical compartment models. J Pharmacokinet Pharmacodyn. 2014;41(2):87–107.
Li L, Gardner I, Dostalek M, Jamei M. Simulation of monoclonal antibody pharmacokinetics in humans using a minimal physiologically based model. AAPS J. 2014;16(5):1097–109.
Elmeliegy M, Lowe P, Krzyzanski W. Simplification of complex physiologically based pharmacokinetic models of monoclonal antibodies. AAPS J. 2014;16(4):810–42.
Zhao L, Ji P, Li Z, Roy P, Sahajwalla CG. The antibody drug absorption following subcutaneous or intramuscular administration and its mathematical description by coupling physiologically based absorption process with the conventional compartment pharmacokinetic model. J Clin Pharmacol. 2013;53(3):314–25.
Kagan L, Zhao J, Mager DE. Interspecies pharmacokinetic modeling of subcutaneous absorption of rituximab in mice and rats. Pharm Res. 2014;31(12):3265–73.
Jamei M, Dickinson GL, Rostami-Hodjegan A. A framework for assessing inter-individual variability in pharmacokinetics using virtual human populations and integrating general knowledge of physical chemistry, biology, anatomy, physiology and genetics: a tale of ‘bottom-up’ vs ‘top-down’ recognition of covariates. Drug Metab Pharmacokinet. 2009;24(1):53–75.
Jamei M, Marciniak S, Feng K, Barnett A, Tucker G, Rostami-Hodjegan A. The Simcyp population-based ADME simulator. Expert Opin Drug Metab Toxicol. 2009;5(2):211–23.
Torkildsen Ø, Utsi E, Mellgren SI, Harbo HF, Vedeler CA, Myhr K-M. Ethnic variation of Fcγ receptor polymorphism in Sami and Norwegian populations. Immunology. 2005;115(3):416–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Katherine L. Gill, Krishna K. Machavaram, Rachel H. Rose and Manoranjenni Chetty are employees of Simcyp (a Certara company) and declare no conflicts of interest that might be relevant to the contents of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gill, K.L., Machavaram, K.K., Rose, R.H. et al. Potential Sources of Inter-Subject Variability in Monoclonal Antibody Pharmacokinetics. Clin Pharmacokinet 55, 789–805 (2016). https://doi.org/10.1007/s40262-015-0361-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-015-0361-4


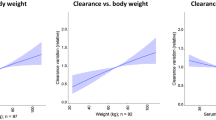

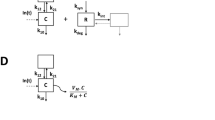

 represent mAb, anti-drug antibodies, FcRn, catabolic enzymes and target receptors
represent mAb, anti-drug antibodies, FcRn, catabolic enzymes and target receptors