Abstract
Germinal matrix hemorrhage (GMH) can be a fatal condition responsible for the death of 1.7% of all neonates in the USA. The majority of GMH survivors develop long-term sequalae with debilitating comorbidities. Higher grade GMH is associated with higher mortality rates and higher prevalence of comorbidities. The pathophysiology of GMH can be broken down into two main titles: faulty hemodynamic autoregulation and structural weakness at the level of tissues and cells. Prematurity is the most significant risk factor for GMH, and it predisposes to both major pathophysiological mechanisms of the condition. Secondary brain injury is an important determinant of survival and comorbidities following GMH. Mechanisms of brain injury secondary to GMH include apoptosis, necrosis, neuroinflammation, and oxidative stress. This review will have a special focus on the mechanisms of oxidative stress following GMH, including but not limited to inflammation, mitochondrial reactive oxygen species, glutamate toxicity, and hemoglobin metabolic products. In addition, this review will explore treatment options of GMH, especially targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
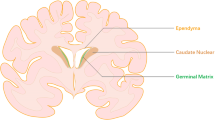
Germinal matrix hemorrhage (GMH), including periventricular and intraventricular hemorrhage, is a common complication of preterm infants [1], predisposing them to cerebral palsy, cognitive deficits, and posthemorrhagic hydrocephalus [2,3,4,5,6]. GMH accounts for 1.7% of all neonatal deaths in the USA and occurs in approximately 3 per 1000 live births [7]. The germinal matrix is a specialized area in the brain where neuronal and glial cell differentiation takes place and is considered a site of rapid angiogenesis relative to other parts in the brain [8, 9]. The germinal matrix is located in the subependyma of ventricular walls, is usually prominent from 7 to 8 weeks of gestation, and almost disappears by 36–37 weeks [10,11,12]. The rich vascular network of the matrix is thin and fragile, which makes it inherently weak and vulnerable to hemorrhage in abnormal conditions [7]. Premature and very low birthweight infants are prone to hemodynamic and cardiorespiratory instability, leading to abrupt fluctuations in cerebral blood flow [10], which is largely impacted by the lack of adequate autoregulatory mechanisms in the immature brain. Moreover, male neonates have higher risk of developing intraventricular hemorrhage (IVH), as compared to female neonates [13]. In fact, male and female infants have different neurodevelopmental profiles, as well as injury response and physiological repair mechanisms, owing but not limited to anatomic and hormonal differences [14]. In premature infants, girls have lower cerebral blood flow than boys of similar gestational and postnatal age [15], in addition to sexual dimorphism in processes of cell proliferation, cell death, and mitochondrial mechanisms [14].
Whereas hemorrhage originates in the germinal matrix of the developing brain, it might often disrupt the ependymal lining, extend into the lateral ventricles, and in severe cases into the brain parenchyma [16, 17]. Currently, there are no standardized protocols to prevent or treat GMH; therefore, thorough understanding of the biological processes involved in the pathogenesis of GMH and in the development of secondary brain injury are necessary to develop new therapies.
GMH-induced brain injury consists of two different phases: primary injury that is caused by the mass effect of the hematoma and secondary injury caused by hemoglobin degradation products, inflammation, death of neurons and glia, microglia activation, excitotoxicity, and oxidative stress [18,19,20,21,22], mechanisms that are interdependent and ensue synchronously. Oxidative stress is described as a state of imbalance between formation of strong oxidants and physiologic antioxidant capacity [23]. Reactive-free radicals include reactive oxygen species (ROS) such as singlet oxygen (1O2), superoxide anion (O2-), hydroxyl radical (OH), and hydrogen peroxide (H2O2), and reactive nitrogen species (RNS), such as peroxynitrite (ONOO-) [24, 25]. These are necessary in low to moderate concentrations for many fundamental cellular functions, including metabolic processes and host defenses [26]; however, their excessive production leads to oxidative damage. Reactive free radicals are intrinsically unstable molecules and thus react with membrane lipids, proteins, and nucleic acids and convert them to free radicals [27]. The resulting oxidative damage to the respective macromolecules leads to their dysfunction and can induce inflammation, apoptosis, autophagy, and destruction of blood brain barrier (BBB) [28]. The brain is particularly vulnerable to oxidative damage because of its high metabolic activity, high levels of lipids prone to peroxidation, high levels of iron and copper (redox-active metals), and relatively weak antioxidant capacity. Importantly, the balance of oxidants and antioxidants before birth is tilted towards oxidant generation because of the poor antioxidant capacity of premature infants, which makes them highly susceptible to oxidative stress [29,30,31]. In the present work, we provide an overview of the mechanisms whereby oxidative stress contributes to GMH-induced brain injury and discuss theoretical areas of possible intervention, so as to limit the severity of this condition and confer neuroprotection.
Secondary Brain Injury Following GMH
Brain injury following GMH is associated with poor prognosis and consists of two different phases—the primary injury, described as primary destructive injury, is mostly induced by the hematoma, including increased intracranial pressure and blockage of cerebrospinal fluid pathways, and a delayed secondary brain injury to the brain parenchyma attributed to neuroinflammation, oxidative stress, cytotoxicity of blood products, hypermetabolism, death of neuron and glia cells, arrest of preoligodendrocyte maturation, and microglia activation, all of which might lead to post-hemorrhagic ventricular dilatation, periventricular leukomalacia, or diffuse white matter injury [5, 32, 33].
When germinal matrix blood vessel rupture, the blood is released into the lateral ventricles and the subsequent IVH results in mechanical disruption of the ventricular lining, facilitating the release of the blood and neural cells populating the periventricular subependymal germinal matrix into the cerebrospinal fluid [27, 34].
As a result, erythrocytes containing hemoglobin, plasma components, products of the coagulation cascade, platelets, and leukocytes are all released into the cerebrospinal fluid (CSF) and participate in the pathogenesis of injury following IVH [4]. Hemolysis of erythrocytes, associated with the release of clotting factors and leukocytes into the CSF, releases large amounts of hemoglobin, free iron, and other neurotoxic substances that cross the BBB and result in a toxic inflammation that is widespread throughout the brain [27, 34, 35]. This sustained inflammation post-IVH is followed by a persistent oxidative stress and tissue injury within the white matter [34]. The developing brain is particularly susceptible to oxidative stress; as such, free radicals altering the redox environment of the brain will cause damage to all important macromolecules resulting in lipid peroxidation, protein oxidation, and DNA fragmentation, which mainly occurs in the peri-hematoma brain tissues and have detrimental effects on the developing brain [33, 35].
Drastic structural modifications in the cells will occur, which in turn can induce inflammation, autophagy, in addition to altering multiple cell-signaling effects that prompt the initiation of apoptosis and the destruction of the BBB [33]. Increasing evidence imply that excessive superoxide generated by nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX) in cells leads to a switch from apoptosis to necrosis that is characterized by swelling of the organelles, rupturing of membranes, and release of cell contents [36].
In addition, activated microglia/macrophages and infiltrating neutrophils following intracerebral hemorrhage (ICH) can also directly induce cell necrosis by attacking complement-bound cells [37]. Moreover, disruption of BBB, which is an important part of the neurovascular unit that strictly regulates the exchange of molecules and ions between brain tissue and peripheral blood circulation, contribute to the fatality of ICH patients [33, 38, 39].
Mechanisms of Oxidative Stress Following GMH
Oxidative stress is the result of imbalance between the production of prooxidants and their elimination by inherent antioxidant mechanisms in the cell [23]. IVH is one of the many complications of prematurity that fall under the umbrella of “the oxygen radical disease of neonatology” as suggested by Saugstad and is thus related to oxidative stress [40, 41]. Whereas antioxidant defense mechanisms are incompletely developed in preterm newborns, several factors such as hypoxia, hyperoxia, infections, ischemia, immune response activation, mitochondrial dysfunction, and Fenton reaction predispose preterm infants to oxidative stress [40, 42].
Inflammation
In a rat model of GMH, RNA-seq analysis revealed upregulation of genes involved in mitochondrial functions, cell cycle progression, activation of immune responses, inflammation, and ferroptosis, in a timely manner [5].
Congruently, inflammation has been linked to oxidative tissue injury where oligodendrocyte progenitor cells (OPCs) were particularly vulnerable to oxidative stress in a rat model of mild to moderate grade of clinical IVH [34]. Experimental IVH was shown to incite a rapid wave of cytokine production, an effect that subsides relatively quickly but is followed by elevated oxidative stress. In parallel, another study in a rabbit model of IVH depicted NOX as the main source of cerebral free radical production [43]. NOX is expressed on the surface of neutrophils and macrophages and stimulates the production of ROS in response to extracellular signals such as hormones and cytokines. Activated microglia and infiltrated neutrophils produce large amounts of ROS and nitric oxide (NO) alongside their release of cytokines and proteases [33]. In the meantime, large amount of superoxide dismutase is consumed to remove free radicals while myeloperoxidase is produced, and this eventually leads to lipid peroxidation at the site of injury [33, 44]. Peroxidated lipids destroy several structures including mitochondrial membranes, which results in loss of membrane function and formation of mitochondrial permeability transition pore [45].
Mitochondrial Dysfunction
Besides, the activated mitochondria act as another important source of ROS. Mitochondria are the cellular energy factories that produce ATP via oxidative phosphorylation, but also generate oxygen free radicals as a biproduct of its respiration under physiologic conditions [46]. Oxygen radicals that escape antioxidant mechanisms can damage proteins, lipids, and DNA. Meanwhile, mitochondrial ROS has been depicted as a major trigger of nucleotide-binding domain-like receptor protein 3 (NLRP3) inflammasome, a component of innate immunity that has been shown to amplify the inflammatory response following ICH and accordingly contribute to oxidative damage [47]. These data demonstrate the bilateral interaction between inflammation and ROS, whereby inflammation is triggered by ROS and at the same time acts as an important source of free radicals through the activated immune cells.
Excitatory Aminoacids
Nevertheless, glutamate toxicity is another pathological process that enhances ROS production. Glutamate is an excitatory neurotransmitter, which acts through N-methyl-d-aspartate (NMDA) receptor, a ligand gated ion channel to increase cerebral blood flow via nitric oxide-mediated vasodilation by upregulating constitutive and inducible nitric oxide synthase (NOS) [27, 48]. Studies have shown that glutamate release is increased but its uptake is reduced after ICH, so that excessive glutamate results in sustained activation of NMDA receptors in postsynaptic neurons [49]. This promotes Ca2+ influx and intracellular Ca2+ overload, activates neuronal nitric oxide synthase (nNOS) and NADPH oxidases (NOXs), and results in synthesis of large amounts of neuronal nitric oxide and superoxide, whose concomitant interaction forms another harmful compound—peroxynitrite [33, 50].
Metabolic Products of Hemoglobin
Moreover, hemoglobin and its metabolic products also contribute to ROS production through Fenton-type reactions [27]. In the presence of superoxide anion generating system (hypoxanthine and xanthine oxidase), free hemoglobin promotes hydroxyl radical formation through the reaction between ferrous heme iron and H2O2, which enhances the peroxidation of membrane lipids [22]. Following ICH, red blood cells degrade and release hemoglobin, which in turn results in hemin, the oxidized form of heme. The latter is highly cytotoxic due to the large amount of ROS it can produce. In fact, hemin is decomposed into bilirubin, free iron (Fe2+), and carbon monoxide by heme oxygenase [51]. The free Fe2+ can generate one of the most reactive oxygen radicals by catalyzing the conversion of superoxide (O2-) and H2O2 into hydroxyl radical (OH-) via Fenton reaction [52]. Iron overload induces toxicity via mechanisms that include ferroptosis, an iron and lipid peroxidation-dependent form of death [53, 54], and neuronal toxicity of iron via transferrin receptor transfer system [55].
Targeting Oxidative Stress Cascades as Treatment Following GMH
Given the central role of oxidative damage in GMH secondary injury, several approaches to cope with oxidative stress are suggested here although most of these are not yet included in clinical trials.
Therapeutic Hypothermia
Therapeutic hypothermia (TH) has been the standard of care for term and late-preterm infants following hypoxic-induced encephalopathy [27, 56]. Neonates core temperatures are maintained at 33.5 °C for 72 h starting within the first 6 h after delivery [57]. The therapeutic effect is meant to reduce the extent of secondary cerebral energy failure following the primary/hypoxic-ischemic insult and to dampen the apoptotic burden [58, 59]. This is primarily achieved through downregulating the cerebral energy metabolism, which decreases the amount of oxygen readily available for the formation of oxygen-based free radicals following reperfusion, thus limiting the oxidative burst [60, 61]. Moreover, TH reduces the release of glutamate and thus protects against neuronal excitotoxicity [59, 61].
Melatonin
Furthermore, melatonin is an endogenous hormone produced by pineal gland and regulates the circadian rhythm of the organism. Melatonin has anti-inflammatory, antioxidant, and anti-apoptotic properties [62, 63], and owing to its lipophilic nature, it can easily cross the BBB and thus might be neuroprotective in GMH [64]. The antioxidant role of melatonin has been well studied by Wang and colleagues, among others, who showed that melatonin treatment following ICH reduces the expression level of NOX-1 and NOX-2 and decreases the levels of ROS in brain tissues [62, 63]. In another study of ischemic/hypobaric hypoxia model, melatonin has been shown to play a major role not only in scavenging superoxide but also in downregulating inducible NOS and promoting the effect of nNOS, thus maintaining a balance in the NO production and protecting against nitrosative damage [65]. In addition, melatonin increased the levels of antioxidants; heme oxygenase (HO-1) and quinone oxidoreductase (NQO1), possibly via activation of the main regulatory system protecting cells against oxidative damage- the nuclear factor erythroid-2-related factor/antioxidant response element (Nrf2/ARE) signaling pathway, thus further contributing to neuroprotection against oxidative stress. Regarding its antiapoptotic effect, treatment with melatonin dampened the upregulation of apoptotic molecules (cleaved caspase 3 and cleaved PARP) and maintained the antiapoptotic/apoptotic balance in favor of anti-apoptosis by increasing the ratio of B cell lymphoma protein 2/Bcl-2-associated X (Bcl-2/BAX) in the brain tissue following ICH. In addition, treatment of the brain tissue samples with melatonin following ICH increased the number of surviving neurons compared to control groups. In another aspect, melatonin protected against mitochondrial damage, where it decreased the levels of cytochrome c in the cytoplasm following ICH [63].
Iron Chelators
On the other hand, given that iron release into the CSF is one of the chief contributors to oxidative stress-induced injury phenotype following IVH, iron chelators are recognized as potential therapeutics. Deferoxamine is one of those chelators that can bind free plasma iron as well as excess iron within tissues and might reduce the generation of reactive hydroxyl radicals by inhibiting Fenton reaction [66]. Interestingly, deferoxamine has been shown to decrease the concentrations of iron and ferritin in the brain tissue and CSF after cerebral hemorrhage and thus decrease the incidence of hydrocephalus in a rat model of IVH [67]. In addition, it also protected against subarachnoid fibrosis that ensues after cerebral hemorrhage by downregulating the expression of Wingless/Integrated 1 (Wnt1) and Wnt3a proteins in brain tissue, given that Wnt signaling pathway has been involved in the development of fibrotic lesions in variety of tissues [67,68,69]. Moreover, deferoxamine treatment improved long-term motor and cognitive function of rat pups post-GMH by reducing cortical, basal ganglia, and white matter loss in addition to posthemorrhagic ventricular dilation [70].
Minocycline, a second-generation tetracycline, is another iron-chelator with broad-spectrum mechanisms, which suggests its potential importance in GMH treatment. Minocycline has been shown to suppress the upregulation of ferritin after GMH, reduce brain edema, hydrocephalus, and brain damage in GMH rats and improve long-term neurological outcomes [71]. Nevertheless, its neuroprotective effect in GMH might not be limited to iron regulation, but could be similar to its protective effect in ICH models where it has been shown to reduce BBB permeability by downregulating matrix metalloproteinases (MMPs) expression and inhibiting neutrophil infiltration, macrophage activation, and production of inflammatory mediator tumor necrosis factor alpha (TNF-α) and interleukin-1 beta (IL-1β) [72]. Importantly, combination therapy of minocycline and deferoxamine reduced the extent of brain damage, neuronal death, and the activation of microglia/macrophages after ICH [73]. These observations indicate that iron chelators might be neuroprotective through reducing iron-triggered oxidative stress.
Peroxisome Proliferator-Activated Receptor-Gamma Agonists
Besides, the peroxisome proliferator-activated receptor-gamma (PPARγ) is a ligand-activated transcription factor with a potential candidacy for GMH treatment. PPARγ plays important role in augmenting the phagocytosis activity of microglia/macrophage and regulating oxidative stress and inflammation [33]. PPARγ stimulation has essentially been shown to improve the long-term neurological function post-GMH in neonatal rats with significant reduction in cortical and white matter loss as well as reduction in post-hemorrhagic ventricular dilation [74]. Treatment with PPARγ agonist augmented phagocytosis and consequently improved hematoma resorption by upregulating CD36 phagocytic receptor expression, together with decreasing the amount of extracellular H2O2 produced during phagocytosis and downregulating the expression of proinflammatory genes, especially those for TNF-a, IL-1b, MMP-9, and inducible NOS, while protecting neurons form secondary injury during this process [74, 75]. Meanwhile, the lipid lowering agent, Simvastatin, has been shown to increase hematoma absorption ratio, reduce ventricular volume, and attenuate neurological dysfunction in rats post-IVH [76], in part by upregulating CD36. Consistently, simvastatin showed similar effects of improving neurological functioning in an ICH rat model, but through activating PPARγ. Therefore, we postulate that simvastatin might act through PPARγ activation to exert its protective functions after GMH.
Other Potential Agents
Moreover, other agents can directly target oxidative stress such as the synthetic antioxidant edaravone, a ROS scavenger. Edaravone reduced brain edema, and lipid peroxidation in rats following IVH, and repeated administration improved learning and memory performance [77]. In addition, hydrogen gas (H2), a potent antioxidant, suppressed mental retardation and cerebral palsy in rats, and normalized brain atrophy after neonatal GMH, although the mechanistic basis was not investigated [78]. Despite diminishing oxidative stress and brain edema in mouse ICH model, inhaled H2 therapy alone was not sufficient to improve delayed ICH clinical outcomes [79].
Albeit the promising preclinical findings of targeting oxidative stress cascades, there is still no clinical evidence of the neuroprotective effects of these agents on GMH/IVH in clinical settings.
Animal Models of IVH
The field of IVH and its complications have been witnessing a remarkable progress throughout the last two decades, as a result of an enhanced understanding of the disease pathogenesis through diverse studies conducted on animal models, as well as advances in neuro-imaging, and clinical trials conducted on premature infants with IVH [80].
Rabbits [81], dogs [82], lambs [83], sheep [84], rats [85], mice [86], and pigs [87] have been used to study GMH, although rodents remain the most commonly used models due to their well characterized neuroanatomy, brain development processes, and synaptogenesis [88,89,90], making them comparable to human brains. Nevertheless, rodents’ brains at birth are less mature than the human brain and IVH do not occur there spontaneously [91].
Therefore, transgenic models have been developed to induce spontaneous bleeding. These include a transgenic mouse with mutations for integrin [92], a transgenic mouse with mutations for procollagen IV [93], and mice overexpressing VEGF [94]. Whereas these models exhibit brain complications that resemble those of IVH, high lethality rates limit their utility to assess long-term neurobehavioral outcomes and neuroinflammation mechanisms.
In addition, GM-IVH has been reproduced by other approaches that instigate bleeding, including glycerol- [95,96,97], blood- [85, 98, 99], or collagenase-[85, 100, 101] induced lesions. These models allow the identification of the exact time and location of bleeding, although the pathophysiology of the lesions hardly resembles that of preterm newborns [91].
Interestingly, GMH occurs spontaneously in 20% of premature rabbit pups [102, 103], which enables the study of triggering factors, and makes rabbits a good candidate model given the similarities between rabbits and human vascular structure of the basal ganglia as well as the perinatal brain growth, and inflammatory changes that occur around the lateral ventricle just like in preterm infants [103].
Discussion and Conclusion
Primary brain injury secondary to GMH is attributed to mechanical pressure induced by the hematoma that forms after ICH. The brain, during all its stages of development including the fully matured brain, is especially sensitive to this kind of injury for two reasons: the neural structures are tightly enclosed by the skulls, making them vulnerable to pressure; and the high oxygen demand of these structures. The presence of these factors makes the damage of primary brain injury spontaneous and practically unavoidable. On the other hand, secondary brain injury is mediated by the various mechanisms explained above and progresses relatively slower than primary brain injury and can possibly be avoided.
The therapeutic approaches to GMH available in the literature to this date are summarized in this review and illustrated in Fig. 1. Many of these approaches are adapted from suggested treatments for ICH or IVH, which share a similar pathophysiology of secondary brain injury [104]. Management approaches currently available or suggested for the treatment of GMH, ICH, or IVH are aimed at slowing damage or in rare occasions stopping it, but there is no therapy aimed at reversing the damage yet [9, 18, 19]. Luckily, neural structures are capable of regeneration to a certain extent, especially in neonates [105]. However, the complexity of these structures and our limited understanding of their function makes therapeutic interventions at this level nearly impossible. For instance, any intervention to reverse brain injury in neonates would not only focus on preventing cell death or cell regeneration but should also take into consideration the synchronized development and function of neurons and glial cells to ensure timely maturation and appropriate connectivity of neural structures [106]. Thus, efforts to develop a therapeutic approach that might reverse the damage of brain injury in neonates should be focused on promoting the natural course of regeneration of neural structures rather than re-inventing the process of regeneration.
Graphical illustration of the oxidative stress mechanisms underlying the pathogenesis of secondary brain injury following germinal matrix hemorrhage and the proposed therapeutic targets. Intraventricular hemorrhage (IVH) induces a rapid wave of cytokine production that activates neutrophils and macrophages. Activated microglia and infiltrated neutrophils produce large amounts of nitric oxide (NO). In addition, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOXs) expressed on the surface of these inflammatory cells stimulates production of reactive oxygen species (ROS) in response to cytokines and other extracellular signals. Minocycline reduces production of inflammatory mediators, whereas melatonin acts to maintain a balance in the NO production protecting against nitrosative damage. After a hemorrhagic event, glutamate release is increased and its uptake is reduced, which results in sustained activation of N-methyl-d-aspartate (NMDA) receptors in postsynaptic neurons. This promotes Ca2+ influx and intracellular Ca2+ overload, activates nitric oxide synthase (NOS) and NOXs, and results in synthesis of large amounts of neuronal NO and superoxide (O2-), whose concomitant interaction forms peroxynitrite (ONOO-). Therapeutic hypothermia (TH) reduces the release of glutamate and thus protects against neuronal excitotoxicity, while melatonin reduces the expression of NOX-1 and NOX-2, thereby limiting the production of ROS. Activated mitochondria generates ROS as a biproduct of its respiration under physiologic conditions. Mitochondrial ROS acts as a major trigger of nucleotide-binding domain-like receptor protein 3 (NLRP3) inflammasome, a component of innate immunity that amplifies the inflammatory response. Melatonin counteracts apoptosis by decreasing the levels of cytochrome C in the cytoplasm, dampening the upregulation of caspase 3, and increasing the ratio of B cell lymphoma protein 2/Bcl-2-associated X (Bcl2/BAX). In parallel, TH also inhibits apoptosis by affecting the levels of Bcl-2 and cytochrome C. Besides, Wingless/Integrated 1 (Wnt1) and Wnt3a protein expression are upregulated in brain tissues resulting in subarachnoid fibrosis. Deferoxamine downregulates Wnt1 and Wnt3a expression, thus protecting against fibrosis. On the other hand, red blood cells degrade and release hemoglobin following hemorrhage, which in turn results in hemin, the oxidized form of heme. Hemin is decomposed into bilirubin, free iron (Fe2+), and carbon monoxide (CO) by heme oxygenase. Free Fe2+ catalyzes the conversion of O2- and H2O2 OH- via Fenton reaction. Deferoxamine and minocycline both act as iron chelators and can inhibit Fenton reaction and production of OH-. Proliferator-activated receptor-gamma (PPARγ) agonist augments phagocytosis mediated by microglia and macrophages and thus improves hematoma resorption, along with decreasing the amount of extracellular H2O2 produced during phagocytosis. Simvastatin can act as PPARγ agonist (Created with Biorender.com).
The fact that oxidative stress is an important determinant in the accumulated damage to neural structures in GMH, ICH, and IVH makes it a favorable target, both from a medical and an economical point of view. For instance, GMH occurs exclusively in neonates while ICH and IVH can affect almost every age group; thus, in theory, developing one therapeutic approach to target several conditions in a wide range of age groups would be appealing to experts and pharmaceutical companies. However, despite promising results of pre-clinical studies, the majority of the proposed treatments did not show encouraging clinical outcomes to date [33]. For example, the trial of deferoxamine mesylate on patients with ICH did not result in a significant difference between the deferoxamine group and placebo group [107], but a post hoc study found significant improvement in disability in patients with a hematoma volume of 10–30 ml only [108]. Delving into the outcomes of the post hoc study [108] reveals the complexity of the disease in question and thus the complexity of management that is to be proposed. Many factors might add to the complexity of brain hemorrhage pathologies. Among those factors are the unique architecture of the neural tissues, special cellular interactions in the brain, and the distinctive regulation of blood flow in the central nervous system. In addition, a closer look into any trial’s population is recommended before drawing conclusions since GMH occurs exclusively in neonates. However, this does not exclude potential benefits of suggested treatments in ICH or IVH if utilized in GMH. Furthermore, sex differences should also be minded in treatment strategies, given that male and female infants have distinct neurodevelopmental profiles. In fact, studies on prophylactic indomethacin for IVH prevention have demonstrated more benefits for male infants from this therapy and emphasized the importance of neonatal sex differences as part of treatment strategies [109, 110]. Congruently, sex-related differences were also observed in TH where males seemed to need deeper levels of hypothermia compared to females for equivalent synaptic protection [14, 111].
Moreover, combining multiple therapeutic approaches may prove efficacious. TH reduces the extent of hypoxic injury by decreasing the high energy demand of brain tissue [27, 56]. TH might be associated with several favorable factors, if used in parallel with one of the pharmacological therapies targeting oxidative stress. One important factor is that TH, in theory, slows cellular death thus slowing the release of oxidative molecules into the brain milieu [59, 60]. Targeting pre-formed oxidative molecules with TH should have a synergistic therapeutic benefit. Moreover, combining TH with other pharmacological therapies would not raise concerns of drug-drug interactions, and we believe that the risk of aggravating drug adverse effects by TH is limited. Pharmacological candidates to be considered for combination with TH include melatonin and deferoxamine. There is evidence that both melatonin and deferoxamine target different oxidative metabolites involved in ICH [62, 63, 66]. Thus, utilizing both medications in combination with TH might prove efficacious in ameliorating the damage of oxidative metabolites in GMH. In fact, melatonin has been administered in combination with TH in a pilot clinical trial in infants with moderate-to-severe hypoxic-ischemic encephalopathy and proved effective in reducing oxidative stress and improving survival without neurological or developmental abnormalities [112].
Moreover, an excellent approach to time sensitive pathologies such as IVH is the “early detection-early intervention” approach. The term “time is brain” commonly linked to stroke can be theoretically extrapolated to IVH as earlier detection and treatment would ultimately be associated with better outcomes. One promising technique is near-infrared spectroscopy (NIRS). NIRS monitoring of the cerebral blood flow and oxygenation levels is an emerging technology aimed for early detection of IVH occurrence [113, 114]. Early detection, if combined with an effective intervention might be a game changer in the management of IVH in premature newborns. We believe that the development of early detection techniques goes hand in hand with new therapeutic approaches as both aspects of the management are of equal importance. Moreover, we hypothesize that NIRS can also be used to monitor and assess treatment efficacy and thus help guide clinical decisions. Alternatively, if proven effective, NIRS can play a role in future research on IVH therapies as it provides real-time in vitro outcome assessment and treatment interval follow-up that can be correlated with real life cases.
Future Directions
Exploring the field of oxidative stress and antioxidants in the neonatal brain unlocks the route to complex interconnected pathways. Findings of future investigations will hold promising results and probably more effective approaches to treat GMH. To that end, prevention measures remain the supreme standard to reduce the risk of IVH until clinical trials incorporate coherent management strategies. Prevention could begin as early as antenatally, with the use of corticosteroids [115], and magnesium sulfate [116], which have proven convenient in reducing the rates of IVH. Postnatal monitoring comes next, especially in the first 72 h after birth, time at which the neonate is most vulnerable to IVH. Minimal handling approach is recommended and currently adopted by many centers, as reduced monitoring such as diaper changes and arterial blood withdrawal, could avoid rapid changes in cerebral blood flow [117]. Collectively, simple acts such as maintaining the head in midline, elevating the head of the incubator, and minimizing IV flushes and rapid arterial blood withdrawal have been sorted out into a “care bundle” that can be easily introduced in any neonatal care unit and would hopefully lower the risk of IVH [118]. Constant surveillance of the cerebral blood flow is also recommended especially in the presence of non-invasive technologies such as NIRS. When combined with blood pressure measurement [119] and targeted neonatal echo (TnEcho) to monitor superior vena cava blood flow [120, 121], NIRS can identify periods of impaired autoregulation and pressure passive states and thus lower the incidence of IVH. Clinical trials are underway to determine the potency of NIRS monitoring in preterm infants in reducing IVH [122]. Meanwhile, NIRS can be utilized in parallel with other techniques for active monitoring until clinical trials validate its efficacy. Prevention, monitoring, and early detection, all pave the way for individual-tailored intervention and hold promise for improved outcomes. Importantly, the areas of active research in the field should focus on identifying accurate neonatal biomarkers implicated in oxidative stress pathways that can predict newborns at high risk of developing secondary brain injury. We also recommend further evaluation of diagnostic methods including imaging techniques such NIRS, to understand the time course of oxidative tissue injury and thus determine the best therapeutic window. Moreover, we hypothesize that combining therapeutic approaches will yield more favorable outcomes and thus should be considered in future trials.
Abbreviations
- Bcl-2/Bax:
-
B cell lymphoma protein 2/Bcl-2-associated X
- H2O2 :
-
Hydrogen peroxide
- IVH:
-
Intraventricular hemorrhage
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NLRP3:
-
Nucleotide-binding domain-like receptor protein 3
- NMDA:
-
N-methyl-d-aspartate
- NMDAR:
-
NMDA receptors
- NO:
-
Nitric oxide
- NOS:
-
Neuronal nitric oxide synthase
- NOX:
-
NADPH oxidase
- ONOO- :
-
Peroxynitrite
- O2 - :
-
Superoxide
- PPARγ:
-
Proliferator-activated receptor-gamma
- ROS:
-
Reactive oxygen species
- TH:
-
Therapeutic hypothermia
- Wnt:
-
Wingless/integrated
- OH:
-
Hydroxyl radical
References
Ballabh P, Braun A, Nedergaard M. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004;16:1–13. https://doi.org/10.1016/j.nbd.2003.12.016.
Brouwer AJ, Groenendaal F, Benders MJ, de Vries LS. Early and late complications of germinal matrix-intraventricular haemorrhage in the preterm infant: what is new? Neonatology. 2014;106:296–303. https://doi.org/10.1159/000365127.
Mukerji A, Shah V, Shah PS. Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: a meta-analysis. Pediatrics. 2015;136:1132–43. https://doi.org/10.1542/peds.2015-0944.
O'Shea TM, Allred EN, Kuban KC, Hirtz D, Specter B, Durfee S, Paneth N, Leviton A. Intraventricular hemorrhage and developmental outcomes at 24 months of age in extremely preterm infants. J Child Neurol. 2012;27:22–9. https://doi.org/10.1177/0883073811424462.
Song J, Nilsson G, Xu Y, Zelco A, Rocha-Ferreira E, Wang Y, Zhang X, Zhang S, Ek J, Hagberg H, et al. Temporal brain transcriptome analysis reveals key pathological events after germinal matrix hemorrhage in neonatal rats. J Cereb Blood Flow Metab. 2022;42:1632–49. https://doi.org/10.1177/0271678x221098811.
Tan AP, Svrckova P, Cowan F, Chong WK, Mankad K. Intracranial hemorrhage in neonates: a review of etiologies, patterns and predicted clinical outcomes. Eur J Paediatr Neurol. 2018;22:690–717. https://doi.org/10.1016/j.ejpn.2018.04.008.
Klebe D, McBride D, Krafft PR, Flores JJ, Tang J, Zhang JH. Posthemorrhagic hydrocephalus development after germinal matrix hemorrhage: established mechanisms and proposed pathways. J Neurosci Res. 2020;98:105–20. https://doi.org/10.1002/jnr.24394.
Ballabh P, Braun A, Nedergaard M. Anatomic analysis of blood vessels in germinal matrix, cerebral cortex, and white matter in developing infants. Pediatr Res. 2004;56:117–24. https://doi.org/10.1203/01.Pdr.0000130472.30874.Ff.
Ballabh P, Xu H, Hu F, Braun A, Smith K, Rivera A, Lou N, Ungvari Z, Goldman SA, Csiszar A, et al. Angiogenic inhibition reduces germinal matrix hemorrhage. Nat Med. 2007;13:477–85. https://doi.org/10.1038/nm1558.
Ballabh P. Pathogenesis and prevention of intraventricular hemorrhage. Clin Perinatol. 2014;41:47–67. https://doi.org/10.1016/j.clp.2013.09.007.
Raybaud C, Ahmad T, Rastegar N, Shroff M, Al Nassar M. The premature brain: developmental and lesional anatomy. Neuroradiology. 2013;55(Suppl 2):23–40. https://doi.org/10.1007/s00234-013-1231-0.
Takashima S, Tanaka K. Microangiography and vascular permeability of the subependymal matrix in the premature infant. Can J Neurol Sci. 1978;5:45–50.
Cuestas E, Bas J, Pautasso J. Sex differences in intraventricular hemorrhage rates among very low birth weight newborns. Gend Med. 2009;6:376–82. https://doi.org/10.1016/j.genm.2009.06.001.
Rosenkrantz TS, Hussain Z, Fitch RH. Sex differences in brain injury and repair in newborn infants: clinical evidence and biological mechanisms. Front Pediatr. 2019;7:211. https://doi.org/10.3389/fped.2019.00211.
Baenziger O, Jaggi JL, Mueller AC, Morales CG, Lipp HP, Lipp AE, Duc G, Bucher HU. Cerebral blood flow in preterm infants affected by sex, mechanical ventilation, and intrauterine growth. Pediatr Neurol. 1994;11:319–24. https://doi.org/10.1016/0887-8994(94)90009-4.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8. https://doi.org/10.1203/PDR.0b013e3181c1b176.
Parodi A, Govaert P, Horsch S, Bravo MC, Ramenghi LA, Agut T, Alarcon A, Arena R, Bartocci M, Bravo M, et al. Cranial ultrasound findings in preterm germinal matrix haemorrhage, sequelae and outcome. Pediatr Res. 2020;87:13–24. https://doi.org/10.1038/s41390-020-0780-2.
Ballabh P, de Vries LS. White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies. Nat Rev Neurol. 2021;17:199–214. https://doi.org/10.1038/s41582-020-00447-8.
Garton T, Hua Y, Xiang J, Xi G, Keep RF. Challenges for intraventricular hemorrhage research and emerging therapeutic targets. Expert Opin Ther Targets. 2017;21:1111–22. https://doi.org/10.1080/14728222.2017.1397628.
Hanley DF. Intraventricular hemorrhage: severity factor and treatment target in spontaneous intracerebral hemorrhage. Stroke. 2009;40:1533–8. https://doi.org/10.1161/strokeaha.108.535419.
Romantsik O, Bruschettini M, Ley D. Intraventricular hemorrhage and white matter injury in preclinical and clinical studies. Neoreviews. 2019;20:e636–52. https://doi.org/10.1542/neo.20-11-e636.
Sadrzadeh SM, Graf E, Panter SS, Hallaway PE, Eaton JW. Hemoglobin. A biologic fenton reagent. J Biol Chem. 1984;259:14354–6.
Czerska M, Mikołajewska K, Zieliński M, Gromadzińska J, Wąsowicz W. Today's oxidative stress markers. Med Pr. 2015;66:393–405. https://doi.org/10.13075/mp.5893.00137.
Hu X, Tao C, Gan Q, Zheng J, Li H, You C. Oxidative stress in intracerebral hemorrhage: sources, mechanisms, and therapeutic targets. Oxid Med Cell Longev. 2016;2016:3215391. https://doi.org/10.1155/2016/3215391.
Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev. 2014;94:909–50. https://doi.org/10.1152/physrev.00026.2013.
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84. https://doi.org/10.1016/j.biocel.2006.07.001.
Martini S, Castellini L, Parladori R, Paoletti V, Aceti A, Corvaglia L. Free radicals and neonatal brain injury: from underlying pathophysiology to antioxidant treatment perspectives. Antioxidants (Basel). 2021;10 https://doi.org/10.3390/antiox10122012.
Orellana-Urzúa S, Claps G, Rodrigo R. Improvement of a novel proposal for antioxidant treatment against brain damage occurring in ischemic stroke patients. CNS Neurol Disord Drug Targets. 2021;20:3–21. https://doi.org/10.2174/1871527319666200910153431.
Dani C, Cecchi A, Bertini G. Role of oxidative stress as physiopathologic factor in the preterm infant. Minerva Pediatr. 2004;56:381–94.
Marseglia L, D'Angelo G, Manti S, Arrigo T, Barberi I, Reiter RJ, Gitto E. Oxidative stress-mediated aging during the fetal and perinatal periods. Oxid Med Cell Longev. 2014;2014:358375. https://doi.org/10.1155/2014/358375.
Ozsurekci Y, Aykac K. Oxidative stress related diseases in newborns. Oxid Med Cell Longev. 2016;2016:2768365. https://doi.org/10.1155/2016/2768365.
Dawes W. Secondary brain injury following neonatal intraventricular hemorrhage: the role of the ciliated ependyma. Front Pediatr. 2022;10:887606. https://doi.org/10.3389/fped.2022.887606.
Zhang Y, Khan S, Liu Y, Wu G, Yong VW, Xue M. Oxidative stress following intracerebral hemorrhage: from molecular mechanisms to therapeutic targets. Front Immunol. 2022;13:847246. https://doi.org/10.3389/fimmu.2022.847246.
Goulding DS, Vogel RC, Gensel JC, Morganti JM, Stromberg AJ, Miller BA. Acute brain inflammation, white matter oxidative stress, and myelin deficiency in a model of neonatal intraventricular hemorrhage. J Neurosurg Pediatr. 2020;26:613–23. https://doi.org/10.3171/2020.5.Peds20124.
Leijser LM, de Vries LS. Preterm brain injury: germinal matrix-intraventricular hemorrhage and post-hemorrhagic ventricular dilatation. Handb Clin Neurol. 2019;162:173–99. https://doi.org/10.1016/b978-0-444-64029-1.00008-4.
Niemczyk E, Majczak A, Hallmann A, Kedzior J, Woźniak M, Wakabayashi T. A possible involvement of plasma membrane NAD(P)H oxidase in the switch mechanism of the cell death mode from apoptosis to necrosis in menadione-induced cell injury. Acta Biochim Pol. 2004;51:1015–22.
Galluzzi L, Vitale I, Aaronson SA, Abrams JM, Adam D, Agostinis P, Alnemri ES, Altucci L, Amelio I, Andrews DW, et al. Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018;25:486–541. https://doi.org/10.1038/s41418-017-0012-4.
Li L, Yun D, Zhang Y, Tao Y, Tan Q, Qiao F, Luo B, Liu Y, Fan R, Xian J, et al. A cannabinoid receptor 2 agonist reduces blood-brain barrier damage via induction of MKP-1 after intracerebral hemorrhage in rats. Brain Res. 2018;1697:113–23. https://doi.org/10.1016/j.brainres.2018.06.006.
Yang C, Hawkins KE, Doré S, Candelario-Jalil E. Neuroinflammatory mechanisms of blood-brain barrier damage in ischemic stroke. Am J Physiol Cell Physiol. 2019;316:C135–53. https://doi.org/10.1152/ajpcell.00136.2018.
Panfoli I, Candiano G, Malova M, De Angelis L, Cardiello V, Buonocore G, Ramenghi LA. Oxidative stress as a primary risk factor for brain damage in preterm newborns. Front Pediatr. 2018;6:369. https://doi.org/10.3389/fped.2018.00369.
Saugstad OD. Hypoxanthine as an indicator of hypoxia: its role in health and disease through free radical production. Pediatr Res. 1988;23:143–50. https://doi.org/10.1203/00006450-198802000-00001.
Liu Y, Wei J, Chang M, Liu Z, Li D, Hu S, Hu L. Proteomic analysis of endothelial progenitor cells exposed to oxidative stress. Int J Mol Med. 2013;32:607–14. https://doi.org/10.3892/ijmm.2013.1419.
Zia MT, Csiszar A, Labinskyy N, Hu F, Vinukonda G, LaGamma EF, Ungvari Z, Ballabh P. Oxidative-nitrosative stress in a rabbit pup model of germinal matrix hemorrhage: role of NAD(P)H oxidase. Stroke. 2009;40:2191–8. https://doi.org/10.1161/strokeaha.108.544759.
Zhang R, Brennan ML, Shen Z, MacPherson JC, Schmitt D, Molenda CE, Hazen SL. Myeloperoxidase functions as a major enzymatic catalyst for initiation of lipid peroxidation at sites of inflammation. J Biol Chem. 2002;277:46116–22. https://doi.org/10.1074/jbc.M209124200.
Kupsco A, Schlenk D. Oxidative stress, unfolded protein response, and apoptosis in developmental toxicity. Int Rev Cell Mol Biol. 2015;317:1–66. https://doi.org/10.1016/bs.ircmb.2015.02.002.
Yao Z, Bai Q, Wang G. Mechanisms of oxidative stress and therapeutic targets following intracerebral hemorrhage. Oxid Med Cell Longev. 2021;2021:8815441. https://doi.org/10.1155/2021/8815441.
Ma Q, Chen S, Hu Q, Feng H, Zhang JH, Tang J. NLRP3 inflammasome contributes to inflammation after intracerebral hemorrhage. Ann Neurol. 2014;75:209–19. https://doi.org/10.1002/ana.24070.
Iadecola C. Bright and dark sides of nitric oxide in ischemic brain injury. Trends Neurosci. 1997;20:132–9. https://doi.org/10.1016/s0166-2236(96)10074-6.
Goulay R, Naveau M, Gaberel T, Vivien D, Parcq J. Optimized tPA: a non-neurotoxic fibrinolytic agent for the drainage of intracerebral hemorrhages. J Cereb Blood Flow Metab. 2018;38:1180–9. https://doi.org/10.1177/0271678x17719180.
Wang Z, Chen Z, Yang J, Yang Z, Yin J, Duan X, Shen H, Li H, Wang Z, Chen G. Treatment of secondary brain injury by perturbing postsynaptic density protein-95-NMDA receptor interaction after intracerebral hemorrhage in rats. J Cereb Blood Flow Metab. 2019;39:1588–601. https://doi.org/10.1177/0271678x18762637.
Qu J, Chen W, Hu R, Feng H. The injury and therapy of reactive oxygen species in intracerebral hemorrhage looking at mitochondria. Oxid Med Cell Longev. 2016;2016:2592935. https://doi.org/10.1155/2016/2592935.
Hanafy KA, Gomes JA, Selim M. Rationale and current evidence for testing iron chelators for treating stroke. Curr Cardiol Rep. 2019;21:20. https://doi.org/10.1007/s11886-019-1106-z.
Li J, Cao F, Yin H-L, Huang Z-J, Lin Z-T, Mao N, Sun B, Wang G. Ferroptosis: past, present and future. Cell Death & Dis. 2020;11:88. https://doi.org/10.1038/s41419-020-2298-2.
Yang WS, Stockwell BR. Ferroptosis: death by lipid peroxidation. Trends Cell Biol. 2016;26:165–76. https://doi.org/10.1016/j.tcb.2015.10.014.
Wan J, Ren H, Wang J. Iron toxicity, lipid peroxidation and ferroptosis after intracerebral haemorrhage. Stroke Vasc Neurol. 2019;4:93. https://doi.org/10.1136/svn-2018-000205.
Douglas-Escobar M, Weiss MD. Hypoxic-ischemic encephalopathy: a review for the clinician. JAMA Pediatr. 2015;169:397–403. https://doi.org/10.1001/jamapediatrics.2014.3269.
Martinello K, Hart AR, Yap S, Mitra S, Robertson NJ. Management and investigation of neonatal encephalopathy: 2017 update. Arch Dis Child Fetal Neonatal Ed. 2017;102:F346–58. https://doi.org/10.1136/archdischild-2015-309639.
Edwards AD, Yue X, Squier MV, Thoresen M, Cady EB, Penrice J, Cooper CE, Wyatt JS, Reynolds EO, Mehmet H. Specific inhibition of apoptosis after cerebral hypoxia-ischaemia by moderate post-insult hypothermia. Biochem Biophys Res Commun. 1995;217:1193–9. https://doi.org/10.1006/bbrc.1995.2895.
Thoresen M, Penrice J, Lorek A, Cady EB, Wylezinska M, Kirkbride V, Cooper CE, Brown GC, Edwards AD, Wyatt JS, et al. Mild hypothermia after severe transient hypoxia-ischemia ameliorates delayed cerebral energy failure in the newborn piglet. Pediatr Res. 1995;37:667–70. https://doi.org/10.1203/00006450-199505000-00019.
Schumacker PT, Rowland J, Saltz S, Nelson DP, Wood LD. Effects of hyperthermia and hypothermia on oxygen extraction by tissues during hypovolemia. J Appl Physiol. 1987;63:1246–52. https://doi.org/10.1152/jappl.1987.63.3.1246.
Thoresen M, Wyatt J. Keeping a cool head, post-hypoxic hypothermia--an old idea revisited. Acta Paediatr. 1997;86:1029–33. https://doi.org/10.1111/j.1651-2227.1997.tb14799.x.
Reiter RJ, Tan DX, Osuna C, Gitto E. Actions of melatonin in the reduction of oxidative stress. A review. J Biomed Sci. 2000;7:444–58. https://doi.org/10.1007/bf02253360.
Wang Z, Zhou F, Dou Y, Tian X, Liu C, Li H, Shen H, Chen G. Melatonin alleviates intracerebral hemorrhage-induced secondary brain injury in rats via suppressing apoptosis, inflammation, oxidative stress, DNA damage, and mitochondria injury. Transl Stroke Res. 2018;9:74–91. https://doi.org/10.1007/s12975-017-0559-x.
Martini S, Austin T, Aceti A, Faldella G, Corvaglia L. Free radicals and neonatal encephalopathy: mechanisms of injury, biomarkers, and antioxidant treatment perspectives. Pediatr Res. 2020;87:823–33. https://doi.org/10.1038/s41390-019-0639-6.
Blanco S, Hernández R, Franchelli G, Ramos-Álvarez MM, Peinado M. Melatonin influences NO/NOS pathway and reduces oxidative and nitrosative stress in a model of hypoxic-ischemic brain damage. Nitric Oxide. 2017;62:32–43. https://doi.org/10.1016/j.niox.2016.12.001.
Matsuki N, Takanohashi A, Boffi FM, Inanami O, Kuwabara M, Ono K. Hydroxyl radical generation and lipid peroxidation in C2C12 myotube treated with iodoacetate and cyanide. Free Radic Res. 1999;31:1–8. https://doi.org/10.1080/10715769900300551.
Meng H, Li F, Hu R, Yuan Y, Gong G, Hu S, Feng H. Deferoxamine alleviates chronic hydrocephalus after intraventricular hemorrhage through iron chelation and Wnt1/Wnt3a inhibition. Brain Res. 2015;1602:44–52. https://doi.org/10.1016/j.brainres.2014.08.039.
Cisternas P, Vio CP, Inestrosa NC. Role of Wnt signaling in tissue fibrosis, lessons from skeletal muscle and kidney. Curr Mol Med. 2014;14:510–22. https://doi.org/10.2174/1566524014666140414210346.
Miao CG, Yang YY, He X, Huang C, Huang Y, Zhang L, Lv XW, Jin Y, Li J. Wnt signaling in liver fibrosis: progress, challenges and potential directions. Biochimie. 2013;95:2326–35. https://doi.org/10.1016/j.biochi.2013.09.003.
Klebe D, Krafft PR, Hoffmann C, Lekic T, Flores JJ, Rolland W, Zhang JH. Acute and delayed deferoxamine treatment attenuates long-term sequelae after germinal matrix hemorrhage in neonatal rats. Stroke. 2014;45:2475–9. https://doi.org/10.1161/strokeaha.114.005079.
Guo J, Chen Q, Tang J, Zhang J, Tao Y, Li L, Zhu G, Feng H, Chen Z. Minocycline-induced attenuation of iron overload and brain injury after experimental germinal matrix hemorrhage. Brain Res. 2015;1594:115–24. https://doi.org/10.1016/j.brainres.2014.10.046.
Liu Y, Li Z, Khan S, Zhang R, Wei R, Zhang Y, Xue M, Yong VW. Neuroprotection of minocycline by inhibition of extracellular matrix metalloproteinase inducer expression following intracerebral hemorrhage in mice. Neurosci Lett. 2021;764:136297. https://doi.org/10.1016/j.neulet.2021.136297.
Li Z, Liu Y, Wei R, Khan S, Xue M, Yong VW. The combination of deferoxamine and minocycline strengthens neuroprotective effect on acute intracerebral hemorrhage in rats. Neurol Res. 2021;43:854–64. https://doi.org/10.1080/01616412.2021.1939487.
Flores JJ, Klebe D, Rolland WB, Lekic T, Krafft PR, Zhang JH. PPARγ-induced upregulation of CD36 enhances hematoma resolution and attenuates long-term neurological deficits after germinal matrix hemorrhage in neonatal rats. Neurobiol Dis. 2016;87:124–33. https://doi.org/10.1016/j.nbd.2015.12.015.
Zhao X, Sun G, Zhang J, Strong R, Song W, Gonzales N, Grotta JC, Aronowski J. Hematoma resolution as a target for intracerebral hemorrhage treatment: role for peroxisome proliferator-activated receptor gamma in microglia/macrophages. Ann Neurol. 2007;61:352–62. https://doi.org/10.1002/ana.21097.
Chen Q, Shi X, Tan Q, Feng Z, Wang Y, Yuan Q, Tao Y, Zhang J, Tan L, Zhu G, et al. Simvastatin promotes hematoma absorption and reduces hydrocephalus following intraventricular hemorrhage in part by upregulating CD36. Transl Stroke Res. 2017;8:362–73. https://doi.org/10.1007/s12975-017-0521-y.
Chen Z, Zhang J, Chen Q, Guo J, Zhu G, Feng H. Neuroprotective effects of edaravone after intraventricular hemorrhage in rats. Neuroreport. 2014;25:635–40. https://doi.org/10.1097/wnr.0000000000000050.
Lekic T, Manaenko A, Rolland W, Fathali N, Peterson M, Tang J, Zhang JH. Protective effect of hydrogen gas therapy after germinal matrix hemorrhage in neonatal rats. Acta Neurochir Suppl. 2011;111:237–41. https://doi.org/10.1007/978-3-7091-0693-8_40.
Manaenko A, Lekic T, Ma Q, Ostrowski RP, Zhang JH, Tang J. Hydrogen inhalation is neuroprotective and improves functional outcomes in mice after intracerebral hemorrhage. Acta Neurochir Suppl. 2011;111:179–83. https://doi.org/10.1007/978-3-7091-0693-8_30.
Cheng B, Ballabh P. Recovery of the brain after intraventricular hemorrhage. Semin Fetal Neonatal Med. 2022;27:101224. https://doi.org/10.1016/j.siny.2021.101224.
Dohare P, Zia MT, Ahmed E, Ahmed A, Yadala V, Schober AL, Ortega JA, Kayton R, Ungvari Z, Mongin AA, et al. AMPA-Kainate receptor inhibition promotes neurologic recovery in premature rabbits with intraventricular hemorrhage. J Neurosci. 2016;36:3363–77. https://doi.org/10.1523/jneurosci.4329-15.2016.
Goddard J, Lewis RM, Alcala H, Zeller RS. Intraventricular hemorrhage--an animal model. Biol Neonate. 1980;37:39–52. https://doi.org/10.1159/000241254.
Wheeler AS, Sadri S, Gutsche BB, DeVore JS, David-Mian Z, Latyshevsky H. Intracranial hemorrhage following intravenous administration of sodium bicarbonate or saline solution in the newborn lamb asphyxiated in utero. Anesthesiology. 1979;51:517–21. https://doi.org/10.1097/00000542-197912000-00007.
Reynolds ML, Evans CA, Reynolds EO, Saunders NR, Durbin GM, Wigglesworth JS. Intracranial haemorrhage in the preterm sheep fetus. Early Hum Dev. 1979;3:163–86. https://doi.org/10.1016/0378-3782(79)90005-7.
Lekic T, Manaenko A, Rolland W, Tang J, Zhang JH. A novel preclinical model of germinal matrix hemorrhage using neonatal rats. Acta Neurochir Suppl. 2011;111:55–60. https://doi.org/10.1007/978-3-7091-0693-8_10.
Segado-Arenas A, Infante-Garcia C, Benavente-Fernandez I, Sanchez-Sotano D, Ramos-Rodriguez JJ, Alonso-Ojembarrena A, Lubian-Lopez S, Garcia-Alloza M. Cognitive impairment and brain and peripheral alterations in a murine model of intraventricular hemorrhage in the preterm newborn. Mol Neurobiol. 2018;55:4896–910. https://doi.org/10.1007/s12035-017-0693-1.
Mayfrank L, Kissler J, Raoofi R, Delsing P, Weis J, Küker W, Gilsbach JM. Ventricular dilatation in experimental intraventricular hemorrhage in pigs. Characterization of cerebrospinal fluid dynamics and the effects of fibrinolytic treatment. Stroke. 1997;28:141–8. https://doi.org/10.1161/01.str.28.1.141.
Christopherson KS, Ullian EM, Stokes CC, Mullowney CE, Hell JW, Agah A, Lawler J, Mosher DF, Bornstein P, Barres BA. Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell. 2005;120:421–33. https://doi.org/10.1016/j.cell.2004.12.020.
Goritz C, Mauch DH, Pfrieger FW. Multiple mechanisms mediate cholesterol-induced synaptogenesis in a CNS neuron. Mol Cell Neurosci. 2005;29:190–201. https://doi.org/10.1016/j.mcn.2005.02.006.
Semple BD, Blomgren K, Gimlin K, Ferriero DM, Noble-Haeusslein LJ. Brain development in rodents and humans: Identifying benchmarks of maturation and vulnerability to injury across species. Prog Neurobiol. 2013;106-107:1–16. https://doi.org/10.1016/j.pneurobio.2013.04.001.
Atienza-Navarro I, Alves-Martinez P, Lubian-Lopez S, Garcia-Alloza M. Germinal matrix-intraventricular hemorrhage of the preterm newborn and preclinical models: inflammatory considerations. Int J Mol Sci. 2020;21 https://doi.org/10.3390/ijms21218343.
McCarty JH, Monahan-Earley RA, Brown LF, Keller M, Gerhardt H, Rubin K, Shani M, Dvorak HF, Wolburg H, Bader BL, et al. Defective associations between blood vessels and brain parenchyma lead to cerebral hemorrhage in mice lacking alphav integrins. Mol Cell Biol. 2002;22:7667–77. https://doi.org/10.1128/mcb.22.21.7667-7677.2002.
Gould DB, Phalan FC, Breedveld GJ, van Mil SE, Smith RS, Schimenti JC, Aguglia U, van der Knaap MS, Heutink P, John SW. Mutations in Col4a1 cause perinatal cerebral hemorrhage and porencephaly. Science. 2005;308:1167–71. https://doi.org/10.1126/science.1109418.
Yang D, Baumann JM, Sun YY, Tang M, Dunn RS, Akeson AL, Kernie SG, Kallapur S, Lindquist DM, Huang EJ, et al. Overexpression of vascular endothelial growth factor in the germinal matrix induces neurovascular proteases and intraventricular hemorrhage. Sci Transl Med. 2013;5:193ra190. https://doi.org/10.1126/scitranslmed.3005794.
Dohare P, Cheng B, Ahmed E, Yadala V, Singla P, Thomas S, Kayton R, Ungvari Z, Ballabh P. Glycogen synthase kinase-3β inhibition enhances myelination in preterm newborns with intraventricular hemorrhage, but not recombinant Wnt3A. Neurobiol Dis. 2018;118:22–39. https://doi.org/10.1016/j.nbd.2018.06.015.
Fischer EG, Lorenzo AV, Landis WJ, Welch K, Ofori-Kwakye SK, Dorval B, Hodgens KJ, Kerr CS. Vasculature to the germinal matrix in rabbit pups. J Neurosurg. 1986;64:650–6. https://doi.org/10.3171/jns.1986.64.4.0650.
Georgiadis P, Xu H, Chua C, Hu F, Collins L, Huynh C, Lagamma EF, Ballabh P. Characterization of acute brain injuries and neurobehavioral profiles in a rabbit model of germinal matrix hemorrhage. Stroke. 2008;39:3378–88. https://doi.org/10.1161/strokeaha.107.510883.
Cherian SS, Love S, Silver IA, Porter HJ, Whitelaw AG, Thoresen M. Posthemorrhagic ventricular dilation in the neonate: development and characterization of a rat model. J Neuropathol Exp Neurol. 2003;62:292–303. https://doi.org/10.1093/jnen/62.3.292.
Strahle JM, Garton T, Bazzi AA, Kilaru H, Garton HJ, Maher CO, Muraszko KM, Keep RF, Xi G. Role of hemoglobin and iron in hydrocephalus after neonatal intraventricular hemorrhage. Neurosurgery. 2014;75:696–705; discussion 706,. https://doi.org/10.1227/neu.0000000000000524.
Li P, Zhao G, Ding Y, Wang T, Flores J, Ocak U, Wu P, Zhang T, Mo J, Zhang JH, et al. Rh-IFN-α attenuates neuroinflammation and improves neurological function by inhibiting NF-κB through JAK1-STAT1/TRAF3 pathway in an experimental GMH rat model. Brain Behav Immun. 2019;79:174–85. https://doi.org/10.1016/j.bbi.2019.01.028.
Tao Y, Li L, Jiang B, Feng Z, Yang L, Tang J, Chen Q, Zhang J, Tan Q, Feng H, et al. Cannabinoid receptor-2 stimulation suppresses neuroinflammation by regulating microglial M1/M2 polarization through the cAMP/PKA pathway in an experimental GMH rat model. Brain Behav Immun. 2016;58:118–29. https://doi.org/10.1016/j.bbi.2016.05.020.
Lorenzo AV, Welch K. Preterm rabbit model of intraventricular hemorrhage. J Neurosurg. 1986;64:688–9. https://doi.org/10.3171/jns.1986.64.4.0688.
Lorenzo AV, Welch K, Conner S. Spontaneous germinal matrix and intraventricular hemorrhage in prematurely born rabbits. J Neurosurg. 1982;56:404–10. https://doi.org/10.3171/jns.1982.56.3.0404.
Aronowski J, Zhao X. Molecular pathophysiology of cerebral hemorrhage: secondary brain injury. Stroke. 2011;42:1781–6. https://doi.org/10.1161/strokeaha.110.596718.
Sanai N, Nguyen T, Ihrie RA, Mirzadeh Z, Tsai HH, Wong M, Gupta N, Berger MS, Huang E, Garcia-Verdugo JM, et al. Corridors of migrating neurons in the human brain and their decline during infancy. Nature. 2011;478:382–6. https://doi.org/10.1038/nature10487.
Salmaso N, Jablonska B, Scafidi J, Vaccarino FM, Gallo V. Neurobiology of premature brain injury. Nat Neurosci. 2014;17:341–6. https://doi.org/10.1038/nn.3604.
Selim M, Foster LD, Moy CS, Xi G, Hill MD, Morgenstern LB, Greenberg SM, James ML, Singh V, Clark WM, et al. Deferoxamine mesylate in patients with intracerebral haemorrhage (i-DEF): a multicentre, randomised, placebo-controlled, double-blind phase 2 trial. Lancet Neurol. 2019;18:428–38. https://doi.org/10.1016/s1474-4422(19)30069-9.
Wei C, Wang J, Foster LD, Yeatts SD, Moy C, Mocco J, Selim M, Palesch Y, Griffin J, Perlmutter A, et al. Effect of deferoxamine on outcome according to baseline hematoma volume: a post hoc analysis of the i-DEF trial. Stroke. 2022;53:1149–56. https://doi.org/10.1161/STROKEAHA.121.035421.
Ohlsson A, Roberts RS, Schmidt B, Davis P, Moddeman D, Saigal S, Solimano A, Vincer M, Wright L. Male/female differences in indomethacin effects in preterm infants. J Pediatr. 2005;147:860–2. https://doi.org/10.1016/j.jpeds.2005.07.032.
Vohr BR, Allan WC, Westerveld M, Schneider KC, Katz KH, Makuch RW, Ment LR. School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics. 2003;111:e340–6. https://doi.org/10.1542/peds.111.4.e340.
Dietz RM, Deng G, Orfila JE, Hui X, Traystman RJ, Herson PS. Therapeutic hypothermia protects against ischemia-induced impairment of synaptic plasticity following juvenile cardiac arrest in sex-dependent manner. Neuroscience. 2016;325:132–41. https://doi.org/10.1016/j.neuroscience.2016.03.052.
D'Angelo G, Chimenz R, Reiter RJ, Gitto E. Use of melatonin in oxidative stress related neonatal diseases. Antioxidants (Basel). 2020;9 https://doi.org/10.3390/antiox9060477.
Elser HE, Holditch-Davis D, Brandon DH. Cerebral oxygenation monitoring: a strategy to detect IVH and PVL. Newborn Infant Nurs Rev. 2011;11:153–9. https://doi.org/10.1053/j.nainr.2011.07.007.
Variane GFT, Chock VY, Netto A, Pietrobom RFR, Van Meurs KP. Simultaneous near-infrared spectroscopy (NIRS) and amplitude-integrated electroencephalography (aEEG): dual use of brain monitoring techniques improves our understanding of physiology. Front Pediatr. 2020;7 https://doi.org/10.3389/fped.2019.00560.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454. https://doi.org/10.1002/14651858.CD004454.pub3.
Doyle LW, Crowther CA, Middleton P, Marret S, Rouse D. Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. Cochrane Database Syst Rev. 2009:CD004661. https://doi.org/10.1002/14651858.CD004661.pub3.
Szymonowicz W, Yu VY, Walker A, Wilson F. Reduction in periventricular haemorrhage in preterm infants. Arch Dis Child. 1986;61:661–5. https://doi.org/10.1136/adc.61.7.661.
de Bijl-Marcus K, Brouwer AJ, De Vries LS, Groenendaal F, Wezel-Meijler GV. Neonatal care bundles are associated with a reduction in the incidence of intraventricular haemorrhage in preterm infants: a multicentre cohort study. Arch Dis Child Fetal Neonatal Ed. 2020;105:419–24. https://doi.org/10.1136/archdischild-2018-316692.
Garvey AA, Kooi EMW, Smith A, Dempsey EM. Interpretation of cerebral oxygenation changes in the preterm infant. Children (Basel). 2018;5 https://doi.org/10.3390/children5070094.
Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2000;82:F188–94. https://doi.org/10.1136/fn.82.3.f188.
Sortica da Costa C, Cardim D, Molnar Z, Kelsall W, Ng I, Czosnyka M, Smielewski P, Austin T. Changes in hemodynamics, cerebral oxygenation and cerebrovascular reactivity during the early transitional circulation in preterm infants. Pediatr Res. 2019;86:247–53. https://doi.org/10.1038/s41390-019-0410-z.
Hansen ML, Pellicer A, Gluud C, Dempsey E, Mintzer J, Hyttel-Sørensen S, Heuchan AM, Hagmann C, Ergenekon E, Dimitriou G, et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomised clinical phase III trial. Trials. 2019;20:811. https://doi.org/10.1186/s13063-019-3955-6.
Funding
No funding or financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nour Eldine, M., Alhousseini, M., Nour-Eldine, W. et al. The Role of Oxidative Stress in the Progression of Secondary Brain Injury Following Germinal Matrix Hemorrhage. Transl. Stroke Res. 15, 647–658 (2024). https://doi.org/10.1007/s12975-023-01147-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-023-01147-3