Abstract
Purpose of Review
The purpose of this paper was to review the role of cardiac computed tomography (CCT) in both the diagnostic and management pathways of heart failure.
Recent Findings
CT has an essential role in non-invasively excluding coronary artery disease but also can provide additional information that can aid the investigation of the patient presenting with heart failure. CT images provide high-quality information about cardiac structure and pericardium. Cardiac anatomical information, such as the location and size of coronary sinuses, can assist in lead placement in cardiac resynchronisation therapy. Cardiac CT with fractional flow reserve calculation can also provide functional information on the severity of coronary stenosis. Cardiac CT with delayed contrast enhancement also has an emerging role in myocardial tissue characterisation which can contribute to risk stratification in cardiomyopathy patients. CT also may fit better into pathways of screening and monitoring of potential adverse cardiac events in the short-term and long-term assessment of cancer patients who may already be getting a CT for other reasons.
Summary
CT has an evolving role in both the diagnosis and management of heart failure and future research could examine the potential risks, benefits, efficiency and costs of clinical pathways where cardiac CT is more central to the diagnosis and management of patients with heart failure and possible cardiomyopathy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) affects approximately 26 million worldwide [1, 2], with estimated total costs in the United States (US) alone predicted to reach $69.7 billion by 2030 [3]. The estimated prevalence of symptomatic HF in the US and Europe ranges from 0.4 to 2% [4], whereas prevalence estimates in Asia are significantly higher, ranging from 1.3 to 6.7% [5].
Currently, the main roles of cardiac computed tomography (CCT) are in calcium scoring in cardiovascular risk stratification and use of computed tomography coronary angiography (CTCA) in diagnostic evaluation of patients presenting with low or intermediate risk of coronary artery disease (CAD) [6]. However, CCT is being increasingly employed among patients with heart failure to ascertain the absence or presence of CAD with additional information obtained in the same acquisition on cardiac structure, pericardium and myocardium.
In investigating what is often a complex clinical picture, non-invasive cardiac imaging can be utilised for both determining aetiology of HF and in risk assessment. Currently, transthoracic echocardiogram is utilised early in the diagnostic pathway to categorise HF based on left ventricular ejection fraction (LVEF) (refer to Fig. 1) [7], whilst cardiac CT is especially appropriate in investigating for an ischaemic aetiology of HF. With the underlying aetiology of heart failure in our populations changing away from the common ischaemic pathologies, cardiac CT may have a role in determining aetiology of other types of heart failure, such as in cardio-oncology, that is screening and assessment of cancer survivors that may subsequently develop cardiomyopathy and HF related to other cardiotoxic agents. CTCA screening in these patients may be a component of chest CT screening, and able to exclude coronary artery disease as well as screen for cardiomyopathy.
Stepwise approach to management of heart failure (as described in [7]). CHF, congestive heart failure; ECG, electrocardiogram; CXR, chest X-ray; LVEF, left ventricular ejection fraction; HFrEF, heart failure with reduced ejection fraction; HFmEF, heart failure with mid-range ejection fraction; HFpEF, heart failure with preserved ejection fraction; CP, constrictive pericarditis; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; CT, computed tomography; MRI, magnetic resonance imaging; ICD, implantable cardioverter defibrillator; ARVC, arrhythmogenic right ventricular cardiomyopathy
Cardiac CT in the Diagnostic Workup of Heart Failure
Cardiac CT has become the investigation of choice for ruling out CAD in patients presenting for the first time with HF, and without a history of known CAD. Its popularity is driven by virtue of its less-invasive nature compared with coronary angiography as well as its very high sensitivity (95–100% in most series) and strong negative predictive value. It also has moderately high specificity for determining the presence of significant CAD. In the same acquisition, CTCA can also provide high-quality information on cardiac structure and depending on acquisition sequencing chosen, ventricular wall function and viability. Hence, whilst echocardiography is undisputedly first line in the initial evaluation of HF, cardiac CT is viewed as having an important role in the overall diagnostic evaluation of a HF patient.
CT Evaluation of Coronary Artery Disease in Heart Failure Patients
Accuracy of CT Coronary Angiography
There is increasing reliance on CTCA in place of invasive coronary angiography for the exclusion of significant CAD (Fig. 1); it is important to consider its negative predictive value for exclusion of an ischaemic aetiology for heart failure. A number of authors have demonstrated the accuracy of CTCA in comparison with invasive coronary angiogram, with or without fractional flow reserve measurement [8,9,10] (refer to Table 1). Further, differences in the number of slices of data captured for every gantry rotation do not appear to affect the accuracy of CTCA on modern scanners [11,12,13,14]. Overall, a high level of accuracy was found for CTCA, with notably excellent sensitivity and negative predictive value (NPV) findings.
As shown in Fig. 1, both CT and cardiac magnetic resonance imaging (CMR) can be used synergistically within a heart failure evaluation pathway. In excluding ischaemia for patients with newly diagnosed systolic HF, one prospective study compared invasive catheter angiography and echocardiography to a novel non-invasive strategy combining CTCA and CMR. The per-patient sensitivity and specificity of CTCA was 100% and 90%, respectively, NPV 100%, positive predictive value (PPV) 78%. Interestingly, combining CTCA with CMR conferred 100% specificity, 100% sensitivity, 100% PPV and 100% NPV for detection or exclusion of CAD [15].
Recent literature also demonstrates that in patients without significant CAD, combining CTCA with CMR improves the overall diagnostic accuracy for detecting CAD. Groothuis et al. found that combining these modalities significantly improved overall accuracy and specificity (91% and 94% respectively) in comparison with the use of either test alone: CTCA (57% and 39% respectively, p < 0.0001) and CMR (83% and 82% respectively, p = 0.016) [16]. A future approach that synthesises the modalities can be considered, although the advantageous increase in accuracy must be weighed alongside the disadvantageous increase in cost and time.
CT Coronary Angiography and the Assessment of Fractional Flow Reserve
It is well established that CTCA is accurate in providing anatomical information regarding coronary artery stenosis. However, there have been doubts regarding its ability to provide functional assessment of coronary artery stenosis. CT-derived fractional flow reserve has been proposed as a viable alternative to invasive fractional flow reserve for detecting coronary ischaemic lesions. A systematic review of 3 significant studies showed high diagnostic accuracy of CT-derived fractional flow reserve [17]. At per-patient analysis for 609 combined data, CT-derived fractional flow reserve had identical sensitivity (both 0.89) but improved specificity (0.71 vs 0.35), PPV (0.70 vs 0.52) and NPV (0.90 vs 0.81) compared with CTCA, but at per-vessel analysis had slightly lower sensitivity (0.83 vs 0.86), identical NPV (both 0.92), but improved specificity (0.78 vs 0.56) and PPV (0.61 vs 0.38). Hence, it is possible that CT-derived fractional flow reserve could provide an adequate assessment of the functional status of the coronary arteries, without the need for invasive procedure.
CT Calcium Scoring in Screening for Ischaemic Heart Failure
The determination of calcium score utilising non-contrast CT potentially provides a non-invasive and low-dose radiation screening technique for coronary atherosclerosis. The quantification of coronary artery calcium score (CAC) using CT is a non-invasive imaging technique requiring minimal radiation exposure without need for contrast or beta blockade [18]. It is reliable in providing a depiction of overall plaque burden [19] in coronary atherosclerosis, by extension playing a role in identifying HF secondary to ischaemic cardiomyopathy. Further, CAC progression has been shown to predict incident HF even independent of cardiovascular risk factors, baseline CAC and clinically overt heart disease [20]. Whilst a calcium score of zero does not completely exclude CAD, it does have a high negative predictive value. Also, as demonstrated by a study of 1308 consecutive symptomatic patients who underwent 64-slice CTCA with a zero calcium score that found obstructive non-calcified plaques (diameter stenosis > 50%) in 7% of patients [21], the yield is dependent on the pre-test probability that it is likely higher in symptomatic compared with asymptomatic patients. In asymptomatic individuals without chest pain, CAC score of zero identified patients to be at low risk of future cardiac events when compared with a score > 0 [22, 23]. Correspondingly, in a review of the literature, a pooled analysis of 10,355 patients found the NPV of a CAC of zero to be high (93%) for CAD [24].
In a notable study, Ten Kate et al. prospectively included 93 symptomatic patients with newly diagnosed HF of unknown aetiology and LVEF < 45% [25]. In all patients, the CAC was determined, and CTCA was performed if CTCS > 0. Invasive coronary angiography was used as the gold standard for distinguishing between patients with HF of CAD-associated aetiology, and those of non-CAD origin, and follow-up data of 20 ± 16 months found that a lack of coronary artery calcification ruled out HF of CAD-associated aetiology in 46% of patients. A CT-based algorithm utilising CAC in all patients and CTCA in those with abnormal CAC had 100% sensitivity, 95% specificity, 67% PPV and 100% NPV for detecting HF of CAD-associated aetiology.
Further, Mylonas et al. demonstrated that quantification of CAC from a single contrast-enhanced CTCA scan was feasible and correlated well with CAC without contrast; a development on the traditional non-contrast CT quantification of CAC [26]. Hence, one can hypothesise that if CAC and CTCA are both done in the same scan with prominent efficacy, then the synergistic use of the two could potentially be used in future evaluation of the coronary arteries, and by extension in ruling out ischaemic aetiology of HF.
A Cardio-Oncological Perspective
Cancer and Atherosclerosis
The development of subclinical atherosclerosis, as determined by CAC, has shown association with a diagnosis of cancer. Interestingly, Whitlock et al. followed up 3,122 subjects over a 10-year period and found the incidence of CAC to be independently associated with cancer even after accounting for atherosclerotic risk factors. However, they failed to establish whether the presence of cancer accelerated CAC over time [27].
Heart Failure Secondary to Cancer Chemotherapy
Cardiac monitoring is having a more defined role in the short-term as well as long-term monitoring of cancer patients and survivors. This is due to the recognition that there are both short- and long-term adverse effects of a variety of cancer chemotherapeutic agents [28,29,30,31,32,33,34,35,36,37,38,39,40]. The highest incidence has been reported by the anthracycline doxorubicin and the most common cardiac adverse event is left ventricular (LV) systolic dysfunction and resultant HF. Early detection of cardiac dysfunction and prompt initiation of heart failure treatment could potentially mitigate the cardiotoxic effects of anthracyclines [41], though further studies are needed.
CT in the Assessment of Ventricular Function
Currently, cardiac CT is not first line in the assessment of ventricular function, and is only indicated for LV assessment following inadequate image procurement from other non-invasive methods, and for right ventricular (RV) assessment in both quantitative evaluation and morphological inspection in suspected arrhythmogenic RV cardiomyopathy [6]. The use of cardiac CT for LV function assessment is hence not commonplace in the investigative pathway of HF. In the context of a good-quality echo, the degree of usefulness of CT needs to be balanced against the greater radiation load, as to acquire LV function assessment on CT, the acquisition needs to comprise retrospective ECG helical gating. Retrospective ECG-gated CTCA are now rarely required to obtain good-quality images of the coronary arteries, particularly in the optimised patient with controlled regular heart rate. Arsanjani et al. demonstrated that CTCA does have the capability to measure LV dysfunction and volumes [42].
Echocardiography is currently the imaging modality of choice for the assessment of ventricular function, despite notable underestimation of LV volumes when compared with the gold standard of CMR [43]. By extension, LV volumes from multi-detector CT are not significantly different to those obtained from cardiac MRI [43]. It is important to note that despite echocardiography’s accessibility and lack of radiation, its resolution is limited in situations such as obesity and the hyperinflated air-trapping of emphysema. In such cases, CMR or cardiac CT scanning may be effectively utilised to assess ventricular function in patients with suspected HF.
Systolic Assessment
HF patients with reduced LVEF have impaired systolic function, and by extension, it is crucial to evaluate the ventricles during systole. Despite being first line for this purpose, echocardiography is known to have inferior accuracy compared with CT and CMR, with the latter modalities being further down the diagnostic pathway mainly due to their accompanying radiation (CTCA) or cost (CMR). Whilst it is possible to assess the ventricles in systole with significant accuracy in CT, CMR is still the superior modality. This was highlighted by Schlosser et al., who found higher LV volumes with lower LVEF and cardiac output findings in multi-detector CT when it was compared with CMR; the discrepancy hypothesised to come from the use of beta-blockers prior to CT scanning [44]. However, with a non-contrast cardiac CT, Nasir et al. did find it possible in a single scan to both gauge CAC and estimate LV size with comparable accuracy to CMR [45]. This added utility provided by CT highlights future promise, despite it being secondary within the investigative hierarchy for systolic ventricular assessment.
Diastolic Assessment
Diastolic LV assessment is a necessity in HF patients with preserved LVEF, and although echocardiography is classically used for this evaluation, cardiac CT does provide a degree of usefulness. Boogers et al. compared cardiac CT (via transmitral velocity and mitral septal tissue velocity) with 2-dimensional echocardiography and demonstrated a 79% diagnostic accuracy in the former for detecting diastolic dysfunction [46]. Whilst CT is rarely used in practice for this purpose, a notable implementation can be seen in the morphological assessment of the pericardium in constrictive pericarditis [47], a cause of diastolic HF with preserved LVEF.
The Role of CT in Myocardial Characterisation
Whilst CMR is currently the gold standard for visualisation of the myocardium [6], in certain situations, cardiac CT’s ability to characterise tissue with a high spatial resolution in short acquisition times may be of use. CMR is not possible in patients with claustrophobia, most patients with cardiac devices, and requires relatively long times for acquisition. In comparison with CTCA, less patient preparation is required for myocardial CT with more freedom in target heart rates, creating the possibility of a more accessible modality despite sharing other limiting factors. However, the beam-hardening artefact of CT creates a problem specific to the myocardium, with contrast in the ventricles resulting in ‘shadowing’ over the myocardium that can compromise adequate evaluation [48].
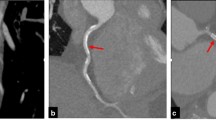
A relatively novel advancement in cardiac CT imaging is use of delayed enhancement to detect myocardial scar within a viability assessment. The practice uses the similar kinetic properties shared by iodinated contrast agents in CT and the gadolinium agents of CMR (where delayed enhancement is classically employed), resulting in comparable myocardial characterisation between modalities [49]. For CMR, quantitative late gadolinium enhancement is established as a potent tool to risk-stratify hypertrophic cardiomyopathy patients, given its prognostic value in predicting sudden cardiac death [50]. The presence of late gadolinium enhancement on CMR predicts all-cause mortality, ventricular arrhythmia, sudden cardiac death, cardiovascular mortality and major adverse cardiovascular events, independent of LVEF in both ischaemic and non-ischaemic cardiomyopathy [51, 52]. In the evaluation of the myocardium post-infarction, animal studies have shown that CT utilising delayed enhancement is a valid imaging modality [53, 54]. Whilst delayed enhancement in CT has some promise, the equivalent phenomenon in CMR is known to have superior resolution and less difficulties in patients with respiratory pathology [49]. In addition, > 18 g of myocardial fibrosis (as assessed by CT) is associated with increased risk of spontaneous ventricular arrhythmias resulting in ICD activation for patients with hypertrophic cardiomyopathy [55]. This opens the possibility of risk-stratifying HF patients who would benefit from implantable defibrillator. Hence, whilst delayed enhancement in CMR is currently (and rightfully so) used over CT, the current promise shown by the latter warrants its consideration in the context of CMR being contra-indicated, as well as supports the notion that future research is needed in the area.
CT in Assessing the Pericardium
CT allows visualisation of the entire pericardium, a feature that can be necessary in diagnosing constrictive pericarditis, which presents classically as mainly right-sided HF. CT is also essential in the preoperative workup of some patients with constrictive pericarditis, especially to depict the extension of calcifications and for those with a history of prior cardiothoracic surgery [56].
However, the CT attenuation of pericardium is similar to that of the myocardium, and hence, the pericardium can be most clearly visualised where it is surrounded by fat and not immediately adjacent to the myocardium [57]. A cardiac CT scan can detect even small amounts of calcification, pericardial thickness > 4 mm, RV narrowing and tubular deformation, normal or small ventricular size and straightening of the inter-ventricular septum. If there is clinical evidence of impaired filling, pericardial thickening is virtually diagnostic of CP [58].
Given its accessibility, echocardiography is currently first line in imaging for pericardial pathology but this at times comes at a cost of limited visualisation of the entire pericardium due to restricted acoustic windows, with lesions in the anterior pericardium particularly affected [59]. Alternatively, whilst being a less accessible imaging modality with the added negative of radiation exposure [60], a 2017 systematic review (40 studies and total of 1,244 patients) recognised that CT is an excellent tool to determine pericardial thickness and the most sensitive technique to identify pericardial calcification, but that echocardiography, followed by CMR, is preferred in the contemporary diagnosis of constrictive pericarditis [61]. In somewhat of a compromise, Alter et al. found that CT provided a modality that can be used in conjunction with echocardiography for substantiation of a diagnosis of constrictive pericarditis [62]. CT is particularly sensitive for identifying pericardial calcification [57]. CT density measurements may provide superior characterisation of pericardial fluid than echocardiography, with pericardial inflammation displaying contrast enhancement [63].
CT in Cardiac Resynchronisation Therapy for Heart Failure
Cardiac resynchronisation therapy (CRT) is well established in management of congestive heart failure refractory to medical therapy [64,65,66]. However, it has been shown that the CRT procedure can be unsuccessful in at least 5 to 12% of patients [67]. Failure of LV lead placement has been attributed to the inability to insert catheters in the coronary sinus and the lack of suitable side branches [68]. The 256-slice CT performed prior to consideration of CRT implantation provides excellent non-invasive visualisation of the cardiac venous anatomy, which may facilitate left ventricular lead positioning for the procedure [69].
A potential solution to the issue of CRT clinical non-responders might be avoiding left ventricular lead placement adjacent to scarred myocardium. Multi-modality imaging utilising imaging-guided LV lead placement using cardiac CT venography, 99 m technetium myocardial perfusion imaging and speckle-tracking echocardiography radial strain has been used to target the optimal coronary sinus branch closest to the non-scarred myocardial segment with latest mechanical activation. Sommer et al. assessed this in comparison with traditional X-ray-guided LV lead implantation in a posterolateral region with late electrical activation, finding more optimal placement in the multi-modality group (83% vs 65%, P = 0.01) [70].
Cardiac CT: an Inter-Play Between Benefits and Risks
Justifying the use of cardiac CT is a product of the play-off between the risks associated with radiation and contrast exposure against the benefits, relative accuracy and convenience of a non-invasive imaging modality that can rapidly exclude a variety of heart disease pathologies including coronary artery disease cardiac structural abnormalities, pericardial abnormalities and potentially myocardial abnormalities. Unlike CMR where the presence of a magnetic field precludes its use in patients with implanted devices or prostheses, CT’s use of radiation instead offers an avenue of imaging in such situations. Notably, as CTCA has some radiation exposure whilst CMR has none, the latter can safely be used during pregnancy where the former is contraindicated.
It is important to limit radiation exposure to patients from diagnostic or interventional medical procedures to minimise their long-term risk of cancer secondary to radiation exposure. CTCA requires radiation exposure, and hence an understanding of the magnitude of the radiation exposure involved is mandatory, with an explanation of the innate risks of the modality being a necessity for optimal patient care. A multicentre 2019 study by Alhailiy et al. found that the effective dose for CTCA is 5.2 mSv [71], which is lower than that expected from invasive coronary angiogram [10]. Further, this radiation dose associated with CTCA is higher in those with greater BMI and higher heart rate [72], or atrial fibrillation [73]. However, with recent improvements in CTCA technology, use of a third-generation dual-source scanner has demonstrated that an effective dose of 0.63 mSv can produce a very good image quality even in overweight or obese patients [74]. This was echoed by Stocker et al., who conducted a study in 2018 of 4502 patients from 61 hospitals in 32 countries who underwent CTCA reported a 78% decrease in total radiation dose per patient when compared with a similar survey from 2007, hence demonstrating considerable reduction of radiation exposure over the last decade [75].
The technique of prospectively triggered CTCA can significantly reduce radiation when compared with retrospectively gated CTCA [76]). Optimising heart rate using beta blockers or calcium channel blockers prior to the procedure also improves image quality and reduces radiation.
CTCA is generally contraindicated in patients with significant renal impairment because of the high risk of acute-on-chronic renal failure secondary to contrast-induced nephrotoxicity. It can be minimised by adequate hydration pre and post CTCA. Davenport et al. performed a large-scale propensity score-matched study and found that intravenous contrast media administration was a risk factor for contrast-induced nephrotoxicity only in patients with an eGFR of less than 30 mL/min/1.73 m2 [77]. Diabetes associated with chronic kidney disease is an additional risk factor for contrast-induced nephrotoxicity [78].
If a patient is known to be allergic to contrast, the prophylactic corticosteroid treatment can potentially avoid an allergic reaction. However, Jung et al. found that despite corticosteroid prophylaxis, 3.4% of high-risk patients still experienced moderate to severe reactions, and 14.3% of patients with a severe index reaction again had a severe reaction [79].
Additionally, image acquisition in CT is possible in a few minutes unlike CMR where patients are exposed to the possibility of claustrophobia with enclosure in the CMR tunnel for 30–60 min. Being non-invasive, CTCA also does not require hospital admission unlike invasive coronary angiogram where monitoring post-procedure is usually crucial. Invasive coronary angiogram would potentially be associated with less than 1% possibility of complications such as vascular complications, stroke, acute myocardial infarction, coronary artery dissection and significantly greater radiation exposure than CT coronary angiogram as mentioned previously. Finally, CT has greater accessibility than CMR, but less than echocardiography.
Financially responsible healthcare requires an assessment of prospective cost-efficiency prior to selecting any potential investigation tool. Cardiac CT is no different, with economic consideration being crucial to correct implementation within functional healthcare infrastructure. In a 2015 study comparing the cost of non-invasive CTCA with conventional invasive conventional coronary angiography for the detection of significant CAD, it was found that the average cost of CTCA (based on the use of a 64-slice CT scanner active for 10 h per day) was approximately 13% of that required for invasive coronary angiography [80]. Whilst it makes sense for a non-invasive procedure to be significantly cheaper than its invasive counterpart, it is also important to consider potential intraprocedural modifications that can be made to further reduce costs in the CTCA. Igarashi et al. found that administering the β-blocker landiolol to appropriately reduce heart rate during cardiac CTCA reduced expected costs by approximately 4% per patient when compared with placebo, demonstrating cost-saving efficacy for CTCA diagnosis in CAD patients with tachycardia [81].
Conclusion
CTCA plays an important role in the exclusion of coronary artery disease in patients with heart failure. Calcium scoring may be a reasonable initial test to reduce the number of patients that require full CTCA with contrast. Cardiac CT also has an evolving role in obtaining non-coronary cardiac information and functional information for coronary stenosis and ventricular function. Cardiac CT may hence provide a reasonable alternative if CMR and/or echocardiography are relatively contra-indicated, or perhaps in the context of improving efficiency, minimising numbers of tests and associated costs in the investigation of this patient cohort. Future research should compare the accuracy, benefits and cost-effectiveness of different clinical pathways involving multi-modality testing for the evaluation of patients with heart failure in the future.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11. https://doi.org/10.15420/cfr.2016:25:2.
Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1(1):4–25. https://doi.org/10.1002/ehf2.12005.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19. https://doi.org/10.1161/HHF.0b013e318291329a.
Guha K, McDonagh T. Heart failure epidemiology: European perspective. Curr Cardiol Rev. 2013;9(2):123–7.
Sakata Y, Shimokawa H. Epidemiology of heart failure in Asia. Circ J. 2013;77(9):2209–17.
Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Cardiovasc Comput Tomogr. 2010;4(6):407 e1–33. doi:https://doi.org/10.1016/j.jcct.2010.11.001.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200. https://doi.org/10.1093/eurheartj/ehw128.
Ramos V, Bettencourt N, Silva J, Ferreira N, Chiribiri A, Schuster A, et al. Noninvasive anatomical and functional assessment of coronary artery disease. Rev Port Cardiol. 2015;34(4):223–32. https://doi.org/10.1016/j.repc.2014.10.008.
Zhang LJ, Wang Y, Schoepf UJ, Meinel FG, Bayer RR 2nd, Qi L, et al. Image quality, radiation dose, and diagnostic accuracy of prospectively ECG-triggered high-pitch coronary CT angiography at 70 kVp in a clinical setting: comparison with invasive coronary angiography. Eur Radiol. 2016;26(3):797–806. https://doi.org/10.1007/s00330-015-3868-z.
Stehli J, Fuchs TA, Bull S, Clerc OF, Possner M, Buechel RR, et al. Accuracy of coronary CT angiography using a submillisievert fraction of radiation exposure: comparison with invasive coronary angiography. J Am Coll Cardiol. 2014;64(8):772–80. https://doi.org/10.1016/j.jacc.2014.04.079.
Uehara M, Takaoka H, Kobayashi Y, Funabashi N. Diagnostic accuracy of 320-slice computed-tomography for detection of significant coronary artery stenosis in patients with various heart rates and heart rhythms compared with conventional coronary-angiography. Int J Cardiol. 2013;167(3):809–15. https://doi.org/10.1016/j.ijcard.2012.02.017.
Petcherski O, Gaspar T, Halon DA, Peled N, Jaffe R, Molnar R, et al. Diagnostic accuracy of 256-row computed tomographic angiography for detection of obstructive coronary artery disease using invasive quantitative coronary angiography as reference standard. Am J Cardiol. 2013;111(4):510–5. https://doi.org/10.1016/j.amjcard.2012.10.036.
Madhok R, Aggarwal A. Comparison of 128-slice dual source CT coronary angiography with invasive coronary angiography. J Clin Diagn Res. 2014;8(6):RC08–11. https://doi.org/10.7860/JCDR/2014/9568.4514.
Sajjadieh A, Hekmatnia A, Keivani M, Asoodeh A, Pourmoghaddas M, Sanei H. Diagnostic performance of 64-row coronary CT angiography in detecting significant stenosis as compared with conventional invasive coronary angiography. ARYA Atheroscler. 2013;9(2):157–63.
Hamilton-Craig C, Strugnell WE, Raffel OC, Porto I, Walters DL, Slaughter RE. CT angiography with cardiac MRI: non-invasive functional and anatomical assessment for the etiology in newly diagnosed heart failure. Int J Card Imaging. 2012;28(5):1111–22. https://doi.org/10.1007/s10554-011-9926-y.
Groothuis JG, Beek AM, Brinckman SL, Meijerink MR, van den Oever ML, Hofman MB, et al. Combined non-invasive functional and anatomical diagnostic work-up in clinical practice: the magnetic resonance and computed tomography in suspected coronary artery disease (MARCC) study. Eur Heart J. 2013;34(26):1990–8. https://doi.org/10.1093/eurheartj/eht077.
Li S, Tang X, Peng L, Luo Y, Dong R, Liu J. The diagnostic performance of CT-derived fractional flow reserve for evaluation of myocardial ischaemia confirmed by invasive fractional flow reserve: a meta-analysis. Clin Radiol. 2015;70(5):476–86. https://doi.org/10.1016/j.crad.2014.12.013.
Kim KP, Einstein AJ, Berrington de Gonzalez A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch Intern Med. 2009;169(13):1188–94. https://doi.org/10.1001/archinternmed.2009.162.
Alluri K, Joshi PH, Henry TS, Blumenthal RS, Nasir K, Blaha MJ. Scoring of coronary artery calcium scans: history, assumptions, current limitations, and future directions. Atherosclerosis. 2015;239(1):109–17. https://doi.org/10.1016/j.atherosclerosis.2014.12.040.
Bakhshi H, Ambale-Venkatesh B, Yang X, Ostovaneh MR, Wu CO, Budoff M, et al. Progression of coronary artery calcium and incident heart failure: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6(4). https://doi.org/10.1161/JAHA.116.005253.
Ito T, Suzuki Y, Ehara M, Matsuo H, Teramoto T, Terashima M, et al. Impact of epicardial fat volume on coronary artery disease in symptomatic patients with a zero calcium score. Int J Cardiol. 2013;167(6):2852–8. https://doi.org/10.1016/j.ijcard.2012.07.026.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–45. https://doi.org/10.1056/NEJMoa072100.
Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2(6):675–88. https://doi.org/10.1016/j.jcmg.2008.12.031.
Nasir K, Clouse M. Role of nonenhanced multidetector CT coronary artery calcium testing in asymptomatic and symptomatic individuals. Radiology. 2012;264(3):637–49. https://doi.org/10.1148/radiol.12110810.
ten Kate GJ, Caliskan K, Dedic A, Meijboom WB, Neefjes LA, Manintveld OC, et al. Computed tomography coronary imaging as a gatekeeper for invasive coronary angiography in patients with newly diagnosed heart failure of unknown aetiology. Eur J Heart Fail. 2013;15(9):1028–34. https://doi.org/10.1093/eurjhf/hft090.
Mylonas I, Alam M, Amily N, Small G, Chen L, Yam Y, et al. Quantifying coronary artery calcification from a contrast-enhanced cardiac computed tomography angiography study. Eur Heart J Cardiovasc Imaging. 2014;15(2):210–5. https://doi.org/10.1093/ehjci/jet144.
Whitlock MC, Yeboah J, Burke GL, Chen H, Klepin HD, Hundley WG. Cancer and its association with the development of coronary artery calcification: an assessment from the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2015;4(11). https://doi.org/10.1161/JAHA.115.002533.
Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med. 2016;375(15):1457–67. https://doi.org/10.1056/NEJMra1100265.
Pai VB, Nahata MC. Cardiotoxicity of chemotherapeutic agents: incidence, treatment and prevention. Drug Saf. 2000;22(4):263–302. https://doi.org/10.2165/00002018-200022040-00002.
Von Hoff DD, Layard MW, Basa P, Davis HL Jr, Von Hoff AL, Rozencweig M, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91(5):710–7.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79. https://doi.org/10.1002/cncr.11407.
Gottdiener JS, Appelbaum FR, Ferrans VJ, Deisseroth A, Ziegler J. Cardiotoxicity associated with high-dose cyclophosphamide therapy. Arch Intern Med. 1981;141(6):758–63.
Martin M, Pienkowski T, Mackey J, Pawlicki M, Guastalla JP, Weaver C, et al. Adjuvant docetaxel for node-positive breast cancer. N Engl J Med. 2005;352(22):2302–13. https://doi.org/10.1056/NEJMoa043681.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53(24):2231–47. https://doi.org/10.1016/j.jacc.2009.02.050.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352(24):2487–98. https://doi.org/10.1056/NEJMoa043445.
Chu TF, Rupnick MA, Kerkela R, Dallabrida SM, Zurakowski D, Nguyen L, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet. 2007;370(9604):2011–9. https://doi.org/10.1016/S0140-6736(07)61865-0.
Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002;20(5):1215–21. https://doi.org/10.1200/JCO.2002.20.5.1215.
Perez EA, Koehler M, Byrne J, Preston AJ, Rappold E, Ewer MS. Cardiac safety of lapatinib: pooled analysis of 3689 patients enrolled in clinical trials. Mayo Clin Proc. 2008;83(6):679–86. https://doi.org/10.4065/83.6.679.
Khakoo AY, Kassiotis CM, Tannir N, Plana JC, Halushka M, Bickford C, et al. Heart failure associated with sunitinib malate: a multitargeted receptor tyrosine kinase inhibitor. Cancer. 2008;112(11):2500–8. https://doi.org/10.1002/cncr.23460.
Bair SM, Choueiri TK, Moslehi J. Cardiovascular complications associated with novel angiogenesis inhibitors: emerging evidence and evolving perspectives. Trends Cardiovasc Med. 2013;23(4):104–13. https://doi.org/10.1016/j.tcm.2012.09.008.
Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacomi G, et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol. 2010;55(3):213–20. https://doi.org/10.1016/j.jacc.2009.03.095.
Arsanjani R, Berman DS, Gransar H, Cheng VY, Dunning A, Lin FY, et al. Left ventricular function and volume with coronary CT angiography improves risk stratification and identification of patients at risk for incident mortality: results from 7758 patients in the prospective multinational CONFIRM observational cohort study. Radiology. 2014;273(1):70–7. https://doi.org/10.1148/radiol.14122816.
Rigolli M, Anandabaskaran S, Christiansen JP, Whalley GA. Bias associated with left ventricular quantification by multimodality imaging: a systematic review and meta-analysis. Open Heart. 2016;3(1):e000388. https://doi.org/10.1136/openhrt-2015-000388.
Schlosser T, Mohrs OK, Magedanz A, Voigtlander T, Schmermund A, Barkhausen J. Assessment of left ventricular function and mass in patients undergoing computed tomography (CT) coronary angiography using 64-detector-row CT: comparison to magnetic resonance imaging. Acta Radiol. 2007;48(1):30–5. https://doi.org/10.1080/02841850601067611.
Nasir K, Katz R, Mao S, Takasu J, Bomma C, Lima JA, et al. Comparison of left ventricular size by computed tomography with magnetic resonance imaging measures of left ventricle mass and volumes: the multi-ethnic study of atherosclerosis. J Cardiovasc Comput Tomogr. 2008;2(3):141–8. https://doi.org/10.1016/j.jcct.2008.01.003.
Boogers MJ, van Werkhoven JM, Schuijf JD, Delgado V, El-Naggar HM, Boersma E, et al. Feasibility of diastolic function assessment with cardiac CT: feasibility study in comparison with tissue Doppler imaging. JACC Cardiovasc Imaging. 2011;4(3):246–56. https://doi.org/10.1016/j.jcmg.2010.11.017.
Flachskampf FA, Biering-Sorensen T, Solomon SD, Duvernoy O, Bjerner T, Smiseth OA. Cardiac imaging to evaluate left ventricular diastolic function. JACC Cardiovasc Imaging. 2015;8(9):1071–93. https://doi.org/10.1016/j.jcmg.2015.07.004.
Shen Z, Lee O, Taguchi K. Beam hardening and motion artifacts in cardiac CT: evaluation and iterative correction method. SPIE Medical Imaging SPIE. 2016.
Rodriguez-Granillo GA. Delayed enhancement cardiac computed tomography for the assessment of myocardial infarction: from bench to bedside. Cardiovasc Diagn Ther. 2017;7(2):159–70. https://doi.org/10.21037/cdt.2017.03.16.
Weng Z, Yao J, Chan RH, He J, Yang X, Zhou Y, et al. Prognostic value of LGE-CMR in HCM: a meta-analysis. JACC Cardiovasc Imaging. 2016;9(12):1392–402. https://doi.org/10.1016/j.jcmg.2016.02.031.
Ganesan AN, Gunton J, Nucifora G, McGavigan AD, Selvanayagam JB. Impact of late gadolinium enhancement on mortality, sudden death and major adverse cardiovascular events in ischemic and nonischemic cardiomyopathy: a systematic review and meta-analysis. Int J Cardiol. 2018;254:230–7. https://doi.org/10.1016/j.ijcard.2017.10.094.
Zaman S, Goldberger JJ, Kovoor P. Sudden death risk-stratification in 2018-2019: the old and the new. Heart Lung Circ. 2019;28(1):57–64. https://doi.org/10.1016/j.hlc.2018.08.027.
Lardo AC, Cordeiro MA, Silva C, Amado LC, George RT, Saliaris AP, et al. Contrast-enhanced multidetector computed tomography viability imaging after myocardial infarction: characterization of myocyte death, microvascular obstruction, and chronic scar. Circulation. 2006;113(3):394–404. https://doi.org/10.1161/CIRCULATIONAHA.105.521450.
Schuleri KH, Centola M, George RT, Amado LC, Evers KS, Kitagawa K, et al. Characterization of peri-infarct zone heterogeneity by contrast-enhanced multidetector computed tomography: a comparison with magnetic resonance imaging. J Am Coll Cardiol. 2009;53(18):1699–707. https://doi.org/10.1016/j.jacc.2009.01.056.
Shiozaki AA, Senra T, Arteaga E, Martinelli Filho M, Pita CG, Avila LF, et al. Myocardial fibrosis detected by cardiac CT predicts ventricular fibrillation/ventricular tachycardia events in patients with hypertrophic cardiomyopathy. J Cardiovasc Comput Tomogr. 2013;7(3):173–81. https://doi.org/10.1016/j.jcct.2013.04.002.
Bogaert J, Francone M. Pericardial disease: value of CT and MR imaging. Radiology. 2013;267(2):340–56. https://doi.org/10.1148/radiol.13121059.
Cosyns B, Plein S, Nihoyanopoulos P, Smiseth O, Achenbach S, Andrade MJ, et al. European Association of Cardiovascular Imaging (EACVI) position paper: multimodality imaging in pericardial disease. Eur Heart J Cardiovasc Imaging. 2015;16(1):12–31. https://doi.org/10.1093/ehjci/jeu128.
Al-Mallah MH, Almasoudi F, Ebid M, Ahmed AM, Jamiel A. Multimodality imaging of pericardial diseases. Curr Treat Options Cardiovasc Med. 2017;19(12):89. https://doi.org/10.1007/s11936-017-0590-y.
Wang ZJ, Reddy GP, Gotway MB, Yeh BM, Hetts SW, Higgins CB. CT and MR imaging of pericardial disease. Radiographics. 2003;23 Spec No::S167–80. https://doi.org/10.1148/rg.23si035504.
Adler Y, Charron P, Imazio M, Badano L, Baron-Esquivias G, Bogaert J, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Rev Esp Cardiol (Engl Ed). 2015;68(12):1126. https://doi.org/10.1016/j.rec.2015.10.008.
Ardhanari S, Yarlagadda B, Parikh V, Dellsperger KC, Chockalingam A, Balla S, et al. Systematic review of non-invasive cardiovascular imaging in the diagnosis of constrictive pericarditis. Indian Heart J. 2017;69(1):57–67. https://doi.org/10.1016/j.ihj.2016.06.004.
Alter P, Figiel JH, Rupp TP, Bachmann GF, Maisch B, Rominger MB. MR, CT, and PET imaging in pericardial disease. Heart Fail Rev. 2013;18(3):289–306. https://doi.org/10.1007/s10741-012-9309-z.
Imazio M, Brucato A, Derosa FG, Lestuzzi C, Bombana E, Scipione F, et al. Aetiological diagnosis in acute and recurrent pericarditis: when and how. J Cardiovasc Med (Hagerstown). 2009;10(3):217–30. https://doi.org/10.2459/JCM.0b013e328322f9b1.
Smolis-Bak E, Dabrowski R, Piotrowicz E, Chwyczko T, Dobraszkiewicz-Wasilewska B, Kowalik I, et al. Hospital-based and telemonitoring guided home-based training programs: effects on exercise tolerance and quality of life in patients with heart failure (NYHA class III) and cardiac resynchronization therapy. A randomized, prospective observation. Int J Cardiol. 2015;199:442–7. https://doi.org/10.1016/j.ijcard.2015.07.041.
Kyriacou A, Pabari PA, Mayet J, Peters NS, Davies DW, Lim PB, et al. Cardiac resynchronization therapy and AV optimization increase myocardial oxygen consumption, but increase cardiac function more than proportionally. Int J Cardiol. 2014;171(2):144–52. https://doi.org/10.1016/j.ijcard.2013.10.026.
Frigerio M, Lunati M, Pasqualucci D, Vargiu S, Foti G, Pedretti S, et al. Left ventricular ejection fraction overcrossing 35% after one year of cardiac resynchronization therapy predicts long term survival and freedom from sudden cardiac death: single center observational experience. Int J Cardiol. 2014;172(1):64–71. https://doi.org/10.1016/j.ijcard.2013.12.005.
Abraham WT, Hayes DL. Cardiac resynchronization therapy for heart failure. Circulation. 2003;108(21):2596–603. https://doi.org/10.1161/01.CIR.0000096580.26969.9A.
Puglisi A, Lunati M, Marullo AG, Bianchi S, Feccia M, Sgreccia F, et al. Limited thoracotomy as a second choice alternative to transvenous implant for cardiac resynchronisation therapy delivery. Eur Heart J. 2004;25(12):1063–9. https://doi.org/10.1016/j.ehj.2004.04.016.
Ma H, Wang X, Xie H, Sun C, Wen Z, Liu Y, et al. Characterization of the cardiac venous system in heart failure patients using 256-slice CT. Int J Cardiol. 2016;203:447–8. https://doi.org/10.1016/j.ijcard.2015.10.135.
Sommer A, Kronborg MB, Norgaard BL, Poulsen SH, Bouchelouche K, Bottcher M, et al. Multimodality imaging-guided left ventricular lead placement in cardiac resynchronization therapy: a randomized controlled trial. Eur J Heart Fail. 2016;18(11):1365–74. https://doi.org/10.1002/ejhf.530.
Alhailiy AB, Ekpo EU, Kench PL, Ryan EA, Brennan PC, McEntee M. The associated factors for radiation dose variation in cardiac CT angiography. Br J Radiol. 2019;92(1096):20180793. https://doi.org/10.1259/bjr.20180793.
Blomster JI, O'Rourke J, Choudhary P, Thiagalingam A, Kovoor P, Adler J, et al. Patient selection essential for computed tomography coronary angiography. Scand Cardiovasc J. 2016;50(4):206–12. https://doi.org/10.1080/14017431.2016.1177659.
Vorre MM, Abdulla J. Diagnostic accuracy and radiation dose of CT coronary angiography in atrial fibrillation: systematic review and meta-analysis. Radiology. 2013;267(2):376–86. https://doi.org/10.1148/radiol.13121224.
Kosmala A, Petritsch B, Weng AM, Bley TA, Gassenmaier T. Radiation dose of coronary CT angiography with a third-generation dual-source CT in a “real-world” patient population. Eur Radiol. 2018;29:4341–8. https://doi.org/10.1007/s00330-018-5856-6.
Stocker TJ, Deseive S, Leipsic J, Hadamitzky M, Chen MY, Rubinshtein R, et al. Reduction in radiation exposure in cardiovascular computed tomography imaging: results from the PROspective multicenter registry on radiaTion dose Estimates of cardiac CT angIOgraphy iN daily practice in 2017 (PROTECTION VI). Eur Heart J. 2018;39(41):3715–23. https://doi.org/10.1093/eurheartj/ehy546.
Menke J, Unterberg-Buchwald C, Staab W, Sohns JM, Seif Amir Hosseini A, Schwarz A. Head-to-head comparison of prospectively triggered vs retrospectively gated coronary computed tomography angiography: meta-analysis of diagnostic accuracy, image quality, and radiation dose. Am Heart J. 2013;165(2):154–63 e3. https://doi.org/10.1016/j.ahj.2012.10.026.
Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH. Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology. 2013;268(3):719–28. https://doi.org/10.1148/radiol.13122276.
Lee J, Cho JY, Lee HJ, Jeong YY, Kim CK, Park BK, et al. Contrast-induced nephropathy in patients undergoing intravenous contrast-enhanced computed tomography in Korea: a multi-institutional study in 101487 patients. Korean J Radiol. 2014;15(4):456–63. https://doi.org/10.3348/kjr.2014.15.4.456.
Jung JW, Choi YH, Park CM, Park HW, Cho SH, Kang HR. Outcomes of corticosteroid prophylaxis for hypersensitivity reactions to low osmolar contrast media in high-risk patients. Ann Allergy Asthma Immunol. 2016;117(3):304–9 e1. https://doi.org/10.1016/j.anai.2016.07.010.
Darlington M, Gueret P, Laissy JP, Pierucci AF, Maoulida H, Quelen C, et al. Cost-effectiveness of computed tomography coronary angiography versus conventional invasive coronary angiography. Eur J Health Econ. 2015;16(6):647–55. https://doi.org/10.1007/s10198-014-0616-2.
Igarashi A, Fujito K, Hirano M, Fukuda T. Cost minimization analysis of beta-blocker at the time of CT imaging for suspected of coronary heart disease in Japan. J Med Econ. 2014;17(2):142–7. https://doi.org/10.3111/13696998.2013.877021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac Computed Tomography
Rights and permissions
About this article
Cite this article
Kovoor, J.G., Thiagalingam, A. & Chow, C.K. Computed Tomography in Heart Failure. Curr Cardiovasc Imaging Rep 12, 36 (2019). https://doi.org/10.1007/s12410-019-9512-6
Published:
DOI: https://doi.org/10.1007/s12410-019-9512-6