Abstract
“Patient Specific” technology introduced in last 5 years, slowly gained popularity but has currently plateaued. We have a number of studies on patient specific instruments where they have been compared with conventional jigs in total knee arthroplasty and reported to have no clear additional benefits. This review discusses their intraoperative and postoperative advantages/disadvantages and cost effectiveness and provides a synopsis in light of current literature. Patient specific implants are not freely available yet, and there is no scientific literature reporting on their use in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patient specific instrumentation (PSI) was introduced as the means to obtain a customized implant fit; quickly and with greater accuracy with the added benefit of shorter rehabilitation and overall reduction in costs. PSI involves greater preoperative planning. Based on a preoperative CT scan or MRI as per the manufacturer’s protocol, along with other inputs from the surgeon, custom made disposable cutting blocks are manufactured by specific software programs. The surgeon can adjust the frontal and sagittal alignment and depth of the cuts on femoral and tibial sides preoperatively. The blocks, thus customized, are meant to fit accurately on the femoral and tibial surfaces and their fit is expected to achieve better alignment of the cuts, compared with conventional jigs.
In patient specific implant (PSIM) total knee arthroplasty (TKA), both the cutting jigs and the implant are specifically designed for the patient. The same preoperative imaging studies used for manufacturing jigs are used for manufacturing custom implants with the native femoral characteristics (intercondylar notch distance, the J curve, the condylar offset, the anteroposterior and mediolateral width), and the native tibial bone characteristics (size and coverage). PSIM TKA aims to restore the native knee anatomy and potentially normal knee kinematics. After Total hip arthroplasty the patient satisfaction is much higher than after TKA probably because of exact restoration of joint center of rotation with similar direction of movement of the joint as the native hip. The same cannot be said about TKA performed in the conventional manner. The idea behind PSIM TKA is to restore native joint line and native direction of movement of the joint.
The objective of this article is to review the current literature and present the performance of “patient specific” technology. There are a large number of studies on PSI TKA but none on PSIM TKA. We have detailed performance of PSI in comparison with conventional and navigated TKA with respect to:
-
(1)
Intraoperative advantages/disadvantages
-
(2)
Postoperative alignment
-
(3)
Postoperative rehabilitation
-
(4)
Final functional recovery
-
(5)
Cost effectiveness.
Intraoperative advantages/disadvantages
Length of incision
The size of the PSI jig is much smaller than the jigs for conventional TKA and it was expected that the incision length with PSI would be reduced. Noble et al [1] in their study noted such a decrease in skin incision length with PSI compared with conventional TKA (136 mm vs 151.8 mm P = 0.014), but none of the other studies have reported on this parameter. Moreover, studies comparing the length of incision with PSI against minimally invasive TKA using conventional jigs are required.
Intraoperative time
PSI jigs were introduced with the idea of decreasing the surgical time taken by eliminating certain steps: eg, opening of the medullary canal, clearing of soft tissues for fitting bigger jigs and referencing the cuts from external landmarks. Barett et al [2] compared 66 PSI TKAs, 86 conventional TKAs, and 88 Navigated TKAs for their tourniquet time and skin incision to skin closure time. They reported that the ‘skin to skin’ time in PSI TKAs was similar to conventional TKAs (74.6 vs 79.8 minutes, P = 0.073) and significantly less than navigated TKAs (74.6 vs 101.2 minutes, P < 0.001). Nunley et al [3] came to a similar conclusion of no significant difference in skin incision to closure time with PSI TKAs vs conventional TKAs (89.6 vs 93.4 minutes, P = 0.262). Stronach et al [4], in their study of 66 prospectively followed PSI TKAs and 62 retrospectively evaluated conventional TKAs, also reported no difference in the tourniquet time between these groups. Noble et al [4] reported a significantly reduced intraoperative time with PSI TKAs against conventional TKAs (121.4 vs 128.1 minutes, P = 0.048). Hamilton et al [5•], in their study of 26 PSI and 26 conventional TKAs measured the time duration for performing 15 surgical steps and total surgical time. They reported significantly more total surgical time in the PSI group compared with conventional group (61.47 minutes vs 57.27 minutes, P = 0.006). This was attributed to intraoperative changes in plan needed for balancing issues. Yoon et al [6] also observed longer intraoperative time with PSI (n = 42) compared with conventional (n = 48) TKAs in his prospective randomized study (59.4 minutes vs 46.6 minutes, P < 0.001). They attributed this longer time with PSI jigs to cross checking of cuts suggested by PSI with conventional methods.
Overall, current literature suggests that intraoperative surgical time for PSI and conventional TKA is similar. However, as experience with PSI jigs improves, there could be further reduction in operative time. Studies done from centers where PSI jigs are routinely used will be helpful to draw conclusions.
Number of trays opened during the surgery
As the number of surgical steps is less with PSI compared with conventional TKR, it was expected that less number of operative trays would have to be opened during surgery, saving on theatre time, sterilization time, and personnel cost. Noble et al [1] found significant reduction in the number of trays used in PSI TKR compared with conventional TKR (4.3 vs 7.5; P < 0.0001). Hamilton et al [5•] also found a decrease in the number of trays used with PSI TKR compared with conventional TKR (2.5 vs 7.3; P < 0.001). PSI TKR decreases the number of trays used for surgery, if all goes as per plan.
Fitting of jigs
Proper fitting of jigs intraoperatively is a necessity for a proper cut. Lustig et al [7] (45 patients) and Spencer et al [8] (15 patients) reported good fitting in all patients, whereas Bali et al [9] et al in their study in 66 consecutive knees found that 8 (12.1 %) femoral and 3 (4.5 %) tibial jigs did not fit properly.
Fitting depends on the kind of preoperative imaging study done (CT scan vs MRI), the software used, the image acquisition process, interpretation of the images for jig manufacturing and the time lag between the imaging study and the surgery. CT scan images do not visualize the articular cartilage thickness and, hence, may be inferior to MRI for manufacturing these jigs although there are no studies to prove or disprove the same. The image acquisition process and the manufacturing process are now standardized for all companies and fitting of the jig is not a major issue currently.
Change in planned size
The sizing of implant in PSI TKR is based on the bony size calculated from images obtained, but a mismatch between this size and that measured during surgery has been observed in many studies. Balancing issues may also necessitate a change in size intraoperatively. Vundelinckx et al [10•] in a comparison of 31 PSI and 31 conventional TKR found a change in the femoral and tibial size in 19.4 % of cases, whereas a change in liner was required in 9.7 % of the cases. Lustig et al [7] in his study of 45 PSI TKAs observed a change in the tibial size in 50 % of cases whereas a change in the femoral size was observed in 48 % of cases. In contrast, Spencer et al [8] in their study of 19 TKAs found no change required in the size of femoral or tibial implant. Stronach et al [4] observed 74 component size changes in 66 consecutive PSI TKA.
We think that despite the improvement in technology and the surgeon experience, balancing issues, especially in cases with deformity, may warrant a change in planned size. If this happens during PSIM TKA surgery than the surgeon will be left with no choice but to use off the shelf implants. So, additional custom implants, 1 size above and below should be available to the surgeon intraoperatively, significantly pushing up the fabrication cost.
Recuts
Recuts may be required for alignment changes, sizing issues, or for balancing issues. Hamilton et al [5•], in their study reported 27 bony recuts, more on femoral side in their series of PSI TKAs compared with 11 bony recuts in conventional TKAs. The greater number of PSI recuts were required for gap balancing and correction of rotation. Hamilton came to the conclusion that lack of familiarity with the blocks and fear of over-resection caused the engineers and surgeon to plan for a distal femoral cut that was not thick enough necessitating recuts. Stronach et al [4] also reported an average of 2.4 changes in plan per surgery with PSI TKR. 166 intraoperative changes were required in 66 consecutive cases (including 74 component size changes and 21 alignment changes). 81 % of these recuts were considered an improvement in alignment from that suggested by the PSI jigs, as judged on postoperative radiographs.
Recuts necessitate opening of conventional TKR instrument sets leading to increased operative time and they also lead to an increase in the cost of surgery.
The number of recuts required with PSI should become less as the surgeon experience improves, but cases having severe deformity and where surgeon is expecting more than mild soft tissue releases should probably be operated with conventional or navigated total knee arthroplasty.
The current literature does not favor any intraoperative advantage of PSI jigs over conventional technique except perhaps in reducing the number of trays used and that too, only when all goes as per plan. In fact, there are potential disadvantages of ill-fitting jigs and increased number of recuts required with PSI jigs.
Postoperative alignment
PSI jigs were introduced for better or similar restoration of the mechanical/kinematic axis and individual component alignment compared with conventional jigs. As the alignment of cuts with PSI is independent of external landmarks to align the jigs, it was supposed to better restore the planned axis. Noble et al [1] in a prospective randomized study of 15 PSI and 14 conventional TKA reported significantly better mechanical axis restoration with PSI (1.7° vs 2.8°, respectively; P = 0.03). Ng et al [11] in a retrospective comparison of 569 PSI and 155 conventional TKR found lesser number of outliers with PSI (9 % vs 22 %, respectively; P = 0.018). However, there were similar numbers of outliers when the individual components were evaluated independently. There was no difference in individual tibial (10 % PSI vs 7 % conventional; P = 0.21) and femoral component (22 % PSI vs 18 % conventional; P = 0.14) alignment between the 2 groups. Hamilton et al [5•] in a prospective randomized study comparing 26 PSI and 26 conventional TKA found no difference in component alignment between the groups except for increased tibial slope in the conventional group. Barret et al [2] in a comparison of 66 PSI and 86 conventional and 81 navigated knees (the PSI group was prospective and the other groups were retrospective) found no difference in component alignment and mechanical axis restoration between the 3 groups. Nunley et al [3] in a retrospective comparison of 57 PSI and 57 conventional TKA found no difference in component alignment and mechanical axis restoration between the groups. Yoon et al [6] in a prospective randomized study of 42 PSI TKA and 48 conventional TKA found no difference in the number of outliers with regards to mechanical axis restoration (12 % vs 10 %, respectively; P = 0.542) or with regards to individual component alignment in the sagittal, coronal, and axial plane. Victor et al [12••] in a randomized controlled trial of 128 patients did not find any difference in the number of outliers between the PSI and conventional groups in the overall coronal alignment (25 % vs 28 %, respectively; P = 0.69), femoral component coronal (7 % vs 14 %, respectively; P = 0.24), and axial alignment (23 % vs17%, respectively; P = 0.50). However, they reported the tibial component coronal (15 % vs 3 %; P = 0.03) and sagittal alignment (21 % vs 3 %, respectively; P = 0.002) as worse in the PSI group compared with the conventional group. Barrack et al [13] in a prospective randomized study of the comparison of 100 PSI and 100 conventional TKA did not find any difference in the number of outliers with regards to mechanical axis restoration between the 2 groups (31/100 vs 23/100, respectively; P = 0.203).
The current literature supports similar restoration of alignment with PSI as conventional TKA, but does not support any better alignment than conventional TKA. There are no prospective randomized studies on the direct comparison of alignment restoration with PSI against navigation.
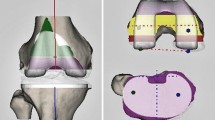
We have personally noted better rotational alignment of the femoral component with PSI TKA (Fig. 1, A and B) in comparison with navigated TKA on postoperative CT scan, but our numbers are small and no statistical evaluation was done to draw a definitive conclusion. The one advantage of PSI TKA over conventional and navigated TKA is the ability to align the prosthesis according to the kinematic axis. The principles of placing components according to the kinematic axis differ from mechanical axis as the primary aim is not to align the femoral component according to the hip-knee-ankle axis but to align the transverse axis of the best fitting femoral component with the primary transverse axis of the femur, about which the tibia flexes and extends. The tibial component is then placed with its longitudinal axis perpendicular to the femoral transverse axis. It has been shown in a few studies that restoring the kinematic alignment does not lead to malposition of the components as judged by the mechanical axis [14, 15]. The ligament length, mobility, and stability in a kinematically aligned knee are restored by the removal of osteophytes, adjusting the plane of the tibial cut, releasing the posterior capsule from the femur, and medializing or lateralizing the tibial component. The perceived clinical benefits of aligning the knee to the kinematic axis are better range of motion, less stiffness, less instability, and a painless fast postoperative recovery. Howell et al [16] in a prospective study of 198 patients(214 knees) with PSI TKAs reported restoration of kinematic alignment with no failure and high function at a mean of 38 months in spite of 75 % of their patients having tibial alignment categorized as varus outliers. Studies on the comparison of longevity and clinical function achieved by aligning the implant according to the mechanical vs kinematic axis are required and if they go in favor of the kinematic axis it could become a game changer in favor of PSI/PSIM TKA.
Postoperative rehabilitation
Duration of hospital stay and blood loss
It was believed at the time of introduction of PSI that a shortened surgery with smaller incision and better alignment would mean faster postoperative rehabilitation and less blood loss. Vundelinckx et al [10•] in a prospective randomized study of 31 PSI and 31 conventional TKR found no difference in hospital stay (6.68 days vs 6.06 days, respectively), or blood loss between the 2 groups. In contrast, Noble et al [1] in a prospective randomized study of 15 PSI and 14 conventional TKAs found significantly decreased duration of hospital stay in the PSI group (59.2 hours vs 66.9 hours; P = 0.043) but observed no difference in blood loss (71 mL for PSI vs 62.5 mL for conventional; P = 0.395). Stronach et al [4] in a comparison of 66 prospectively followed PSI TKA and 62 retrospectively evaluated conventional TKA and found no difference in blood loss (114.2 mL vs 107.9 mL). Yoon et al [6] in a prospective randomized study of 42 PSI and 48 conventional TKAs did not observe any difference in blood loss between the groups (783.7 mL vs 843.8 mL, respectively).
So, the current literature suggests similar blood loss with PSI as with conventional TKA and is equivocal on the duration of hospital stay. There are no studies on the amount of blood loss or duration of hospital stay with PSIM TKA although no major difference in comparison to PSI TKA is expected.
Final functional recovery
Vundelinckx et al [10•], in a prospective randomized study comparing 31 PSI and 31 Conventional TKAs, measured pain on the Visual Analogue Scale (VAS), Knee injury and Osteoarthritis Outcome Score (KOOS), Lysholm Score, and Range of Motion as the parameters of postoperative functional recovery. There was no difference observed in all 4 parameters between the 2 groups. None of the other studies have reported on the functional recovery and more studies are required to draw a conclusion on this count.
There are no studies comparing the final functional recovery achieved with PSIM in comparison to conventional implants and only time will tell whether PSIM would decrease the number of dissatisfied patients by achieving a closer to native knee anatomy and natural knee kinematics.
Cost effectiveness
The 1 contention given in favor of patient specific implants inserted with patient specific jigs is a reduction in overall cost due to a decrease in number of trays, smaller turnover time, decreased number of personnel employed, and the decrease in cost of maintenance of inventory of both instruments and implants. Slover et al [17••] did a cost benefit analysis of the use of PSI by the Markov model and he came to the conclusion that the high preoperative costs of imaging and manufacturing PSI jigs can only be offset by significantly reduced revision rates, when compared with conventional TKAs. This appeared hard to achieve but this cost analysis did not take into account the savings caused by decrease in number of trays, smaller turnover time, decreased number of personnel, and shorter hospital stay. Watters et al [18] in a prospective study of 12 conventional, 12 PSI, and 12 navigated TKA found savings of $391 per case with PSI TKA in comparison to conventional TKA ($290 for processing fewer trays and $101.01 for 13 minutes shorter operative time). However, the cost of imaging was not considered in this study. Barrack et al [13] in a comparison of 5 consecutive cases of PSI TKA and 5 conventional TKA found an additional average cost of $1475 for jig manufacturing (including cost of MRI and cost of fabrication of jigs) with an average savings of $322.23 with PSI TKA due to shorter operative time and lesser cost of sterile processing time of trays. All postoperative alignment parameters in his complete study of 100 PSI TKAs vs 100 conventional TKAs did not show any difference between the 2 groups, so he concluded that PSI jigs do not add financial value to the surgery.
Many of the advantages of PSI jigs expected to decrease the cost of surgery as shorter operative time and decreased numbers of personnel are perceived advantages and not proven advantages. In addition, these costs vary from one hospital to the other; thus, individual hospitals would have to do their own cost benefit analysis to come to a conclusion regarding savings in the operation theatre. Even if there is a significant saving in the operation theatre costs, it is definitely not going to offset the preoperative costs of imaging and fabrication of these jigs. Only a significant reduction in revision rates can turn around the balance and make these jigs cost effective. Conventional teaching tells us that alignment from 2.4° of varus to 7.2° of valgus is required for longer life of the implant but a recent study with a 15-year follow-up of 650 arthroplasties showed longer survival of implants outside this range. Even if PSI is able to give us improved alignment, whether it will lead to a decrease in the revision rate is not known and, hence, the cost effectiveness of PSI is extremely difficult to reach.
Conclusions
PSI was introduced for a faster, more accurate, and cost-effective surgery but none of these benefits have been realized so far. A definite reduction in number of trays required during surgery has been reported, if all goes as per plan. However, a frequent change in plan is reported in many studies, which offset the benefit of fewer trays required. It is likely that increased experience with PSI may result in fewer changes in plan, but the need to change plan can never be completely eliminated. Second, with PSI surgical duration may be reduced but this is counterbalanced by the lengthy preoperative planning and uploading of data required by the surgeon. Third, the high costs of imaging studies and manufacturing jigs in PSI reduce their cost-effectiveness. Last, the results with PSI are similar to conventional TKA in terms of mechanical axis alignment.
It must be noted that PSI/PSIM has the unique ability to align implants to the patient’s kinematic axis accurately; which is not possible with conventional or navigated TKA. The role of implant alignment to the patient’s kinematic axis is under fresh review. So, whether this special feature of “Patient Specific” technology becomes crucial to the long-term survival of implants remain to be seen.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Noble WJ, Moore CA, Ning L. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27:153–6.
Barrett W, Hoeffel D, Dalury D, Bohannon Mason J., Murphy J, Himden S. In-vivo alignment comparing patient specific instrumentation with both conventional and computer assisted surgery (CAS) instrumentation in total knee arthroplasty. J Arthroplasty. 2013. Available at: doi: 10.1016/j.arth.2013.06.029.
Nunley RM, Ellison BS, Ruh EL, Williams BM, Foreman K, Ford AD, et al. Are patient-specific cutting blocks cost-effective for total knee arthroplasty? Clin Orthop Relat Res. 2012;470:889–94.
Stronach BM, Pelt CE, Erickson J, Peters CL. Patient-specific total knee arthroplasty required frequent surgeon-directed changes. Clin Orthop Relat Res. 2013;471:169–74.
Hamilton GW, Parks NL, Saxena A. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty. 2013;28(96). A prospective randomized study (level 1 study) of the comparison of 26 PSI and 26 conventional TKA; where the time period of 15 surgical steps was compared between the groups. This comparison of time, required for surgical steps, is the most detailed of all the studies.
Roh YW, Kim TW, Lee S, Seong SC, Lee MC. Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of 1 system. Clin Orthop Relat Res. 2013;471:3988–95.
Lustig S, Scholes CJ, Oussedik SI, Kinzel V, Coolican MRJ, Parker DA. Unsatisfactory accuracy as determined by computer navigation of Visionaire patient-specific instrumentation for total knee arthroplasty. J Arthroplasty. 2013;28:469–73.
Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intraoperative events and long leg coronal alignment. Int Orthop. 2009;33:1571–5.
Bali K, Walker P, Bruce W. Custom-fit total knee arthroplasty: our initial experience in 32 knees. J Arthroplasty. 2012;27:1149–54.
Vundelinckx BJ, Bruckers L, Mulder KD, Schepper JD, Van Esbroeck G. Functional and radiographic short-term outcome evaluation of the Visionaire system, a patient-matched instrumentation system for total knee arthroplasty. J Arthroplasty. 2013;28:964–70. This is the only study comparing the postoperative functional recovery of PSI TKA with conventional TKA.
Ng VY, DeClaire JH, Berend KR, et al. Improved accuracy of alignment with patient specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99.
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res. 2013;472:263–71. This is the only study reporting that individual femoral and tibial component alignment was worse with PSI compared with conventional TKA.
Barrack RL, Ruh EL, Williams BM, Ford AD, Foreman K, Nunley RM. Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94-B(Suppl A):95–9.
Nogler M, Hozack W, Collopy D, Mayr E, Deirmengian G, Sekyra K. Alignment for total knee replacement: a comparison of kinematic axis vs mechanical axis techniques. A cadaver study. Int Orthop. 2012;36:2249–53.
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically vs mechanically aligned total knee arthroplasty. Orthopedics. 2012;35:e160–9.
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471:1000–7.
Slover JD, Rubash HE, Malchau H, et al. Cost-effectiveness analysis of custom total knee cutting blocks. J Arthroplasty. 2012;27:180. This is the most important study for cost benefit analysis of PSI TKA.
Watters TS, Mather III RC, Browne JA, Berend KR, Lombardi Jr AV, Bolognesi MP. Analysis of procedure-related costs and proposed benefits of using patient specific approach in total knee arthroplasty. J Surg Orthop Adv. 2011;20:112–6.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Rajesh N. Maniar has been a consultant for DePuy Orthopedics, India. Tushar Singhi declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maniar, R.N., Singhi, T. Patient specific implants: scope for the future. Curr Rev Musculoskelet Med 7, 125–130 (2014). https://doi.org/10.1007/s12178-014-9214-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-014-9214-2