Abstract
Patient-Specific Instruments have revolutionized the way of approaching an orthopedic intervention. They progressively invaded the operative rooms from the 2010s to assist the surgeons during total knee arthroplasties. Nevertheless, they have been invented much earlier in the middle of 1990s for rare applications. Their manufacturing has evolved deeply. From subtracting milling at its beginning, instruments are now manufactured by material addition. This chapter reminds the history of patient-specific instruments, the manufacturing evolution, and their slow acceptation by the medical field. Instruments for knee arthroplasty will be described, as well as the report on the controversy about their claimed accuracy and usefulness. Finally, innovative applications will be exposed showing the high potential Patient-Specific Instruments can bring.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Personalized medicine is today a reality. Patient-specific drug treatments based on genetics analysis are now available permitting significant improvements in treatment efficacy. The arrival of computers in medicine has opened new possibilities producing a tremendous step forward in radiology and, as a direct consequence, in surgery. Orthopedics was a pioneer in the field benefiting from the higher resolution images and the ease to extract bone contours from a standard computed tomography acquisition. Computerized assistances were then developed to perform preoperative planning, bringing the possibility of analyzing pathologies in three-dimensions. The understanding of the bone shape or its deformation has permitted to anticipate bone cuttings to restore a normal anatomy.
The transfer toward the operative room has also benefitted from computers. Robots and navigations systems have been put on the market to reliably reproduce the planning, making surgery safer and more accurate. In the recent years, new intra-operative assistances have arose with a strong trend toward simplification.
This chapter will introduce the concept of Patient-Specific Instruments (PSI) and the recent advances in their surgical applications. Firstly, the history of PSI will be detailed, from their invention in Aachen, to these days. Secondly, we will approach knee arthroplasty which is today the main use of PSI. Finally, recent and innovative applications will be presented to understand the potential they bring in the operative room.
PSI History
The general belief is that PSI have been created only few years ago by implant manufacturers to provide cutting jigs for knee arthroplasty. Personalization of orthopedic surgical treatments arose much earlier in the middle of the 90s. This belief is certainly due to their slow acceptation that made them a minor evolution. Indeed, at this period, robotics and optical navigation systems were considered the future of computer assistances for orthopedic surgeries. The claimed accuracy was highly promising, new sensors were appearing and several clinical applications were investigated. The community of scientists and surgeons was very enthusiastic in developing these new intelligent systems. Some improvements were still required to widely spread the technology. The main concern was related to the intra-operative time dedicated to the assistances. The computation power and display devices available at this moment were sufficient to achieve their objectives, but not as efficiently as desired. Other minor concerns were the size of the machines in the operative room, the important additional costs and the relative low ergonomics of the systems which required complex interactions with computerized systems. The technology was highly dependent of the expected increase in computation power and miniaturization.
Based on these considerations, a team of researchers (Radermacher, Rau, Staudte, et al.) at Helmholtz Institute for Biomedical Engineering (Aachen University, Germany) has developed an alternative to fully computerized systems. They proposed a “relatively simple, low cost solution that facilitates exact safe and fast implementation of planned surgery on bone structures, eliminates the need for continual radiographic monitoring and avoids overburdening surgery with complex equipment and time consuming procedures” [29]. By molding the shape of the target bone structure into a generic template, they have created “Individual Templates”, that are today known as Patient-Specific Instruments. The bone-specific surface provided a mean to find the physical correspondence between a pre-operative 3D bone model and the actual bone structure in the operative room. The spatial correspondence was physically embedded into the template during the manufacturing stage instead of creating it in the operating room. The positioning was straightforward and did not require a matching of bony structures nor time-consuming computations. They have described the whole process from image processing to the sterilization for the first time in 1994 in a conference paper [31]. Cervical spine decompression and triple pelvic osteotomies were the first proposed clinical applications, followed by pedicle screw placement and total knee arthroplasty few years later [29].
The manufacturing process of the individual templates was fast and quite easy. First, a Computerized Tomography (CT) was used to extract the shape of bone structures and create a 3D reconstruction. Then, a pre-operative planning was performed to virtually execute the surgery using a dedicated software installed on a DISOS workstation [28]. The instruments were manufactured by subtractive manufacturing using a desktop milling machine. Milling technique was preferred to additive manufacturing because the latter was much expensive at the moment (3000 euros for a bone model) [24]. The instrument was sterilized by standard autoclave at 135 °C. According to the authors, less than 1 h was needed from the data transmission to the use of PSI in the operative room. This delay seems optimistic since the sterilization process itself lasts more than 1 h (30 min for automatic washing, 1 h for manual wrapping and steam sterilization).
In the operative room, the PSI were combined with additional hardware to achieve specific tasks. They were equipped with interfaces to adapt a handle that allows an easy manipulation. Some drill guides or conventional osteotomy guides could be inserted and bone pins could be used to rigidly fix the PSI on the bony structure. They also acted as an interface between the bone and the usual standard template.
The PSI have been widely tested by the Aachen team to assess their accuracy and impact on time during the surgery. The early reported results on accuracy of PSI applied on bone replicas were encouraging. Positioning measurements have shown an angulation error below 0.6° in the spine and the tibia and 1° in the femur [30]. Converting angles into distance, the error was found below 1 mm on tibia and spine, while a maximum of 1.6 mm error was found for a femoral head drilling. Cadaveric experiments have been led and showed clinically acceptable results in spine [35] with a few number of errors above 2 mm when compared to the conventional method. It should be noted that a software failure has caused important errors. It emphasizes that computer assistances are subject to software computations and can lead to severe errors.
In matter of time, studies have shown a shorter duration of the surgery in two different applications. A cadaveric experimentation has demonstrated that PSI decreased the time to find the entry point of the drilling in a vertebra pedicle [35]. For triple pelvic osteotomies on actual patients, the whole surgery time has been decreased by 23 % to gain 35 min [36]. This improvement is easily understandable by the “plug and play” characteristic of the instrument. The user places the instrument in the correct position and connects standard devices to achieve the desired task. The decrease of intra-operative irradiation thanks to a lesser use of fluoroscopy is also an added-value of the technology. It has been shown that it is significantly decreased when using PSI [4]. The clinical impact has also been reported, but conclusions are less clear because of rare clinical cases that makes the production of comparative data difficult.
Surprisingly, although all their positive aspects, PSIs have disappeared quite rapidly. The main reason is that PSI technology seemed to be very demanding, with the need for having a specific workstation with specific software, a skilled technician and the milling machine. This kind of machine was mainly dedicated to the industry and was rarely user friendly to be used by a newbie. The conceivers claimed that a surgeon can use the system within few minutes to create a patient specific instrument. Some stages still required the presence of a technician to be present to perform the pre-operative planning, design the instrument and set up the machine.
In the meantime, navigation systems have become the standard option for computerized assistances in many applications (knee, hip and shoulder arthroplasties, spine instrumentation, ilio-sacral screw placement). Navigation being intensively pushed by the implant manufacturers, strong innovations such as bone morphing has been developed, contributing to its promotion. It has appeared to be more flexible and stand alone with the ability to plan the surgery on the machine that will be used during the surgery. Early clinical results were enforcing these considerations with an excellent accuracy for several joint arthroplasties.
PSI for TKA
During several years, navigation systems, provided by specific manufacturers (praxim, brainlab, Amplitude, Medtronic, stryker,…) was used to perform knee, hip and shoulder arthroplasties. These companies provided surgeons with virtual 3D models of the implants to adapt the pre-operative planning to the intended implant. With the success of navigation systems, implant manufacturers have developed their own solutions. Progressively, implant manufacturers have put on the market navigation systems to place their own implants. The announced accuracy of these systems made it a gold standard spreading the technology around the world.
However, controversy has arose progressively on the actual added value for the patient. Some clinical papers were discussing on the supposed benefits relative to the involved costs in terms of investment and consumables. Furthermore, the global accuracy of such system had reached a plateau at approximately 1 mm. This incompressible residual error found its source in the camera resolution and in the matching process. Other drawback of the method was the time to create the link between the patient and its preoperative images. The acquisition process of points was time consuming and could even fail leading to long wasted minutes to set-up the system. Finally, as described by the Aachen Team, the size of the machine and screen interactions could be painful for the user and the team.
Based on these considerations, in the middle of the 2000s, PSI for total knee arthroplasty have been reworked. Advances in the additive manufacturing technology have brought an alternative to milling manufacturing. This emerging technology, also called rapid prototyping and more widely known as 3D printing, was continuously improved. Its resolution and accuracy were by far sufficient to be used in a surgical context as well as new biocompatible and sterilizable materials were developed. The technology being more popular, its cost decreased largely making it an affordable solution.
In 2006, the first paper about the technique and the feasibility was published [17]. The authors reported the principle of the required planning and their first use of “patient-specific templating” on cadavers and plastic bones. They also reported a short cost-efficacy study. The feasibility of surgery using PSI has been assessed on 45 plastic and cadaver knees. The different components of this technique (planning, material, 3D machine) have been found suitable to carry out the required tasks. Their findings about accuracy were encouraging since a low error was shown. The maximum error was 2.3° for rotations and 1.1 mm for translations. There are some limitations on these accuracy measurements since they are partially reported (no sagittal alignment for the femur, translations are not well described) and also were not systematic (only 6 postoperative CTscan, randomly selected). The intra-operative time has been decreased when compared to the conventional method, but significance was not mentioned. The cost analysis has concluded that the PSI were not as costly as standard templates. However, in their analysis, the authors have taken into account the manufacturing cost of the standard instruments, a cost that is supported by the implant manufacturer. Furthermore, the sterilization costs of conventional instrumentation seem overestimated while the production costs for PSI were astonishingly low (200$) and the cost for the specific software was not mentioned. Despite these limitations, this first experimental paper has definitely raised a new field for knee arthroplasties.
The concept was relatively simple. CT or MRI data were transferred to the company by using a secured server on sending a CD-ROM. The preoperative planning consisted in determining the optimal positioning of the implant with respect to the bony specificity. The planning started with landmarks acquisition by an operator who was responsible for finding the correct anatomical point that will construct a local reference coordinate system. Once the referential determined, the implant size and position were chosen, defining de facto the cutting trajectories. The result was sent back to the surgeon who was usually provided with an interface (web, file, in 2D or false 3D) to verify the conformance of the planned surgery with the patient’s needs. Some distance and angle measurements were also provided. The surgeon had the possibility to accept or reject the pre-operative planning. In case rejection, the planning was adapted by the operator. Once approved, the 3D planning was validated, standard templates were individualized with patient’s bone surfaces embedding flat surfaces or slots to perform cuttings, alternatively drilling guides to position a standard ancillary. The instruments were manufactured by Selective Laser Sintering as follow. A laser draws a 2D shape on top of a polyamide powder container. The polyamide is instantaneously melted under the action of high energy provided by the laser. A hardened 2D shape is then obtained. A thin layer of powder is then sprayed on top of the container, over the 2D shape. The laser draws a new 2D shape that melts the free powder to the previous layer. The process is repeated layer by layer until the 3D model is completed. After intensive free powder cleaning, the instruments were packed, labelled and sent to the surgeon’s institution to be sterilized by standard steam autoclave before entering into the intra-operating room.
Two different approaches have been implemented for the preoperative planning: CT- or MRI-based. CTscan is usually preferred because of its availability in most institutions and a presumed higher resolution for bony landmarks. The main drawback of CTscan is the radiation exposure that may cause radio-inducted cancers. On the other hand, MRI represents a safer modality providing an excellent image of cartilage that may be used as contact surface for the PSI. In terms of costs, the CTscan compares favorably to the MRI. Accuracy of both philosophies have been investigated by several authors [33, 39, 42] yielding to diverging conclusions.
White et al. have extracted bone structures from MRI and CTscan and manufactured replicas using Selective Laser Sintering. They have compared measures taken from the replicas and the actual bone. Obtained data are highly surprising with deviation up to 11 mm between the MRI model and the actual bone. These impressive errors should result from an improper segmentation of the MRI since manual editing and several semi-automated segmentations were required to extract the bone contours. Conclusions drawn from this experiment may not be representative of the reality.
Rathnayaka et al. and Van den Broeck et al. compared virtual bone models derived from CTscan and MRI with a model considered as gold standard. Rathnayaka et al. have acquired their gold standard by a mechanical contact scanner. Van den Broeck et al. have generated their reference by a high resolution optical scanner. They have matched MRI and CTscan models to the reference and computed the average distance between both models. Both studies have shown non-significant differences between MRI and CT concluding that both modalities were equivalent in terms of accuracy. Rathnayaka et al. have investigated the accuracy on 5 different target zones. Interestingly, MRI has produced a significantly higher error on the distal extremity of bone, zone of interest for patient-specific instruments. According to these latter two studies, both modalities can safely be used to create patient-specific instruments provided that the segmentation method is accurate and reproducible.
Once the feasibility established, implant manufacturers have implemented the technology and proposed PSI associated to their implant. OtisMed Corporation (later bought by Stryker) was the first to commercialize the technology in 2008. First published results seemed very poor with a wide range of obtained angles on the femur as well as on the tibia [21]. However, the reported figures were measured against the mechanical axis while the concept of the OtisMed prosthesis and associated instruments was to restore the initial anatomy rather than a neutral alignment. Thus, this study does not report actually accuracy error of the instruments, since the target angles were unknown.
This paper has been criticized in a letter to the editor [40] invoking that one author of this study was involved in a pre-commercial evaluation led by OtisMed. They also report that they have pursued their experience in using the OtisMed PSI, treating 650 patients within the next 14 months. Without providing any figures, authors conclude that this system is much more reliable and accurate that Klatt et al. has reported. The letter to the editor has been followed by a ‘In Reply’ [19] that was more a personal clarification than a scientific criticize. A second published paper has reported 48 patients treated by using PSI showing encouraging results [18]. A satisfying accuracy was obtained in most cases except 3 % where instruments did not fit perfectly to the bony structure. It has been established that the error found its source into the preoperative planning that was inaccurately executed by the technical operator. A last paper in the early life of PSI was published in 2008 [22]. After an initial cadaveric experiment, authors reported an interesting experience using PSI to guide pins that will align the standard cutting block. The accuracy was reported to be within 2.3°, but there was any explanation about which angle has been measured nor about the methodology. This incomplete analysis of accuracy demonstrates the lack of standardization in the postoperative assessment of accuracy.
In the few years following 2008, PSI has become a real trend to quickly replace the navigation system. The main advantage is that the investment is minimal for the hospital (no heavy investment to acquire the machine) and the learning curve is very short (intuitive usage). The accuracy of the manufacturing was very good since the resolution was 0.2 mm, a way lower than the resolution of optical navigation systems.
The year 2012 has seen several published studies to assess PSI accuracy for knee arthroplasty. A meta-analysis summarizing this specific literature [37] has concluded that PSI may improve accuracy of implant positioning even if the quality of obtained data are inconsistent. Furthermore, the clinical aspect was not observed at this time, basing the judgment on the fact that an implant accurately positioned implied a satisfying clinical outcome.
This conclusion has then been revised by several studies showing that PSI were not necessarily improving implant positioning [1, 25]. These studies were among the first to negatively conclude on PSI. Authors have compared groups of patients treated using either the conventional technique or the PSI. The postoperative measurements have shown more outliers in the PSI group than in the conventional group. A more recent meta-analysis [38] has shown that alignment over several reference planes were not improved using PSI. The authors conclude that the system is of no clinical benefit for the patient.
Recently, a new turn has been observed. The French chapter of CAOS international has had a conference where the usage of PSI has been discussed. Interesting questions have been raised leading to a new trend. First of all, it has been emphasized that the preoperative planning must be strictly supervised by the surgeon. The preoperative planning is crucial in the success of implant positioning by using PSI. The operator who is virtually positioning the implant obeys to a systematic procedure. The accuracy, repeatability and reproducibility of the method is questionable as sensitivity analysis tends to demonstrate. The planning designer must provide the surgeon with efficient tools to visualize the acquisition of reference axes. Doing so, the surgeon is able to check if point acquisition reflects the reality of the involved bones. Also, implant positioning must be controlled by the surgeon himself to ensure there will be no unsatisfying result such as anterior femoral step or undesired tibial slope. In the current days, the planning is largely underestimated, leading to potential misconception that are not related PSI accuracy.
Secondly, the instrument design has been criticized. It has been observed that instrument could reach several positions on the bony surface because of primary instability. Instrument could also slip from the target surface because of poor intrinsic in-place locking. Finally, mechanical constraints during K-wires or pins insertion can cause an instrument movement. These potential pitfalls can explain the unsufficient accuracy results described in the literature.
Surgeons should keep in mind that the overall system requires a high attention at all stages, from the images acquisition to the intra-operative use. If one link is weak, the resulting accuracy may be strongly affected. Even if these requirements are met, evidence of any clinical added value for the patient must still be proven.
Current Innovative Applications
PSI for knee arthroplasty has favored the growing popularity of additive manufacturing and made it affordable for medical use. The resurgence of PSI has bring back all the advantages described by Radermacher et al. But many others were also gained: production costs were decreased, resolution was improved and manufacturing process was located into certified medical facilities. This new picture of the market has permitted the development of numerous applications to treat complex bone pathologies or correct skeletal abnormalities.
Spine Instrumentation
Scoliosis correction is a challenging surgery requiring a high accuracy in inserting screws into pedicles that can be narrow and deformed. It is the reason why spine instrumentation has benefitted from the latest innovations such as navigation systems and, lastly, PSI. The latter has known extensive developments to reach clinical usage in early 2009 [23, 43]. It has shown excellent results with a significantly decreased pedicle perforation rate. Since then, research projects have been launched to further develop the concept, improving the design of instruments, leading to an increased stability [15]. Surprisingly, commercial applications are not widely available.
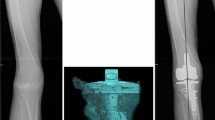
Degenerative spine correction is a similar application where the deformation can be first corrected by performing a bone resection and fixing the spine in an anatomical position. A specific planning determines the optimal positioning of the spine while preserving the spinal cord. A PSI is then manufactured to guide the saw blade during osteotomies. The PSI can either be molded onto the bone model using medical acrylic (Fig. 13.1) or virtually design and manufactured by additive manufacturing.
Joint Arthroplasties
Several joint arthroplasties are now benefitting from PSI to be planned and positioned. Several research projects have led to commercial products. For the shoulder arthroplasty, Imascap (Brest, France) has developed a software to give the surgeon the ability to perform its virtual pre-operative planning. This software is now proposed by Tornier (Montbonnot Saint-Martin, France) as the Blueprint® solution. Imascap has also developed and brought onto the market a PSI to transfer the planning into the operative room.
Hip prosthesis is also benefitting from PSI to increase accuracy of implant positioning. Several research projects are validating the concept [20, 34, 43]. Increased accuracy has been proven when using the PSI, showing that the technology may be useful in a clinical situation. However, there is no commercial application to date even if a patent has been registered in 2013 and a clinical study launched in the next few months.
The situation is more advanced for ankle arthroplasty were developments have been validated and transferred to a commercial product. Wright Medical has put on the market the Prophecy® Inbone® to position their prosthesis. Berlet et al. [3] have observed a high repeatability in positioning the instrument, leading to a final implant positioning within ± 3° when compared to the planned position. However, the solution is not an actual positioning instrument and clinical data are not available yet.
Bone Tumor Surgery
In tumor surgery, surgical excision must be highly accurate to ensure the total removal of the pathologic tissue without infraction of the tumor. Other way, a local recurrence of the tumor can arise leading to a failure of the initial treatment. The conventional method has shown unsufficient clinical results with a local recurrence rate observed in 28–35 % in case of pelvic tumors [9]. These clinical results have been confirmed by in vitro experiments leading to intralesional resections on plastic pelves [5, 6]. Preoperative assistances have been developed to plan the tumor removal. Tumor extension is delineated on the MRI and merged with the CTscan to combine anatomical and functional data. Based on the generated 3D view, cutting trajectories are chosen including a user-defined safe Margin (Fig. 13.2) [26]. When needed, a reconstruction strategy can be planned as well, using either a frozen allograft [27] or a commercial implant. The transfer into the operating theater was made possible by using a customized optical navigation system. The overall accuracy of the process has been assessed on plastic pelves [5]. A significant improvement has been shown with a reduced error during bone cuttings from 11.2 mm down to 2.8 mm (p < 0.001). The system has been used to surgically treat a small number of patients [14]. The technique has been more widely described by Docquier et al. the creators of the overall system [13].
Preoperative planning of a tumor surgery. (a) Shows the cutting trajectories around the tumor, including a safe margin. (b) Shows the instrument designed to resect the tumor. Allograft selection can be performed virtually (c) according to reconstruction needs. An instrument can also be designed to actually cut the allograft (d)
The previously described resurgence of PSI has conducted the developers of the assistances to move toward this new accessible technique. PSI have been tested on plastic pelves to assess the feasibility of tumor resection and estimate their accuracy [7]. The mean accuracy was below 2 mm, showing a significant improvement when compared to the conventional method and a non-significant improvement regarding the optical navigation. Since then, PSI have been used on actual patients to treat several bone (Figs. 13.3 and 13.4). Their excellent accuracy has permitted to decrease the target safe margin from 10 mm (standard desired safe margin) down to 4 mm in some cases. The objective of decreasing the target safe margin is crucial since it allows the preservation of important anatomical structures such as joints, ligament insertions or nerves.
Instruments use during the surgery. The instrument for resection is positioned onto the bone and fix using KWires (a). The process is repeated for the allograft (b). After allograft cutting, the accuracy is checked on the allograft model (c). Finally, the cut allograft is impacted in the defect (d). A perfect fit is obtained with contact for each of the 7 cutting planes
A spin-off company from the Université catholique de Louvain (3D-Side, Belgium) has been launched to put the technology on the market. To date, 55 patients have been successfully treated in several European countries. Clinical series have been reported in the literature showing good oncological results [2, 16]. No local recurrence linked to a bone contamination has been observed postoperatively even if the post-operative follow up is too short to draw strong conclusions. A local recurrence has arose because of a contaminated soft tissue margin. R0 safe margins have been systematically obtained except in one case where the tumor has been morselized to urgently extract it from the patient who was suffering from severe bleeding and poor cardiovascular conditions. A further cost-efficiency study will be led to assess a potential financial benefit of the technique regarding the prevented cost of local recurrence.
Corrective Osteotomies
Patients who have suffered from a bone fracture usually recover a fully normal limb function. In some cases, a non-anatomical bone fusion can be observed yielding to a limited function of the involved limb. When the limitation prevents a normal everyday life, a corrective surgery is indicated. The required correction is often a complex biplanar bone cutting representing a solid angle. By using a conventional manual method, the obtained correction is often suboptimal, leading to an over- or a sub-correction. A 3D simulation of the cuttings is highly helpful to visualize the initial position and estimate the appropriate correction that should be brought.
Some companies (Materialise, 3D-side, Cartis) and academic research projects propose a 3D analysis showing a reconstruction of the bone and proposing a strategy to restore a normal anatomy [11, 12, 41]. The retained surgical option is transferred into the operating room by using PSI. Three different approaches can be adopted.
The first method is based on a PSI that serves as hole driller and saw guide. Firstly, holes are drilled into the involved bone, representing the trajectories of future screws. Secondly, the PSI is used to cut the bone thanks to a slot guiding a saw blade. The PSI is removed from the bone and the reconstruction is performed by inserting a dedicated plate and the pre-drilled screws. This technique requires the use of 3D models from screws and plates of an implant manufacturer during the preoperative planning. Also, the technique does not allow any change in plate and screws sizes.
In the second philosophy, the PSI is positioned onto the bone and fixed in place by using two-by-two parallel k-Wires. The PSI indicate the osteotomy to be performed, guiding the saw blade (Fig. 13.5). After bone cutting, the k-Wires are parallelized to obtain the correct limb alignment as planned preoperatively. This second solution is not dependent from any implant manufacturer and thus any osteosynthesis material can be used to make the osteosynthesis.
Finally, the third method consists in determining a single cut that may correct the anatomy. A PSI allows to perform the cutting and drilling the future screws trajectories. Finally, a patient-specific plate, including a solid angle portion corresponding to the correction that will be brought, is designed to realign the bone segments into an anatomic position. The plate is manufactured by additive manufacturing and implanted during the surgery.
Other Applications
Synostosis
This pathology, abnormal fusion between two bones, usually affects the calcaneonavicular or the talocalcaneal junctions. It occurs in approximatively 1 % of the population, specifically in young people. The treatment is a surgical resection in the coalition zone, removing sufficient portion of bones. The recurrence rate is relatively high because of unsufficient resection. In case of breakage of the healthy joint, hidden by the bones, the foot can be painful. Accuracy can be improved by performing a simulation of the resection and actually create it using a PSI (Fig. 13.6). The planning permits to ensure a complete resection of the degenerative joint. The depth control preventing breaching the healthy joint can be achieved if the saw depth is determined at the stage of preoperative planning. This technique has been reported, as well as early clinical results on 9 patients [10]. No recurrence has been observed at last follow-up.
Paprovsky Pathology
This pathology is a degenerative process of the hip that can lead to incapacity of walking for the patient. In many cases, the hip cannot be restored properly since bone loss is too extensive to accept a standard hip implant. This surgery was among the first to benefit from PSI. A synthetic metallic implant was designed to fill the hip defect and restore a normal anatomy. The implant is manufactured using additive manufacturing, usually in titanium or Cobalt-chromium alloys. The manufacturing process produces porous surfaces, once in contact with patient’s bone present excellent properties to accept bone ingrowth. Regarding the joint, a finishing is required to produce smooth surfaces allowing a normal function of the joint. An associated instrument is designed to perform an accurate resection and ensure an optimal fitting of the implant with the anatomy. Mobelife, a spin-out from Materialise (Leuven, Belgium) has put this solution on the market in the years 2010. The main disadvantage of the methodology is the high cost of the manufacturing that leads to a very expensive solution for the surgeon. The medical benefit should be balanced against the economic profit that may incur. In some countries, the social system has accepted a reimbursement.
Ilio-Sacral Screws
Stabilization of joint dislocation or sacral fractures is usually performed by inserting screws through the sacro-iliac joint. The accuracy is crucial in this surgery to ensure a bone insertion without breaching sacral nerves. Recently, PSI have been clinically used in 16 patients [8]. Reported results were promising when compared with conventional fluoroscopic insertion. A significant improvement in accuracy has been shown. PSI are particularly suitable for this application since the surfaces of the iliac crest are highly discriminant allowing an easy positioning and an immediate stability of PSI.
Conclusion
Patient-Specific Instruments has deeply modified the orthopedic surgery, bringing new possibilities [32]. Supported by what is considered as the third industrial revolution, namely additive manufacturing, PSI have invaded the operative room. Emphasize must be put on the pre-operative planning which takes a crucial role. Firstly, it has to be as accurate as possible since the assistance is meant to replicate the planning on the actual bone. Secondly, the planning must first conform to the situation that will be met in the operative room. It implies that the surgeon anticipates how surgery will be performed several days or weeks before the actual surgery. For example, the surgical approach must be firmly defined since it has a strong impact on the instrument design or the contact surface with bone. Finally the planning must be performed using 3D data to define cutting or drilling trajectories in the 3D space. This new approach generates new tasks to perform and new tools to understand for the surgeon. That’s why an engineer is often responsible for handling the computerized tools that produces the pre-operative planning. The cooperation between the surgeon and the engineer is thus critical to generate a planning that reaches the desired target and meets the medical requirements.
The story of PSI is very interesting to understand how a disruptive technology can be adopted. While it has shown to be of great help, accurate, safe and easy to use, Patient-Specific Instruments have not met the success that could have been forecasted. Proposed applications were scientifically interesting, but financially not mature enough to be widely pulled on the market by customers. When implant manufacturers have adopted the technology, a large push has been observed. Then, the technique has been quickly and widely approved at first, surfing over a positive wave. A large amount of literature has been published concluding that PSI was the best option, without any supporting data. This statement has rapidly been destroyed by evidence-based medicine and the clinical observation that from the patient’s side, no benefit was shown. Today, it seems that the expectations curve is finding an inflection point with a resurgence in favor of PSI for total knee arthroplasty. The future of this application is certainly between a large enthusiasm and the total rejection. In particularly deformed bones or rare pathologies, PSI should be of great help, improving the understanding of the pathology and guiding the surgical gesture. In these days, PSI are still in use for this application since manufacturers are displaying amazing figures: Materialise, has manufactured 146.000 PSI in 2013. The evolution of this figure in 2015 should give an overview of the future trend for PSI.
References
Barrack RL, Ruh EL, Williams BM, Ford AD, Foreman K, Nunley RM. Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94:95–9. doi:10.1302/0301-620X.94B11.30834.
Bellanova L, Paul L, Docquier P-L. Surgical guides (patient-specific instruments) for pediatric tibial bone sarcoma resection and allograft reconstruction. Sarcoma. 2013;2013:787653. doi:10.1155/2013/787653.
Berlet GC, Penner MJ, Lancianese S, Stemniski PM, Obert RM. Total ankle arthroplasty accuracy and reproducibility using preoperative CT scan-derived. Patient-specific guides. Foot Ankle Int. 2014;35:665–76. doi:10.1177/1071100714531232.
Birnbaum K, Schkommodau E, Decker N, Prescher A, Klapper U, Radermacher K. Computer-assisted orthopedic surgery with individual templates and comparison to conventional operation method. Spine. 2001;26:365–70.
Cartiaux O, Banse X, Paul L, Francq BG, Aubin C-É, Docquier P-L. Computer-assisted planning and navigation improves cutting accuracy during simulated bone tumor surgery of the pelvis. Comput Aided Surg. 2013;18:19–26. doi:10.3109/10929088.2012.744096.
Cartiaux O, Docquier P-L, Paul L, Francq BG, Cornu OH, Delloye C, Raucent B, Dehez B, Banse X. Surgical inaccuracy of tumor resection and reconstruction within the pelvis: an experimental study. Acta Orthop. 2008;79:695–702. doi:903404236.
Cartiaux O, Paul L, Francq BG, Banse X, Docquier P-L. Improved accuracy with 3D planning and patient-specific instruments during simulated pelvic bone tumor surgery. Ann Biomed Eng. 2014;42:205–13. doi:10.1007/s10439-013-0890-7.
Chen B, Zhang Y, Xiao S, Gu P, Lin X. Personalized image-based templates for iliosacral screw insertions: a pilot study. Int J Med Robot. 2012;8:476–82. doi:10.1002/rcs.1453.
Delloye C, Banse X, Brichard B, Docquier P-L, Cornu O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am. 2007;89:579–87.
De Wouters S, Tran Duy K, Docquier P-L. Patient-specific instruments for surgical resection of painful tarsal coalition in adolescents. Orthop Traumatol Surg Res. 2014;100:423–7. doi:10.1016/j.otsr.2014.02.009.
Dobbe JGG, du Pré KJ, Kloen P, Blankevoort L, Streekstra GJ. Computer-assisted and patient-specific 3-D planning and evaluation of a single-cut rotational osteotomy for complex long-bone deformities. Med Biol Eng Comput. 2011;49:1363–70. doi:10.1007/s11517-011-0830-3.
Dobbe JGG, Vroemen JC, Strackee SD, Streekstra GJ. Patient-tailored plate for bone fixation and accurate 3D positioning in corrective osteotomy. Med Biol Eng Comput. 2013;51:19–27. doi:10.1007/s11517-012-0959-8.
Docquier P-L. Computer-navigated bone cutting in the resection of a pelvic bone tumor and reconstruction with a massive bone allograft. JBJS Essent Surg Tech. 2011;1:1–13. doi:10.2106/JBJS.ST.K.00013.
Docquier P-L, Paul L, Cartiaux O, Delloye C, Banse X. Computer-assisted resection and reconstruction of pelvic tumor sarcoma. Sarcoma. 2010;2010:125162. doi:10.1155/2010/125162.
Ferrari V, Parchi P, Condino S, Carbone M, Baluganti A, Ferrari M, Mosca F, Lisanti M. An optimal design for patient-specific templates for pedicle spine screws placement. Int J Med Robot. 2013;9:298–304. doi:10.1002/rcs.1439.
Gouin F, Paul L, Odri GA, Cartiaux O. Computer-assisted planning and patient-specific instruments for bone tumor resection within the pelvis: a series of 11 patients. Sarcoma. 2014;2014:e842709. doi:10.1155/2014/842709.
Hafez MA, Chelule KL, Seedhom BB, Sherman KP. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop. 2006;444:184–92. doi:10.1097/01.blo.0000201148.06454.ef.
Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–63.
Hozack WJ. In reply. J Arthroplasty. 2008;23:638. doi:10.1016/j.arth.2008.03.008.
Kitada M, Sakai T, Murase T, Hanada T, Nakamura N, Sugano N. Validation of the femoral component placement during hip resurfacing: a comparison between the conventional jig, patient-specific template, and CT-based navigation. Int J Med Robot. 2013;9:223–9. doi:10.1002/rcs.1490.
Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23:26–9. doi:10.1016/j.arth.2007.10.001.
Lombardi AV, Berend KR, Adams JB. Patient-specific approach in total knee arthroplasty. Orthopedics. 2008;31:927–30. doi:10.3928/01477447-20080901-21.
Lu S, Xu YQ, Zhang YZ, Li YB, Xie L, Shi JH, Guo H, Chen GP, Chen YB. A novel computer-assisted drill guide template for lumbar pedicle screw placement: a cadaveric and clinical study. Int J Med Robot. 2009;5:184–91. doi:10.1002/rcs.249.
McGurk M, Amis AA, Potamianos P, Goodger NM. Rapid prototyping techniques for anatomical modelling in medicine. Ann R Coll Surg Engl. 1997;79:169–74.
Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop. 2012;470:895–902. doi:10.1007/s11999-011-2222-2.
Paul L, Cartiaux O, Docquier P-L, Banse X. Ergonomic evaluation of 3D plane positioning using a mouse and a haptic device. Int J Med Robot. 2009;5:435–43. doi:10.1002/rcs.275.
Paul L, Docquier P-L, Cartiaux O, Cornu O, Delloye C, Banse X. Selection of massive bone allografts using shape-matching 3-dimensional registration. Acta Orthop. 2010;81:250–5. doi:10.3109/17453671003587127.
Radermacher K, Bliem R, Hennecke C, Staudte HW, Rau G. A desktop image processing system for computer-assisted orthopedic surgery (DISOS). Stud Health Technol Inform. 1996;29:675–80.
Radermacher K, Portheine F, Anton M, Zimolong A, Kaspers G, Rau G, Staudte HW. Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop. 1998 (354):28–38.
Radermacher K, Portheine F, Zimolong A, Eichhorn C, Staudte H-W, Rau G. Image guided Orthopedic Surgery using individual templates. In Troccaz J, Grimson E, Mösges R, editors. CVRMed-MRCAS’97, Lecture notes in computer science. Berlin/Heidelberg: Springer; 1997. p. 606–15.
Radermacher K, Staudte HW, Rau G. Computer assisted orthopedic surgery by means of individual templates-aspects and analysis of potential applications. In DiGioia A, editor. Proceedings of the first international symposium on medical robotics and computer assisted surgery. Presented at the first international symposium on medical robotics and computer assisted surgery, Pittsburgh; 1994. p. 42–8.
Radermacher K. Renaissance of computer-assisted orthopedic surgery with individual templates: evolution or revolution? In: Haaker R, Konermann W, editors. Computer and template assisted orthopedic surgery. Berlin/Heidelberg: Springer; 2013. p. 11–21.
Rathnayaka K, Momot KI, Noser H, Volp A, Schuetz MA, Sahama T, Schmutz B. Quantification of the accuracy of MRI generated 3D models of long bones compared to CT generated 3D models. Med Eng Phys. 2012;34:357–63. doi:10.1016/j.medengphy.2011.07.027.
Sakai T, Hanada T, Murase T, Kitada M, Hamada H, Yoshikawa H, Sugano N. Validation of patient specific surgical guides in total hip arthroplasty. Int J Med Robot. 2014;10:113–20.
Schkommodau E, Decker N, Klapper U, Birnbaum K, Staudte H-W, Radermacher K. Pedicle screw implantation using the DISOS template system. In: Navigation and robotics in total joint and spine surgery. Berlin/Heidelberg: Springer; 2004. p. 501–5.
Staudte H-W, Schkommodau E, Honscha M, Portheine F, Radermacher K. Pelvic osteotomy with template navigation. In: Navigation and robotics in total joint and spine surgery. Berlin/Heidelberg: Springer; 2004. p. 455–63.
Thienpont E. Recent advances in knee surgery. The Knee. 2013 (20 Suppl 1):S1–2. doi:10.1016/S0968-0160(13)70002-4.
Thienpont E, Schwab PE, Fennema P. A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Joint J. 2014;96-B:1052–61. doi:10.1302/0301-620X.96B8.33747.
Van den Broeck J, Vereecke E, Wirix-Speetjens R, Vander Sloten J. Comparing CT and MRI segmentation accuracy of long bones [WWW Document]. 2013. https://lirias.kuleuven.be/handle/123456789/413823. Accessed 11 Mar 2014.
Vernace JV, Bodenstab A. Letter to the editor. J Arthroplasty. 2008;23:637–8. doi:10.1016/j.arth.2008.03.007.
Victor J, Premanathan A. Virtual 3D planning and patient specific surgical guides for osteotomies around the knee: a feasibility and proof-of-concept study. Bone Joint J. 2013;95-B:153–8. doi:10.1302/0301-620X.95B11.32950.
White D, Chelule KL, Seedhom BB. Accuracy of MRI vs CT imaging with particular reference to patient specific templates for total knee replacement surgery. Int J Med Robot. 2008;4:224–31. doi:10.1002/rcs.201.
Zhang YZ, Chen B, Lu S, Yang Y, Zhao JM, Liu R, Li YB, Pei GX. Preliminary application of computer-assisted patient-specific acetabular navigational template for total hip arthroplasty in adult single development dysplasia of the hip. Int J Med Robot. 2011;7:469–74. doi:10.1002/rcs.423.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Laurent, P. (2016). Patient-Specific Instruments in Orthopedics. In: Ritacco, L., Milano, F., Chao, E. (eds) Computer-Assisted Musculoskeletal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-12943-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-12943-3_13
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12942-6
Online ISBN: 978-3-319-12943-3
eBook Packages: MedicineMedicine (R0)