Abstract
Purpose
We aimed to evaluate the efficacy and outcomes of radioembolization with Yttrium-90 (Y-90) microspheres in patients with unresectable and chemorefractory colorectal cancer liver metastasis (CRCLM).
Methods
This single-center study included 43 patients (34 male, 9 female) who underwent radioembolization with Y-90 for unresectable, chemorefractory CRCLM between September 2008 and July 2014. Overall survival (OS), liver progression-free survival (LPFS), overall response rate (ORR), local disease control rate (LDCR), and relations of these parameters with patient disease characteristics were evaluated. OS and LPFS rates were compared according to microspheres. Survival rates were calculated with Kaplan-Meier method, and potential prognostic variables were evaluated on univariate analyses.
Results
Post-procedural median OS was 12.8 months. LPFS was 5.6 months. ORR was 33%, LDCR was 67% on 3rd month follow-up. Low tumor burden (< 25%) was associated with higher median OS after radioembolization (< 25 vs > 25–50% p < 0.0001 and < 25 vs > 50% p = 0.005). Patients with left colon tumors exhibited significantly longer median OS after metastasis than right colon tumors (p = 0.046). Extrahepatic disease and synchronicity showed poorer survival parameters; however, the difference was not significant (p = 0.1 and p = 0.3, respectively). In subgroup analyses, the distribution of patient number and characteristics showed heterogeneity as number of patients with low tumor burden was higher in resin Y-90 group. Resin Y-90 group exhibited significantly higher median OS and LPFS compared to glass Y-90 group (16.5 vs. 7 months, p = 0.001; 6.73 vs. 3.38 months, p = 0.023, respectively).
Conclusion
Radioembolization is a safe local-regional treatment option in chemorefractory, inoperable CRCLM. Radioembolization at earlier stages may lead to more favorable results especially with lower tumor burden patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the second most common cancer worldwide with more than 1.2 million new cases diagnosed each year [1]. It has a high mortality and is the third most common cause of death related to cancer [2]. Liver is the most common site of metastasis, as well as recurrence [3]. Nearly one third of CRC patients have liver metastasis (CRCLM) at the time of diagnosis; and half of the rest develops metastasis during the course of the disease [4, 5]. Overall 5-year survival rate among distant metastatic disease is reported 11.7% and the major cause of death is liver failure due to hepatic metastases [2, 6]. Management mainly includes surgery followed by chemotherapy, also in selected cases resection of the metastatic lesions.
Even though resection is curative in early liver metastatic disease, its feasibility depends on a number of factors such as presence of extrahepatic disease; number, location, and size of hepatic tumors and comorbidities, and it can be done in only 20% of patients [6, 7]. Moreover, despite the high survival rates achieved by surgery, about 70% of patients develop recurrence within 3 years [8]. With recent advances in conventional chemotherapeutics and introduction of molecular targeted biological agents, overall survival has improved. However, unresectable, chemorefractory CRCLM is still an important cause of mortality and morbidity.
Radioembolization (RE) with Yttrium-90 (Y-90) delivers locoregional radiation therapy to unresectable primary and secondary hepatic malignancies. RE uses the dual blood supply of liver parenchyma and includes intraarterial infusion of Y-90 embedded resin or glass microspheres which disperse in the tumor bed. It decreases blood supply of the tumor at a microvascular level, minimizes the systemic effect of radiation as well as achieving a dose with an endovascular approach that cannot be possible externally [9, 10]. Currently, two different types of Y-90 microspheres, glass or resin, are commercially available. Although having differences in specific activity and dosimetry methods, they both have shown to be effective, safe, and well tolerated with encouraging results [10,11,12,13,14,15,16,17,18]. However, latest clinical guidelines of European Society of Medical Oncology (ESMO) endorse treatment with only Y-90 resin microspheres in patients with CRCLM failing available chemotherapeutic options with a level of evidence 4B [19].
The primary aim of this study is to document our institutional outcomes of Y-90 radioembolization in unresectable chemorefractory CRCLM. As a secondary outcome survival rates right versing left colon tumors, and of resin versing glass microspheres were compared.
Patients and Methods
Patient Selection and Demographics
Forty-three patients with CRCLM who underwent RE with Y-90 between September 2008 and July 2014 were included in this retrospective study. RE treatment decision was determined by a multidisciplinary team consisting of a medical oncologist, a general surgeon, an interventional radiologist, and a nuclear medicine specialist.
The inclusion criteria for Y-90 treatment were as follows: (1) pathological diagnosis of adenocancer by surgical specimen or colonoscopic biopsy, (2) proof of disease progression under chemotherapy by cross-sectional imaging [computed tomography (CT), magnetic resonance imaging (MRI)] or fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography (18-FDG-PET/CT), (3) liver dominant metastatic disease not feasible for resection or ablation, and (4) Eastern Cooperative Oncology Group (ECOG) performance status less than 2. The exclusion criteria were as follows: (1) active dominant extrahepatic disease, (2) uncorrectable gastrointestinal leak in technetium-99m-labeled macroaggregated albumin (Tc-99m-MAA) scan, (3) estimated lung dose more than 30 Gy, (4) inadequate hepatic reserve (bilirubin > 2 mg/dl, albumin < 3 g/dl), (5) concurrent chemotherapy or radiotherapy, and (6) any contraindication for anesthesia, angiography, or selective catheterization.
All patients underwent routine baseline serology, including liver and renal function tests, coagulation tests, and complete blood count, as well as cross-sectional imaging (CT and/or MRI) and 18F-FDG-PET. In addition, after an informed consent was obtained for the procedure, each patient underwent a liver angiography with Tc-99m-MAA scintigraphy to identify the hepatic anatomy and percentage of lung shunting. Parasitic arteries of the tumors and arteries such as gastroduodenal artery or right gastric artery that increased the risk for extrahepatic leakage were occluded. The total volume of the liver and the volume of the right and left lobe also the percentage of the liver tumor burden were calculated using preoperative imaging studies. RE was performed within 1 month of preliminary angiography with Y-90-glass (TheraSphere; MDS Nordion Ottawa, ON, Canada) or Y-90-resin (SIR-Spheres; SIRTeX Medical Limited, Sydney, Australia) microspheres. The choice between the microspheres was related with the tender purchasing policies followed by the hospital at that time. The treatment strategy of lobar, sequential lobar, or whole liver Y-90 RE was determined according to the patients’ extent of disease. All patients were hospitalized overnight and discharged the next day.
All patients were followed up on first month and then every 2–3 months until death. In addition to clinical examination and routine laboratory tests, cross-sectional imaging (CT or MRI) and/or 18-FDG-PET/CT were obtained and assessed at each follow-up visit.
Study Design and Definitions
All patient files were retrospectively analyzed through hospital archives and electronical data base. Clinicopathologic and treatment-related data were reviewed. Adverse events were recorded according to National Cancer Institute Common Terminology Criteria for Adverse Events v4.03. For the primary outcome of the study, overall survival (OS) and liver tumor response were evaluated. Tumor response on cross-sectional imaging (CT/MRI) was assessed using modified RECIST 1.1 (Response Evaluation Criteria in Solid Tumors) criteria or/and on PET imaging using PERCIST (PET Response Evaluation Criteria in Solid Tumors) criteria. Overall response rate (ORR), local disease control rate (LDCR), and liver progression-free survival (LPFS) were noted. Patient and disease characteristics and previous treatments were evaluated in relation to OS and LPFS. As a secondary outcome, response rates and OS between resin and glass microspheres were compared.
OS was evaluated both for the time period from initial RE and also from the time period of diagnosis of liver metastasis to patient death. LPFS was defined as the time from initial RE to documented liver progression using modified RECIST and/or PERCIST. ORR was defined for the patients with complete response (CR) and partial response (PR). LDCR was defined for patients with CR, PR, and stable disease (SD).
Statistical Analysis
Data were recorded and verified using SPSS version 17 and 22. Median OS from the date of diagnosis of the hepatic metastasis and from the date of first RE, as well as LPFS, was calculated according to Kaplan-Meier analysis. All patients’ time of death was found through state healthcare system. Patients who were lost to follow-up and who died before the first evaluation were excluded from LPFS calculation since imaging data were not available. Statistical analyses between OS of glass vs resin microspheres and left vs right colon tumors were done with Kaplan-Meier analysis and log rank tests. Significant variable on univariate analyses for OS and LPFS was calculated with Cox regression. Multivariate analysis was not performed due to inadequate number of patients.
Results
Patients’ Characteristics
Forty-three patients (34 male, 9 female, mean age: 52.5 ± 10.8) with CRCLM who underwent RE were included in the study. The primary tumor was in the right colon in 9 patients and in the left colon in 30 patients. Four patients had the primary tumor in the transverse colon. Thirty-three patients (76.7%) had synchronous metastasis and 10 (23.3%) had metachronous metastasis. Extrahepatic non-dominant tumor was present in 19 patients (44%). All patients scored less than 2 in ECOG performance status. All patients were heavily pretreated and all exhibited progression under multiple lines of chemotherapy prior to RE. Prior to radioembolization, 33 patients had oxaliplatin-based chemotherapy, 10 of these patients has oxaliplatin-based chemotherapy twice during their treatment. Thirty-two patients had irinotecan-based chemotherapy. Six of these patients had irinotecan for 12 weeks and one patient had for 19 weeks. Nine patients had had their first line, 18 had their second line, 13 had their third line, and 3 had their forth line of chemotherapy before radioembolization. Thirty-two patients received only bevacizumab, two received only cetuximab, and six (14%) received both agents in addition to standard chemotherapy lines. In total, 97% of patients had received a molecular targeted biological agent.
Patient and disease characteristics are summarized in Table 1.
Twenty-eight patients (65%) had bilobar disease and 15 patients (35%) had unilobar disease. In five patients with bilobar disease, TACE with irinotecan was preferred to the contralateral lobe as they had very limited disease in the contralateral lobe.
Median Y-90 activity was 1.40 GBq (range 0.81–9.5). RE was generally well tolerated; all adverse events were transient and controlled with symptomatic treatment. Greater intraoperative pain was observed by the operators when resin microspheres were used. Of note, at that time, sterile water was used for injection with resin microspheres. No grade 3 or 4 adverse event was reported.
Among 43 patients, four patients were lost to follow-up and six patients died before the first imaging control. Their time of death was accessed via state health care system, and they were included in OS calculations. However, since imaging data were not available for these ten patients, they were excluded from LPFS evaluation.
Mean follow-up time for patients were 11.2 months (range: 1.53–27.8). Median time from metastasis to RE was 18.2 months. The median OS after the first treatment was 12.8 months and median OS after metastasis was 32.8 months. Six-, 12-, 18-, 24-, 30-, 36-, and 60 month survival were 74.4, 48.8, 32.5, 27.9, 13.9, 11.6, and 2.3%, respectively. Median liver progression-free survival (LPFS) was calculated 5.6 months (1.1–27.6).
In patients with left colon tumors, median OS after metastasis was 40.8 months (95% confidence interval [CI], 24–57.6), median OS after RE was 13.7 months (95% confidence interval [CI], 5.5–21.8), and LPFS was 7.1 months (95% confidence interval [CI], 4–10.2).
In patients with right colon tumors, median OS after metastasis was 23 months (95% confidence interval [CI], 13.2–32.6), median OS after RE was 9.6 months (95% confidence interval [CI], 5.2–13.9), and LPFS was 5.2 months (95% confidence interval [CI], 3.5–6.9),
Median OS after metastasis was significantly longer in patients with left colon tumor (p = 0.046). Median OS after RE and LPFS were also longer in patients in this group; however, the difference was not statistically significant (p = 0.35 and p = 0.22, respectively).
Resin microspheres were used in 27 (62.8%) patients (23 male, 4 female; mean age 52.6 ± 9.7) and glass microspheres in 16 (37.2%) (12 male, 4 female; mean age 52.2 ± 12.8). Median Y-90 activity received was 1.26 GBq (range 0.81–2.77) for resin Y-90 and 2.75 GBq (range 1.06–9.5) for glass Y-90. The calculated Y-90 activity could not be delivered in four patients (9%) due to early stasis during infusion with resin microspheres. Disease and treatment characteristics and survival parameters according to the type of microspheres are summarized in Table 2.
After exclusion of patients who were lost to follow-up and died before the first follow-up, 3rd month evaluation of images of remaining patients (n = 33) based on target lesion showed CR in 2 (6%), PR in 9 (28%), and SD in 11 (33%) patients. Eleven patients (33%) had progressive disease (PD) at the end of 3 months. ORR was 33%, LDCR was 67%. Six-month follow-up of patients with local disease control (n = 22) showed SD in 12 patients and PD in 10 patients.
Subgroup analyses for two different Y-90 product showed ORR and LDCR on 3rd month follow-up, as 26 and 65.2% in resin Y-90 group and 31.2 and 43.7% in glass Y-90 group, respectively. Median LPFS was 6.73 months for resin Y-90 and 3.38 months for glass Y-90; the difference was statistically significant (p = 0.023).
Median OS after metastasis was 40.8 months (95% confidence interval [CI], 21–61) in resin Y-90 group and 23 months (95% CI, 21–25) in glass Y-90 group (Fig. 1). Median OS after initial RE was 16.5 months (95% CI, 8.4–27.2) in resin Y-90 group and 7 months (95% CI, 2.4–9) in glass Y-90 group (Fig. 2). Both differences were statistically significant (p = 0.026 and p = 0.001, respectively).
Median OS after RE was significantly higher in patients with less than 25% tumor burden (< 25 vs > 25–50% p < 0.0001 and < 25 vs > 50% p = 0.005). The difference was significant in glass Y-90 group as well (< 25 vs > 25–50% p = 0.02). Although longer OS was found with lesser tumor burden in resin Y-90 group, the difference was not statistically significant.
Patients with low tumor burden also exhibited longer LPFS; however, the difference was not significant (< 25 vs > 25–50% p = 0.87 and < 25 vs > 50% p = 0.88). Presence of extrahepatic disease and synchronicity indicated poorer survival parameters but the difference was not significant (Table 3). At subgroup analysis according to microsphere types, no significant difference was found between resin and glass microsphere groups as well (Table 4).
Discussion
Liver is not only the major metastasis site for CRC but also the most common recurrence site [3]; however, only a small number of patients are candidates for surgery. In the last decades, advances in chemotherapeutics as well as introduction of molecular targeted biological agents have enabled a better prognosis for patients with inoperable CRCLM. Nevertheless, there is still a significant percentage of patients that are refractory to chemotherapy. Locoregional therapies have become important therapeutic options for these inoperable and chemo-resistant cases. Among these, radioembolization with Y-90 has been shown to have encouraging results [2, 10,11,12,13,14,15,16,17,18].
Radioembolization, also known as selective internal radiation therapy, is based on the dual blood supply of hepatic parenchyma: hepatic tumors predominantly have arterial supply whereas normal hepatic parenchyma gets its blood supply from portal venous system. Thus, by transarterial administration of Y-90 embedded particles, the adequate amount of radiation can be provided in the tumor bed, sparing the normal liver parenchyma [9, 10].
In this study, we aimed to investigate the OS and LPFS in chemorefractory, inoperable CRCLM patients after performing radioembolization as a salvage therapy. Survival rates of resin versing glass microspheres were also compared as a secondary outcome.
All of our patients had progression under chemotherapy. Seventy-six percent of patients had presented with synchronous metastasis. More than half of our patients had bilobar disease and 44% had extrahepatic disease at the time of radioembolization. A locoregional therapy was already performed in one third of patients prior to RE and majority of patients had received one or more molecular targeted biological agent.
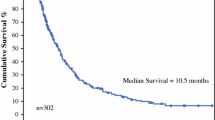
Our study group showed median OS after the procedure and after metastasis as 12.8 and 32.8 months, respectively. Both of our results corroborate the literature [2, 14,15,16, 20,21,22,23,24,25,26]. Our survival rates reinforce findings of Saxena et al. [21], whose study of 302 patients exhibited a median OS of 10.5 months. Kennedy et al. [25] reported a median OS of 9.6 months in their multicentered evaluation of 606 CRCLM patients. Moreover, in their retrospective analysis of 214 patients, Lewandowski et al. [2] found that biological agents caused lower post-Y-90 survival rates, potentially due to adverse effects of chemotherapeutics. In our study, 97% of patients were treated with ≥ 1 biological agents prior to RE. Studies where radioembolization is applied earlier in the course of disease or radioembolization is combined with chemotherapeutics have shown promising results [27,28,29,30]. Recently presented, SIRFLOX study which involves more than 500 CRCLM patients that underwent radioembolization together with FOLFOX6 as a first line therapy strongly suggests better hepatic tumor control compared to FOLFOX6-only group [27]. The high survival rates despite heavy disease burden and cytotoxic agents may strongly substantiate that radioembolization should be performed at an earlier stage of treatment in CRCLM [2, 16, 17, 21].
Our patients experienced very low toxicity similar to literature [10, 14,15,16, 20, 21]. Greater intraoperative pain was observed by the operators when resin microspheres were used which can be explained by the time sterile water was used for injection.
Six patients unexpectedly died before the first follow-up imaging outside the hospital and four patients were lost to follow-up. With exclusion of these ten patients since there were no images available for evaluation, LPFS was 5.6 months. At 3-month follow-up based on target lesion, ORR was 33% and LDCR was 67%. Both ORR and LPFS were substantially low compared to SIRFLOX study (ORR: 78.8%, LPFS: 20.5 months) [27]. We ascribed this difference mainly to the advanced stage of our patients and that all our procedures were performed as salvage therapy.
In the literature, a number of parameters such as tumor burden, extrahepatic disease, biological agents, the number of lines of chemotherapy, and tumor stage at the time of diagnosis were found to be associated with OS [2, 10, 20,21,22,23,24,25,26]. In our study, the only statistically significant difference was observed for OS with tumor burden ≤ 25%. The difference was also significant in glass Y-90 group. LPFS was higher in patients with low tumor burden but the difference was not significant. Cox regression analysis also showed patients with extrahepatic disease, and synchronous tumors were more likely to have poorer OS and LPFS but the differences were not significant. We believe that this could be due to the small sample size and the lack of detailed information on the previous medical history of these patients since they are mostly referred to our department from other institutions.
Tumor sidedness has been shown as an important predictor of pathogenesis and outcome in CRC possibly due to genetic and environmental factors [31, 32]. In our study, median OS after metastasis was significantly longer in patients with left colon tumor. However, the difference was not significant in median OS after RE and LPFS. We may hypothesize that primary tumor localization is not significantly effective on RE response, but this should be studied further with larger patient groups.
Survival outcomes were also compared according to type of microspheres used. In our study, median OS after metastasis, median OS after RE, and LPFS were significantly longer in resin Y-90 group than glass Y-90 group. This difference could be explained due to the heterogeneity between the groups, as resin group had higher number of patients and also a higher percentage of low tumor burden patients. Also, the number of extrahepatic metastasis was higher in glass group showing advance stage disease. In the literature, studies with both microspheres are reported for salvage therapy in advanced CRC. In their latest guidelines, however, ESMO recommends RE with resin microspheres for CRCLM where the disease is limited to the liver and does not respond to chemotherapy [19].
Our study has many limitations, above of all its retrospective nature. This is a single-center-based study, and some patients were excluded due to lacking detailed data on patients’ previous medical history, thus leading to a smaller sample size than expected. Absence of a control group is another weakness of this study.
In conclusion, our results, in line with a great number of reports in literature, show that radioembolization is a safe option in advanced stage, chemorefractory, inoperable CRCLM. It provides high clinical benefit at local tumor control with low toxicity. Survival was statistically longer for patients with low tumor burden (< 25%). Patients with left colon tumors exhibited significantly longer median OS after metastasis than right colon tumors. Recent studies, together with its success in heavily treated patients with high tumor burden and comorbidities strongly suggest that early introduction of radioembolization in the treatment may lead to better outcomes.
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. Cancer. 2011;61:69–90.
Lewandowski RJ, Memon K, Mulcahy MF, Hickey R, Marshall K, Williams M, et al. Twelve-year experience of radioembolization for colorectal hepatic metastases in 214 patients: survival by era and chemotherapy. Eur J Nucl Med Mol Imaging. 2014;41(10):1861–9. https://doi.org/10.1007/s00259-014-2799-2.
Seo SI, Lim SB, Yoon YS, Kim CW, Yu CS, Kim TW, et al. Comparison of recurrence patterns between ≤5 years and >5 years after curative operations in colorectal cancer patients. J Surg Oncol. 2013;108(1):9–13. https://doi.org/10.1002/jso.23349.
Kemeny N, Kemeny M, Lawrence T. Liver metastases. In: Abeloff M, Armitage J, Niederhuber J, Lichter A, editors. Clinical oncology. 3rd ed. Philadelphia, PA: Elsevier Clinical Oncology; 2004. p. 1141–78.
Manfredi S, Bouvier AM, Lepage C, Hatem C, Dancourt V, Faivre J. Incidence and patterns of recurrence after resection for cure of colonic cancer in a well defined population. Br J Surg. 2006;93(9):1115–22. https://doi.org/10.1002/bjs.5349.
Geoghegan JG, Scheele J. Treatment of colorectal liver metastasis. Br J Surg. 1999;86(2):158–69. https://doi.org/10.1046/j.1365-2168.1999.01013.x.
Xing M, Koooby DA, El-Rayes BF, et al. Locoregional therapies for metastatic colorectal carcinoma to the liver--an evidence-based review. J Surg Oncol. 2014;110(2):182–96. https://doi.org/10.1002/jso.23619.
Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Kalva SP, Thabet A, Wicky S. Recent advances in transarterial therapy of primary and secondary liver malignancies. Radiographics. 2008;28(1):101–17.
Sato KT, Lewandowski R, Mulcahy MF, et al. Unresectable chemorefractory liver metastases: radioembolization with 90Y microspheres- safety, efficacy, and survival. Radiology. 2008;247(2):507–15.
Andrews JC, Walker SC, Ackermann RJ, Cotton LA, Ensminger WD, Shapiro B. Hepatic radioembolization with yttrium-90 containing glass microspheres: preliminary results and clinical follow-up. J Nucl Med. 1994;35(10):1637–44.
Lewandowski RJ, Thurston KG, Goin JE, Wong CYO, Gates VL, Buskirk MV, et al. 90Y microsphere (TheraSphere) treatment for unresectable colorectal cancer metastases of the liver: response to treatment at targeted doses of 135-150 Gy as measured by [18F]fluorodeoxyglucose positron emission tomography and computed tomographic imaging. J Vasc Interv Radiol. 2005;16(12):1641–51. https://doi.org/10.1097/01.RVI.0000179815.44868.66.
Kennedy AS, Coldwell D, Nutting C, et al. Resin Y90-microsphere brachytherapy for unresectable colorectal liver metastases: modern USA experience. Int J Radiat Oncol Biol Phys. 2006;65(2):412–25.
Jakobs TF, Hoffmann R, Dehm K, et al. Hepatic yttrium-90 radioembolization of chemotherapy-refractory colorectal cancer liver metastases. J Vasc Interv Radiol. 2008;19(8):1187–95.
Cianni R, Urigo C, Notarianni E, et al. Selective internal radiation therapy with SIR-spheres for the treatment of unresectable colorectal hepatic metastases. Cardiovasc Intervent Radiol. 2009;32(6):1179–86.
Cosimelli M, Golfieri R, Cagol PP, et al. Multi-centre phase II clinical trial of yttrium-90 resin microspheres alone in unresectable, chemotherapy refractory colorectal liver metastases. Br J Cancer. 2010;103(3):324–31.
Nace GW, Steel JL, Amesur N, et al. Yttrium-90 radioembolization for colorectal cancer liver metastases: a single institution experience. Int J Surg Oncol. 2011;2011:571261.
Bester L, Meteling B, Pocock N, et al. Radioembolisation with Yttrium-90 microspheres: an effective treatment modality for unresectable liver metastases. J Med Imaging Radiat Oncol. 2013;57(1):72–80.
Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422.
Kalva SP, Rana RS, Liu R, Rachamreddy N, Dave B, Sharma A, et al. Yttrium-90 radioembolization as salvage therapy for liver metastases from colorectal cancer. Am J Clin Oncol. 2017;40(3):288–93. https://doi.org/10.1097/COC.0000000000000151.
Saxena A, Meteling B, Kapoor J, et al. Is yttrium-90 radioembolization a viable treatment option for unresectable, chemorefractory colorectal cancer liver metastases? A large single-center experience of 302 patients. Ann Surg Oncol. 2015;22(3):794–802.
Martin LK, Cucci A, Wei L, et al. Yttrium-90 radioembolization as salvage therapy for colorectal cancer with liver metastases. Clin Colorectal Cancer. 2012;11(3):195–9.
Bester L, Meteling B, Pocock N, et al. Radioembolization versus standard care of hepatic metastases: comparative retrospective cohort study of survival outcomes and adverse events in salvage patients. J Vasc Interv Radiol. 2012;23(1):96–105.
Seidensticker R, Denecke T, Kraus P, et al. Matched-pair comparison of radioembolization plus best supportive care versus best supportive care alone for chemotherapy refractory liver-dominant colorectal metastases. Cardiovasc Intervent Radiol. 2012;35(5):1066–73.
Kennedy AS, Ball D, Cohen SJ, et al. Multicenter evaluation of the safety and efficacy of radioembolization in patients with unresectable colorectal liver metastases selected as candidates for (90)Y resin microspheres. J Gastrointest Oncol. 2015;6(2):134–42.
Hickey R, Lewandowski RJ, Prudhomme T, Ehrenwald E, Baigorri B, Critchfield J, et al. 90Y radioembolization of colorectal hepatic metastases using glass microspheres: safety and survival outcomes from a 531-patient multicenter study. J Nucl Med. 2016;57(5):665–71. https://doi.org/10.2967/jnumed.115.166082.
Van Hazel GA, Heinemann V, Sharma NK, et al. SIRFLOX: randomized phase III trial comparing first-line mFOLFOX6 (plus or minus bevacizumab) versus mFOLFOX6 (plus or minus bevacizumab) plus selective internal radiation therapy in patients with metastatic colorectal cancer. J Clin Oncol. 2016;34(15):1723–31.
van Hazel G, Blackwell A, Anderson J, et al. Randomised phase 2 trial of SIR-spheres plus fluorouracil/ leucovorin chemotherapy versus fluorouracil/ leucovorin chemotherapy alone in advanced colorectal cancer. J Surg Oncol. 2004;88:78–85.
Chua TC, Bester L, Saxena A, Morris DL. Radioembolization and systemic chemotherapy improves response and survival for unresectable colorectal liver metastases. J Cancer Res Clin Oncol. 2011;137(5):865–73. https://doi.org/10.1007/s00432-010-0948-y.
Sharma RA, Van Hazel GA, Morgan B, Berry DP, Blanshard K, Price D, et al. Radioembolization of liver metastases from colorectal cancer using Yttrium-90 microspheres with concomittant systemic oxaliplatin, fluorouracil, and leucovorin chemotherapy. J Clin Oncol. 2007;25(9):1099–106. https://doi.org/10.1200/JCO.2006.08.7916.
Lee G, Malietzis G, Askari A, et al. Is right-sided colon cancer different to left-sided colorectal cancer? – a systematic review. Eur J Surg Oncol. 2015;41(3):300–8.
Modest DP, Stintzing S, von Weikerstal LF, et al. Exploring the effect of primary tumor sidedness on therapeutic efficacy across treatment lines in patients with metastatic colorectalcancer: analysis of FIRE-3 (AIOKRK0306). Oncotarget. 2017;8(62):105749–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective study was approved by Institutional Ethical Commission Review Board.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Türk, G., Eldem, G., Kılıçkap, S. et al. Outcomes of Radioembolization in Patients with Chemorefractory Colorectal Cancer Liver Metastasis: a Single-Center Experience. J Gastrointest Canc 50, 236–243 (2019). https://doi.org/10.1007/s12029-018-0053-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-018-0053-z