Abstract
Purpose
The aim of this study was to analyze the safety, treatment characteristics and survival outcomes of Yttrium-90 (Y90) radioembolization for unresectable colorectal carcinoma (CRC) liver metastases refractory to standard of care therapy.
Methods
A total of 214 patients with CRC metastases were treated with Y90 radioembolization over 12 years. Toxicity was assessed using National Cancer Institute common terminology criteria. Overall survival was analyzed from date of diagnosis of primary cancer, hepatic metastases and from the first Y90. Uni/multivariate analyses were performed. Substratification by era of chemotherapeutics was performed.
Results
Most patients were male (60 %) and <65 years old (61 %). Of them, 98 % had been exposed to chemotherapy. Grade 3 lymphocyte, bilirubin, albumin, ALP and AST toxicities were observed in 39 %, 11 %, 10 %, 8 % and 4 % of patients, respectively. Grade 4 lymphocyte and ALP toxicities were observed in 5 % and 3 % of patients, respectively. Median overall survival was 43.0, 34.6, and 10.6 months from date of diagnosis of primary cancer, hepatic metastases and first Y90, respectively. Survival was significantly longer in patients: (1) who received ≤2 cytotoxic drugs (n = 104) than those who received 3 (n = 110) (15.2 vs. 7.5 months, p = 0.0001); and (2) who received no biologic agents (n = 52) compared with those that did (n = 162) (18.6 vs. 9.4 months, p = 0.0001). Multivariate analyses identified ≤2 cytotoxic agents, no exposure to biologics, ECOG 0, tumor burden <25 %, lack of extrahepatic disease and albumin >3 g/dL as independent predictors of survival.
Conclusion
In this largest metastatic CRC series published to date, Y90 radioembolization was found to be safe; survival varied by prior therapy. Further studies are required to further refine the role of Y90 in metastatic CRC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common malignancy in the United States. It is also the third most common cause of cancer-related mortality. According to the National Cancer Institute, 141,210 new cases were diagnosed in 2011. Standard of care treatment includes surgery followed by systemic agents to prevent local recurrence and treat extra-intestinal disease, or surgical treatment for resectable metastases. Up to 60% of patients with CRC develop liver metastases [1]. About one-third of patients have hepatic metastatic disease at diagnosis and half of those with early disease develop metastases after resection [2]. Overall 5-year survival after distant metastases have been discovered is 11.7%. Resection is limited by the number, location, burden of hepatic lesions as well as hepatic function, extrahepatic disease, medical comorbidities, and is a therapeutic option for 20% of patients [3]. Five-year survival rate after surgical resection of liver-confined disease is 35% [4]. Substantial progress has been made in the development of systemic agents to improve survival outcomes in patients with CRC; median overall survival now varies from 15 to 22 months [5–7]. The introduction of molecular targeted biologic agents has also generated improvements in survival [5, 8, 9].
Unresectable hepatic metastases remain an important cause of morbidity and mortality in CRC [10, 11]. The last decade has seen substantial progress in the development of locoregional therapies such as hepatic artery infusion, chemoembolization and radioembolization. Outcomes of these therapies have been very encouraging. Y90 radioembolization has gained widespread recognition for the treatment of hepatocellular carcinoma as well as liver metastases [7, 12–19]. This study aims at analyzing safety and pretreatment variables that affect survival following radioembolization. Given the rapid development of systemic treatments for CRC, we also sought to analyze the effect of pre-Y90 systemic therapy on survival after diagnosis of the primary disease and hepatic metastases and from treatment with Y90. The intent was to explore the effect of Y90 timing on survival in the face of multiple lines of available systemic therapy as part of the continuum of care.
Methods
Patient cohort
Between November 2001 and January 2013, 214 patients with liver-dominant hepatic colorectal metastases were treated with Y90 radioembolization. The study was approved by Institutional Review Board and was Health Insurance Portability and Accountability Act compliant. This report also complies with the research reporting standards for radioembolization [13]. This study represents a report of prospectively collected data at a large, comprehensive cancer center with significant expertise in locoregional therapies. Study inclusion criteria included: (1) unresectable metastases from colorectal cancer (assessed at weekly gastrointestinal tumor board); (2) progressive disease confirmed on imaging refractory to previous systemic/locoregional therapy; (3) ECOG status ≤2; (4) ability to undergo angiography and selective visceral catheterization; and (5) adequate hematology (granulocyte count ≥1.5 × 109 /L, platelets ≥50 × 109 /L), renal function (creatinine ≤2.0 mg/dL) and liver function (bilirubin ≤2.0 mg/dL). Exclusion criteria included: (1) significant extrahepatic disease (life expectancy <3 months); (2) evidence of uncorrectable gastrointestinal flow observed on angiography or 99mTc-Macroaggregated albumin (MAA) scans; (3) estimated lung dose >30 Gy in a single session; and (4) concurrent chemotherapy or radiotherapy.
Patient evaluation and workup
All patients underwent history and physical examinations, baseline laboratory tests and radiological imaging within 1 month of treatment. This imaging information was used to determine baseline imaging characteristics including tumor burden, uni/multifocality and presence/absence of extrahepatic metastases. Pretreatment angiography was performed to determine proper catheter position and identify any collateral flow to the gastrointestinal tract (GI) [20–24]. Prophylactic embolization of aberrant vessels was performed when appropriate. 99mTc-MAA scan was performed to detect GI flow and lung shunt fraction [21].
Treatment plan
The decision to treat patients with Y90 was determined by a multidisciplinary team of medical/surgical oncologists and interventional radiologists during gastrointestinal tumor board. All radioembolization procedures were performed with a glass-based Y90 device (BTG, Canada). This device is currently approved for patients with hepatocellular carcinoma in the United States and liver neoplasia (worldwide) [25]. The method for determining injected activity (to obtain 120 Gy dose) has been published previously [13, 21, 26, 27]. All patients received Y90 therapy via a lobar arterial approach; the other lobe (when necessary) was subsequently treated after 1–2 months.
All procedures were performed on an outpatient basis. Baseline laboratory values were obtained on treatment day. Additional treatments were performed for treatment completion or for progression in treated disease after response assessment at regular clinic visits.
Data collection and clinical follow-up
All patients were evaluated for adverse events 4 weeks post treatment, and subsequently at 2–3 month intervals. The last patient was enrolled in January 2013. Data were closed on April 30, 2013. Patients were followed until death or censored to the last clinic follow-up.
Toxicity analysis
Clinical and laboratory adverse events were recorded using National Cancer Institute common terminology criteria v3.0 during scheduled clinic visits. Laboratory and clinical toxicities exhibited anytime during follow-up are reported herein (no 30-day cut-off).
Overall survival
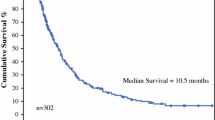
All 214 patients were available to calculate overall survival (Kaplan-Meier) and the effect of different baseline variables on survival [28]. Overall survival (OS) was calculated from the day of diagnosis of primary cancer, date of diagnosis of hepatic metastases and from first Y90 treatment. In order to further dissect the cohort, subgroup survival analyses were performed to assess the effect of factors such as previous cytotoxic (oxaliplatin, irinotecan, 5FU) and/or biologic agents (bevacizumab, cetuximab, panitumumab). Furthermore, to analyze the effect of trends in patient selection for Y90 treatment on survival (salvage vs. 1st or 2nd line), survival was analyzed based on the era of first Y90 treatment (<2004 vs. >2004). We chose the cut-off of 2004 because it coincided with the introduction of biologic agents. Median time from diagnosis of hepatic metastases to first Y90 was also analyzed to explore if earlier treatment with Y90 led to better survival outcomes, or if there was a trend for longer time to Y90 treatment with the development of new agents.
Uni/multivariate analyses
Uni/multivariate analyses were performed using Cox proportional hazards model. Variables entered in the univariate analyses included demographics (gender, age), performance status (ECOG), previous therapy (cytotoxic and biologic agents), tumor characteristics (stage at diagnosis, burden, distribution and extrahepatic disease) and liver function (albumin, bilirubin). Variables with p ≤ 0.25 by univariate analysis were included in the multivariate model. Hazard ratio estimates were based on simultaneous analysis of all variables. Assumption of proportionality was tested using log-minus-log plot and was met. Type I error of multiple comparisons on univariate analyses were corrected using Bonferroni methodology [29, 30]. All analyses were performed using SAS 9.2 (Cary, NC); p < 0.05 was considered significant.
Results
Baseline characteristics
Table 1 summarizes the baseline characteristics. Most patients were <65 (61%) years old, male (60%), had multifocal/bilobar disease (90%/83%) with ≤25% (81%) tumor burden. Fifty-eight percent had liver-only disease; 42% had limited extrahepatic disease (lungs, bones, lymph nodes, peritoneum, adrenals). Twenty-two percent had previously received local therapies. All (except 5 patients) received standard therapy before Y90 (Fig. 1). Forty-eight percent of patients had received ≤2 cytotoxic drugs, while 52% of patients received three cytotoxic agents. Twenty-four percent of patients received no biologic agent; 76% received at least one biologic agent. Combining cytotoxic/biologic agents, 14, 35, 60, 57 and 43 patients received 1, 2, 3, 4 and 5 regimens, respectively, while 22% had previous liver-directed therapy.
Y90 dosimetry
Two-hundred fourteen patients received a total of 381 treatment sessions (mean 1.8, range 1–3 per patient). The rate of prophylactic coil embolization was <10%; these were most commonly the right gastric, falciform and other gastric arterial variants (rarely gastroduodenal). Median activity infused was 2.35 GBq (range 0.6–10), median radiation dose was 122 Gy (range 83-157) and 4.5 Gy (range 0.1-29.8) to the liver and lungs, respectively. Dosage infused was >98% in all cases (no stasis observed).
Toxicities
Table 2 summarizes treatment toxicities. Grade 1 and 2 clinical toxicities included fatigue (50%), pain (26%), nausea (15%), vomiting/fever (5%), anorexia (4%) and abdominal discomfort/diarrhea (2%); there were no grade 3–4 clinical toxicities. Grade 3 absolute lymphocyte, bilirubin, albumin, ALP and AST toxicities were observed in 39%, 11%, 10%, 8% and 4% patients, respectively. Grade 4 absolute lymphocyte and ALP toxicities were observed in 5% and 3% of patients, respectively. No patient experienced grade 4 ALT, AST, albumin/bilirubin toxicity or gastrointestinal ulceration. No patient experienced radioembolization-induced liver disease or pneumonitis. There were no treatment-related deaths.
Overall survival
Survival outcomes are summarized in Table 3. One hundred fifty three of 214 patients had died at the time of the analysis. Median OS was 43.0 months (95% CI 39.0–47.0) from diagnosis of primary tumor, 34.6 months (95% CI 28.0–42.0) from diagnosis of hepatic metastases, and 10.6 months (95% CI 8.5–15.0) from first Y90. Median time from the diagnosis of hepatic metastases to first Y90 was 21.4 months (95% CI 18.0–22.0). OS from first Y90 was significantly longer for patients who received ≤2 cytotoxic agents vs. all three before Y90 (15.2 vs. 7.5 months, p = 0.0001); however, survival from diagnosis of primary cancer and liver metastases was not affected by previous exposure to cytotoxic drugs. Median time from diagnosis of hepatic metastases to first Y90 was shorter when receiving ≤2 drugs vs. all 3 (13.9 vs. 27.5 months, p < 0.0001). Survival from first Y90 was longer for patients naïve of biologic agent vs. those receiving at least one before Y90 (18.6 vs. 9.4 months, p = 0.0001). OS from diagnosis of primary cancer and liver metastases was not affected by previous exposure to biologic agents. Time from metastases to first Y90 was shorter for patients naïve of biologic agents (12.6 vs. 24.4 months, p < 0.0001). Analyzed by era, survival was significantly longer for patients treated prior to vs. after 2004 (18.7 vs. 10.6 months, p = 0.0086); however, as seen above, survival from diagnosis of primary cancer and liver metastases was not affected by the era of Y90. Again, median time from diagnosis of hepatic metastases to first Y90 was significantly shorter for patients treated prior to 2004 (13.0 vs. 22.1 months, p = 0.0003).
Uni/multivariate analyses
Table 4 summarizes uni/multivariate analyses. Better survival outcomes were predicted by ≤2 cytotoxic agents (p = 0.0001), no exposure to biologic agents (p = 0.0001), stage ≤2 at diagnosis (p = 0.043), performance status 0 (p < 0.0001), tumor burden ≤25% (p < 0.0001), unilobar (p = 0.017) and no extrahepatic disease (p < 0.0001), albumin >3 g/dL (p < 0.0001) and bilirubin ≤1.3 mg/dL (p = 0.006). On multivariate analyses, exposure to ≤2 cytotoxic agents (HR 0.67; 95% CI 0.46–0.98), no exposure to biologic agents (HR 0.56; 95% CI 0.36–0.88), performance status 0 (HR 0.34; 95% CI 0.22–0.53), no extrahepatic disease (HR 0.58; 95% CI 0.41–0.83) and albumin >3 g/dL (HR 0.51; 95% CI 0.35–0.76) independently predicted better survival outcomes.
Discussion
The majority of patients with CRC develop hepatic metastases. Unfortunately, only a minority are suitable for resection or ablation. Therefore, hepatic metastases from unresectable CRC pose a serious challenge in terms of improving survival outcomes. Standard of care employs systemic therapy with FOLFOX/FOLIFRI +/- biologic agents. In the salvage setting, systemic agents have led to survival benefits over best supportive care, showing OS of 6.4 months (regorafenib), 6.1 months (cetuximab) and 9.0 months (panitumumab) [31–33]. However, once disease progresses, the outcomes are not very encouraging. In addition, the high rate of clinical adverse events and molecular mechanisms of resistance to systemic biologics makes these therapies less beneficial to certain patient subpopulations [34].
Locoregional transarterial therapies have emerged as therapeutic options for unresectable colorectal metastases refractory to systemic agents. In particular, Y90 has led to promising response rates, improved survival, time-to-progression outcomes and an acceptable toxicity profile [7, 17, 18, 35]. Other studies have combined Y90 with systemic agents and have found the combination is well-tolerated with encouraging outcomes [36, 37]. In this study, we primarily investigated survival outcomes in patients with hepatic colorectal metastases refractory to previous local/systemic therapy. Our results suggest that radioembolization is a safe treatment option for these patients. Since most patients had received some form of systemic or local therapy, radioembolization was primarily done in the salvage setting. These results corroborate previous studies; current phase 3 studies combining systemic chemotherapy with radioembolization for first or second line treatment may lead to a paradigm shift that abandons lines of therapy and focuses on individualizing therapeutic options according to disease characteristics [6, 7].
Y90 is administered via a trans-arterial catheter into the hepatic artery or its branches supplying tumor. The therapeutic advantage is based on the dual blood supply of the liver where tumors primarily dwell on hepatic arterial blood and normal hepatic parenchyma thrives on portal venous blood [38, 39]. This fact is exploited during radioembolization where highly focused radiation is directed towards the hypervascular tumor, relatively sparing the normal parenchyma [40]. Consequently, most of the clinical toxicities observed in this cohort were transient and controlled symptomatically without requiring hospitalization. Grade 3–4 laboratory toxicities were limited and compare favorably with other cohort studies, confirming the safety of this treatment (no gastrointestinal ulcers).
Overall survival from the diagnosis of primary cancer and hepatic metastases were 43.0 and 34.6 months, respectively. The 10.6 months OS from first Y90 treatment is in line with recent reports and is promising given that 42% of patients had extrahepatic disease in the salvage setting [17, 35, 41]. These results are competitive with those achieved by existing salvage systemic agents and supports the concept that radioembolization should be considered for patients early after second line failure. Median time from diagnosis of hepatic metastases to first Y90 was 21.4 months, accurately representing the time when patients were receiving varying systemic agents. When survival outcomes were analyzed by previous exposure to cytotoxic agents, we found that patients who received ≤2 of these agents exhibited better post-Y90 survival outcomes than those who received all three drugs (possible lead time bias). Given the adverse effects of chemotherapeutic agents, if patients receive Y90 early in the course of disease, survival outcomes are encouraging and incidence of adverse effects could be potentially lowered. However, overall survival from the diagnosis of primary cancer and hepatic metastases was not different whether patients received Y90 after being exposed to ≤2 agents or all 3. Time from diagnosis of hepatic metastases was significantly shorter for those patients who received ≤2 agents. This potentially indicates the reason for longer survival for patients who received ≤2 agents was in part due to earlier treatment with Y90 (13.9 vs. 27.5 months). Similar findings were observed when survival was analyzed by previous exposure to biologic agents. Longer post-Y90 survival, similar survival times from the diagnosis of primary and from hepatic metastases, and significantly shorter time-to-Y90 were observed in patients who received no biologic agent. This again indicates that longer post-Y90 survival was potentially due to Y90 early in the course of disease.
Survival was also analyzed by era of Y90. We chose the cut-off of 2004 since it coincided with the clinical introduction of biologic agents. We found that patients treated with Y90 up to 2004 had significantly longer post-Y90 survival and shorter time-to-Y90, in line with the observations discussed above. This indicates that up to 2004, patients were treated with Y90 early in the course of disease whereas after 2004, patients transitioned to being more heavily pre-treated with systemic agents prior to consideration of Y90. These observations indicate that although an earlier treatment with Y90 may not prolong OS; it may be considered earlier in the disease course either alone after failure of systemic agents, during a chemotherapy holiday, or in combination with systemic agents. Current phase III trials are evaluating Y90 in combination with standard of care systemic for both first and second line patients with metastatic CRC.
The results of uni/multivariate analyses offer insight in predicting OS. Interestingly, tumor stage ≤2 at the time of diagnosis of primary cancer predicted improved post-Y90 survival, reflecting better tumor biology. However, stage was not found to be a significant factor on multivariate analysis. Performance status and liver function were significant predictors of survival on both univariate and multivariate analyses. The presence of extrahepatic disease was also associated with worse outcomes. Bilobar disease also trended towards worse OS but was not found significant on multivariate analysis. Finally, exposure to ≤2 agents and no previous biologic were associated with significantly better survival on both univariate and multivariate analyses, similar to recent reports in heavily treated patients [42].
The study has limitations. First, this is a single center experience with significant expertise in Y90. All comparisons and subgroup analyses were performed on baseline characteristics before Y90. Ideally, they could have been performed on the basis of patient characteristics when the decisions were made to treat patients with 2, 3 or more lines of systemic agents vs. Y90. It is possible that patients who received all 3 cytotoxic agents had more advanced disease (higher hepatic and extrahepatic disease burden) than those who received ≤2 agents. Lead time bias confounding survival analyses is also possible.
There are strengths. This is the largest series of Y90-treated colorectal liver metastases reported to date, with comprehensive mature follow-up and important granularity of detail in terms of prior exposure to systemic agents stratified by era. The study was initiated years after introduction of this device; the methodology was well-established with no technical learning curve. Toxicities were reported at any time during follow-up, eliminating the artificial 30-day cutoff often seen in oncology studies as well as potential biases of toxicity attribution to the treatment. Despite being heavily pre-treated, survival outcomes were promising. Finally, responder versus non-responder analysis was purposefully not performed given its flawed nature, inherent guarantee-time bias and limited pre-treatment clinical utility.
Conclusion
Y90 radioembolization for hepatic colorectal metastases is safe and leads to encouraging survival outcomes. Survival was longer for patients who had received ≤2 cytotoxic agents, no biologic agents and were treated earlier in the course of disease. Survival was also affected by performance status, liver function, and presence/absence of extrahepatic disease. This study supports the role of Y90 radioembolization in the multimodality treatment of patients with hepatic colorectal metastases who have limited therapeutic options. Current randomized phase 3 studies are evaluating Y90 in combination with systemic therapy for first and second line treatment.
References
Sasson AR, Sigurdson ER. Surgical treatment of liver metastases. Semin Oncol. 2002;29:107–18.
Macdonald J. Adjuvant therapy of colon cancer. CA Cancer J Clin. 1999;49:202–19.
Bentrem DJ, Dematteo RP, Blumgart LH. Surgical therapy for metastatic disease to the liver. Annu Rev Med. 2005;56:139–56. doi:10.1146/annurev.med.56.082103.104630.
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80. doi:10.1200/JCO.2007.11.0833.
Albert M, Kiefer MV, Sun W, Haller D, Fraker DL, Tuite CM, et al. Chemoembolization of colorectal liver metastases with cisplatin, doxorubicin, mitomycin C, ethiodol, and polyvinyl alcohol. Cancer. 2011;117:343–52. doi:10.1002/cncr.25387.
Goldberg RM, Rothenberg ML, Van Cutsem E, Benson 3rd AB, Blanke CD, Diasio RB, et al. The continuum of care: a paradigm for the management of metastatic colorectal cancer. Oncologist. 2007;12:38–50. doi:10.1634/theoncologist.12-1-38.
Mulcahy MF, Lewandowski RJ, Ibrahim SM, Sato KT, Ryu RK, Atassi B, et al. Radioembolization of colorectal hepatic metastases using yttrium-90 microspheres. Cancer. 2009;115:1849–58.
Giantonio BJ, Catalano PJ, Meropol NJ, O'Dwyer PJ, Mitchell EP, Alberts SR, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25:1539–44. doi:10.1200/JCO.2006.09.6305.
Emmanouilides C, Sfakiotaki G, Androulakis N, Kalbakis K, Christophylakis C, Kalykaki A, et al. Front-line bevacizumab in combination with oxaliplatin, leucovorin and 5-fluorouracil (FOLFOX) in patients with metastatic colorectal cancer: a multicenter phase II study. BMC Cancer. 2007;7:91. doi:10.1186/1471-2407-7-91.
Bengtsson G, Carlsson G, Hafstrom L, Jonsson PE. Natural history of patients with untreated liver metastases from colorectal cancer. Am J Surg. 1981;141:586–9.
Wagner JS, Adson MA, Van Heerden JA, Adson MH, Ilstrup DM. The natural history of hepatic metastases from colorectal cancer. A comparison with resective treatment. Ann Surg. 1984;199:502–8.
Salem R, Lewandowski RJ, Kulik L, Wang E, Riaz A, Ryu RK, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140:497–507 e2. doi:10.1053/j.gastro.2010.10.049.
Salem R, Lewandowski RJ, Gates VL, Nutting CW, Murthy R, Rose SC, et al. Research reporting standards for radioembolization of hepatic malignancies. J Vasc Interv Radiol. 2011;22:265–78. doi:10.1016/j.jvir.2010.10.029.
Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, et al. Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010;138:52–64. doi:10.1053/j.gastro.2009.09.006.
Bangash AK, Atassi B, Kaklamani V, Rhee TK, Yu M, Lewandowski RJ, et al. 90Y radioembolization of metastatic breast cancer to the liver: toxicity, imaging response, survival. J Vasc Interv Radiol. 2007;18:621–8.
Kennedy AS, Dezarn WA, McNeillie P, Coldwell D, Nutting C, Carter D, et al. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol. 2008;31:271–9.
Jakobs TF, Hoffmann RT, Dehm K, Trumm C, Stemmler HJ, Tatsch K, et al. Hepatic yttrium-90 radioembolization of chemotherapy-refractory colorectal cancer liver metastases. J Vasc Interv Radiol. 2008;19:1187–95. doi:10.1016/j.jvir.2008.05.013.
Kennedy AS, Coldwell D, Nutting C, Murthy R, Wertman Jr DE, Loehr SP, et al. Resin 90Y-microsphere brachytherapy for unresectable colorectal liver metastases: modern USA experience. Int J Radiat Oncol Biol Phys. 2006;65:412–25.
Gates VL, Marshall KG, Salzig K, Williams M, Lewandowski RJ, Salem R. Outpatient single-session yttrium-90 glass microsphere radioembolization. J Vasc Interv Radiol. 2014;25:266–70. doi:10.1016/j.jvir.2013.11.005.
Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Nemcek Jr AA, Kulik L, et al. Radioembolization with (90)y microspheres: angiographic and technical considerations. Cardiovasc Intervent Radiol. 2007;30:571–92.
Salem R, Thurston KG. Radioembolization with 90Yttrium microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 1: Technical and methodologic considerations. J Vasc Interv Radiol. 2006;17:1251–78.
Salem R, Thurston KG. Radioembolization with 90yttrium microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 2: special topics. J Vasc Interv Radiol. 2006;17:1425–39.
Salem R, Thurston KG. Radioembolization with yttrium-90 microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies: part 3: comprehensive literature review and future direction. J Vasc Interv Radiol. 2006;17:1571–93.
Salem R, Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Ibrahim S, et al. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol. 2007;10:12–29.
Salem R, Thurston KG, Carr BI, Goin JE, Geschwind JF. Yttrium-90 microspheres: radiation therapy for unresectable liver cancer. J Vasc Interv Radiol. 2002;13:S223–9.
Ho S, Lau WY, Leung TW, Chan M, Johnson PJ, Li AK. Clinical evaluation of the partition model for estimating radiation doses from yttrium-90 microspheres in the treatment of hepatic cancer. Eur J Nucl Med. 1997;24:293–8.
Lau WY, Ho S, Leung TW, Chan M, Ho R, Johnson PJ, et al. Selective internal radiation therapy for nonresectable hepatocellular carcinoma with intraarterial infusion of 90yttrium microspheres. Int J Radiat Oncol Biol Phys. 1998;40:583–92.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
Gyorffy B, Gyorffy A. Tulassay Z [The problem of multiple testing and solutions for genome-wide studies]. Orv Hetil. 2005;146:559–63.
Cleophas TJ, Zwinderman AH. Clinical trials are often false positive: a review of simple methods to control this problem. Curr Clin Pharmacol. 2006;1:1–4.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12. doi:10.1016/S0140-6736(12)61900-X.
Jonker DJ, O'Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357:2040–8.
Hecht JR, Patnaik A, Berlin J, Venook A, Malik I, Tchekmedyian S, et al. Panitumumab monotherapy in patients with previously treated metastatic colorectal cancer. Cancer. 2007;110:980–8. doi:10.1002/cncr.22915.
Bardelli A, Siena S. Molecular mechanisms of resistance to cetuximab and panitumumab in colorectal cancer. J Clin Oncol. 2010;28:1254–61. doi:10.1200/JCO.2009.24.6116.
Benson 3rd AB, Geschwind JF, Mulcahy MF, Rilling W, Siskin G, Wiseman G, et al. Radioembolisation for liver metastases: results from a prospective 151 patient multi-institutional phase II study. Eur J Cancer. 2013;49:3122–30. doi:10.1016/j.ejca.2013.05.012.
Sharma RA, Van Hazel GA, Morgan B, Berry DP, Blanshard K, Price D, et al. Radioembolization of liver metastases from colorectal cancer using yttrium-90 microspheres with concomitant systemic oxaliplatin, fluorouracil, and leucovorin chemotherapy. J Clin Oncol. 2007;25:1099–106.
Hendlisz A, Van den Eynde M, Peeters M, Maleux G, Lambert B, Vannoote J, et al. Phase III trial comparing protracted intravenous fluorouracil infusion alone or with yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol. 2010;28:3687–94. doi:10.1200/JCO.2010.28.5643.
Breedis C, Young G. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30:969–77.
Ackerman NB, Lien WM, Silverman NA. The blood supply of experimental liver metastases. 3. The effects of acute ligation of the hepatic artery or portal vein. Surgery. 1972;71:636–41.
Kennedy A, Nag S, Salem R, Murthy R, McEwan AJ, Nutting C, et al. Recommendations for radioembolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the radioembolization brachytherapy oncology consortium. Int J Radiat Oncol Biol Phys. 2007;68:13–23.
Evans KA, Richardson MG, Pavlakis N, Morris DL, Liauw W, Bester L. Survival outcomes of a salvage patient population after radioembolization of hepatic metastases with yttrium-90 microspheres. J Vasc Interv Radiol. 2010;21:1521–6. doi:10.1016/j.jvir.2010.06.018.
Sofocleous CT, Garcia AR, Pandit-Taskar N, Do KG, Brody LA, Petre EN, et al. Phase I trial of selective internal radiation therapy for chemorefractory colorectal cancer liver metastases progressing after hepatic arterial pump and systemic chemotherapy. Clin Colorectal Cancer. 2014;13:27–36. doi:10.1016/j.clcc.2013.11.010.
Role of funding
There was no funding provided for this study.
Conflict of interest
RJL, MFM, ABB, and RS are advisors to BTG. None of the other authors have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lewandowski, R.J., Memon, K., Mulcahy, M.F. et al. Twelve-year experience of radioembolization for colorectal hepatic metastases in 214 patients: survival by era and chemotherapy. Eur J Nucl Med Mol Imaging 41, 1861–1869 (2014). https://doi.org/10.1007/s00259-014-2799-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2799-2