Abstract
Purpose of Review
Review the role of coronary artery calcium (CAC) testing in designing future clinical trials in primary prevention.
Recent Findings
While there are numerous new agents that have been found to lower cardiovascular event rates in clinical trials, these studies have required a large sample size, in part due to low event rates as well as improved baseline treatments. More precise risk assessment could allow for better identification of individuals who stand to derive the most benefit from various therapies. Coronary CAC testing offers a simple method for identifying high-risk primary prevention cohorts, and thus may allow for improved efficiency of clinical trials, enhanced efficacy of various therapies, and ultimately more favorable cost-effectiveness estimates.
Summary
The use of CAC testing as part of the inclusion criteria used in clinical trials may result in identifying high-risk individuals who were previously not included in such studies while achieving favorable absolute risk reductions. The advantages afforded by using CAC to enrich clinical trials offer a potential road map for future clinical trials in primary prevention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction: the Current Challenge
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality globally and in the USA [1]. Despite increasing options for treating individuals with known or suspected cardiovascular disease, direct and indirect costs related to cardiovascular care continue to increase [2, 3]. The combined effect of an increased prevalence of cardiovascular disease (CVD) and rising costs has led to a need to develop more effective strategies for preventing CVD and identifying individuals who would derive the most benefit from intense primary prevention efforts. In the past, investigators proposed a trial-based approach for primary prevention [4, 5], where the inclusion criteria used for various trials would determine which patients benefit from preventive therapies. While this approach has demonstrated efficacy among higher-risk patients (trials using mostly a secondary prevention population), most individuals eligible for treatment have a low absolute risk of cardiovascular events questioning the net benefit of treatment [6]. The challenge remains in designing clinical trials in a patient population where the risk of future events is heterogenous, even among those deemed to be of higher risk.
Furthermore, while statin use has become more common, additional novel therapies are often used as an adjunct to the current standard of care therapies, and the incremental benefit of such treatments may be low. As a result, many contemporary trials have a large sample size, require long-term follow-up, and have lower efficacy than anticipated. A clinical trial yielding small absolute risk reduction is unfavorable in a healthcare system focused on value, even if the therapy results in a beneficial outcome [7••, 8].
Why Coronary Artery Calcium (CAC) Testing?
The detection of coronary atherosclerosis has been shown to result in improved risk assessment when compared to various blood biomarkers and clinical risk scores [9].
CAC testing offers an inexpensive and simple method to identify the presence and amount of plaque and is a powerful predictor of future cardiac events [10,11,12,13,14]. Importantly, the absence of CAC ( calcium score of zero) has been found to be a robust negative risk factor in primary prevention and is currently the most definitive predictor of low risk [14,15,16,17,18]. CAC’s value as a powerful predictive tool has been demonstrated in both young and elderly patient populations [13, 19,20,21]. CAC scoring requires minimal expertise and does not require contrast, thus making it easy to use across multiple sites. With current technologies, CAC testing is associated with radiation exposures as low as 1.0 millisievert per study [22].
Enriching Clinical Trials Through CAC Testing
In the realm of primary prevention clinical trials, the challenge remains to efficiently identify high-risk populations that will have a sufficiently high absolute event rate that there will be a favorable absolute risk reduction. Relying on estimations of risk based on age or clinical risk factors makes it challenging to separate low-risk patients from high-risk patients [15]. CAC testing can enrich clinical trials by having inclusion criteria that are based on a single CAC score threshold (e.g., CAC > 300) or a CAC score threshold combined with risk factors to identify patients at the desired risk of cardiovascular disease (CVD) events. Such an approach can reduce risk heterogeneity and provide a more refined risk assessment.
A recent proof of concept study using data from the Multi-Ethnic Study of Atherosclerosis cohort explored the implications a CAC-based enrichment strategy would have on a hypothetical primary prevention trial [23•]. Cainzos-Achirica et al. [23•] demonstrated that a higher CAC burden is associated with a more significant 5-year incidence of CVD events and consistently identified participants that would derive the most considerable absolute benefit from a hypothetical add-on therapy. A comparison of the sample size utilizing a CAC score as an entry criterion instead of the estimated ASCVD risk demonstrated that a CAC score threshold of > 400 yielded the smallest estimated sample size (33 to 57% smaller assuming a 15% RRR of the hypothetical add-on therapy). Furthermore, the combination of a 10-year ASCVD risk above the 7.5% threshold with a CAC score enrichment criteria (CAC score > 100 or > 400) yielded the lowest cost in terms of included participants and screening ($296.1 million vs. $623.4 million) [24]. While there is a possible downside of restricting potentially benefiting therapies to a higher-risk cohort using CAC-based inclusion criteria, this concern should be balanced against the improved efficiency, lower cost, and higher potential value of therapies that may otherwise have lower efficacy. It is noteworthy that any clinical trial using CAC testing for patient enrichment does not need to mandate such testing in all patients. For example, some trials can have various potential criteria for trial entry, with CAC testing representing one possible approach. Other approaches could be based on a combination of clinical data, and blood biomarkers or findings from other available invasive or non-invasive tests, which if appropriately utilized, could identify patients with a similar risk profile.
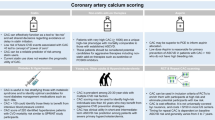
Figure 1 provides a schematic illustration of the rationale for CAC testing to enhance clinical trials. Ideally, clinical trials should focus on selecting patients who are most likely to benefit from investigational treatments while avoiding excess costs associated with treating those who derive the least benefit. Such a design would be particularly useful in a setting of limited resources and could have a significant impact on the overall cost of preventive care [25].
Rationale for coronary artery calcium (CAC) testing in clinical trials. CAC testing is a simple, and reproducible test. Its advantages include an ability to identify higher-risk patients and safely exclude low-risk patients. Selecting higher-risk patients based on CAC testing at the time of enrollment would result in lowering the sample size, shorter follow-up, and lower number needed to treat. If a treatment is proven to be effective based on its greater absolute risk reduction at a lower cost, then the trial is also more likely to be cost-effective. The improved cost-effectiveness could result in increased adoption by payors and healthcare systems
Lessons from Current and Past Clinical Trials
Table 1 summarizes CAC’s use in past, present, and future clinical trials [26,27,28,29,30,31,32,33]. Lessons learned from these experiences emphasize the importance of selecting the right sample size, adequate follow-up duration, and reliably identifying individuals who will derive clinical benefit from the growing ubiquity of aggressive medical therapies. Recent experience utilizing CAC score as part of the enrollment criteria in a CVD risk reduction trial has demonstrated that it is possible to achieve manageable sample sizes yielding favorable absolute risk reductions within a reasonable follow-up [30]. Future experiences may provide further insight into how CAC can help guide additional therapies in patients at high CVD risk [32], as an adjunct to global risk factor algorithms [29], or as the direct determinant of ASCVD risk to guide initiation of preventive therapy [7••, 31].
Is There a Way Forward?
The advantages afforded by the use of CAC to enrich clinical trials offer a potential road map for future clinical trials in primary prevention (Fig. 2). CAC testing can be used to assess the efficacy of multiple novel therapies in a primary prevention population deemed to be at the highest risk for future events (e.g., CAC score of > 300). Importantly, the value of CAC testing may be greatest when evaluating therapies which are expensive or when there is concern regarding potential risk.
How can CAC be used in future clinical trials? CAC testing can be used in industry-funded clinical trials to assess the efficacy of established therapies for ASCVD in a high-risk primary prevention cohort without a history of prior CVD events. Novel therapies for aggressive lipid-lowering or new mechanisms for lipid-lowering can also be studied in a high-risk primary prevention cohort using CAC testing. NIH-funded trials utilizing CAC testing as part of risk assessment can evaluate the impact CAC-guided preventive strategy may have among high-risk young adults as well as low-risk older adults not included in clinical trials
In terms of risk stratification, CAC provides an opportunity to focus prevention efforts on specific populations often excluded in clinical trials, including those at the extreme range of age. Among young adults, particularly women, rates of acute myocardial infarction have been increasing, yet preventive therapies are seldomly initiated prior to the development of cardiovascular events [34]. Recent observational studies suggest that the presence of CAC among young adults is a robust risk marker of future coronary heart disease events [20, 35]. Thus, while prevention trials have not been performed in very young adults (e.g., age < 40), the use of CAC testing could be used to identify a suitable population for a primary prevention clinical trial in the young [36]. Another opportunity for a clinical trial is to utilize CAC testing among older adults, where a CAC of ≤ 10 may be associated with a very low risk [19]. Clinical trials focusing on refining treatment decisions in older adults may improve treatment efficacy, reduce potential adverse effects from various therapies, and lower healthcare costs by reducing unnecessary medical expenditure.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
ViraniSalim S, Alvaro Alonso, Benjamin Emelia J, et al. Heart Disease and Stroke Statistics—2020 Update: a report from the American Heart Association. Circulation. 2020;141:e139–596.
Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44.
Dunbar SB, Khavjou OA, Bakas T, et al. Projected costs of informal caregiving for cardiovascular disease: 2015 to 2035: a policy statement from the American Heart Association. Circulation. 2018;137:e558–77.
Ridker PM, Wilson PWF. A trial-based approach to statin guidelines. JAMA. 2013;310:1123.
Ridker PM, Rose L, Cook NR. A proposal to incorporate trial data into a hybrid ACC/AHA algorithm for the allocation of statin therapy in primary prevention. J Am Coll Cardiol. 2015;65:942–8.
Bødtker Mortensen Martin, Erling Falk, Dong Li, et al. Statin trials, cardiovascular events, and coronary artery calcification. JACC Cardiovasc Imaging. 2018;11:221–30.
•• Greenland P, Michos ED, Redmond N, et al. Primary prevention trial designs using coronary imaging: a national heart, lung, and blood institute workshop. JACC Cardiovasc. Imaging. 2020. Available at: https://imaging.onlinejacc.org/content/early/2020/09/09/j.jcmg.2020.06.042. Accessed 8 Oct 2020. This study highlights the findings from the 2019 NHLBI multi-disciplinary working group reviewing the evidence and the appropriateness of further research on CAC testing and other cardiac imaging modalities for primary preventive therapies in CVD disease.
Rozanski A, Muhlestein JB, Berman DS. Primary prevention of CVD: the role of imaging trials. JACC Cardiovasc Imaging. 2017;10:304–17.
Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73:3153–67.
Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–70.
Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45.
Polonsky TS. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610.
Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J. 2012;33:2955–62.
Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2:675–88.
Khurram Nasir, Bittencourt Marcio S, Blaha Michael J, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines. J Am Coll Cardiol. 2015;66:1657–68.
Khurram N. Message for 2018 Cholesterol management guidelines update. J Am Coll Cardiol. 2018;72:3243–5.
Dzaye O, Dardari ZA, Cainzos-Achirica M, et al. Warranty period of a calcium score of zero: comprehensive analysis from the multiethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2020.
Blaha Michael J, Ron Blankstein, Khurram Nasir. Coronary artery calcium scores of zero and establishing the concept of negative risk factors∗. J Am Coll Cardiol. 2019;74:12–4.
Yano Y, O’Donnell CJ, Kuller L, et al. Association of coronary artery calcium score vs age with cardiovascular risk in older adults: an analysis of pooled population-based studies. JAMA Cardiol. 2017;2:986–94.
Carr JJ, Jacobs DR, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol. 2017;2:391–9.
Miedema MD, Dardari ZA, Nasir K, et al. Association of coronary artery calcium with long-term, cause-specific mortality among young adults. JAMA Netw Open. 2019;2:e197440.
Hecht HS, de Siqueira MEM, Cham M, et al. Low- vs. standard-dose coronary artery calcium scanning. Eur Heart J Cardiovasc Imaging. 2015;16:358–63.
• Cainzos-Achirica M, Bittencourt MS, Osei AD, et al. Coronary artery calcium to improve the efficiency of randomized controlled trials in primary cardiovascular prevention. JACC Cardiovasc Imaging. 2021;14:1005–16. Findings from this study suggest the use of CAC testing in a future randomized primary prevention trial can lower the sample size, and reduce projected costs by identifying participants with the highest risk for future cardiovascular events.
Cainzos-Achirica M. Coronary artery calcium to improve the efficiency of randomized controlled trials in primary cardiovascular prevention. Cardiovasc Imaging. 2020:12.
Faulkner E, Annemans L, Garrison L, et al. Challenges in the development and reimbursement of personalized medicine—payer and manufacturer perspectives and implications for health economics and outcomes research: a report of the ISPOR Personalized Medicine Special Interest Group. Value Health. 2012;15:1162–71.
Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study Randomized Clinical Trial. J Am Coll Cardiol. 2005;46:166–72.
O’Malley PG, Feuerstein IM, Taylor AJ. Impact of electron beam tomography, with or without case management, on motivation, behavioral change, and cardiovascular risk profile: a randomized controlled trial. JAMA. 2003;289:2215–23.
Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing: the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) Prospective Randomized Trial. J Am Coll Cardiol. 2011;57:1622–32.
Denissen SJ, van der Aalst CM, Vonder M, Oudkerk M, de Koning HJ. Impact of a cardiovascular disease risk screening result on preventive behaviour in asymptomatic participants of the ROBINSCA trial. Eur J Prev Cardiol. 2019;26:1313–22.
Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020;383:1838–47.
Marwick TH, Whitmore K, Nicholls SJ, et al. Rationale and design of a trial to personalize risk assessment in familial coronary artery disease. Am Heart J. 2018;199:22–30.
Amgen. A double-blind, randomized, placebo-controlled, multicenter study to evaluate the impact of evolocumab on major cardiovascular events in patients at high cardiovascular risk without prior myocardial infarction or stroke.clinicaltrials.gov; 2020. Available at: https://clinicaltrials.gov/ct2/show/NCT03872401. Accessed 3 Dec 2020.
Intermountain Health Care, Inc. Effectiveness of a proactive cardiovascular primary prevention strategy, with or without the use of coronary calcium screening, in preventing future major adverse cardiac events. clinicaltrials.gov; 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT03439267. Accessed 3 Dec 2020.
Singh A, Collins BL, Gupta A, et al. Cardiovascular risk and statin eligibility of young adults after an MI: partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71:292–302.
Sameer Arora, Stouffer George A, Kucharska-Newton Anna M, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–56.
Miedema MD, Nauffal VD, Singh A, Blankstein R. Statin therapy for young adults: a long-term investment worth considering. Trends Cardiovasc Med. 2020;30:48–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Dr. Khurram Nasir is on the Advisory Boards of Amgen, Novartis, and Novo Nordisk. His research is partly supported by the Jerold B. Katz Academy of Translational Research.
Dr. Blankstein has received research support from Amgen Inc. and Novartis Inc; and is on the Advisory boards of Caristo and Roivant Sciences Inc, outside the submitted work.
The other authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Evidence-Based Medicine, Clinical Trials and Their Interpretations
Rights and permissions
About this article
Cite this article
Fentanes, E., Cainzos Achirica, M., Nasir, K. et al. The Role of Coronary Artery Calcium Testing for Value-Based Clinical Trials in Primary Prevention. Curr Atheroscler Rep 23, 73 (2021). https://doi.org/10.1007/s11883-021-00969-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11883-021-00969-6