Abstract
Background
Although radical resections are recommended for the surgical management of liver hydatid disease (LHD), whether closed (CCR) or opened (OCR) cyst resections should be performed remains unclear. The aim of this study was to compare the postoperative and long-term outcomes of CCR and OCR for primary and recurrent LHD.
Materials and Methods
Medical charts of patients who underwent surgery at a single centre were retrospectively reviewed and compared with respect to major postoperative complications and recurrence rates.
Results
Seventy-nine CCRs and 37 OCRs were included. The major morbidity rates were 19% and 5% in the OCR and CCR groups, respectively (P = 0.036). In multivariate analysis, OCR (P = 0.030, OR = 5.37) and the operative time (P < 0.001, OR = 18.88) were the only independent predictors of major complications. The 5-year and 10-year recurrence rates were both 0% in the CCR group compared to 18% and 27%, respectively, in the OCR group (P < 0.001). The mean time to recurrence was 10.5 (± 8) years.
Discussion
Closed cyst resection for LHD is a safe and effective approach with a low risk of recurrence. Considering that recurrence could appear more than 10 years after surgery, follow-up of patients should be adapted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cystic echinococcosis is a parasitic disease caused by Echinococcus granulosus, in which humans are considered accidental hosts. Although liver hydatid disease (LHD) is usually a quiescent disease, rupture of the cyst in the biliary tract, peritoneal or pleural cavity or portosystemic venous system exposes patients to life-threatening complications.1 Hydatidosis represents a significant public health issue in endemic areas, causing socioeconomic losses with a current global burden estimated at 188,000 disability-adjusted life years.2 Liver hydatid disease could be definitively cured if the cyst could be removed entirely which is called radical surgery. Surgical procedures are divided into conservative approaches, including simple puncture/aspiration of the cyst, unroofing or partial cystectomies and radical resections with total cystectomy and anatomic hepatic resections, taking into account that the more conservative the approach, the lower the perioperative risk will be and the higher the recurrence rate and cavity-related complications.3,4,5 Radical treatment is often criticised for its aggressiveness for a benign disease. Nonetheless, this is the best healing procedure6. Most studies comparing conservative and radical techniques do not assess the effects of the open cyst resection (OCR) or closed cyst resection (CCR) approach, inducing a bias when reporting on the postoperative morbidity or recurrence rate.6,7,8,9 This is a different point of view of classical discussion of conservative or radical surgery although the CCR could only interest radical surgery. We did not focus on the differences between radical and conservative surgeries but on the opening fact. First described by Bourgeon in 1964,10 CCRs are proposed to limit the risk of small peritoneal seeding that occurs during the open-cyst approach, which aims to decrease liver and peritoneal recurrences, but poses the risk of uncontrolled accidental cyst rupture or important structures around the cyst. The aim of this study was to compare CCR and OCR, irrespective of the surgical approach (conservative or radical), with respect to postoperative and long-term outcomes, for primary and recurrent LHD.
Materials and Methods
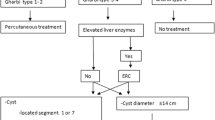
The STROBE guidelines were followed to ensure high-quality presentation of the conducted study.11 All consecutive patients who underwent surgical resection of a primary or recurrent LHD, confirmed by specimen analyses, from January 1995 to December 2017 were retrospectively identified in a prospectively maintained database after specimen analyses. Patients with both OCR and CCR during the same surgery and/or associated extrahepatic cysts were not included. Medical charts were compared according to the opened or closed resection technique, irrespective of the surgical treatment (conservative or radical). A preoperative diagnosis was performed using ultrasonography (US) or computed tomography (CT) when classical features of a hydatid cyst, according to the Gharbi’s classification, were demonstrated,12 as well as serological tests using indirect hemagglutination or ELISA.13 Magnetic resonance imaging (MRI) and endoscopic retrograde cholangiopancreatography (ERCP) were supplementary and performed for suspected biliovascular complication. The diagnosis was suspected according to the criteria established by the World Health Organization (WHO)14 and confirmed by the analysis of the surgical specimen. Since 2000, patients were administered albendazole 10–15 mg/kg preoperatively for 7 days and 1 month after according to WHO guidelines.14 Postoperative complications were defined by the Dindo-Clavien classification15 and serious postoperative complication were defined by III-IV-V event of this classification. The primary endpoint was the occurrence of serious postoperative complications. Secondary endpoints were the onset of accidental cyst rupture during CCR and recurrence of LHD. The study was approved by the Institutional Review Board of Aix-Marseille University.
Surgical Technique
All patients, except one (laparoscopy), underwent a right (± left) subcostal incision with upper midline extension. The procedures began with a thorough examination of the abdominal cavity. Cholangiography was performed in the case of biliocystic communication (BCC) or when anatomical variation was suspected on the preoperative workup. The resection technique, i.e. OCR or CCR, was selected at the surgeon’s discretion (Figs. 1 and 2). Total cystectomies were carried out by removing the cyst, and the dissection was conducted most often in contact with the cyst. Parenchymal transection was performed using the clamp-crush technique or ultrasonic dissection during intermittent vascular inflow occlusion using the Pringle manoeuvre and intermittent occlusion of the inferior cava vein when necessary. Conservative strategies (partial cystectomies and unroofing) were limited only to lesions involving major biliovascular elements whose resection was judged too deleterious considering the benign nature of the disease (Fig. 2). Preference between cystectomy and anatomic resection depended on what was considered to be the simplest by the surgical team. OCRs were conducted as follows: (i) protection of the areas around the cyst by scolex-killer solution (10% hydrogen peroxide solution or hypertonic solution)-soaked packs; (ii) hermetic aspiration of the cyst content; (iii) large opening of the cyst roof and sterilisation by injection without pressure of a scolex-killer solution to avoid embolism accidents; (iv) reaspiration of the solution and resection. Treatment of biliocystic communications (BCC) depended on the location of the fistula along the biliary tract. In case of distant BCC away from the biliary convergence, first intention management was the sectioning of the involved biliary duct distant from the cyst during hepatic resection. In case of proximal or complex BCC, the fistula was sutured on T-tube drain to avoid hazardous bile duct reparation. Parasitic bile duct obstructions were treated by choledochotomy followed by T-tube placement. Biliary fistulas were managed according to patient’s clinical tolerance and the effectiveness of the initial surgical drainage. In case of incomplete drainage associated with symptoms, radiological drainage, ERCP and in last instance reoperation was proposed. In other cases, scarring of the biliary fistulas occurred spontaneously. Drainage of the peritoneal cavity was routinely performed.
Multilocular cyst of the right liver and segment I, 15 cm in diameter, in a 39-year-old woman with symptomatic biliocystic fistula. Due to the close relationship with the back of the hepatic pedicle and inferior vena cava, the cyst was treated by open cyst subtotal resection and right hepatectomy, resecting the biliocystic fistula. Two units of RBC were transfused. The postoperative course (12 days) was complicated by delayed gastric emptying
Data Collection
The following data were collected and compared: age; sex; symptoms; comorbidities according to the American Society of Anaesthesiologists (ASA) score;16 cyst characteristics on imaging according to Gharbi’s classification;14 size, number and location of the cysts; surgical procedure; total time of the Pringle manoeuvre; operative time; accidental rupture of the cyst; postoperative events classified according to Dindo-Clavien;15 length of hospital stay (LOHS) and recurrence. Hepatic resections were classified according to the Brisbane classification.16 Postoperative bile leakage was defined according to the International Study Group of Liver Surgery.17 Recurrence was diagnosed radiologically by the reappearance of hydatid cysts close to the excision site (loco-regional recurrence) or the appearance of new cysts outside the abdomen. Recurrence delay was determined from the date of the first operation to the date of operation for recurrence, including patients whose first operation was conducted outside the department. Follow-up consisted of regular physical examinations, serology and abdominal ultrasonography first completed in the outpatient clinic by the operative surgeon and then by regular examination by the general practitioner. For this report, the general practitioner of each patient was contacted again when it was possible. Recurrence-free survival was calculated for all patients from the date of the first operation, wherever it was performed, to the date of the recurrence diagnosis. Patients who underwent surgery in the department for recurrent LHD were censored after the second operation to avoid duplicates in the survival analysis.
Statistical Analysis
Statistical analyses were performed using IBM SPSS 20.0 (IBM Inc., New York, NY, USA). Categorical variables were described in terms of frequency (percentages) and continuous variables as medians (range). Owing to the retrospective nature of this work, some variables were missing: percentages were thus recorded as valid percentages based on the number of patients with the data available. Continuous data were first studied linearly and then were stratified into categorical variables using receiver operating characteristic (ROC) curves. Univariate analyses were conducted using Student’s t test or the Mann-Whitney test for continuous variables and chi-squared test or Fisher’s exact test for categorical variables. A two-tailed P value ≤ 0.05 was considered statistically significant. Multivariate analyses were performed using a backward stepwise logistic regression model adjusted for covariates significant at P ≤ 0.1 on univariate analysis. Recurrences were assessed using the Kaplan-Meier method and compared between groups by the log-rank test.
Results
During the study period, 502 benign liver lesions were operated, 120 (24%) of which were LHD. In all, 116 patients (99 primary LHD and 17 recurrent LHD) fulfilled the inclusion criteria and were selected for further analyses: 79 CCRs and 37 OCRs (Fig. 3). Median age of the population, 57 women and 59 men, was 42 (16–77) years.
Baseline Features and Cyst Characteristics (Table 1)
Liver hydatid disease was symptomatic in 90 cases (78%). Most common clinical presentations were abdominal pain (n = 80, 69%), septic signs (n = 18) and jaundice (n = 17). Number of treated cyst was 167: 87 patients with single cysts and 29 patients with multiple cysts (18 with two cysts, four with three cysts and seven with four or more cysts). Between OCR and CCR, features were comparable: age, sex, ASA score, previous LHD surgery, hydatid serology, Gharbi’s classification, size of cyst, except for jaundice (P = 0.044) and location at segment I (P = 0.003).
Surgical Procedures (Table 2)
All the patients in the CCR group underwent radical resection (55 anatomical hepatic resection and 25 total cystectomies) compared with 11 in the OCR group (P < 0.001). In radical resection, only right hepatectomy was more common in CCR group (P < 0.001). Ten patients required blood transfusion. Exploration of the biliary tract, by choledochotomy, was performed in 11 and 12 patients for respectively CCR and OCR (P = 0.020) and followed by a T-tube. Biliocystic fistula was found more frequently in the OCR than in the CCR group (P = 0.003), although rate of cholangiography did not differ between the two groups. Synchronous resection of adjacent structures was needed in 24 cases for tight adherences: 19 diaphragmatic resections, 1 right colectomy, 1 right adrenalectomy and 1 atypical pulmonary resection through the diaphragm. One patient had bilateral ovariectomy for ovarian cysts mimicking ovarian hydatidosis, and another required embolectomy of the pulmonary artery for parasitic spread by sternotomy 2 weeks before hepatectomy. There was no difference between the two groups according to synchronous resection of adjacent structure.
Postoperative Outcomes (Table 2)
Overall, 30 patients developed at least one postoperative complication. One patient died a few hours after surgery from a myocardial infarction. In all, four patients in the CCR group developed severe postoperative complications compared with seven in the OCR group (P = 0.036). Clavien III–IV events were distributed as follows: symptomatic pleural effusion requiring drainage (n = 3), bile leakage requiring ERCP (n = 2), acute respiratory distress syndrome requiring prolonged stay in ICU (n = 2), Budd-Chiari syndrome due to left hepatic vein stenosis (n = 1), intra-abdominal abscess (n = 1) and migration of a peritoneal drain (n = 1). Postoperative biliary fistula was presented for nine patients among one without cholangiography, three without choledochotomy and five with a BCC. There was a trend toward more postoperative bile leakage in the OCR group (P = 0.463), although not statistically significant. In univariate analysis (Table 3), only the operative time (≥ 210 min) and rupture of the cyst during surgery were associated with serious postoperative complications. In the multivariate analysis, variables that independently correlated with the occurrence of a serious postoperative event were OCR and an operative time ≥ 210 min.
Accidental rupture of the cyst occurred four times during CCRs. The median size of ruptured cysts was 8 cm (7–10), not different from the non-ruptured ones (8-cm range (2–20), P = 0.950). Only the location seemed to influence cyst rupture since cysts located at segment I were more subject to rupture than others (P = 0.048). However, multivariate logistic regression analysis failed to identify independent predictors of rupture.
Follow-up
Among the 18 patients who underwent surgery for recurrent LHD, 2 patients were excluded from the recurrence analysis because of insufficient data relative to the first intervention. Another patient without recurrence was excluded because of the lack of follow-up. Overall, recurrence analysis was conducted on 113 patients. The median follow-up of the series was 10 (1–40) years.
None of the patients who underwent CCR in the department experienced recurrence. Overall, including the patients who underwent the first surgery at another centre, two patients developed local recurrence in the OCR group at 14 and 17 years compared with one in the CCR group at 21 years (supplementary table S1). The 5- and 10-year recurrence rates were both 0% in the CCR group compared with 18% and 27%, respectively, in the OCR group (P < 0.001; Fig. 4). The median time to recurrence was 5 (1–20) years and did not differ between groups (Table 4).
Discussion
For liver hydatid cyst, the best surgical strategy remains controversial because the conclusions of studies reporting on radical and conservative resections are discordant7, 9, 17,18,19,20,21. Particularly, most series do not assess whether closed or opened cyst resection was performed,8, 9, 17, 19,20,21 this option is often left to the surgeon’s discretion, thus introducing a confounding factor that could impair results. Indeed, OCR is believed to be safer than CCR since the technique avoids the accidental rupture of cysts. Thus, the risk of peritoneal seeding is limited, and better control of major biliovascular structures is achieved, whose preservation is mandatory for a “benign” disease. Furthermore, OCR could limit the specific risks of liver radical resection surgery. By contrast, because CCR consists of harvesting the adjacent parenchyma to keep the cyst unopened, this technique is supposed to decrease local recurrence and avoid complications related to pericyst preservation, such as bile leakage and postoperative abscess20, 22. However, CCR techniques most refer to anatomic hepatic resection; thus, they are believed to increase severe postoperative complications.
The results of our study do not support this opinion since we found that CCR did not increase the risk of severe morbidity following resection compared with OCR (5% vs 19%; P = 0.036) which was the only independent predictive factor of severe postoperative complications, together with the operative time. Finally, OCR increased the risk of disease recurrence. Thus, this study suggests the superiority of CCR over OCR for the management of primary and recurrent LHD with respect to postoperative and long-term outcomes.
In the present study, the rate of severe complications was 19% in the OCR group. This result is in accordance with a 21% morbidity rate after OCR in a series of 1412 LHD cases.12 The most frequent complication was postoperative bile leakage (8%), followed by pleural effusion (3%). The higher incidence of bile leakage following conservative approaches is a direct consequence of unroofing or partial cystectomy techniques that do not treat the pericyst, thus disregarding micro-BCC that postoperatively decompensates in the form of abscess and bile leakage.10, 18 Moreover, the inhibition of parenchymal regeneration due to local inflammation favoured by cyst liquid and/or perioperative local sterilisation could maintain cavity-related complications.18
However, the higher rate of bile leakage could also result from a selective bias. Considering biliary symptoms, (i) 24% of OCR patients presented with jaundice compared to 10% in CCRs; (ii) a clinical BCC was observed in 43% of OCRs vs 18% of CCRs; (iii) the rate of T-tube drain placement in the OCR group was more than twice that in the CCR group. Actually, biliary involvement in OCR patients was more frequent than in CCR patients. For those patients, OCR could have been preferred to CCR as a safer alternative to treat BCC, avoiding the need to perform a high-risk biliary reconstruction since the opening of the cyst allowed for simply controlling and repairing the biliary tract. Thus, the higher rate of biliary fistula in OCRs could also be interpreted as the consequence of a higher rate of biliary reconstruction in this group.
Considering the cyst location, all cysts involvement segment I benefited from OCR. Cysts located at segment I are more complex to manage because of accessibility and tight contact with the IVC, rendering CCR more dangerous notably when IVC reconstruction is necessary. As for patients with biliary tract involvement, the forecast of a complex surgical repair in the case of CCR could have influenced the decision to perform an OCR. There are not enough events in this series to demonstrate a higher morbidity among CCR patients with suspected BCC and/or cyst at segment I. However, it should be noted that all the patients who experienced biliary fistula in the OCR group healed spontaneously—except one who required an endoscopic procedure—and none required relaparotomy for this complication. Thus, OCR for patients with biliary tract involvement or segment I could be an interesting alternative to CCR to avoid complex biliovascular reconstruction or accidental cyst rupture.
The main limit of CCR is accidental rupture of the cyst, leading to peritoneal seeding and disease recurrence.19, 23 In this series, four patients experienced accidental rupture of the cyst during CCR. Baseline features of patients, cyst characteristics and surgical technique did not differ between groups, such that no independent predictive factors of cyst rupture could have been identified in the multivariate analysis. However, no anaphylactic shock or peritoneal recurrence was observed.
Anatomical hepatic resections were the most frequently performed procedures during CCR (68%). This rate is the highest in the literature, and this specificity has already been discussed in a previous report by our team.20 As a result, comparison with other studies is difficult, for example, one of the most important published series reported only 125 liver resections among 1680 procedures (7%).12 This attitude was chosen from the beginning of the study period because of a preference for a radical treatment with CCR and probably secondary to a developed hepatic surgical activity. In these cases, anatomic hepatic resections were more frequently chosen because of the wide destruction of the hepatic parenchyma by cysts.
In the present study, all recurrences, except one, were observed after an open-cyst approach. Hence, OCR represents an important risk of recurrence and must be considered only when a CCR appears hazardous for treating a benign disease. Since the other authors focused on the radical or conservative nature of surgery, it seemed important to us to focus on the open or closed criterion of surgery which limits the possibility of comparison. For example, Tagliacozzo et al.18 reported a 30% recurrence rate for conservative surgery compared with 1% for radical procedures, whereas El Malki et al.13 reported a 2% and 4% rate for conservative and radical approaches, respectively. A meta-analysis including 19 studies concluded that radical resections significantly reduce the risk of long-term recurrence (OR = 0.16; 95% CI 0.11–0.23).6 One reason of higher recurrences in a conservative approach have been explained by Voros et al., who constated that protoscoleces are also contained in the pericyst and are left in place in conservative techniques.22 Concerning OCR, the effect of sterilisation is incomplete, ranging from 50 to 91%21, 22 and favouring peritoneal/local recurrence.
Finally, as our study has one of the long follow-ups thanks to the updating of the follow-up of patients, we were able to analyse late recurrences which are rarely reported. Generally, the follow-up is 5–6 years old6, 7, 9, 20, 21 and probably do not know about late recidivism. However, the long period until recurrence is poorly known. This is a novelty that must be considered in patient follow-up.
This study has several limitations that may prevent an immediate change in clinical practice: (i) the retrospective nature of the work induced inherent and unintentional selection bias that is impossible to be ruled out; (ii) the inclusion period over 12 years may have inserted inherent differences related to staging and treatment techniques,24,25,26 especially anaesthesia for liver surgery; (iii) because of the policy of the department favouring CCRs, OCRs were mainly performed in the case of complex LHD (perihilar or pericaval), possibly leading to an overestimation of the morbidity in the OCR group, especially for bile leakage; (iv) in contrast to CCRs, the OCR group comprised conservative and radical resection techniques, which could have artificially increased the morbidity and recurrence rates in this group11. However, these criteria have been taken into account in the statistical analysis and have not been found to be independent factors; (v) the series comes from a liver surgery expert centre, questioning the reproducibility of the results in other centres, notably for CCR and radical resection that are routinely performed in the department. This limit restricts the extrinsic validity as it depends on the expertise of the centre; (vi) because of insufficient data concerning patients included for recurrent LHD, the statistical analysis for possible confounders could not be adjusted.
Conclusion
Closed cyst resection showed a lower severe morbidity and recurrence rate when compared to OCRs, and thus should be the gold standard for the surgical management of primary and recurrent LHD without perihilar or pericaval involvement. For those patients, OCRs should be preferred to avoid hazardous biliovascular reconstructions and critical related postoperative complications. Due to the long delay of recurrence observed in this study, the patient follow-up must be prolonged over 10 years.
References
Moro P., Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13(2):125–33. https://doi.org/10.1016/j.ijid.2008.03.037.
Torgerson PR., Devleesschauwer B., Praet N., Speybroeck N., Willingham AL., Kasuga F., et al. World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis. PLOS Med. 2015;12(12):e1001920. https://doi.org/10.1371/journal.pmed.1001920.
Sielaff TD., Taylor B., Langer B. Recurrence of hydatid disease. World J Surg. 2001;25(1):83–6.
Demirci S., Eraslan S., Anadol E., Bozatli L. Comparison of the results of different surgical techniques in the management of hydatid cysts of the liver. World J Surg. 1989;13(1):88–90; discussion 90-91.
Kayaalp C., Bostanci B., Yol S., Akoglu M. Distribution of hydatid cysts into the liver with reference to cystobiliary communications and cavity-related complications. Am J Surg. 2003;185(2):175–9.
Pang Q., Jin H., Man Z., Wang Y., Yang S., Li Z., et al. Radical versus conservative surgical treatment of liver hydatid cysts: a meta-analysis. Front Med. 2017:669–75. https://doi.org/10.1007/s11684-017-0559-y.
Yüksel O., Akyürek N., Şahin T., Salman B., Azili C., Bostanci H. Efficacy of radical surgery in preventing early local recurrence and cavity-related complications in hydatic liver disease. J Gastrointest Surg. 2008;12(3):483–9. https://doi.org/10.1007/s11605-007-0301-1.
Secchi MA., Pettinari R., Mercapide C., Bracco R., Castilla C., Cassone E., et al. Surgical management of liver hydatidosis: A multicentre series of 1412 patients. Liver Int. 2010;30(1):85–93. https://doi.org/10.1111/j.1478-3231.2009.02116.x.
El Malki HO., Souadka A., Benkabbou A., Mohsine R., Ifrine L., Abouqal R., et al. Radical versus conservative surgical treatment of liver hydatid cysts. Br J Surg. 2014;101(6):669–75. https://doi.org/10.1002/bjs.9408.
Bourgeon R., Mouuiel J. The merits of radical surgery in the treatment of hydatid cysts of the liver. Memoires Acad Chir Fr. 1964;90:355–61.
von Elm E., Altman DG., Egger M., Pocock SJ., Gøtzsche PC., Vandenbroucke JP., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann Intern Med. 2007;147(8):573. https://doi.org/10.7326/0003-4819-147-8-200710160-00010.
Gharbi HA., Hassine W., Brauner MW., Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139(2):459–63. https://doi.org/10.1148/radiology.139.2.7220891.
Sbihi Y., Rmiqui A., Rodriguez-Cabezas MN., Orduña A., Rodriguez-Torres A., Osuna A. Comparative sensitivity of six serological tests and diagnostic value of ELISA using purified antigen in hydatidosis. J Clin Lab Anal. 2001;15(1):14–8.
Brunetti E., Kern P., Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114(1):1–16. https://doi.org/10.1016/j.actatropica.2009.11.001.
Dindo D., Demartines N., Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Strasberg SM. Nomenclature of hepatic anatomy and resections: A review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–5. https://doi.org/10.1007/s00534-005-0999-7.
Dziri C., Haouet K., Fingerhut A., Zaouche A. Management of Cystic Echinococcosis Complications and Dissemination: Where is the Evidence? World J Surg. 2009;33(6):1266–73. https://doi.org/10.1007/s00268-009-9982-9.
Gollackner B., Längle F., Auer H., Maier A., Mittlböck M., Agstner I., et al. Radical Surgical Therapy of Abdominal Cystic Hydatid Disease: Factors of Recurrence. World J Surg. 2000;24(6):717–21. https://doi.org/10.1007/s002689910115.
Motie MR., Ghaemi M., Aliakbarian M., Saremi E. Study of the Radical vs. Conservative Surgical Treatment of the Hepatic Hydatid Cyst: A 10-Year Experience. Indian J Surg. 2010;72(6):448–52. https://doi.org/10.1007/s12262-010-0163-8.
Tagliacozzo S., Miccini M., Bonapasta SA., Gregori M., Tocchi A. Surgical treatment of hydatid disease of the liver: 25 years of experience. Am J Surg. 2011;201(6):797–804. https://doi.org/10.1016/j.amjsurg.2010.02.011.
Gupta N., Javed A., Puri S., Jain S., Singh S., Agarwal AK. Hepatic Hydatid: PAIR, Drain or Resect? J Gastrointest Surg. 2011;15(10):1829–36. https://doi.org/10.1007/s11605-011-1649-9.
Voros D., Kalovidouris A., Gouliamos A., Vlachos L., Danias N., Papadimitriou J. The real incidence of extracapsular (satellite) cysts of liver echinococcus. HPB Surg World J Hepatic Pancreat Biliary Surg. 1999;11(4):249–52.
Mottaghian H., Saidi F. Postoperative recurrence of hydatid disease. Br J Surg. 1978;65(4):237–42.
Kern P., Menezes da Silva A., Akhan O., Müllhaupt B., Vizcaychipi KA., Budke C., et al. The Echinococcoses. Advances in Parasitology, vol. 96. Elsevier; 2017. p. 259–369.
Atmatzidis KS., Pavlidis TE., Papaziogas BT., Mirelis C., Papaziogas TB. Recurrence and long-term outcome after open cystectomy with omentoplasty for hepatic hydatid disease in an endemic area. Acta Chir Belg. 2005;105(2):198–202.
Lv H., Jiang Y., Peng X., Zhang S., Wu X., Yang H., et al. Subadventitial cystectomy in the management of biliary fistula with liver hydatid disease. Acta Trop. 2015;141:223–8. https://doi.org/10.1016/j.actatropica.2014.06.006.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Julien, C., Le Treut, Y.P., Bourgouin, S. et al. Closed Cyst Resection for Liver Hydatid Disease: a New Standard. J Gastrointest Surg 25, 436–446 (2021). https://doi.org/10.1007/s11605-019-04509-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04509-1