Summary
Background
Hepatic hydatid cystic disease continues to be a serious health problem and is endemic in Iraq. There are of two types of cysts: noncomplicated and complicated cysts. Open surgery is widely practiced for both types. The aim of this study was to evaluate the clinical features, management, and outcome of surgical treatment in both types of cyst.
Methods
The study included 150 patients operated on between 1996 and 2014. The patients’ demographic data, location, number, size, type of cysts, surgical procedure performed, morbidity, recurrences, and duration of hospital stay were recorded.
Results
There were 102 female and 48 male patients with an age range of 4–70 years. There were more patients with noncomplicated cysts than complicated cysts – 94 and 56 patients, respectively. The complicated disease group had significantly more pronounced clinical presentations (p < 0.001) and higher postoperative morbidity (p < 0.001), and without significant change in recurrence rate (p = 0.059). Mean postoperative hospitalization time for noncomplicated cysts was 3.2 days, and for complicated cysts 5.6 days (p < 0.001).
Conclusion
The most common type of hydatid cyst is the noncomplicated type, which has lower complication rates and shorter hospital stay regardless of the management technique of the cyst cavity. Therefore, complicated and noncomplicated cysts should be considered as different forms of the disease entity with different outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hydatid disease is a parasitic disease of worldwide distribution. It is endemic in Iraq [1, 2] owing to infestation by the Echinococcus granulosus parasite, and it continues to be an important and challenging medical health problem. Factors such as lack of health care and education as well as poor hygiene conditions contribute to the development of the disease. The disease is complex and dynamic, and the liver is the most commonly involved organ [3, 4]. Patients may be asymptomatic for years and usually present with nonspecific complaints, or they may be symptomatic owing to an increase in the size or complications of the cyst such as infection, rupture (internal or contained, intrabiliary, intraperitoneal, or intrapleural rupture), or pressure on the adjacent structures [5].
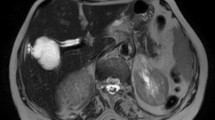
The key for successful management is early diagnosis by sophisticated medical imaging and timely surgical intervention. The present work focuses on hepatic hydatid cysts of both the noncomplicated (NCHHC) and complicated (CHHC) types. Hepatic hydatid cysts are best diagnosed and monitored using imaging studies including ultrasound (US). Computed tomography (CT) and magnetic resonance imaging (MRI and MRCP) are used in certain selected cases.
Hepatic hydatid cysts can be treated with different methods such as surgery, chemotherapy, and/or percutaneous aspiration, but surgery remains the established treatment [6]. The most effective treatment of noncomplicated hydatid disease is evacuation of the cyst contents and decreasing of the dead space of the cystic cavity; however, in the complicated type there is no standard surgical management [7] and treatment is determined according to the stage of the cyst and the relation of the cyst to the biliary ducts or surrounding organs.
This study was carried out to identify the clinical presentation, management, and the outcomes of surgical treatment of NCHHC and CHHC.
Methods
We retrospectively reviewed 150 patients with hepatic hydatid cysts who were treated surgically between March 1996 and August 2014. Preoperative diagnosis was based on history, clinical examination, and abdominal US. Liver function tests and blood eosinophils have a very low sensitivity and therefore were not routinely used to support the diagnosis except in selected cases.
The patients were divided into two groups according to cyst type: NHHC and CHHC.
Informed consent was obtained from patients included in the study, oral consent until December 2001 and then written consent for the rest, which was obtained during hospital admission prior to operation explaining all the benefits and risks of the surgical procedure by the resident doctor.
Exclusion criteria were cysts smaller than 4 cm in diameter, located deep in the liver parenchyma (more than 4 cm from the liver surface on US imaging), calcified cysts, and associated extrahepatic hydatid cysts.
The choice of operative approach between conservative and radical procedures in addition to other surgical procedures performed at the same time, such as cholecystectomy and choledochotomy and T‑tube insertion, depended on the type, location, and complications of the cyst. In all cases the approach was through laparotomy (paramedian or subcostal incision), and the operative field was carefully isolated by gauze packs. After a drainage procedure was selected, the cyst contents were aspirated and evacuated completely; the cavity was then carefully examined for sites of bile leakage, which were sutured if possible. Management of the residual cavity following conservative surgery was performed with either external drainage or omentoplasty. Deroofing and omentoplasty were performed by constructing an omental flap followed by packing and fixation of the flap in the residual cavity.
Statistical analyses were performed with SPSS version 19, using the Student t test for quantitative variables, and the chi-square test and Fisher’s exact test for categorical variables. A value of p < 0.05 was considered significant.
Results
During the study period, 150 consecutive patients who had hepatic hydatid cyst were operated on. The age range was 4–70 years (average, 33.26 ± 15.29 SD). There were 102 female and 48 male patients. Female patients outnumbered their male counterparts in both groups (F/M, 2.1/1), as shown in Fig. 1, but the sex ratio was not statistically different between the two groups (p = 0.028 for male patients and p = 0.054 for female patients).
The right lobe (n = 120 patients) was more involved than the left lobe (n = 17 patients), while both lobes were involved in 13 patients, as shown in Fig. 2. Single cysts were found in 117 patients and multiple cysts in 33 patients. The cyst diameter ranged from 5 to 20 cm in diameter on US examination (see Table 1).
a Liver lobes involved by hydatid cyst (R right lobe, L left lobe, B both lobes). b Large complicated hepatic hydatid cyst, bile stained with ruptured membrane. c Complete excision of hepatic hydatid cyst (radical operation ). d Large hydatid cyst with hundreds of daughter cysts. e CT scan of upper abdomen showing multiple hydatid cysts of the liver. f CT scan of abdomen with multiple hepatic hydatid cysts. g CT scan with detached membrane of liver hydatid cyst owing to internal rupture
CT was performed in 25 % cases (with suspicious hydatid cyst on US and in multiple cysts). MRI and MRCP were ordered for patients with features of biliary obstruction (3.3 %).
The complicated cyst group included patients with internal rupture (with and without bile-stained content), intrabiliary and intraperitoneal rupture, suppuration of the cyst, and cyst with pressure effects on the adjacent organs.
Noncomplicated cysts were seen in 62.6 % of patients (94 patients) while the complicated type was observed in 37.3 % (56 patients), as shown in Fig. 1. Types of complicated cysts were as follows: internal (contained) rupture in 37 cases, intrabiliary rupture in five cases, pressure effect in three cases, infection in ten cases, intraperitoneal rupture in one case (see Table 2).
Significant differences in the clinical manifestations of the two forms of the disease were seen, with fever, jaundice, and abdominal mass/tenderness more common in patients with CHHC, and incidental discovery of the disease occurring in more patients of the NHHC group. Presenting signs and symptoms are demonstrated in Table 3.
The type of surgical operation was simple drainage of the cyst in 143 patients, omentoplasty in four patients, and radical cyst excision in three patients. An additional operation was performed on several patients, i. e., cholecystectomy in seven patients, choledochotomy and insertion of T‑tube in three patients, and both T‑tube with cholecystectomy in two patients (see Table 4).
The outcomes of surgical treatment and hospital stay were: two patients had anaphylactic shock, ten patients had chest infection, with no statistical difference between complicated and noncomplicated cases, and there were local surgical complications including bile leak and fistula in 44 cases (p < 0.001) and wound infection in 11 cases (p < 0.001).
Recurrence was detected in 13 patients, but it was not statistically significant (p = 0.059), as shown in Table 5.
The NCHHC group had a mean hospital stay of 3.7 days, whereas for patients in the CHHC group the mean hospital stay was 5.6 days (statistically significant difference at p < 0.001). There was no mortality in any of the groups.
The follow-up period in the current study was 2–5 years. The first follow-up visit was after 3 months and then every 6 months; imaging was performed by sonographic examination and in the case of recurrence a CT scan was ordered.
Discussion
In general, hepatic hydatid cysts are commonly located in the right lobe of the liver and are single and noncomplicated [8, 9]. Cysts may persist for many years without any symptoms but in some cases they can cause complications such as rupture into the biliary tree, abdominal cavity, or pleural cavity. Also the cyst might become infected and eventually replace the liver parenchyma. Considering the possibility of such risks, the disease must be diagnosed and treated effectively [10, 11].
The incidence of CHHC reported in various studies ranges between one third to as high as 60 % of the total number of patients diagnosed and treated for echinococcal disease [12, 13].
In the current study, 94 patients (62.6 %) had NHHC and 56 patients (37.3 %) had CHHC: There was internal rupture in 37 patients (24.6 %), with infection in ten patients (6.6 %), intrabiliary rupture in five patients (3.3 %), pressure effect in three patients, (2 %) and intraperitoneal rupture in one patient (0.6 %). Internal rupture was the most frequent type of complicated cyst; it is detected by the detachment of the endocyst from the pericyst and is probably related to decreasing intracystic pressure, degeneration, host response, trauma, or response to medical therapy and percutaneous drainage [14–16].
The variation in the disease process has led to a wide range of treatment modalities with an equally wide range of technological and training backgrounds necessary for implementation and delivery. Therefore, there is no “one size fits all” management approach available, and a stage-specific approach currently appears to be the best way to manage this condition [17]. Surgical treatment still remains the primary treatment of choice in the management of hydatid disease. Treatment of the cystic cavity is the principal issue in this disease. Many debatable results have been reported in relation to the surgical treatment of the cystic cavity. Some authors prefer radical operations, such as hepatectomy, resection of the cyst, or pericystectomy. Cysts located peripherally and pedunculated cysts can be excised entirely. Such operations have high morbidity and mortality rates and can be considered radical procedures for such a benign disease. As a result, conservative surgical procedures were selected more frequently in both groups in our study.
The surgical procedures selected to manage complicated and noncomplicated cysts are demonstrated in Table 4. Several methods have been put forward for the management of the residual cyst cavity, and depending on the site, size, type, and preference of the surgeon, these techniques are:
-
1.
Open drainage of the cyst cavity into the peritoneal cavity in the case of small, superficial, and shallow uninfected cysts. A complication is intestinal entrapment if the cavity is at the inferior aspect of the liver or abscess formation particularly if the cyst is near the diaphragm, which did not apply in our cases.
-
2.
Obliteration of the residual cavity in the case of deeply located cysts by capsulorrhaphy. The cavity is filled with normal saline and the opening of the cavity is closed without any drain. Capitonnage: the dead space is obliterated by a series of purse-string sutures starting from the bottom of the pericyst. Introflexion: is a modification of capitonnage in which the upper edge of the pericyst is sutured to the deepest part of the cavity with absorbable sutures and then the edge of the pericyst is sutured to the collapsed edge by a running suture. The risk of this procedure is injury to the blood vessels and biliary tract, which is why it was avoided in the current study. In omentoplasty, a flap of omentum is brought to rest within the pericyst cavity with the assumption that the omentum will seal small biliary leaks and obliterate the cavity, tool.
-
3.
External tube drainage: An tube drain with an appropriate diameter is placed in the cyst cavity after complete evacuation of its content and the drain is brought out through a separate opening in the case of infected cysts and cysts with biliary communication. From all these procedures, external drainage seems to be the most effective in my experience, and it is simple and safe regardless of the cyst number and position.
Less invasive techniques include a percutaneous approach under ultrasound guidance: PAIR (puncture, aspiration, injection, reaspiration) is indicated for accessible cysts, infected cysts, recurrent cysts after operation, or if a patient is not fit for or refuses surgery. Laparoscopic surgery is another option, and needs proper patient selection and experienced laparoscopic surgeons. However, there have been no controlled clinical trials comparing the efficacy of the less invasive techniques with open surgery. In a large series of 304 patients, external tube drainage was associated with a high incidence of infective complications (29.5 %) and long-lasting biliary fistulae (8.2 %) [18]. In our study, biliary leak and fistula were seen in only 44 patients (29.3 %). In all, 14 patients with NCHHC and 30 patients with CHHC were managed by external tube drainage and all of the discharge disappeared after 4–8 weeks without the need for a surgical or endoscopic intervention.
Omentoplasty is useful in patients with a small biliary communication [19], and is used mainly for cysts with an accessible roof, a thick wall, and those that are uncomplicated (not infected and no definite bile leak). A flap of omentum is brought to rest within the pericyst cavity with the assumption that the omentum will seal small biliary leaks and obliterate the cavity and also protect against infection by promoting reabsorption of serosal fluid and by inducing macrophage migration in septic foci. Omentoplasty was carried out on only four patients in this study and cannot be applied in the following cases: cysts located in the superior–posterior aspect of the liver, large cysts, multiple cysts, cysts with a thin wall, and complicated cysts.
Internal (contained) rupture was seen in 37 patients (24.6 %) in this study and 60 % of internal rupture cysts with bile-stained content were treated by external tube drainage in 35 patients and with deroofing and omentoplasty in one patient; three patients had radical excision. Infection of the cyst was encountered in 6.6 % of patients. The presence of cyst leakage leads to bacterial contamination of the endocystic fluid, and therefore it is believed that the cystobiliary communication is the more frequent cause of infection [20, 21]. Clinical manifestations in acute cyst infection resemble those of liver pyogenic abscess (pyrexia, chills, and increased abdominal pain).
Intrabiliary rupture was detected in five patients (3.3 %) and all of them presented with jaundice, fever, and a tender right hypochondrium. A dilated biliary duct was seen ON US and confirmed by MRCP in three patients, who were treated by drainage of the cyst content and choledochotomy with T‑tube insertion. After 10 days, T‑tube cholangiography was performed and the tube was removed. Three patients had a fistula, which closed spontaneously after a maximum period of 8 weeks without endoscopic or surgical intervention.
Peritoneal rupture of echinococcal cysts is a rare but hazardous complication. Abdominal trauma combined with the presence of large, superficial, thin-walled cysts in the anterior and inferior part of the liver are factors predisposing toward cyst rupture, although spontaneous rupture is not uncommon [12, 22].
Peritoneal rupture is sometimes silent, and disseminated secondary abdominal echinococcosis is found after a long asymptomatic period, with the patient unaware of when the rupture occurred [23]. In this study, we encountered one patient with intraperitoneal rupture of the hepatic hydatid cyst that presented as acute abdomen (board-like rigidity) with hypotension and urticaria following blunt trauma to the abdomen; the patients had an uneventful recovery following drainage of the cyst and peritoneal toilet.
The higher incidence of postoperative complications in the CHHC group is a rather predictable result considering the difficulties associated with complicated disease management.
Outcomes were measured by postoperative cavity-related complications, such as biliary leakage (leakage for 10 days or less), biliary fistula (leakage for more than 10 days), cavity infections, recurrence, and postoperative hospitalization. Medical complications include anaphylactic shock in two patients and chest infection in ten patients, with no significant difference between the groups.
Surgical complications included 44 patients with bile discharge, namely, 34 patients with biliary leakage and ten patients with biliary fistula, which continued discharging bile in the range of 250–300 ml/day, and then reduced gradually over 4–8 weeks without any surgical or endoscopic intervention. There was also superficial wound infection in eight patients and deep abdominal abscess in three patients. These complications were encountered in the CHHC group more than in the NCHHC with a statistically significant difference between groups for certain complications such as wound infection (p = 0.001), bile leak and fistula, as well as hospital stay (p < 0.001).
Despite the number of therapies now available, recurrence remains one of the major problems in the management of hydatid disease, ranging from 4.6 to 22.0 % in different series [24, 25]. Recurrence of the cyst was observed in 13 patients (8.6 %), regardless of the type of intervention: in five patients with NCHHC and eight patients with CHHC (p = 0.059; not significant). The main reasons for recurrence appeared to be microscopic spillage of live parasites, failure to remove all viable cysts at inaccessible or difficult locations, or leaving a residual cyst wall at the initial operation. The latter was especially true among patients with long-standing active cysts where there may have been penetration through the original pericyst.
A limitation of the current study is that the technical procedure of choice is controversial, since there is a lack of appropriate randomized controlled studies to optimize the methods of treatment and to reduce the recurrence rate and need for postoperative treatment.
Conclusion
In conclusion, the most common type of hepatic hydatid cyst is the noncomplicated type, which has lower complication rates and a shorter hospital stay than the complicated type, regardless of the management technique used for the cavity. Therefore, complicated and noncomplicated cysts should be considered different forms of this disease entity with different outcomes.
References
Asakkal N. Human hydatid disease in Mosuil. Iraqi Med J. 1982;29:80–6.
Mohmood S, Al Janabi BM. Hydatid disease in children & youth in Mousil, Iraq. Annals of Tropical Med. 1983;77:237–8.
Rinaldi F, Brunetti E, Neumayr A, Maestri M, Goblirsch S, Tamarozzi F. Cystic echinococcosis of the liver: A primer for hepatologists. World J Hepatol. 2014;6(5):293–305.
Milicevic M. Hydatid disease. In: Blumgart LH, Fong Y, editors. Surgery of the Liver and Biliary Tract, 3rd edn. London: Churchill Livingstone; 1994. pp. 1121–50.
Al-Toma AA, Vermeijden RJ, Van De Wiel A. Acute pancreatitis complicating intrabiliary rupture of liver hydatid cyst. Eur. J Intern Med. 2004;15:65–7.
Vagholkar KR, Nair SA, Rokade N. Disseminated intraabdominal hydatid disease. Bombay Hosp J. 2004;46:2–7.
Ariogul O, Emre A, Alper A, Uras A. Introflexion as a method of surgical treatment for hydatid disease. Surg Gynecol Obstet. 1989;169:356–8.
Kumar A, Chatropadhyay TK. Management of hydatid disease of the liver. Postgrad Med J. 1992;68:853–6.
Yilmaz E, Gokok N. Hydatid disease of the liver: current surgical management. BJCP 1990; 44: 612–5.
Safioleas M, Misiakos E, Mann C, Karsikas D, Skalkeas G. Diagnostic evalution and surgical management of hydatid disease of the liver. World J Surg. 1994;18:859–65.
Demirci S, Eraslan S, Anadol E, Bozatli L. Comparison of the results of different surgical techniques in the management of hydarid cysts of the liver. World J Surg. 1989;13:88–91.
Akcan A, Sozuer E, Akyildiz H, et al. Predisposing factors and surgical outcome of complicated liver hydatid cysts. World J Gastroenterol. 2010;16:3040–8.
Chautems R, Buhler LH, Gold B, et al. Surgical management and long-term outcome of complicated liver hydatid cysts caused by Echinococcus granulosus. Surgery. 2005;137:312–6.
Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid Disease from Head to Toe. Radiographics. 2003;23:475–94.
Pedrosa I, Saiz A, Arrazola J, Ferreiros J, Pedrosa CS. Hydatid disease: Radiologic and pathologic features and complications. Radiographics. 2000;20:795–817.
Tuzun M, Hekimoglu B. Various locations of cystic and alveolar HD: CT appearances. J Comput Assist Tomogr. 2001;25:81–7.
Junghanss T, da Silva AM, Horton J, Chiodini PL, Brunetti E. Clinical management of cystic echinococcosis: state of the art, problems, and perspectives. Am J Trop Med Hyg 2008; 79: 301-311 [PMID: 18784219].
Balik AA, Başoğlu M, Celebi F, Oren D, Polat KY, Atamanalp SS, Akçay MN. Surgical treatment of hydatid disease of the liver: review of 304 cases. Arch Surg. 1999;134:166–9.
Al-Hashimi HM. Intrabiliary rupture of hydatid cyst of the liver. Br J Surg. 1971;58:228–32.
Agayev RM, Agayev BA. Hepatic hydatid disease: Surgical experience over 15 years. Hepatogastroenterology. 2008;55:1373–9.
Kayaalp C, Sengul N, Akoglu M. Importance of cyst content in hydatid liver surgery. Arch Surg. 2002;137:159–63.
Gunay K, Taviloglu K, Berber E, et al. Traumatic rupture of hydatid cysts: A 12-year experience from an endemic region. J Trauma. 1999;46:164–7.
El Malki HO, El Mejdoubi Y, Mohsine R, et al. Intraperitoneal perforation of hepatic hydatid cyst. Gastroenterol Clin Biol. 2006;30:1214–6.
Sielaff TD, Taylor B, Langer B. Recurrence of hydatid disease. World J Surg. 2001;25:83–6.
Kapan M, Kapan S, Goksoy E, et al. Postoperative recurrence in hepatic hydatid disease. J Gastrointest Surg. 2006;10:734–9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H.H. Ibrahim states that there are no conflicts of interest.
Ethical standards
Consent was obtained from all patients identifiable from images or other information within the manuscript. In the case of underage patients, consent was obtained from a parent or legal guardian.
Rights and permissions
About this article
Cite this article
Ibrahim, H.H. Hepatic hydatid cysts. Eur Surg 48, 290–295 (2016). https://doi.org/10.1007/s10353-016-0431-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-016-0431-3