Abstract
The hepatic hydatid cyst is a major health problem in endemic areas. Surgery is still the best choice for the treatment of hydatid cyst of the liver. There is controversy regarding efficacy of radical versus conservative surgical approaches. In this study, we aimed to evaluate the two surgical methods in patients treated for the hepatic hydatid cyst. This is a retrospective review of the medical records of 135 patients who underwent surgery for the hepatic hydatid cyst from 1993 to 2003. Surgery comprised conservative methods (evacuation of the cyst content and excision of the inner cyst layers) and radical methods (total excision of the cyst and removal of its outer layer). One hundred thirty five patients underwent liver surgery. Conservative surgery was performed for 71 (53%), whereas, the remaining 64 patients (47%) underwent radical surgery. Local recurrence rate of the cysts was lower in the radical versus conservative surgery group and the mean length of hospital stay was shorter in the radical surgery group. Radical surgery of the hepatic hydatid cyst may be the preferred treatment because of its low rate of local recurrence, as well as short hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
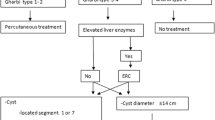
Hydatid disease results from infection by tapeworm larvae of the genus Echinococcus. It is an endemic disease in the Middle East areas and the Mediterranean countries. Traveling and tourism has change its pattern to a wide spread disease even in developed countries. [1–4] Hydatid cyst has been treated using medical treatment and cutaneous drainage and surgery, [5–8] but the main treatment has been surgery using different techniques which generally is divided in two subgroups; radical one and conservative. [9–11]
Using conservative procedure, the cyst would be drained out without omitting the pericystial layer; while radical procedure focuses on removing all the cyst layers as well as percystial one. [2, 3, 7, 12]
Conservative therapies are simple and safe procedures but comparing to radical one post operative complications, recurrence and hospital stay time are higher. [12–15]
In this study 135 patients with hydatid cyst have been retrospectively evaluated during 10 years of experience and the outcomes of different techniques have been compared to see if the radical therapy has less complications and recurrence.
Patients and Methods
In this study we have evaluated 141 cases with hepatic hydatid cyst with the an average of age of 46 years old ranging from 4 to 81 (SD = 4.2) and a male to female ratio of 71 over 64; they were admitted and operated on by several general surgery assistants under the supervision of one senior surgeon in the general surgery department, Imam Reza hospital during 1993 to 2003. Five patients were discharged without a specific treatment as they did not have any clinical symptoms with a small calcified cyst. One patient was discharged from the hospital as he did not consent to the operation.
The remaining number of cases, 135 patients, whom were operated on are the substantial part of this study. Using the conservative procedure all the cyst’s contents and its internal layers would be removed, while in the radical approach it will include the external layer as well. The patients’ allocation for the surgery was based on the size, number, and location of the cysts as well as intraoperative findings. In a way that large cysts, diffuse multiple cyst, those near to great vessels and deep cyst were operated using the conservative procedure. The patients had their drains only till its daily excretions reached less than 30 cc, which was the time that they could be discharged from hospital.
All of the patients received Albendazole for 6 months after completion of the surgery.
The patients were followed up in every 6–12 months periods up to 5 years after the operation by the mean of physical examination, liver function tests and abdominal ultrasonography. Considering 15 patients (13 from conservative group and 2 from the other one) who did not participate during the following up, an exact fisher test was used in statistical processes.
Results
74 patients out of total number of operated patients (135) were female and 61 male. Their age ranged from minimum of 4 to a maximum of 81 years old. 27 patients (20%) had already been operated because of hepatic hydatid cysts once or several times. While abdominal pain was the most common complaint, the other clinical signs include dyspepsia, fever, jaundice, and abdominal mass (Table 1). Serological tests, plain abdominal x-rays, abdominal ultra-Sonography, and CT scan and in jaundice cases an ERCP are used as diagnostic procedures.
Evaluating all 135 patients revealed the total number of 190 hydatid cysts: 146 in the right hepatic lobe and 44 in the left one. 74 percents of patients (100) had only one hepatic cyst while the evaluations showed the remaining to have several cysts. The cysts’ size ranged from minimum of 2 cm to a maximum of 32 cm with the average number of 12 cm. A biliary fistula and daughter cysts in extra-hepatic ducts were find in 44 (33%) and 19 patients (13%) respectively. Other patient’s demographics are listed in Table 2.
There was a passage between thoracic cavity and the cyst through diaphragm in 4 patients (3%). There was more than one location of cysts, other than liver, in 17 patients (13%); 10 splenic hydatid cyst and 7 peritoneal one.
The conservative therapy was performed on 71 patients (53%) and the radical surgery on 64 ones (47%). In 50 out of these 71 patients the remaining cavity closed using capitonage maneuver and in the rest of them parts of external layer of the cyst which laid out of hepatic tissue were omitted, then the remaining cavity was drained out. We did not use any of the procedures such as omentoplasty, cyst—jejunum anastomosis, or marsupialization in this study.
51 out of 64 patients who were treated with radical surgery underwent cystectomy. The liver was resected in a wedge pattern in 7 cases in whom the cyst was small in size and located peripherally. A hepatic lobectomy was performed in six cases; two of them because of cyst multiplicity in a single lobe, and four of them due to the cyst which had taken the entire hepatic lobe space up. The cyst wall was omitted in all patients and those with residuals were excluded from the study.
An intra-operative cholangiography would be performed if clinical or intra-operative findings were suggesting involvement of biliary tract in either group, radical or conservative. Should see any passage between cyst and biliary system, it would be closed by absorbable sutures, a cholecystectomy performs and a drain would be placed through cystic duct.
16 cases out of 19 in which the cyst had been ruptured into the biliary tract along with daughter cysts and/or pieces of cyst wall in common bile duct faced a choledoctomy and T-tube insertion. Among those, seven patients needed trans-duodenal sphincterotomy as well. Thoraco-laparotomy was performed on 4 patients whose cyst has been drained in the right pleural cavity; 2 of them with only a cyst drained into the pleural cavity and 2 of them with the cyst fistulized into the pulmonary parenchyma whom had to face a pulmonary lobectomy as well.
Having other cysts in peritoneal cavity consistence to the hepatic cyst, those should be treated in the same time. Ten have undergone splenectomy and 7 had total peritoneal resection of cysts.
The post-operative mortality rate (in a 30 day post-operatively interval) was 2.2 % (3 out of 135). One in radical surgery group died because of anaphylactic shock intra-operatively, and 2 from conservative group due to acute cholangitis and hepato-renal syndrome during days 8 to 12 after the operation.
The mean complication rate was 23.7% (32 patients) consisting 28% of conservative’ group and 19% in radical surgery group (Table 3); 7 cases needed re-operation (2 in radical group and 5 in conservative group) because of hemorrhage and infection.
The average duration of draining was 8 ± 1.9 days in conservative group and 3 ± 0.9 days in radical one (Table 2).
The mean hospital stay time measured to be 5 ± 1.5 days in radical group, and 15 ± 3.1 days in conservative one (Table 2).
During 5 years of following up 13 cases (10.8%) of recurrence after the primary operation were detected in which 10 of them were in conservative group and 3 in radical surgeries. The recurrence in 10 patients was in the original site while 3 had the recurrence in a different location. All of these 13 cases were those whose primary cysts had several daughter cysts.
Discussion
Hydatid cyst is one of the challenging health problems in endemic countries.[1, 2, 11] The symptoms would show up when the cyst is in such a size that pushes adjacent structures or when it is complicated.[2, 16, 17] Abdominal pain would be the most common sign, as it is so in our study as well.[2, 17, 18]
Some proposed remedies for hydatid cyst consist of medical therapy, percutaneous drainage, and surgery; the inadequacy of effects in medical therapy and the complications of percutaneous drainage make the surgical approach to be the main effective treatment. [16, 17, 19]
The surgical approaches divide in two main categories; radical one and conservative’s, although the operation of choice is controversial. Those who believe in the radical approach (total removal of cyst) credit its less post-operative complications and recurrence. [7, 15, 20]
Bulber’s et al [11] concluded that outcomes were the same in both approaches but according to Smiths-Mtisen’s et al [21] the radical approach had more complications. Our study showed the complication rate to be as high as 28% in conservative approach and 19% in the radical one. The most common complication reported in hydatid cyst operation is bile leakage, more than 50% in some studies. [22, 23]
The main cause of bile leakage is abnormal path between the cyst and biliary tracts. After cyst drainage a pressure gradient makes bile flow direction to change from duodenum to the cyst cavity [24] and if not drained perfectly leads to an abscess in the remained cavity, biloma, or peritonitis. [7, 20]
As there might be tiny path between the cyst and biliary tracts, which would not be evaluated during conservative approach and keep hidden, an external biliary fistula formation is more probable compared to the radical approach in which the connections are more noticeable and will be legated easier.[6, 24] Demirci et al treated 260 cases of hepatic hydatid cysts using either radical or conservative approach, with a biliary leakage rate of 3.5% and 27.5% respectively.[25] In another study performed in Spain they reported biliary leakage as the most common post operative complication among 372 cases of hepatic hydatid cyst with a rate of 4.3% in those who underwent a radical approach and 25.6% in conservative one.[6]
In this study, Biliary leakage was reported not to be statistically significant different using exact fisher test (p = 0.47) between the two groups of conservative (14%) and radical (6%).
Local recurrence is another important part of surgical treatment of hepatic hydatid cyst which rate has been reported to be 1.1 to 9.6% in several studies. [6, 24]
Finding the exact mechanisms of daughter cyst formation put some lights on this problem. By gradual swelling of hydatid cyst, small particles of the inner layer dissent into the cyst cavity, helping daughter cyst formation. [24] The rate of daughter cyst formation has been reported to be around 29.5%.[26] Germinative layer advances toward the external layer (adventitia) by chance, which leads to some daughter cyst formation outside the cyst inner cavity known as exogenous daughter cyst (EDC). Among 64 cases in our study we had 12 cases of EDC (19%).
The EDCs if not treated are one of the disease recurrence causes which might not be visible if the external layer would not been removed entirely. That is why the radical approach is more acceptable than the other methods based on the recurrence rate. [12–14, 24] That is so obvious in our study as 9 out of total number of 10 local recurrence cases, were treated using the conservative approach. There was one case that had undergone a radical surgery and still met a recurrence, which probably was because one part of his external cyst layer was not completely excised due to cyst adhesion to vessels. Based on exact Fisher test there was a statistically significant difference between the local recurrence rate in two groups; 12.5% in conservative group (9 out of 71 cases), and 1.5% in the radical one (1 out of 64 cases) (P = 0.019).
The hospital stay was longer in conservative group than the radical one in this study (P < 0.05). This is compatible with the other studies, and expresses lesser hospital stay time in radical approach [6, 9, 10, 24] which could be due to longer draining (Table 2), more biliary fistulization, and more complication in conservative group compared to the radical one.
Furthermore, we compared the operation time which was longer in radical group than the conservative one (P < 0.05) probably as a consequence of more complex procedures accomplished in radical one.
Although the complication rate was higher in conservative group but this difference was not statically significant (P = 0.228).
It should be mentioned that in this study the limitation of patient selection might have influenced the final results by the meaning of a selection bias, e.g. impossible radical resection due to specific anatomical location (liver hilum), or diffuseness and multiplicity of cysts.
Local recurrence and hospital stay time in radical approach are lesser compared to conservative one; by the way for choosing the appropriate approach, important factors are needed to be concern, those such as the cyst’s location, size, number, relation to biliary tract and vessels, and for sure the surgeon’s experience.
References
Balik AA, Basoğlu M, Celebi F, Oren D, Polat KY, Atamanalp SS, Akçay MN (1999) Surgical treatment of hydatid disease of the liver: review of 304 cases. Arch Surg 134:166–169
Safioleas MC, Misiakos EP, Kouvaraki M, Stamatakos MK, Manti CP, Felekouras ES (2006) Hydatid disease of the liver. Arch Surg 141:1101–1108
Smego RA Jr, Sebanego P (2005) Treatment options for hepatic cystic echinococcosis. Int J Infect Dis 9:69–76
Avgerinos ED, Pavlakis E, Stathoulopoulos A, Manoukas E, Skarpas G, Tsatsoulis P (2006) Clinical presentations and surgical management of liver hydatidosis: our 20 year experience. HPB 8:189–193
Buttenschoen K, Schorcht P, Reuter S, Kern P, Carli Buttenschoen D, Henne-Bruns D (2004) Surgical treatment of hepatic infections with Echinococcus granulosus. Z Gastroenterol 42:1101–1108
Priego P, Nuño J, López Hervás P, López Buenadicha A, Peromingo R, Díe J, Rodríguez G (2008) Hepatic hydatidosis. Radical vs. conservative surgery: 22 years of experience. Rev Esp Enferm Dig 100:82–85
Vagenas C, Spyropoulos C, Stratis C, Maroulis J, Ce V (2006) Surgery for hepatic hydatidosis endoscopic treatment of complications. Arch Hellen Med 23:351–358
Dziri C, Haouet K, Fingerhut A (2004) Treatment of hydatid cyst of the liver: where is the evidence? World J Surg 28:731–736
Tasev V, Dimitrova V, Draganov K, Bulanov D, Popadiin N, Gaĭdarski R (2002) Hepatic echinococcosis: radical or conservative surgical treatment. Khirurgiia 58:10–13
Chautems R, Buhler L, Gold B, Chilcott M, Morel P, Mentha G (2003) Long term results after complete or incomplete surgical resection of liver hydatid disease. Swiss Med Wkly 133:258–262
Bülbüller N, Ilhan YS, Kirkil C, Yeniçerioğlu A, Ayten R, Cetinkaya Z (2006) The results of surgical treatment for hepatic hydatid cysts in an endemic area. Turk J Gastroenterol 17:273–278
Magistrelli P, Masetti R, Coppola R, Messia A, Nuzzo G, Picciocchi A (1991) Surgical treatment of hydatid disease of the liver. A 20-year experience. Arch Surg 126:518–522
Cangiotti L, Giulini SM, Muiesan P, Nodari F, Begni A, Tiberio G (1991) Hydatid disease of the liver: long term results of surgical treatment. G Chir 12:501–504
Karavias DD, Vagianos CE, Bouboulis N, Rathosis S, Androulakis J (1992) Improved techniques in the surgical treatment of hepatic hydatidosis. Surg Gynecol Obstet 174:176–180
Moreno González E, Jover navalón JM, Landa García JI, Moreno Azcoíta M, Silecchia G, Gómez Gutiérrez M, Arias Díaz J (1985) Surgical management of liver hydatidosis. 10-year experience with 269 patients. Ital J Surg Sci 15:267–273
Angelica MD, Fong Y (2007) The Liver. Sabiston Textbook of Surgery, 18th ed. Saunders pp 1494–1496
Christians KK, Pitt HA (2007) Hepatic abscess and cystic disease of the liver. Maingots abdominal operations, 11th ed. McGraw Hill pp 768–774
Gourgiotis S, Stratopoulos C, Moustafellos P, Dimopoulos N, Papaxoinis G, Vougas V, Hadjiyannakis E (2007) Surgical techniques and treatment for hepatic hydatid cysts. Surg Today 37:389–395
Alonso Casado O, Moreno González E, Loinaz Segurola C, Gimeno Calvo A, González Pinto I, Pérez Saborido B, Paseiro Crespo G, Ortiz Johansson C (2001) Results of 22 years of experience in radical surgical treatment of hepatic hydatid cysts. Hepatogastroenterology 48:235–243
Agarwal S, Sikora SS, Kumar A, Saxena R, Kapoor VK (2005) Bile leaks following surgery for hepatic hydatid disease. Indian J Gastroenterol 24:55–58
Schmidt-Matthiesen A, Schott O, Encke A (2002) Surgery and long term follow-up of hepatic echinococcosis outside endemic regions. Z Gastroenterol 40:51–57
Yildirgan MI, Başoğlu M, Atamanalp SS, Aydinli B, Balik AA, Celebi F, Oren D (2003) Intrabiliary rupture in liver hydatid cysts: results of 20 years’ experience. Acta Chir Belg 103:621–625
Kayaalp C, Bzeizi K, Demirbag AE, Akoglu M (2002) Biliary complications after hydatid liver surgery incidence and risk factors. J Gastrointest Surg 6:706–712
Yüksel O, Akyürek ŞT, Salman B, Azili C, Bostanci H (2008) Efficacy of radical surgery in preventing early local recurrence and cavity-related complications in hydatid liver disease. J Gastrointest Surg 12:483–489
Demirci S, Eraslan S, Anadol E, Bozatli L (1989) Comparison of the results of different surgical techniques in the management of hydatid cyst of the liver. World J Surg 13:88–91
Voros D, Kalovidouris A, Gouliamos A, Vlachos L, Danias N, Papadimitriou J (1999) The real incidence of extracapsular (satellite) cysts of liver echinococcus. HPB Surg 11:249–252
Acknowledgement
We are very grateful to Ms. M. Hassanpour for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Motie, M.R., Ghaemi, M., Aliakbarian, M. et al. Study of the Radical vs. Conservative Surgical Treatment of the Hepatic Hydatid Cyst: A 10-Year Experience. Indian J Surg 72, 448–452 (2010). https://doi.org/10.1007/s12262-010-0163-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-010-0163-8