Abstract
Objective
The objectives of this paper are to examine the effect of chronic intermittent hypoxia (CIH) on the morphological changes in the kidney of growing rats and to explore the mechanisms underlying the CIH-induced renal damage.
Methods
Forty Sprague-Dawley rats were randomly divided into two groups: 2 and 4 weeks CIH groups (2IH, 4IH), and in the control group 2 and 4 weeks air-stimulated groups (2C, 4C), with 10 rats in each group. Pathological changes of renal tissue were observed by HE staining, PAS staining, and Masson staining. Real-time PCR method was used to detect the mRNA expression of HIF-1α, CuZnSOD/ZnSOD, and MnSOD in renal tissue.
Results
(1) Intermittent hypoxia (IH) caused morphological damage in the kidney. Hypertrophy of epithelial cells in the kidney tubules and dilation in the glomeruli were observed under light microscope in HE and PAS stain, especially in 4IH group. Masson staining showed no significant fibrotic response in the IH groups. (2) Compared with the corresponding control groups, the levels of serum SOD were significantly lower in CIH groups, and especially in 4IH group. The mRNA expression of Cu/ZnSOD and MnSOD in CIH groups decreased significantly as compared to control groups. The mRNA levels of HIF-1α in the kidney were significantly higher in CIH groups than those in the corresponding control groups.
Conclusion
Oxidative stress played a critical role in renal damage by up-regulating HIF-1α transcription and down-regulating Cu/ZnSOD and MnSOD transcription after chronic intermittent hypoxia exposure in growing rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea hypopnea syndrome (OSAHS) is the most common type of sleep-disordered breathing associated with excessive daytime sleepiness, snoring, recurrent oxyhemoglobin desaturations, and arousals from sleep [1]. It is characterized by recurrent episodes of airway collapse during sleep. The prevalence of OSAHS in children in the clinic is not unusual; an epidemiological survey in 2007 showed that the prevalence of OSAHS in children was 2% [2]. Another epidemiological survey in Hong Kong in 2010 showed that the OSAHS prevalence rate among school-age children was at 3.8% for girls and 5.8% for boys [3]. Children are a susceptible group, as they are in growth and development period; their tissues and organs demand more oxygen than adults, therefore they are more sensitive to hypoxia. So, the impact of OSAHS on children is of more importance; it can occur in newborns till adolescents at any stage, but more commonly in preschool children.
OSAHS involves multiple system dysfunctions such as the cardiovascular, respiratory, digestive, genitourinary, endocrine, vascular, neurodevelopmental, and muscular system and also participates in retinopathy of prematurity and impaired growth [4,5,6,7,8,9,10,11]. In our previous studies, we found that nervous system injury and cognitive dysfunction were more common in children with OSAHS [12, 13]. There are ample evidence that inflammatory responses to the perturbations associated with OSAHS trigger a variety of genes and signaling cascades that ultimately lead to end-organ injury and changes in the kidney function and protein expression. It can also cause renal damage which has been clinically confirmed [14, 15]. The kidney is a high blood flow, high-perfused organ; its oxygen supply and oxygen tension changes are more sensitive, thus vulnerable to hypoxic injury [16]. Renal function, proteinuria, and renal tubular dysfunction are mainly nocturnal, but its molecular mechanism remains unclear. Repeated hypoxia and re-oxygenation, similarly to ischemia and reperfusion, causes cell mitochondria to produce more reactive oxygen species (ROS), therefore resulting in oxidative stress which is an important pathophysiological mechanism of renal damage caused by OSAHS. The aim of this study was to test the hypothesis that oxidative stress played an important role in the pathogenesis of CIH-associated renal damage in growing rats.
Materials and methods
This study was authorized by the Ethics Committee of Wenzhou Medical University. SPF Sprague-Dawley (SD) rats were purchased from Experimental Animal Center of Wenzhou Medical University. The design, preparation of intermittent low oxygen stainless steel chamber, compressed oxygen (concentration > 99.5%), high purity compressed nitrogen (concentration > 99.99%), and compressed air were purchased from Wenzhou Medical oxygen plant filling.
Animal model of OSAHS and experimental groups
Animal grouping of SPF SD male rats, weighing between 90 and 110 g, and aged 3–4 weeks; 40 rats were randomly divided into 4 groups by the method of random number table so that the number in each group was 10 and named as follows: chronic intermittent hypoxia (IH) for 2 weeks and 4 weeks group (2IH, 4IH) and control group 2 and 4 weeks (group 2C, 4C). Rats excluding the control groups were laid in intermittent hypoxia cabin, an automated alternate nitrogen/oxygen gas delivery system (Scientific research center of Wenzhou Medical University, Zhejiang, China) to deliver hypoxia/re-oxygenation. There were two durations of chronic intermittent hypoxia (CIH) which were studied: 2 weeks (2IH) and 4 weeks (4IH).
Intermittent hypoxia exposure
Establishment of CIH animal model was according to Wang Y [17] with modifications. To generate IH and air control, a steel cabin was created with an automated nitrogen/oxygen gas delivery system to deliver hypoxia/re-oxygenation using our previously described protocol [18]. Briefly, the experimental parameters were set as follows: O2 concentration could be reduced to a nadir of 9% ± 1.5% in 30 s by infusion of 99.99% nitrogen with the pressure kept at 0.3 KPa, stabilized at that level for 30 s, and then gradually increased to 21.0 ± 0.5% over the next 12 s by infusion of 99.50% oxygen (25 L/min) into the cabin. The oxygen concentration in the tank was maintained at 9% ± 1.5% in the hypoxia phase and in the re-oxygenation was maintained at 21.0% ± 0.5%, and the concentration of CO2 in the tank was less than 0.01%.This process was computer controlled. This cycle was repeated every 90 s over 7.5 h (from 8:00 to 15:30) during the animals’ diurnal sleep period for certain days according to the experimental design. The control groups were placed in cabin filled with compressed air for 2 weeks as 2C group or for 4 weeks as the 4C group, respectively. The O2 concentration was kept at 21.0 ± 0.5% in the control cabin. Ambient temperature was kept at 22–24 °C and humidity 40~50%. At the end of each day, the rats were grouped in additional cages, which were illuminated with fluorescent lamps to simulate daytime conditions. The rat’s activity and diet were ad libitum.
Test of the chronic intermittent hypoxia cabin
Validation of the CIH cabin was carried out before this experiment. Ten rats were anesthetized with 35 mg/kg pentobarbital (Sigma, USA) through intraperitoneal injection. The carotid artery was then catheterized using a catheter with heparin anticoagulation, which was inserted in the left carotid artery and sutured in place. When the rats recovered from surgery, 5 rats were randomly chosen and put individually in the CIH cabin and the other 5 in the control cabin. The experimental protocol was performed for 2 hours. The blood samples were collected at 22.5-s intervals during a single IH cycle continuous blood for 5 times, every <3 s, with the initial nitrogen gas input as the first sample, respectively. Arterial blood samples (0.5 ml) were collected in a 5-gauge needle at the end of each consecutive condition and immediately analyzed using a blood gas analyzer (GEM Premier 3000; America).
Specimen collection
Four rats in each group were anesthetized; thoracotomy with separation of the heart was performed to collect 5 mL of arterial blood which was refrigerated in a temperature of 4 °C for 2 h. Subsequently, the arterial blood was centrifuge at 4 °C 4000rpm for l5 min and the serum was preserved at − 80 °C in refrigerator. The serum was then used to detect total superoxide dismutase (SOD) activity. The remaining 6 rats were afterwards anesthetized by intraperitoneal injection of 3% phenobarbital sodium (40 mg/kg). Laparotomy was done to expose the left and right kidneys. The renal vein was injected with pre-cooled saline. The right and left kidneys were collected when it became pale. The left kidney was placed on an ice plate. The right kidney was fixed in 4% paraformaldehyde solution.
Renal histopathological staining
HE staining, PAS staining, and Masson staining
The tissue sections were paraffin-embedded and 4-μm sections were used. The sections were routinely dewaxed with xylene, washed with ethanol at all levels, and stained with HE, PAS, and Masson, respectively. Tissue samples from the kidneys were scored histopathologically. Pathological scoring (0–4) was used to assess the degree which was defined as glomerular swelling, renal tubular epithelial cell swelling, mesangial proliferation, and glomerular and interstitial fibrosis. Counts were performed in at least 10 different fields of square micrometers, using scores on a scale of 0 (< 5%), 1 (5–25%), 2 (25–50%), 3 (50–75%), and 4 (> 75%). The severity of each injury was assessed by 0~4 scores: 0 = minor damage, 1 + = mild damage, 2 + = moderate damage, 3 + = severe damage, and 4 + =serious damage. All the above four pathological scores were added into 0~16 points.
Real-time PCR
The expression of HIF-1α, Cu/Zn-SOD, and MnSOD mRNA in the left kidney was detected by real-time PCR. Total RNA was extracted from the renal tissue using the Trizol reagent according to manufacturer’s instructions. The RNA was purified and quantified by RNAi, reverse transcribed into cDNA, and amplified using a PCR amplification apparatus. PCR reaction conditions were 95 °C 5 min; 95 °C 10 s, 60 °C 10 s, 72 °C 10 s, and 45 cycles of amplification. β-actin was used as an internal control by previous work [12]. β-actin, HIF-1α, Cu/Zn SOD, and MnSOD primer sequences were designed and synthesized by Shanghai Shengong Bioengineering Co. Ltd., and the sequences were as follows: HIF-1 α: upstream 5′-TGAACATCAAGTCAGCAACG-3′, downstream: 5′-CACAAATCAGCACCAAGCAC-3′, Cu/ZnSOD: upstream 5′-GTGGTGGAGAACCCAAAGGA-3′, downstream 5′-GCGTGCTCCCACACATCAAT-3′, MnSOD: upstream 5′-ATGGGGACAATACACAAGGC-3′, downstream 5′-TCATCTTGTTTCTCGTGGAC-3′, β-actin: upstream 5′-TCACCAACTGGGACGATATG-3′, and downstream 5′-GTTGGCCTTAGGGTTCAGAG-3′. The relative expression of the target gene was calculated according to the formula 2−ΔCt (ΔCT = Ct value of the target gene−Ct value of the internal reference gene) using β-actin as the internal reference gene using Lightcycler48015.0 software.
Determination of SOD
The hydroxylamine oxidation method was used to detect the activity of SOD. All experimental procedures were performed according to the manufacturer’s instructions (kit assay, Jiancheng Limited Company, Jiangsu China). UV spectrophotometric colorimetry was used to detect the absorbance of the sample at 550 nm. Enzyme values are presented as U/ml.
Statistical analysis
In addition to the renal pathological score, all groups were normal measurement data; with the mean + standard deviation (\( \overline{X} \) ±SD), the renal pathological scores were expressed as a median, with SPSS 21 statistical software processing. Renal pathological scores were examined by Kruskal-Wallis test. Other data were compared using multiple factor analysis of variance (two-way ANOVA), if the variance was homogeneous the LSD test was used, and if not, Dunnett’s T3 test was used to test the variance. The differences were considered significant if P values were < 0.05.
Results
Blood gas analysis
Blood gas analysis in rats was made in order to validate the CIH cabin. The result showed that over the course of the IH event for 2 h, the PaO2 fluctuated from 44 ± 3 to 80 ± 9 mmHg and SaO2 from 75 ± 3 to 95 ± 1 mmHg, respectively, in a cycle of 90 s. The PaO2 and SaO2 in control group exhibited no significant difference among the five time points. The magnitude of oxygen saturation that was induced in our model was consistent with the degree of hypoxia that occurs in moderate to severe OSAHS [19, 20].
Histopathological changes in each group
HE
The structure of glomerular and tubular epithelial cells was normal in 2C and 4C groups. There was mild hyperplasia of glomerular mesangial cells in IH groups. Compared to the 2IH group, the 4IH group had significant changes such as glomerular and renal cysts and renal tubular epithelial cell swelling (Fig. 1).
PAS staining
There was no significant thickening of the glomerular basement membrane, mesangial and no loss of the tubular epithelial cell brush border in the 2C and 4C groups. In the IH groups, glomerular basement membrane was slightly thickened, the brush border structure of renal tubular epithelial cells were incomplete, and the damage in the 4IH group was significantly higher than that of the 2IH group, as shown in Fig. 2.
Masson staining
No blue collagen fibers were identified in the glomerular and tubulointerstitial tissues neither in the IH groups nor the C groups as shown in Fig. 3.
Pathological score
In the four groups (n = 6), it showed that the IH group (4IH group was 5, 2IH 3) had more severe pathological damage compared to air control group (2C and 4C group were 0.5) and the difference was statistically significant (P < 0.05).The pathological damage of the 4IH group was more obvious than that of the 2IH group (P < 0.05), and the pathological damage was serious; the difference was statistically significant (P < 0.05) (refer to Table 1).
The mRNA expression of HIF-1α, MnSOD, and Cu/ZnSOD in the kidney tissues of each group was observed
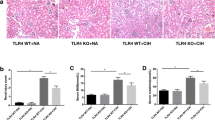
Effect of IH on expression of HIF-1α (Fig. 4 and Table 2)
IH had significant effect on the expression of HIF-1αmRNA (F = 151.683. P < 0.001) and the time effect (F = 42.693, P < 0.001). The interaction between the treatment and the time effect was also significant (F = 52.212, P < 0.001). The expression of HIF-1αmRNA in the renal tissue of 2IH group was increased (P < 0.05) compared to the 2C group, similarly for the 4IH group compared to the 4C group (P < 0.05). The expression of the 4IH group was significantly higher than the 2IH group (P < 0.05).
The level of HIF-1α, Cu/ZnSOD, and MnSOD mRNA expression. a, b, c, d Real-time quantitative PCR was used to detect the expression of HIF-1α, Cu/ZnSOD, MnSOD, and SOD in kidney mean±SD. Statistically significant differences are indicated by ▲P < 0.05 vs 2C group; ■P < 0.05vs 4C group; ★P < 0.05 vs 2IH group
Effect of IH on expression of MnSOD (Fig. 4 and Table 2)
IH had significant effect on the expression of MnSOD mRNA (F = 108.613 P < 0.001). The time effect (F = 1.390, P > 0.05) and the interaction between treatment and the time effect was not significant (F = 2.551, P > 0.05). The expression of MnSOD mRNA of the 2IH was lower than that of 2C (P < 0.05); likewise, the 4IH group compared to 4C was significantly decreased (P < 0.05), but the 4IH compared to 2IH had no significant difference (P > 0.05).
Effect of IH on expression of Cu/ZnSOD (Fig. 4 and Table 2)
IH had significant effect on the expression of Cu/ZnSOD mRNA (F = 107.511 P < 0.001). The time effect (F = 3.912, P > 0.05) and the interaction between treatment and the time effect was not significant (F = 0.676, P > 0.05). The expression of Cu/ZnSOD mRNA in 2IH and 4IH groups were lower than those in 2C and 4C groups (P < 0.05), but there was no significant difference between 4IH group and 2IH group (P > 0.05) and 2C and 4C (P > 0.05).
Determination of serum SOD activity (Fig. 4 and Table 2)
2IH and 4IH groups’ serum SOD activity were lower than the control groups 2C and 4C (P < 0.05); 4IH group was significantly lower than 2IH group (P < 0.05); 2C and 4C groups were not statistically significant (P > 0.05).
Discussion
OSAHS is a multi-system functional disorder with intermittent hypoxia and sleep fragmentation as its main pathophysiological mechanism resulting in nocturnal apnea. The process of hypoxia-re-oxygenation is similar to the pathological process of ischemia-reperfusion injury (IRI), which can result in oxidative stress and free radical production. Long-term accumulation leads to multi-system organ damage. In the study of the molecular mechanism of cardiovascular disease and cognitive impairment in OSAHS, oxidative stress is considered to be one of the major mechanisms of injury [21,22,23]. In IRI, oxidative stress is the most common molecular mechanism of cell destruction and relatively low concentration of antioxidant enzymes makes it more susceptible to oxidative stress injury [16].
OSAHS-associated renal damage has been clinically confirmed [24, 25] mainly for chronic kidney disease, nocturnal polyuria, renal functional changes, proteinuria, renal tubular dysfunction, etc. In animal model of CIH [26, 27], it has been found that OSAHS can cause kidney tissue structure, ultrastructure, and proteomics changes, but the studies were performed on adult animals. It is still unclear whether OSAHS can cause similar changes in the children; therefore, we design a self-developed computer-controlled intermittent hypoxic oxygen chamber to study the effects of OSAHS on renal tissue in 3- to 4-week-old SD rats. The test for the hypoxia cabin confirmed that the magnitude of oxygen saturation that was induced in our model of IH was equivalent to the pathophysiological changes of moderate to severe intermittent hypoxia exposure.
In our study, we did not investigate mild OSAS but Butchner et al. [28] and Wissing et al. [29] investigated mild to moderate OSAS and its treatment on renal hemodynamics assessed by the renal resistance index. They found in multivariate analyses that the renal resistance index was independent of hypertension, diabetes mellitus, age, and baseline renal function. Their study demonstrated an impairment of renal hemodynamics in OSAS. These changes in renal blood flow may identify OSAS patients who are at risk of declining renal function. Further studies are warranted to determine OSAS’s direct influence on renal impairment in children.
Previous studies demonstrated that proximal tubule epithelial cells were one of the most vulnerable cells in IRI in the kidney [30, 31]. In this study, there were pathological changes of renal tissue; mainly in the IH group, mild hyperplasia of glomerular mesangial cells, edema of the renal tubular epithelial cells, and loss of complete brush border structure were identified. At the same time, glomerular changes were confirmed by PAS staining. Chronic hypoxia is a key factor in renal interstitial fibrosis. In this study, renal tissue fibrosis was not identified in neither 2 weeks nor 4 weeks IH group in Masson staining, but Sun et al. [32] and other studies in adult mice showed that after 8 weeks of IH exposure, there were significant decrease of antioxidant levels and significant increases of renal inflammation, oxidative damage, cell death, and renal fibrosis, suggesting the severity of renal fibrosis by IH depending on the length of time and the degree of hypoxia.
The mechanism of hypoxia in OSAHS is similar to that of IRI, which is characterized by CIH and different durations of hypoxia, which is a more serious type of hypoxia. Gozal et al. exposed (pheochromocytoma-12, PC12) pheochromocytoma cells to continuous hypoxia (5%O2) and intermittent hypoxia (hypoxia 5%O2 35 min, 21% O2 21 min) 2 to 4 days; they found that 2 days exposure to IH can lead to cell apoptosis [33]. HIF-lα is a transcription factor that regulates oxygen balance. It is a heterogeneous two polymer structure composed of oxygen-sensitive alpha subunit and stably expressed beta subunit. The content of HIF-1α in the local tissue can indirectly reflect the hypoxia of tissue cells. Continuous hypoxia increased the expression of HIF-1α through mediating hypoxic adaptive response. IH also upregulated HIF-1α expression, but the signal transduction pathway was different from that of continuous hypoxia [34]. Da Rosa et al. [35] found that HIF-1 alpha protein was upregulated in lung tissue and liver in CIH. Therefore, the expression of HIF-1 alpha mRNA in renal tissue can reflect the renal anoxia in CIH condition. In this study, real-time quantitative PCR was used to detect hypoxia-related HIF-1αmRNA expression in renal tissue, which showed that the expression of HIF-1αmRNA was upregulated in a time-dependent manner, therefore indicating that hypoxia occurred in the kidney tissue.
A number of clinical studies show a decrease in oxidative stress [21, 36, 37] and anti-oxidative capacity in patients with OSAHS [38]. SOD is the first in vivo antioxidant enzyme reaction. Cu/Zn superoxide dismutase (copper-zinc superoxide, dismutase, Cu/ZnSOD) and manganese superoxide dismutase (manganese superoxide, dismutase, MnSOD) are the main two types. Cu/ZnSOD was mainly expressed in the cytoplasm and MnSOD was mainly located in the mitochondria. In our previous study, we found out that the level of 8-ISO-PGF2α, an in vivo oxidative stress marker, was significantly high in the CIH groups compared to the corresponding control groups, therefore suggesting that CIH induced oxidative stress injury [18]. In this study, the total SOD activity in serum of CIH rats was determined by chemical colorimetry; we found that SOD activity was decreased, which was negatively correlated with time, and the results showed the antioxidant capacity decreased in CIH SD rats. Real-time fluorescence quantitative detection showed that the expression of Cu/ZnSOD and MnSODmRNA in renal tissue was downregulated, which indirectly indicated that IH induced oxidative stress in renal tissue. Nanduri et al. [39] also showed that PC12 cells were mainly downregulated by IH after MnSOD expression, whereas other antioxidant enzymes were unchanged. These results suggest that IH exposure mainly results in downregulation of MnSOD expression. In this study, the expression of Cu/ZnSOD in the cytoplasm of IH group was lower than the control group. The hypoxia time was prolonged and the expression of MnSOD in the mitochondria was downregulated in CIH rats, which indicated oxidative stress played a critical role in renal damage CIH rats.
Our study had limitations. Firstly, our model of intermittent hypoxia does not entirely represent all of the events that occur during obstructive sleep apnea. Intermittent hypoxia does not cause negative intrathoracic pressure swings or obstruction of the airway. Second, we used 2 weeks and 4 weeks exposure to intermittent hypoxia which cannot predict if the changes in mRNA expression we found would be maintained or augmented with a longer exposure. Third, we only analyzed gene but it would have been better to analyze protein also in the kidney tissue. By immunohistochemistry, we could confirm that Cu/ZnSOD is mainly expressed in the cytoplasm, while MnSOD is mainly expressed in the mitochondria. Lastly, to better evaluate the kidney morphological changes, more stained sections should have been done.
Conclusion
In summary, oxidative stress played a critical role in renal damage by up regulating HIF-1α transcription and downregulating Cu/ZnSOD and MnSOD transcription after chronic intermittent hypoxia exposure in growing rats. Future research is needed to determine the clinical significance of these preliminary findings.
Abbreviations
- CIH:
-
chronic intermittent hypoxia
- OSAHS:
-
obstructive sleep apnea hypopnea syndrome
- HIF-1α:
-
hypoxia-inducible factor 1-alpha
- SOD:
-
superoxide dismutase
- Cu/ZnSOD:
-
copper-zinc superoxide dismutase
- MnSOD:
-
manganese superoxide dismutase
- PAS:
-
periodic acid–Schiff stain
- HE:
-
hematoxylin and eosin stain
- qRT-PCR:
-
real-time polymerase chain reaction
- ROS:
-
reactive oxygen species
- IRI:
-
ischemia reperfusion injury
References
Guilleminault C, Abad VC (2004) Obstructive sleep apnea syndromes. Med Clin N Am 88(3):611–630, viii. https://doi.org/10.1016/j.mcna.2004.01.002
Wildhaber JH, Moeller A (2007) Sleep and respiration in children: time to wake up! Swiss Med Wkly 137(49–50):689–694
Li AM, So HK, Au CT, Ho C, Lau J, Ng SK, Abdullah VJ, Fok TF, Wing YK (2010) Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study. Thorax 65(11):991–997. https://doi.org/10.1136/thx.2010.134858
Levy P, Tamisier R, Arnaud C, Monneret D, Baguet JP, Stanke-Labesque F, Dematteis M, Godin-Ribuot D, Ribuot C, Pepin JL (2012) Sleep deprivation, sleep apnea and cardiovascular diseases. Front Biosci (Elite Ed) 4:2007–2021
Schober AK, Neurath MF, Harsch IA (2011) Prevalence of sleep apnoea in diabetic patients. Clin Respir J 5(3):165–172. https://doi.org/10.1111/j.1752-699X.2010.00216.x
Badran M, Golbidi S, Devlin A, Ayas N, Laher I (2014) Chronic intermittent hypoxia causes endothelial dysfunction in a mouse model of diet-induced obesity. Sleep Med 15(5):596–602. https://doi.org/10.1016/j.sleep.2014.01.013
Bhattacharjee R, Kheirandish-Gozal L, Pillar G, Gozal D (2009) Cardiovascular complications of obstructive sleep apnea syndrome: evidence from children. Prog Cardiovasc Dis 51(5):416–433. https://doi.org/10.1016/j.pcad.2008.03.002
Serebrovskaya TV, Xi L (2015) Intermittent hypoxia in childhood: the harmful consequences versus potential benefits of therapeutic uses. Front Pediatr 3:44. https://doi.org/10.3389/fped.2015.00044
Martin RJ, Wang K, Koroglu O, Di Fiore J, Kc P (2011) Intermittent hypoxic episodes in preterm infants: do they matter? Neonatology 100(3):303–310. https://doi.org/10.1159/000329922
Martin RJ, Di Fiore JM, Macfarlane PM, Wilson CG (2012) Physiologic basis for intermittent hypoxic episodes in preterm infants. Adv Exp Med Biol 758:351–358. https://doi.org/10.1007/978-94-007-4584-1_47
Bass JL, Corwin M, Gozal D, Moore C, Nishida H, Parker S, Schonwald A, Wilker RE, Stehle S, Kinane TB (2004) The effect of chronic or intermittent hypoxia on cognition in childhood: a review of the evidence. Pediatrics 114(3):805–816. https://doi.org/10.1542/peds.2004-0227
Cai XH, Li XC, Jin SW, Liang DS, Wen ZW, Cao HC, Mei HF, Wu Y, Lin ZD, Wang LX (2014) Endoplasmic reticulum stress plays critical role in brain damage after chronic intermittent hypoxia in growing rats. Exp Neurol 257:148–156. https://doi.org/10.1016/j.expneurol.2014.04.029
Cai XH, Li XC, QQ H, CY Y, Zhou YH, MS S, Zhao YP, YL H, Wang LX (2013) Multiple system morbidities associated with children with snore symptom. Pediatr Pulmonol 48(4):381–389. https://doi.org/10.1002/ppul.22653
Verhulst SL, Van Hoeck K, Schrauwen N, Haentjens D, Rooman R, Van Gaal L, De Backer W, Desager KN (2008) Sleep-disordered breathing and proteinuria in overweight and obese children and adolescents. Horm Res 70(4):224–229. https://doi.org/10.1159/000151594
Krishna J, Shah ZA, Merchant M, Klein JB, Gozal D (2006) Urinary protein expression patterns in children with sleep-disordered breathing: preliminary findings. Sleep Med 7(3):221–227. https://doi.org/10.1016/j.sleep.2005.09.010
Eckardt KU, Rosenberger C, Jurgensen JS, Wiesener MS (2003) Role of hypoxia in the pathogenesis of renal disease. Blood Purif 21(3):253–257
Wang Y, Guo SZ, Bonen A, Li RC, Kheirandish-Gozal L, Zhang SX, Brittian KR, Gozal D (2011) Monocarboxylate transporter 2 and stroke severity in a rodent model of sleep apnea. J Neurosci 31(28):10241–10248. https://doi.org/10.1523/JNEUROSCI.1462-11.2011
Cai XH, Zhou YH, Zhang CX, LG H, Fan XF, Li CC, Zheng GQ, Gong YS (2010) Chronic intermittent hypoxia exposure induces memory impairment in growing rats. Acta Neurobiol Exp (Wars) 70(3):279–287
Lee EJ, Woodske ME, Zou B, O'Donnell CP (2009) Dynamic arterial blood gas analysis in conscious, unrestrained C57BL/6J mice during exposure to intermittent hypoxia. J Appl Physiol (1985) 107(1):290–294. https://doi.org/10.1152/japplphysiol.91255.2008
Morgan BJ (2009) Intermittent hypoxia: keeping it real. J Appl Physiol (1985) 107(1):1–3. https://doi.org/10.1152/japplphysiol.00304.2009
Jurado-Gamez B, Fernandez-Marin MC, Gomez-Chaparro JL, Munoz-Cabrera L, Lopez-Barea J, Perez-Jimenez F, Lopez-Miranda J (2011) Relationship of oxidative stress and endothelial dysfunction in sleep apnoea. Eur Respir J 37(4):873–879. https://doi.org/10.1183/09031936.00027910
Nair D, Dayyat EA, Zhang SX, Wang Y, Gozal D (2011) Intermittent hypoxia-induced cognitive deficits are mediated by NADPH oxidase activity in a murine model of sleep apnea. PLoS One 6(5):e19847. https://doi.org/10.1371/journal.pone.0019847
Khayat R, Patt B, Hayes D Jr (2009) Obstructive sleep apnea: the new cardiovascular disease. Part I: obstructive sleep apnea and the pathogenesis of vascular disease. Heart Fail Rev 14(3):143–153. https://doi.org/10.1007/s10741-008-9112-z
Chou YT, Lee PH, Yang CT, Lin CL, Veasey S, Chuang LP, Lin SW, Lin YS, Chen NH (2011) Obstructive sleep apnea: a stand-alone risk factor for chronic kidney disease. Nephrol Dial Transplant 26(7):2244–2250. https://doi.org/10.1093/ndt/gfq821
Nicholl DD, Ahmed SB, Loewen AH, Hemmelgarn BR, Sola DY, Beecroft JM, Turin TC, Hanly PJ (2012) Declining kidney function increases the prevalence of sleep apnea and nocturnal hypoxia. Chest 141(6):1422–1430. https://doi.org/10.1378/chest.11-1809
Ding W, Cai Y, Wang W, Ji L, Dong Y, Zhang X, Su M, Liu J, Lu G, Zhang X (2016) Adiponectin protects the kidney against chronic intermittent hypoxia-induced injury through inhibiting endoplasmic reticulum stress. Sleep Breath. https://doi.org/10.1007/s11325-016-1321-4
Abuyassin B, Sharma K, Ayas NT, Laher I (2015) Obstructive sleep apnea and kidney disease: a potential bidirectional relationship? J Clin Sleep Med 11(8):915–924. https://doi.org/10.5664/jcsm.4946
Buchner NJ, Wissing KR, Stegbauer J, Quack I, Weiner SM, Kramer BK, Rump LC (2011) The renal resistance index is increased in mild-to-moderate obstructive sleep apnoea and is reduced under continuous positive airway pressure. Nephrol Dial Transplant 26(3):914–920. https://doi.org/10.1093/ndt/gfq472
Wissing KR, Buchner NJ, Stegbauer J, Rump LC (2007) Renal resistance index in patients with obstructive sleep apnea. Dtsch Med Wochenschr 132(36):1815–1819. https://doi.org/10.1055/s-2007-984970
Bonventre JV, Yang L (2011) Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 121(11):4210–4221. https://doi.org/10.1172/JCI45161
Tirapelli LF, Barione DF, Trazzi BF, Tirapelli DP, Novas PC, Silva CS, Martinez M, Costa RS, Tucci S Jr, Suaid HJ, Cologna AJ, Martins AC (2009) Comparison of two models for evaluation histopathology of experimental renal ischemia. Transplant Proc 41(10):4083–4087. https://doi.org/10.1016/j.transproceed.2009.09.061
Sun W, Yin X, Wang Y, Tan Y, Cai L, Wang B, Cai J, Fu Y (2012) Intermittent hypoxia-induced renal antioxidants and oxidative damage in male mice: hormetic dose response. Dose Response 11(3):385–400. https://doi.org/10.2203/dose-response.12-027.Cai
Gozal E, Sachleben LR Jr, Rane MJ, Vega C, Gozal D (2005) Mild sustained and intermittent hypoxia induce apoptosis in PC-12 cells via different mechanisms. Am J Phys Cell Physiol 288(3):C535–C542. https://doi.org/10.1152/ajpcell.00270.2004
Yuan G, Nanduri J, Khan S, Semenza GL, Prabhakar NR (2008) Induction of HIF-1alpha expression by intermittent hypoxia: involvement of NADPH oxidase, Ca2+ signaling, prolyl hydroxylases, and mTOR. J Cell Physiol 217(3):674–685. https://doi.org/10.1002/jcp.21537
da Rosa DP, Forgiarini LF, Baronio D, Feijo CA, Martinez D, Marroni NP (2012) Simulating sleep apnea by exposure to intermittent hypoxia induces inflammation in the lung and liver. Mediat Inflamm 2012:879419. https://doi.org/10.1155/2012/879419
Westhoff M, Litterst P (2012) Obstructive sleep apnoea and oxidative stress. Pneumologie 66(10):610–615. https://doi.org/10.1055/s-0032-1325691
Ntalapascha M, Makris D, Kyparos A, Tsilioni I, Kostikas K, Gourgoulianis K, Kouretas D, Zakynthinos E (2013) Oxidative stress in patients with obstructive sleep apnea syndrome. Sleep Breath 17(2):549–555. https://doi.org/10.1007/s11325-012-0718-y
Katsoulis K, Kontakiotis T, Spanogiannis D, Vlachogiannis E, Kougioulis M, Gerou S, Daskalopoulou E (2011) Total antioxidant status in patients with obstructive sleep apnea without comorbidities: the role of the severity of the disease. Sleep Breath 15(4):861–866. https://doi.org/10.1007/s11325-010-0456-y
Nanduri J, Wang N, Yuan G, Khan SA, Souvannakitti D, Peng YJ, Kumar GK, Garcia JA, Prabhakar NR (2009) Intermittent hypoxia degrades HIF-2alpha via calpains resulting in oxidative stress: implications for recurrent apnea-induced morbidities. Proc Natl Acad Sci U S A 106(4):1199–1204. https://doi.org/10.1073/pnas.0811018106
Acknowledgements
This work was supported by Zhejiang Provincial Natural Science Foundation Grant (LY17H010004), Scientific Research Foundation of Health Bureau of Zhejiang Province (2018ZD010), Wenzhou City Science and Technology Bureau Grant (Y20170133), National Science-technology Support Program (2015BAI12B09), and Project of Key Innovative Disciplines of Children Sleep Medicine of Zhejiang.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Poonit, ND., Zhang, YC., Ye, CY. et al. Chronic intermittent hypoxia exposure induces kidney injury in growing rats. Sleep Breath 22, 453–461 (2018). https://doi.org/10.1007/s11325-017-1587-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1587-1