Abstract
Objective
Several studies suggest that obstructive sleep apnea syndrome (OSAS) is associated with oxidative stress. However, there are also contrary observations and the role of antioxidant mechanisms has not been fully explored.
Patients and methods
The present study evaluated serum total antioxidant status (TAS) in 32 OSAS patients without comorbidities, before and after a diagnostic sleep study and at a second sleep study after continuous positive airway pressure (CPAP) application.
Results
Lower TAS values were found in the morning, immediately after the first sleep study, compared with those before sleep (1.68 ± 0.11 vs. 1.61 ± 0.10 mmol/l, p < 0.01); this was evident in patients with less severe syndrome [apnea–hypopnea index (AHI) <30; 1.73 ± 0.08 vs. 1.65 ± 0.09 mmol/l, p = 0.01] but not in severe syndrome (AHI ≥30; 1.64 ± 0.12 vs. 1.58 ± 0.10 mmol/l, p = 0.07). After CPAP application, a statistically significant decrease in TAS values was observed in patients with less severe syndrome (1.72 ± 0.05 vs. 1.63 ± 0.04 mmol/l, p = 0.003). On the contrary, no statistically significant changes in TAS were observed in patients with severe syndrome.
Conclusions
The present study supports a reduction in antioxidant capacity during sleep in otherwise healthy patients with OSAS. This reduction was evident in less severe syndrome. However, a single night of CPAP application seems to ameliorate this antioxidant disturbance only in less severe syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is characterized by recurrent nocturnal obstruction of the upper airway. Patients with OSAS experience recurrent episodes of cessation of breathing which leads to hypoxia and reoxygenation. These repeated changes of oxygen saturation could be considered analogous to recurrent episodes of ischemia–reperfusion injury, which causes damage after the restoration of blood flow to ischemic or hypoxic tissues through increased generation of reactive oxygen species (ROS) [1, 2].
Oxidative stress is characterized by an imbalance between oxidant and antioxidant mechanisms, in which many different enzymatic and non-enzymatic antioxidants take place [3]. Increased generation of ROS in vivo can lead to the depletion of one or more antioxidants, and the loss of antioxidants can be measured as an index of oxidative stress [4]. Several studies have provided evidence supporting an increase of oxidative stress in OSAS, either as enhanced ROS production [5–7] or as increased lipid peroxidation products[8, 9].
However, there are also contradictory observations on oxidative stress and OSAS [10–13]. Several potential confounders, such as hypertension, ischemic heart disease, diabetes, and smoking, which are common comorbidities in OSAS patients, as well as the time of measurements, may influence final results. On the other hand, the role of blood antioxidants in OSAS patients has not been fully elucidated.
The aim of the present study was to evaluate the antioxidant status before and after sleep in strictly selected OSAS patients with no other comorbidities as well as the effect of continuous positive airway pressure (CPAP) treatment on antioxidant status. We tested the hypothesis that a possible increase in the oxidant burden in OSAS patients would have an impact on antioxidant status and treatment with CPAP would ameliorate this antioxidant disturbance. The influence of the severity of OSAS was additionally evaluated.
Materials and methods
Subjects
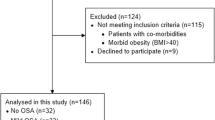
Seventy-six consecutive subjects with clinically suspected sleep apnea syndrome were screened through interviews and were evaluated for inclusion in this study. All subjects were referred for snoring, witnessed apneas, and excessive daytime sleepiness. Patients were included only if they suffered from OSAS (determined as apnea–hypopnea index >5 events/h of sleep), were non-smokers, and had no comorbidities. None of the participants was taking any chronic medication and none had suffered from an infection for 4 weeks prior to the inclusion in the study. Thirty-eight of the evaluated subjects fulfilled these inclusion criteria and only 32 males were enrolled as OSAS patients, after initial sleep study, while six patients refused to participate. Written informed consent was obtained from all patients and the protocol was approved by the Institutional Ethics Committee.
Sleep studies
All patients were studied by attended overnight polysomnography in the sleep laboratory of “Agios Pavlos” General Hospital, using the SOMNO screen system (SOMNOmedics GmbH and Co., Germany). We recorded central electroencephalogram, electrooculogram, submental, and bilateral leg electromyograms as well as electrocardiogram. A thermistor and a pressure sensor (nasal cannula) were used to monitor oronasal flow, a microphone to record snoring sounds, thoracic and abdominal piezoelectric belts to define respiratory efforts, a body position sensor to detect the patient’s position, and an activity monitor. A pulse oxymeter with a silicone-embedded finger probe was used for continuous recording of arterial oxyhemoglobin saturation. After the diagnostic sleep study, the patients received detailed information concerning CPAP treatment and the appropriate mask was chosen carefully. In order the patients to familiarize themselves with the device, a short CPAP trial during wakefulness was introduced. CPAP titration was performed with an Autoset device (Resmed; North Ryde, Australia). During CPAP titration, CPAP flow, CPAP pressure, and CPAP snore were assessed through a pressure transducer. All data were recorded continuously at 16 bit with an adjustable sampling rate up to 512 per second. Sleep stages were scored manually in 30-s epochs following Rechtschaffen and Kales criteria [14]. Episodes of absence of airflow for 10 s or longer in the presence of respiratory effort were defined as obstructive apneas. Episodes of clear reduction of airflow lasting for ≥10 s associated with either an oxygen desaturation of >3% or an arousal were defined as hypopneas [15]. The arousals were defined following the recommendations of Atlas Task Force [16]. Apnea–hypopnea index (AHI) was defined as the total events per hour of sleep.
Antioxidants measurements
Serum total antioxidant status (TAS) was measured using a commercially available kit (Randox Ltd., Crumlin, UK) based on a colorimetric method. In this method, incubation of 2,2′-azinobis-3-ethylbenothiazoline 6-sulfonate (ABTS®) with a peroxide (metmyoglobin) results in production of the radical cation ABTS+. This species is blue green in color and can be detected at 600 nm. Antioxidants in the added sample cause inhibition of this color production to a degree that is proportional to their concentration. A Daytona RX, Randox, analyzer was used for the measurement and the reagent was calibrated with the standards contained in the kit. Reproducibility, range error, and accuracy of the method according to the manufacturer are as follows:
1. Precision (reproducibility) | |||
Intra-assay | |||
Level 1 | Level 2 | Level 3 | |
Mean (mmol/l) | 1.11 | 1.76 | 2.43 |
SD | 0.03 | 0.06 | 0.07 |
CV (%) | 2.77 | 3.65 | 2.83 |
n | 20 | 20 | 20 |
Inter-assay | |||
Level 1 | Level 2 | Level 3 | |
Mean (mmol/l) | 1.11 | 1.86 | 2.28 |
SD | 0.07 | 0.05 | 0.06 |
CV (%) | 6.06 | 2.43 | 2.76 |
n | 20 | 20 | 20 |
2. Range error: 10.1% | |||
3. Accuracy: 0.21–2.94 mmol/l | |||
Study details
Anthropometric measurements of body mass index (BMI) and neck circumference as well as serum creatinine, total cholesterol, fasting blood glucose levels, and peripheral white blood cell counts were measured in all patients. Venous blood samples were drawn at 23:00 before polysomnography and at 7:00 just after waking in the morning. All study participants were readmitted for another one-night polysomnography under CPAP application, within 1 week of the diagnostic polysomnography. Venous blood samples were drawn at the same time as in the first study. Serum TAS was measured before and after the diagnostic sleep study plus before and after CPAP application. According to the severity of OSAS, defined as apnea–hypopnea index (AHI), they were divided in severe (AHI ≥30, n = 19) and less severe group (AHI <30, n = 13).
Statistical analysis
Results are expressed as mean ± SD. Paired t test was used for the comparison in measurements of antioxidants before and after polysomnography, as well as before and after polysomnography with CPAP application. Unpaired t test was used for comparing parameters before and after each sleep study in patients with severe and less severe syndrome. The Statistical Program for Social Science (SPSS version 17, Chicago, IL, USA) was used for the analysis.
Results
Subjects’ demographics and sleep characteristics are shown in Table 1. Measurements of TAS are shown in Table 2.
In the whole population, a statistically significant decrease in TAS after the first sleep study was observed compared with the measurement before (1.68 ± 0.11 vs. 1.61 ± 0.10 mmol/l, p < 0.01). This decrease was obscured after the second sleep study with CPAP application (1.68 ± 0.10 vs. 1.64 ± 0.14 mmol/l, NS; Fig. 1). No statistically significant differences were observed in TAS before sleep between the two sleep studies. However, TAS was increased after CPAP application compared with TAS after the first sleep study, although this did not reach statistical significance. In patients with less severe syndrome (AHI <30), a statistically significant decrease in TAS was observed after the first sleep study compared with the measurement before (1.73 ± 0.08 vs. 1.65 ± 0.09 mmol/l, p = 0.01) and statistically significant decrease was still observed after the second sleep study (1.72 ± 0.05 vs. 1.63 ± 0.04 mmol/l, p = 0.003)
In patients with severe syndrome (AHI ≥30), TAS was decreased after the first sleep study compared with the measurement before but not statistically significantly (1.64 ± 0.12 vs. 1.58 ± 0.10 mmol/l, NS) while no differences in TAS were observed after the second sleep study (1.65 ± 0.12 vs. 1.65 ± 0.18 mmol/l, NS). The two groups had no difference in age or BMI. However, TAS values before the first sleep study were statistically significantly lower in patients with severe syndrome compared to those with less severe syndrome (1.64 ± 0.12 vs. 1.73 ± 0.08 mmol/l, p < 0.05) (Table 2). Similar results were observed for TAS values before the second sleep study in patients with severe syndrome compared to patients with less severe syndrome (1.65 ± 0.12 vs. 1.72 ± 0.05 mmol/l, p = 0.05) (Table 2).
After the first sleep study, TAS values were lower in severe syndrome compared to less severe syndrome (1.58 ± 0.10 vs. 1.65 ± 0.09 mmol/l, p < 0.05). However, after the second sleep study with CPAP application, no difference was found between the two groups (1.65 ± 0.18 vs. 1.63 ± 0.04 mmol/l, NS).
Discussion
In the present study, the serum antioxidant capacity of OSAS patients without comorbidities was studied by evaluating TAS before and after an overnight diagnostic sleep study, as well as before and after CPAP application. Decreased TAS was found in the morning compared to the night before sleep, and it was improved after one night with CPAP treatment.
The current knowledge on the presence of increased oxidative stress in OSAS is controversial. Schulz et al. [5] demonstrated enhanced neutrophil superoxide release in OSAS patients compared with controls, which was reversed by CPAP therapy. Increased production of ROS from leukocytes has been reported by Dyugovskaya et al. [6] and increased systemic oxidative stress has been recently found in severe OSAS [7]. Barcello et al. [8] and Lavie et al. [9] have found increased lipid peroxidation in patients with OSAS than in controls. In contrast, several studies have failed to confirm increased oxidative stress, either by finding no differences in lipid peroxidation products [10–13] or in circulating free nitrotyrosine [17].
The role of free radical scavengers in OSAS patients remains unclear. Christou et al. [18] showed that patients with severe OSAS have reduced values of antioxidant capacity and negative correlation between antioxidant capacity and severity of the disease. Wali et al. [12] showed no significant differences in antioxidant enzymes activity such as glutathione peroxidase and catalase in red blood cells in hypoxic and non-hypoxic patients. Additionally, no significant difference was found for superoxide dismutase between patients and control subjects [13].
Recently, further information about the antioxidant status of OSAS patients has been provided. Barcelo et al. [19] reported that patients with OSAS had lower TAS, and vitamin A and vitamin E levels. In accordance with the latter study, the results of our study indirectly support the presence of oxidative stress in OSAS through decreased TAS. However, the present study is differentiated in two points. First, in contrast to many prior studies, two blood samples were drawn for each patient, one before and one after each sleep study. We feel that at least two consecutive measurements should be done in order to demonstrate what has really happened during sleep time. Second, and more important, all our patients were meticulously selected in order to exclude patients with any comorbidities that could have an impact on oxidative stress status and in turn influence the antioxidant status.
In a recent study, Svatikova et al. [11] found that otherwise healthy OSAS patients, without any other comorbidities, do not manifest evidence of higher oxidative stress, as assessed by measuring plasma lipid peroxidation products before sleep and after 4 h of untreated OSAS. However, a split-night protocol was followed meaning that the second measurement took place after only 4 h of sleep and not after waking in the morning. The same limitation could also explain the absence of influence of a few hours’ CPAP treatment on oxidative stress.
Surprisingly, when we divided the patients according to the severity of the disease, decreased TAS in the morning after the first sleep study was revealed only for patients with less severe and not for those with severe syndrome. A plausible explanation could be the difference between any acute effect of hypoxemia immediately resulting from apneic sleep and any chronic state of heightened oxidative stress that may be sustained in severe OSAS patients even during the daytime. In our study, TAS before sleep was statistically significantly decreased in severe compared with less severe OSAS patients, further supporting the aforementioned hypothesis. Furthermore, in the group with severe OSAS, no significant changes in TAS values during the two sleep studies were observed, although most of them were lower than those in the group with less severe syndrome. It is probable that in patients with severe OSAS, the adaptation of the antioxidant mechanisms to increased oxidant burden may restrain the excess diminution of antioxidants levels.
At a first glance, TAS values after CPAP application in the whole population seem to be influenced from TAS values in the group with severe syndrome as no significant change was found compared with the measurements before sleep, while significant decrease in TAS values was still observed in the group with less severe syndrome. However, this finding must be interpreted with caution because in the first group almost all the TAS values were lower than those in the second group and no significant changes during the two sleep studies were observed. Thus, it is not clear whether TAS values in the severe syndrome group are maintained in similar levels as a result of one night of CPAP application or as a consequence of adaptation of the antioxidant mechanisms to increased oxidant burden. We speculate that the decreased TAS values in the severe syndrome could be attributed to either some kind of resistance to increased oxidative stress or a permanent insufficiency of the antioxidant mechanism.
A limitation of the present study is the absence of a second evaluation after prolonged treatment with CPAP application (e.g., 3 months later), as has been performed in previous studies [7], [19]. It seems that CPAP does not immediately ameliorate the redox imbalance despite the improvement in certain oxygenation parameters.
In conclusion, the present study further supports in an indirect way the presence of oxidative stress in otherwise healthy OSAS patients through decreased TAS. One night of CPAP treatment seems to have an additional benefit on OSAS by ameliorating any antioxidant disturbance although not in the same way regarding the severity of the disease. Further studies are warranted on the impact of oxidative stress in antioxidant status and the benefit of prolonged CPAP treatment in patients with severe OSAS.
Abbreviations
- OSAS:
-
Obstructive sleep apnea syndrome
- CPAP:
-
Continuous positive airway pressure
- TAS:
-
Total antioxidant status
- PSG:
-
Polysomnography
- BMI:
-
Body mass index
- AHI:
-
Apnea–hypopnea index
References
McCord MJ (1985) Oxygen derived free radicals in post ischemic tissue injury. New Engl J Med 312:159–163
Douglas NJ, Polo O (1994) Pathogenesis of sleep apnoea/hypopnoea syndrome. Lancet 344:653–655
Bast A, Haenen GRMM, Doelman CJA (1991) Oxidants and antioxidants: state of the art. Am J Med 91(3C):2S–12S
Haliwell B, Gutteridge JMC (1998) Detection of free radicals and other reactive species: trapping and fingerprinting. In: Haliwell B, Gutteridge JMC (eds) Free radicals in biology and medicine, 3rd edn. Oxford University Press, Oxford, pp 351–429
Schulz R, Mahmoudi S, Hattar K, Sibelius U, Olschewski H, Mayer K, Seeger W, Grimminger F (2000) Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea: impact of continuous positive airway pressure therapy. Am J Respir Crit Care Med 162:566–570
Dyugovskaya L, Lavie P, Lavie L (2002) Increased adhesion molecules expression and production of reactive oxygen species in leukocytes of sleep apnea patients. Am J Respir Crit Care Med 165:934–939
Christou K, Kostikas K, Pastaka C, Tanou K, Antoniadou I, Gourgoulianis KI (2009) Nasal continuous positive airway pressure treatment reduces systemic oxidative stress in patients with severe obstructive sleep apnea syndrome. Sleep Med 10(1):87–94
Barcelo A, Miralles C, Barbe F, Vila M, Pons S, Agusti AGN (2000) Abnormal lipid peroxidation in patients with sleep apnoea. Eur Respir J 16:644–647
Lavie L, Vishnevsky A, Lavie P (2004) Evidence for lipid peroxidation in obstructive sleep apnea. Sleep 27:123–128
Ozturk L, Mansour B, Yuksel M, Yalcin AS, Celikoglou F, Gokhan N (2003) Lipid peroxidation and osmotic fragility of red blood cells in sleep-apnea patients. Clin Chim Acta 332:83–88
Svatikova A, Wolk R, Lerman LO, Juncos LA, Greene EL, McConnell JP, Somers VK (2005) Oxidative stress in obstructive sleep apnoea. Eur Heart J 26:2435–2439
Wali SO, Bahammam AS, Massaeli H, Pierce GN, Iliskovic N, Singal PK, Kryger MH (1998) Susceptibility of LDL to oxidative stress in obstructive sleep-apnea. Sleep 21:290–296
Alzoghaibi MA, Bahammam AS (2005) Lipid peroxides, superoxide dismutase and circulating IL-8 and GCP-2 in patients with severe obstructive sleep apnea: a pilot study. Sleep Breath 9:119–126
Rechtschaffen A, Kales A (eds) (1968) A manual of standardized terminology, techniques, and scoring system for sleep stages of human subjects. US Department of Health, Education, and Welfare Public Health Service—NIH/NIND
(1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
The Atlas Task Force (1992) EEG arousals: scoring rules and examples; a preliminary report from the sleep disorders Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Svatikova A, Wolk R, Wang HH, Otto ME, Bybee KA, Singh RJ, Somers VK (2004) Circulating free nitrotyrosine in obstructive sleep apnea. Am J Physiol Regul Integr Comp Physiol 287:284–287
Christou K, Moulas AN, Pastaka C, Gourgoulianis KI (2003) Antioxidant capacity in obstructive sleep apnea patients. Sleep Med 4:225–228
Barcelo A, Barbe F, de la Pena M, Vila M, Perez G, Pierola J, Duran J, Agusti AGN (2006) Antioxidant status in patients with sleep apnoea and impact of continuous positive airway treatment. Eur Respir J 27:756–760
Conflict of interest
All authors declare that they have no conflict of interest and have received no financial or other support or benefit from any source regarding the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katsoulis, K., Kontakiotis, T., Spanogiannis, D. et al. Total antioxidant status in patients with obstructive sleep apnea without comorbidities: the role of the severity of the disease. Sleep Breath 15, 861–866 (2011). https://doi.org/10.1007/s11325-010-0456-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0456-y